Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Diagnostic Accuracy of Capillary Blood Glucometer Testing for Gestational Diabetes
Authors Gallardo-Rincón H , Lomelin-Gascon J, Martinez-Juarez LA , Montoya A , Ortega-Montiel J , Galicia-Hernandez V, Álvarez-Hernández DA , Ávila-Domínguez R, Reyes-Muñoz E , Illescas-Correa LM, Diaz Martinez DA, Magos Vázquez FJ , Vargas Ávila EO, Benitez-Herrera AE, Reyes-Gómez D, Carmona-Ramos MC, Hernández-González L, Romero-Islas O, Mújica-Rosales R , Tapia-Conyer R
Received 18 September 2022
Accepted for publication 1 December 2022
Published 14 December 2022 Volume 2022:15 Pages 3855—3870
DOI https://doi.org/10.2147/DMSO.S389420
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Héctor Gallardo-Rincón,1,2 Julieta Lomelin-Gascon,2 Luis Alberto Martinez-Juarez,2 Alejandra Montoya,2 Janinne Ortega-Montiel,2 Victoria Galicia-Hernandez,2 Diego-Abelardo Álvarez-Hernández,2 Rosangela Ávila-Domínguez,2 Enrique Reyes-Muñoz,3 Lucía Marcela Illescas-Correa,4 Daniel Alberto Diaz Martinez,5 Francisco Javier Magos Vázquez,5 Edwin Oswaldo Vargas Ávila,5 Alejandro Efraín Benitez-Herrera,6 Diana Reyes-Gómez,6 María Concepción Carmona-Ramos,6 Laura Hernández-González,6 Oscar Romero-Islas,6 Ricardo Mújica-Rosales,2 Roberto Tapia-Conyer7
1University of Guadalajara, Health Sciences University Center, Guadalajara, Jalisco, Mexico; 2Carlos Slim Foundation, Mexico City, Mexico; 3Coordination of Gynecological and Perinatal Endocrinology, National Institute of Perinatology, Mexico City, Mexico; 4Maternal and Childhood Research Center (CIMIGEN), Mexico City, Mexico; 5Ministry of Health of the State of Guanajuato, Guanajuato, Mexico; 6Ministry of Health of the State of Hidalgo, Pachuca, Hidalgo, Mexico; 7National Autonomous University of Mexico, School of Medicine, Mexico City, Mexico
Correspondence: Luis Alberto Martinez-Juarez, Carlos Slim Foundation, Lago Zurich 245, Presa Falcon Building (Floor 20), Miguel Hidalgo, Mexico City, 11529, Mexico, Tel +52 55 53 39 17 70, Fax +52 55 53 39 17 70, Email [email protected]
Purpose: Few pregnant women in low-resource settings are screened for gestational diabetes mellitus (GDM) using the gold standard oral glucose tolerance test (OGTT). This study compared capillary blood glucose testing with 2-h plasma glucose measurements obtained using the 75-g OGTT to screen for GDM at primary healthcare clinics in Mexico.
Patients and Methods: Pregnant women who participated in a previous prospective multicenter longitudinal cohort study and who had not been previously diagnosed with diabetes were included. Participants were evaluated using the plasmatic 2-h 75-g OGTT with simultaneous capillary blood glucose measurements using a glucometer. The study endpoint was the comparability of the glucometer results to the gold standard OGTT when collected simultaneously. Sensitivity, specificity, and area under the curve of the glucose measurements obtained for capillary blood compared with venous plasma (gold standard) were calculated to determine diagnostic accuracy.
Results: The study included 947 pregnant women who had simultaneous glucose measurements available (blood capillary [glucometer] and venous blood OGTT). Overall, capillary blood glucose testing was very sensitive (89.47%); the specificity was 66.58% and the area under the curve (95% confidence interval) was 0.78 (0.74– 0.81). The sensitivity, specificity and area under the curve of each capillary measurement were: 89.47%, 66.58% and 0.78 (0.74– 0.82) for the fasting measurement, 91.53%, 93.24% and 0.92 (0.88– 0.96) for the one-hour measurement, and 89.80%, 93.32%, 0.91 (0.87– 0.95) for the second-hour measurement, respectively. No adverse events were reported.
Conclusion: Capillary OGTT is a valid alternative to the gold standard OGTT for screening of GDM in low-resource situations or in situations where there are other limitations to performing the OGTT as part of primary healthcare services.
Keywords: capillary blood glucose, gestational diabetes mellitus, low-resource, Mexico, oral glucose tolerance test, screening
Introduction
Gestational diabetes mellitus (GDM) is a condition diagnosed during pregnancy that was not clearly overt diabetes prior to gestation.1 GDM is a neglected risk to the health of both mothers and children and can lead to numerous pregnancy-related complications including babies with a larger birth weight, high blood pressure, and obstructed labor.2 Approximately half of women who experience GDM subsequently develop type 2 diabetes mellitus in the 5–10 years after their baby is delivered.2 The estimated global prevalence of GDM in 2021 was between 4.3% and 38.1%.3 The prevalence for North America and the Caribbean is reported to be 20.7%,4 and in Mexico, while data are insufficient to determine the national prevalence of GDM, it is estimated to be between 10% and 12%.5,6
Screening and diagnostic strategies for GDM have been a focus of international debate.7,8 Currently, the 75-g oral glucose tolerance test (OGTT) is considered the gold standard for diagnosing GDM. The American Diabetes Association (ADA) recommends OGTT with three plasma glucose measurements (fasting and 1 and 2 h after consuming 75 g glucose) at 24–28 weeks of gestation for the diagnosis of GDM.1 In Mexico, these same criteria are recommended.5,9 However, there have been studies suggesting that capillary blood glucose measurement, an approach that could be provided more widely, including in low-resource settings, is sufficiently sensitive for diagnosis of GDM.10–12 Moreover, the International Association of Diabetes and Pregnancy Study Group (IADPSG) criteria suggest a 75-g OGTT at 24–28 weeks, and indicate a GDM diagnosis if any one of the following cutoffs of fasting plasma glucose are met: ≥5.1 mmol/L (≥92 mg/dL), 1-h OGTT ≥10 mmol/L (≥180 mg/dL), or 2-h OGTT ≥8.5 mmol/L (≥153 mg/dL).13 In fact, the prevalence of GDM is nearly three-fold higher using the IADPSG criteria compared with the ADA criteria.6
Although early diagnosis is key to improving outcomes among mothers with GDM and their babies, there are difficulties with GDM screening and limited OGTT availability in low-resource settings.14–17 Providing more readily available, simple, easy-to-use GDM screening methods such as the glucometer that provide rapid results, particularly in situations where there are limitations to performing the OGTT as part of primary healthcare services, may help to ameliorate this burden. The aim of this study was to compare capillary blood glucometer testing to 2-h plasma glucose measurements using OGTT for GDM diagnosis at primary healthcare clinics in Mexico.
Patients and Methods
Sample Selection and Study Design
This analysis included information of pregnant women who participated in the prospective multicenter longitudinal cohort study Cuido Mi Embarazo in Mexico. This study included data from six different sites, three of which were primary healthcare facilities in Hidalgo, two in Guanajuato, and one in Mexico City. The data used for this study came from pregnant women who took the 2-h 75-g OGTT between 24 and 28 weeks of gestation. In order to be included in the analysis, these women had to agree to participate in the Cuido Mi Embarazo cohort study and have complete information available from April 2019 to May 2021. Women who were diagnosed with pregestational diabetes or who had a multiple pregnancy were excluded from this analysis.
For this study, we chose 947 women from the 1306 enrolled in the Cuido mi Embarazo cohort who met the criteria for complete data (this included the three venous glucose measurements of the 2-hr 75-g OGTT [gold standard] and the three capillary glucose measurements taken at the time of gold-standard measurement). There was no specific selection criterion.
Interventions
Data regarding socio-demographic characteristics, medical history, regular medical visits, laboratory and ultrasound data, pregnancy resolution, and management of self-monitoring for GDM were collected using standardized questionnaires. Pregnant women were evaluated for GDM between weeks 24 and 28 of their pregnancy. Evaluations included the gold standard plasma 2-h 75-g OGTT performed according to the IADPSG criteria13 with simultaneous glucose measurement of capillary whole blood using a glucometer (Accu-Check Instant®; Roche, Basel, Switzerland) for safety and quality control of the test across the centers. The glucometer readings were taken before the participant drank the 75-g glucose solution for the OGTT and 1 h and 2 h afterwards. Glucose levels measured by capillary blood and venous plasma during the 2-h 75-g OGTT were collected for all participants.
A diagnosis of GDM was made based on the 2020 criteria of the ADA, which are similar to the diagnostic criteria recommended by Mexican guidelines (any single value met or exceeded the following: a fasting value of 5.1 mmol/L [92 mg/dL]; a 1-h value of 10.0 mmol/L [180 mg/dL]; or a 2-h value of 8.5 mmol/L [153 mg/dL]).1,18 For this analysis, the same diagnostic criteria were applied to the 2-h 75-g OGTT and glucometer readings. The results of the glucometer were immediately available while those from the 2-h 75-g OGTT were delayed due to the processing times at the diagnostic laboratory. Diagnosis and treatment decisions were made based on the plasma OGTT results.
Endpoint
The primary endpoint of this study was the comparability of the glucometer results to the gold standard 2-h 75-g OGTT when the tests were done on the same person at the same time. The diagnostic accuracy was determined by calculating the sensitivity, specificity, and area under the receiver operating characteristic (ROC) curve of the glucose measurements obtained for capillary blood compared with venous plasma (gold standard).
Ethics
The study protocol was approved by the Research and Ethics Committees of the Secretary of Health of Hidalgo State (FSSA2018076) and the Secretary of Health of Guanajuato State (CONBIOETICA-11-CEI-003-20190704), and all participants provided written informed consent. The study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonization guidelines for Good Clinical Practice, and applicable local laws and regulations. The study was registered at researchregistry.com (researchregistry7405). This report was prepared according to Standards for Reporting of Diagnostic Accuracy guidelines for accurate reporting.19
Statistical Analysis
Patient characteristics and biomarkers were compared between the GDM and non-GDM groups. Continuous variables are presented as mean and standard deviation (SD), and categorical variables are presented as n (%). Categorical variables were compared using the chi-square test and between-group comparisons were made using the independent Student’s t-test.
To determine whether a different cutoff value for GDM diagnosis should be considered, a sensitivity and specificity analysis was conducted. Diagnostic accuracy was evaluated by calculating the area under the ROC curve, and the sensitivity and specificity of the glucometer test compared with the plasma test using the known cutoff points of the gold standard. The Youden’s J statistic20 was used to determine the empirical cutoff that maximizes the diagnostic effectiveness of the OGTT. Statistical significance was set at p <0.05. No indeterminate results were reported. Data were analyzed using STATA software, version 15.0 (College Station, TX, USA).
Results
Data from a total of 947 pregnant women from the Cuido Mi Embarazo study were analyzed. Of these, 133 participants were diagnosed with GDM (14.04%) and 814 had normal blood glucose levels. Participant demographic and baseline characteristics are shown in Table 1. The percentage of women with GDM increased with age; 67.7% versus 48.4% of women in the GDM and non-GDM groups, respectively, were ≥25 years (p=0.001). Pregestational body mass index, family history of diabetes, and capillary casual glucose at enrollment were also significantly higher in the GDM versus the non-GDM group. As expected, all three glucose values (fasting, 1 h, and 2 h) after the 2-h 75-g OGTT were significantly higher in the GDM group versus the non-GDM group. Although the capillary blood glucometer values (fasting, 1-h, and 2-h) were slightly higher than venous plasma values, they followed the same trend.
 |
Table 1 Participant Demographic and Background Characteristics |
Capillary Blood Glucose versus Plasma OGTT
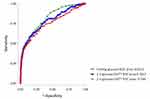
There were 391 (41.29%) pregnant women diagnosed with GDM using glucometer measurements and 133 (14.04%) using venous plasma glucose measurements. The area under the ROC curve of the capillary blood measurements with respect to the venous plasma measurements (gold standard) is shown in Figure 1. The area under the ROC curve (95% confidence interval [CI]) for the capillary blood glucometer measurement was 0.78 (0.74–0.81) and the sensitivity and specificity were 89.47% and 66.58%, respectively (Table 2). Sensitivity and specificity data for fasting, 1-h, and 2-h capillary blood glucose analysis using different cutoff points are shown in Tables 3–5, respectively. The empirical optimal cutoff using the maximum of Youden’s J statistic was ≥5.2 mmol/L (≥93 mg/dL) for the fasting value, ≥9.7 mmol/L (≥174 mg/dL) for the 1-h value, and ≥8.4 mmol/L (≥152 mg/dL) for the 2-h value (maximum of Youden’s J statistic: 0.61, 0.86, and 0.87, respectively). The area under the ROC curve at fasting, 1 h, and 2 h were 0.78 (0.74–0.82), 0.92 (0.88–0.96), and 0.91 (0.87–0.95), respectively. The sensitivity and specificity at fasting were 85.23% and 71.59%, respectively, 91.53% and 93.24% at 1 h, and 89.80% and 93.32% at 2 h (Table 2).
 |
Table 2 Area Under the ROC Curve, Sensitivity, and Specificity of Capillary Blood Glucose Measurements with Respect to the Gold Standard (Venous Plasma Glucose Measurements) |
 |
Table 3 Sensitivity and Specificity of Different Cutoff Points from the Fasting Capillary Blood Glucose Test |
 |  |  |  |
Table 4 Sensitivity and Specificity of Different Cutoff Points from the 1-h Capillary Blood Glucose Test |
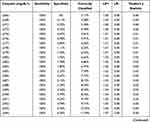 |  |  |  |
Table 5 Sensitivity and Specificity of Different Cutoff Points from the 2-h Capillary Blood Glucose Test |
The rate of true positives for the capillary blood glucose measurements was 89.5% and the true negative rate was 66.6% (Table 6). The false positive and false negative rates were 33.4% and 10.5%, respectively. There were no adverse events reported in this study.
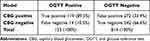 |
Table 6 Rate of True Positives, False Positives, and False Negatives for Capillary Blood Glucose Measurements |
Discussion
This analysis, conducted with data from the Cuido Mi Embarazo cohort, analyzed alternative strategies for detecting and diagnosing GDM. Preliminary findings indicate that capillary blood glucose testing may be considered an alternative method for GDM screening when gold standard testing is unavailable or when other barriers to an OGTT exist, such as younger maternal age, lower socioeconomic status, higher parity, intolerance of or prior unpleasant experiences with the test protocol, competing priorities, inconvenience, difficulty arranging transport or childcare, and social or mental health issues.21–24
When 2-h 75-g OGTT was assessed using capillary blood glucose measurements, the area under the ROC curve of 0.78 (95% CI, 0.74–0.81) supported the use of glucometer readings for GDM screening using the same reference values as those used for the gold standard testing.1,18 Capillary blood glucose values are reported to be similar to venous plasma glucose values, with an insignificant mean difference of 0.01 mmol/L (0.18 mg/dL) between the two methods.10 Some studies suggest that capillary blood glucose is adequately sensitive and specific to be considered an alternative method to plasmatic OGTT for GDM screening.10–12 The present study reported a sensitivity of 89.47% and a specificity of 66.58% with capillary blood glucose measurements; the specificity value is somewhat lower than that reported in similar studies.
Sensitivity and specificity could be improved by considering new diagnostic values for use with capillary blood measurements, prioritizing the sensitivity of the test. For example, when the cutoff point for the fasting capillary blood glucose test is adjusted to ≥5.2 mmol/L (≥93 mg/dL), which is the empirical optimal cutoff point (maximum of Youden’s J statistic, 0.61), the sensitivity and specificity were 84.09% and 76.48%, respectively. Similar adjustments could be made for the 1-h and 2-h timepoint, where the respective empirical optimal cutoff points were ≥9.7 mmol/L (≥174 mg/dL) and ≥8.4 mmol/L (≥152 mg/dL) (maximum of Youden’s J statistic, 0.86 and 0.87, respectively). At these optimal cutoff points, the sensitivity and specificity were 96.61% and 89.19%, respectively, for the 1-h value and 93.88% and 92.76%, respectively, for the 2-h value. A comparison of the GDM diagnostic abilities of the Accu-Chek glucometer (capillary whole blood) versus venous puncture found a 100% specificity and 95% sensitivity for the capillary whole blood method versus the venous puncture method using a blood glucose level cutoff of 7.8 mmol/L (140 mg/dL).25 Together, these findings support the use of a simpler diagnostic test for GDM.
Capillary glucose levels obtained from pregnant women 2 h after consuming 75-g glucose had a sensitivity of 80.2% and a specificity of 98.5% relative to venous plasma glucose levels using a 7.8 mmol/L (140 mg/dL) blood glucose cutoff level, supporting a recommendation of standard cutoff values for GDM screening using capillary blood glucose measurements.11 However, a similar study found a sensitivity and specificity of 62.3% and 80.7%, respectively, using a 7.8 mmol/L (140 mg/dL) cutoff, which was improved when a cutoff of 6.1 mmol/L (110 mg/dL) was used (78.3% and 92.5%, respectively), suggesting that cutoff values may need further assessment.12
Although sensitivity and specificity analyses in the present study indicated that the specificity of diagnosis using capillary blood glucose values was lower compared with venous plasma, we consider it best to use the current consensus cutoff values for screening. This may lead to overdiagnosis of GDM; however, most pregnant women diagnosed with GDM are required to perform at-home glucose self-monitoring using a glucometer and capillary blood prior to determining the appropriate therapeutic approach for each patient. Decisions on therapeutic approach are based on the capillary self-monitoring results. Initially, most patients are advised to control their glucose levels with non-pharmacological strategies such as lifestyle changes focused on nutrition and exercise. These recommendations benefit all pregnant women, not just those diagnosed with GDM.
In this study, 33.4% of the capillary blood glucose measurements were false positives, while 89.5% were true positives. It is important to note that these false positives were based on the gold-standard OGTT cutoff values as recommended by the ADA and the Mexican guidelines for diagnosing GDM. However, as previously discussed, the sensitivity and specificity of this test could be improved if more accurate cutoff values for capillary blood screening were considered. Overall, we recommend adhering to the ADA’s proposed cutoff values when performing OGTT with capillary measurements, as there are significant advantages to false positive values. False positives identify patients with glucose values that are close to the level required for a GDM diagnosis but that have not yet reached that level. Such patients would likely benefit from being identified as high-risk for developing GDM and may receive more focused medical attention in the weeks following their false-positive result. As such, they may be instructed on non-pharmacological strategies focused on nutrition and lifestyle changes. Dietary interventions such as dietary counseling have been shown to reduce the risk for GDM and significantly lower gestational weight gain compared with pregnant women who did not receive counseling26,27 and may reduce the incidence of caesarean sections.27 Physical activity interventions have also been reported to reduce the risk of GDM and lower gestational weight gain.28,29 Combined dietary and physical activity interventions may provide even greater benefit than either type of intervention alone, particularly for certain populations, such as those who are overweight or obese during pregnancy.26,30,31
Furthermore, early changes in lifestyle can significantly reduce the incidence of GDM among high-risk pregnant women.31,32 Detection of risk factors using a predictive tool such as The Fetal Medicine Foundation’s risk assessment for GDM may be useful during the first weeks of pregnancy,33 though differences among populations must be considered. Overall, when coupling information regarding GDM prevention with GDM screening using capillary blood glucose testing this may benefit both pregnant women and their babies in low-resource areas where venous blood collection is difficult or impossible.
Given the substantial health effects of GDM on both pregnant women and their babies, which may include short-term effects such as spontaneous abortion, preeclampsia, and neonatal respiratory distress syndrome and long-term effects such as impaired glucose metabolism, type 2 diabetes, cardiovascular disease/hypertension, and obesity,34,35 a validated, simple method for GDM screening may be quite beneficial. Additionally, the ease of operational use of the capillary blood glucometer in low-resource settings should be acknowledged when considering appropriate screening and diagnosis approaches. Obtaining venous blood samples may be challenging or even impossible in low-resource settings given venous blood collection requires more training compared with capillary blood collection.12,25 Furthermore, capillary blood collection is minimally invasive, better tolerated, portable, and is expected to be more cost-effective.
This study had several limitations. Mexican women were exclusively enrolled, potentially limiting the generalizability. Additionally, a single blood capillary glucose testing device was evaluated; different devices may vary in sensitivity.
Conclusion
The results of the present retrospective cohort analysis demonstrate the adequate sensitivity of capillary blood glucose testing. Although plasma blood glucose testing is considered the gold standard screening test for GDM, there are a number of challenges to its widespread use, including a lack of availability in low-resource settings, where we suggest consideration of capillary blood glucose testing as an alternative screening method.
Data Sharing Statement
The full deidentified dataset is shown in Supplementary Appendix 1. The full study protocol is available from the corresponding author upon request.
Ethics Approval and Informed Consent
The cohort protocol was approved by each site’s institutional review board, and all participants provided written informed consent. The study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonization guidelines for Good Clinical Practice, and applicable laws and regulations. The study was registered at researchregistry.com (researchregistry7405).
Consent for Publication
All authors agree to the publication of this paper.
Acknowledgments
This study was funded by Global Health Partnerships Eli Lilly and Company. The authors thank Sarah Bubeck, PhD, of Edanz (www.edanz.com) for providing medical writing support, which was funded by the Carlos Slim Foundation, in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). Preliminary results of this study were previously presented at the American Diabetes Association’s 80th Scientific Sessions (June 12–16, 2020). The abstract has been published (Gallardo H et al Diabetes 2020;69 (Supplement_1):1358-P). We acknowledge the support of the Centre for Maternal and Infant Research (CIMIGEN) and the Ministry of Health of the States of Hidalgo and Guanajuato for their help in performing this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding for this study was provided by Global Health Partnerships Eli Lilly and Company. The funder had no role in the study design; collection, analysis, and interpretation of data; writing of the report; or the decision to submit the report for publication. Carlos Slim Foundation developed the study design, analysis and interpretation of data, and was involved in the writing of the report; the Ministry of Health Guanajuato was involved in the collection of data; the Ministry of Health Hidalgo was involved in the collection of data; and CIMIGEN was involved in the collection of data.
Disclosure
HGR, JLG, LAMJ, AM, JOM, VGH, DAAH, RAD and RMR, are employees of the Carlos Slim Foundation. The authors report no other conflicts of interest in this work.
References
1. American Diabetes Association Professional Practice Committee. Chapter 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17–38. doi:10.2337/dc22-S002
2. International Diabetes Federation. Care & prevention; 2020. Available from: https://www.idf.org/our-activities/care-prevention/gdm.
3. International Diabetes Federation. Hyperglycaemia in pregnancy (Hip) (20–49 y): prevalence of gestational diabetes mellitus (GDM). Available from: https://diabetesatlas.org/data/en/indicators/14/.
4. International Diabetes Federation. Diabetes atlas 2021. 10th edition; 2021. Available from: https://diabetesatlas.org/atlas/tenth-edition/.
5. Centro Nacional de Equidad de Género y Salud Reproductiva. Diabetes y Embarazo: lineamiento técnico [Diabetes and Pregnancy: technical guidelines]. Ciudad de Mexico; 2017. Available from: http://cnegsr.salud.gob.mx/contenidos/descargas/SMP/LineamientoDiabetesyEmbarazo.pdf.
6. Reyes-Muñoz E, Parra A, Castillo-Mora A, Ortega-González C. Effect of the diagnostic criteria of the international association of diabetes and pregnancy study groups on the prevalence of gestational diabetes mellitus in urban Mexican women: a cross-sectional study. Endocr Pract. 2012;18(2):146–151. doi:10.4158/EP11167.OR
7. Huhn EA, Rossi SW, Hoesli I, Göbl CS. Controversies in screening and diagnostic criteria for gestational diabetes in early and late pregnancy. Front Endocrinol. 2018;9:696. doi:10.3389/fendo.2018.00696
8. Vince K, Perković P, Matijević R. What is known and what remains unresolved regarding gestational diabetes mellitus (GDM). J Perinat Med. 2020;48(8):757–763. doi:10.1515/jpm-2020-0254
9. Secretaria de Salud de Mexico. Algoritmos de atención clínica: embarazo [Clinical care algorithms: Pregnancy care]. Ciudad de Mexico; 2019. Available from: http://educads.salud.gob.mx/sitio/recursos/EMBARAZO.pdf.
10. Kumar G, Sng BL, Kumar S. Correlation of capillary and venous blood glucometry with laboratory determination. Prehospital Emerg Care. 2004;8:378–383. doi:10.1016/j.prehos.2004.06.010
11. Balaji V, Madhuri BS, Paneerselvam A, Arthi T, Seshiah V. Comparison of venous plasma glucose and capillary whole blood glucose in the diagnosis of gestational diabetes mellitus: a community-based study. Diabetes Technol Ther. 2012;14:131–134. doi:10.1089/dia.2011.006
12. Bhavadharini B, Mahalakshmi MM, Maheswari K, et al. Use of capillary blood glucose for screening for gestational diabetes mellitus in resource-constrained settings. Acta Diabetol. 2016;53(1):91–97. doi:10.1007/s00592-015-0761-9
13. Metzger BE, Gabbe SG, Persson B, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi:10.2337/dc09-1848
14. Putoto G, Somigliana E, Olivo F, et al. A simplified diagnostic work-up for the detection of gestational diabetes mellitus in low resources settings: achievements and challenges. Arch Gynecol Obstet. 2020;302(5):1127–1134. doi:10.1007/s00404-020-05708-x
15. Bhavadharini B, Uma R, Saravanan P, Mohan V. Screening and diagnosis of gestational diabetes mellitus – relevance to low and middle income countries. Clin Diabetes Endocrinol. 2016;2:13. doi:10.1186/s40842-016-0031-y
16. Budreviciute A, Damiati S, Sabir DK, et al. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. 2020;8:574111. doi:10.3389/fpubh.2020.574111
17. Atlaw D, Sahiledengle B, Assefa T, et al. Incidence and risk factors of gestational diabetes mellitus in Goba town, Southeast Ethiopia: a prospective cohort study. BMJ Open. 2022;12(9):e060694. doi:10.1136/bmjopen-2021-060694
18. Diario Oficial de la Federación. NORMA Oficial Mexicana NOM-007-SSA2-2016 para la atención de la mujer durante el embarazo, parto y puerperio, y de la persona recién nacida [Mexican Official Standard NOM-007-SSA2-2016 for the care of women during pregnancy, childbirth and puerperium, and of the newborn]. Available from: https://www.dof.gob.mx/nota_detalle.php?codigo=5432289&fecha=07/04/2016#gsc.tab=0.
19. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. Clin Chem. 2015;61(12):1446–1452. doi:10.1373/clinchem.2015.246280
20. Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35.
21. Lachmann EH, Fox RA, Dennison RA, Usher-Smith JA, Meek CL, Aiken CE. Barriers to completing oral glucose tolerance testing in women at risk of gestational diabetes. Diabet Med. 2020;37(9):1482–1489. doi:10.1111/dme.14292
22. Sunny SH, Malhotra R, Ang SB, et al. Facilitators and barriers to post-partum diabetes screening among mothers with a history of gestational diabetes mellitus-a qualitative study from Singapore. Front Endocrinol. 2020;11:602. doi:10.3389/fendo.2020.00602
23. Sanderson H, Loveman E, Colquitt J, Royle P, Waugh N, Tan BK. Improving uptake of postnatal checking of blood glucose in women who had gestational diabetes mellitus in universal healthcare settings: a systematic review. J Clin Med. 2018;8(1):4. doi:10.3390/jcm8010004
24. Dennison RA, Fox RA, Ward RJ, Griffin SJ, Usher-Smith JA. Women’s views on screening for type 2 diabetes after gestational diabetes: a systematic review, qualitative synthesis and recommendations for increasing uptake. Diabet Med. 2020;37(1):29–43. doi:10.1111/dme.14081
25. Dacus J, Schulz K, Averill A, Sibai B. Comparison of capillary Accu-Chek blood glucose values to laboratory values. Am J Perinatol. 1989;6(3):334–336. doi:10.1055/s-2007-999608
26. Facchinetti F, Dante G, Petrella E, Neri I. Dietary interventions, lifestyle changes, and dietary supplements in preventing gestational diabetes mellitus: a literature review. Obstet Gynecol Surv. 2014;69(11):669–680. doi:10.1097/OGX.0000000000000121
27. Tanentsapf I, Heitmann BL, Adegboye AR. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. BMC Pregnancy Childbirth. 2011;11:81. doi:10.1186/1471-2393-11-81
28. Russo LM, Nobles C, Ertel KA, Chasan-Taber L, Whitcomb BW. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(3):576–582. doi:10.1097/AOG.0000000000000691
29. Sanabria-Martínez G, García-Hermoso A, Poyatos-León R, Álvarez-Bueno C, Sánchez-López M, Martínez-Vizcaíno V. Effectiveness of physical activity interventions on preventing gestational diabetes mellitus and excessive maternal weight gain: a meta-analysis. BJOG. 2015;122(9):1167–1174. doi:10.1111/1471-0528.13429
30. Silva-Zolezzi I, Samuel TM, Spieldenner J. Maternal nutrition: opportunities in the prevention of gestational diabetes. Nutr Rev. 2017;75(suppl 1):32–50. doi:10.1093/nutrit/nuw033
31. Petrella E, Malavolti M, Bertarini V, et al. Gestational weight gain in overweight and obese women enrolled in a healthy lifestyle and eating habits program. J Matern Fetal Neonatal Med. 2014;27(13):1348–1352. doi:10.3109/14767058.2013.858318
32. Koivusalo SB, Rono K, Klemetti MM, et al. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish gestational diabetes prevention study (RADIEL): a randomized controlled trial. Diabetes Care. 2016;39(1):24–30. doi:10.2337/dc15-0511
33. The Fetal Medicine Foundation. Risk assessment for gestational diabetes mellitus; 2022. Available from: www.fetalmedicine.org/research/assess/gdm.
34. American Diabetes Association. 14. Management of diabetes in pregnancy: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl1):S200–S10. doi:10.2337/dc21-S014
35. McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5:47. doi:10.1038/s41572-019-0098-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.