Back to Journals » Risk Management and Healthcare Policy » Volume 17
Development of the Readiness for Hospital Discharge Scale for Patients with Bile Duct Carcinoma Catheterized After Percutaneous Transhepatic Cholangial Drainage: A Validity and Reliability Study
Authors Zhao J, Ding W, Fan B, Chen C, Wang L
Received 20 October 2023
Accepted for publication 20 December 2023
Published 12 January 2024 Volume 2024:17 Pages 117—126
DOI https://doi.org/10.2147/RMHP.S445841
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gulsum Kubra Kaya
Jia Zhao,1,* Wenbin Ding,1,* Benfang Fan,2 Chunxia Chen,1 Lihua Wang2
1Department of Interventional Radiology, Nantong First People’s Hospital, Nantong, 226001, People’s Republic of China; 2Nursing Department, Nantong First People’s Hospital, Nantong, 226001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lihua Wang, Nursing Department, Nantong First People’s Hospital, No. 666 of Shengli Road, Chongchuan District, Nantong, 226001, People’s Republic of China, Tel +86 513 81111039, Email [email protected]
Objective: We develop the Readiness for Hospital Discharge Scale (RHDS) for patients with bile duct carcinoma catheterized after percutaneous transhepatic cholangial drainage (PTCD) and test the reliability and validity of the scale, so as to provide a quantitative tool for evaluating the discharge readiness of patients catheterized after PTCD.
Methods: The initial scale was developed following literature review, qualitative interviews, expert consultation, and other methods based on Meleis’ Theory of Transition. We selected a total of 286 patients with bile duct carcinoma catheterized after PTCD from four tertiary A-grade hospitals in Nantong City. We conducted a cross-sectional survey using the initial scale to test the validity and reliability of the scale.
Results: RHDS for patients catheterized post-PTCD consisted of five dimensions, with a cumulative variance contribution rate of 74.6%. The Cronbach’s α coefficient of the scale was 0.856, and that of each dimension was between 0.740 and 0.891; the scale-content validity index (S-CVI) was 0.875.
Conclusion: RHDS for patients with bile duct carcinoma catheterized after PTCD developed in this study, has good reliability and validity, and can be a useful tool for evaluating the discharge readiness of patients with bile duct carcinoma catheterized after PTCD.
Keywords: bile duct carcinoma, discharge readiness, percutaneous transhepatic cholangial drainage, scale
Background
Although immune checkpoint inhibitors (ICIs) have revolutionized the treatment landscape of bile duct carcinoma,1–4 percutaneous transhepatic cholangial drainage (PTCD), which causes relatively minor trauma and can rapidly relieve patients’ jaundice symptoms while ameliorating liver function, has become the best treatment for malignant obstructive jaundice caused by bile duct carcinoma.5–7
For patients with advanced cholangiocarcinoma who have lost the opportunity for radical surgery, PTCD drainage tube plays an important role in relieving biliary obstruction, and it is also a “life pipeline”, so it is particularly important to teach patients how to maintain the pipeline and always keep the pipeline in place and unobstructed before discharge. At present, commonly, patients are discharged from hospital and live with a catheter after PTCD, but there still exist problems such as long survival time with catheter and high complications in catheter nursing after the patient is discharged with a catheter.8 In the current clinical practice, most studies involving patients’ discharge readiness adopt universal scale and some assessment tools for discharge readiness of special groups involve parturients, surgical patients, schizophrenia patients, and so on. Obviously, it lacks tools to evaluate whether patients with a catheter after PTCD are discharged with the required knowledge of the disease, whether they have the ability to maintain catheters, their psychological status, whether they are well-prepared for discharge, and other aspects remain a challenge, which affects the quality of managing hospital treatment and post-discharge nursing. Thus, it is important to effectively explore tools for evaluation of discharge readiness in patients post-PTCD. In this study, we aimed to develop a Readiness for Hospital Discharge Scale (RHDS) suitable for patients with bile duct carcinoma catheterized after PTCD and to test the validity and reliability of the scale, so as to provide a quantitative tool for evaluating the discharge readiness of patients catheterized post-PTCD.
Study Design
Theoretical Framework and Operational Definition
In this study, we adopted the following operational definition of the discharge readiness of patients with bile duct carcinoma catheterized after PTCD based on Meleis’ Theory of Transition:9 Discharge readiness of patients with bile duct carcinoma catheterized after PTCD refers to the catheterized patients’ ability to adapt to the transition from hospital to home after PTCD for bile duct carcinoma. Based on literature review, analysis of existing RHDS,10–16 experiences of catheterized patients with bile duct carcinoma after PTCD, domestic medical and cultural background, and other aspects, we finalized the dimensions of this scale to include physiological status, psychological status, role adaptation, social support, and self-efficacy.
Development of the Initial Scale
We generated the item pool mainly through literature analysis, qualitative interviews, expert consultation, and other methods, which are detailed below:
- Literature analysis: According to the definition of “discharge readiness of patients with bile duct carcinoma catheterized after PTCD” and the definition and description of RHDS dimensions, we systematically searched Chinese and English databases using keywords such as “PTCD”, “percutaneous transhepatic cholangial drainage”, “discharge readiness”, “psychological status”, and “self-efficacy”, and collected literature on the nursing and discharge readiness of patients catheterized post-PTCD as sources for item generation for RHDS for patients catheterized post-PTCD.12
- Qualitative study: In view of the diversity in gender, age, economic level, education, and other characteristics, for this study, we selected patients catheterized post-PTCD from a tertiary A-grade hospital in Nantong City from August to September 2021 using maximum difference purposive sampling for in-depth semi-structured interviews. Interviewees were asked to share their experience, including their actual experiences (needs), and we adopted methods such as phenomenology17 to explore the deep knowledge and insight of the lived experience that the participants shared in the interviews.
Additionally, in order to ensure the accuracy and preciseness of the study, the research team held repeated discussions based on Meleis’ Theory of Transition and the definition of discharge readiness, and after a thorough literature analysis, identified the domains before drafting the preliminary interview guide. Data were processed and analyzed using Colaizzi’s descriptive phenomenological method, which consists of a seven-step analysis.18 We identified the corresponding thematic concepts from the interview data transcripts. Finally, we extracted five themes on the condition based on the experience and feeling (needs) of patients catheterized post-PTCD collected in these semi-structured interviews, which provided the reference for exploring the dimensions of the scale and constructing the item pool.
- Referring to existing RHDSs: The item pool of the scale was established by referring to the relevant aspects in questionnaires or scales such as the “Readiness for Hospital Discharge scale, RHDS”,13 “Readiness for Hospital Discharge Scale – New Mother Form (RHDS-NMF)”,14 “Readiness for Hospital Discharge Scale for Enterostomy”,14 and “Readiness for Hospital Discharge Scale for Stroke Patients”.16
- Evaluation by experts: The items to be validated were screened and supplemented by expert judges. Seventeen medical experts from the intervention department or hepatological surgery department were invited to participate in the Delphi expert consultation. They were asked to score the importance of the items in the scale by email. The total points were averaged, ensuring that the mean point was at least 4.0 and the variable coefficient was at least 0.25. The items were screened based on this; the consultation was completed after experts reached a consensus. At the same time, the response rate of questionnaires in two rounds of expert consultation was counted, based on which the expert consultation was achieved.19 The positivity was measured; the expert positivity coefficient was calculated, and the result was the proportion of valid questionnaires in the total; a number of more than 70% indicated that experts were highly positive.20 Formal questionnaire is shown in Supplementary Material 1.
The results showed that the positivity coefficients in two rounds of expert consultation were 100%, the overall expert authority coefficient was 0.892, and the coordination coefficients were 0.179 and 0.095 (Supplementary Material 2). The items of the scale were screened and modified using expert consultation. The initial scale of discharge readiness of patients after PTCD of bile duct carcinoma consisting of 32 items across 5 dimensions was developed and pre-tested.
Testing of Validity and Reliability of the Scale
Patients
We used convenience sampling to identify patients with bile duct carcinoma catheterized after PTCD. They were selected from four tertiary A-grade hospitals in Nantong City from August 2021 to August 2022. Inclusion criteria were as follows: (1) Patients with bile duct carcinoma catheterized after PTCD, diagnosis confirmed by pathology findings; (2) Age ≥ 18 years; (3) Patients with no psychiatric disorder and with normal comprehension, listening, and speaking capabilities; (4) Patients who gave their signed informed consent. Exclusion criteria were as follows: (1) Patients with congenital biliary tract disease; (2) Patients in severe condition or with unstable vital signs.
According to factor analysis, the ratio of scale items to sample size was required to be 1:5–10,21 and including invalid questionnaires, the sample size was determined to be 200. We, however, distributed a total of 300 questionnaires, and effectively recovered 286, with a response rate of 95.3%.
Tools
The questionnaire consisted of two parts: (1) General data: consisting of gender, age, education, catheterization duration, jaundice grade, and so on; (2) The self-developed initial “RHDS for Patients with Bile Duct Carcinoma Catheterized after PTCD” consisting of 32 items across five dimensions.
Methods
Survey Implementation and Quality Control
The researcher and trained nursing staff from four hospitals conducted a one-on-one survey with patients catheterized post-PTCD. The questionnaires were collected back immediately after patients completed them and were checked carefully to ensure no items were omitted or missed. Specifically, 1) Before the commencement of the questionnaire survey, the nurses who were involved were given full information about the survey and trained on how to guide participants to complete the questionnaires; 2) The questionnaires were collected back immediately after patients completed them and were checked for integrity of responses; 3) The questionnaires were double-checked throughout, from editing to data collection, to ensure accuracy; 4) After the questionnaires were collected, those where the respondents took too long a time (≥20 min) or too short a time (≤2 min) for filling it up were eliminated. (The study was approved by the ethics committee of the hospital before implementation)
Statistical Analysis
Item Analysis
We analyzed the heterogeneity and homogeneity of scale items as follows: 1) Critical ratio method: Scores of the scale were calculated, and the first 27% samples were selected as the high-score group and the last 27% samples as the low-score group according to the order of the scores. We used the independent sample t-test to determine their corresponding critical ratios, with the critical ratio < 3.0 as the deletion criteria; 2) Correlation coefficient method: We analyzed the correlation between the item and the scale score, with the correlation coefficient < 0.4 as the deletion criteria;22 3) Cronbach’s α coefficient method: If the total score had a relatively higher Cronbach’s α coefficient after an item was deleted, this suggested that the attribute of the item to be measured in the scale was different from that of other items, and was deleted;23 4) Factor analysis: This involved two indicators, namely “communality” and “factor load based on which we analyzed the relationship between the item and the scale; when the factor load value was <0.4 or common load occurred, the item was deleted.24
Validity Evaluation
1) Content validity: 10 medical experts from the intervention department or hepatological surgery department were invited to evaluate the content validity. We ensured balance in age, work experience, designation, education level, and other aspects when selecting them. The experts were asked to rate the importance of items using a 5-point rating scale, wherein 5 indicated “Very important” and 1 indicated “Very unimportant and we then calculated the content validity index (CVI) of the scale.25 2) Construct validity: We evaluated the construct validity of the scale using exploratory factor analysis.26,27 It included three aspects: a. The factor loading value of the item under the relevant dimension was >0.40; b. The loading value of the item under other dimensions was smaller, with a difference value > 0.25; c. Dimensions’ variance contribution rate > 50%.
Reliability Evaluation
The reliability of the scale was evaluated by calculating the Cronbach’s α coefficient and split-half reliability coefficient. The Cronbach’s α coefficient of the scale was >0.7, suggesting that the scale had good reliability.
Results
General Data
In this study, we distributed a total of 300 paper questionnaires, of which we recovered 287, including 286 valid questionnaires, with a valid response rate of 95.33%. In this survey, there were 161 patients over 61 years, accounting for 56.3% of the total sample. There were 155 patients with catheterization duration of 1–9 months, accounting for 54.2% of the total sample. General data of the respondents are shown in Table 1.
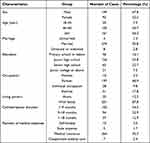 |
Table 1 General Data of Patients |
Item Analysis
Results of the study showed that there were significant differences in the critical ratios of items between the high-score group and low-score group (P < 0.05), except for item 13 and item 22. The critical ratios were between 4.24 and 13.57, suggesting that these items had a high degree of differentiation. No relevant items were deleted in the correlation analysis method, Cronbach’s α coefficient method and factor analysis method. Based on the above item analyses, we deleted two items.
Exploratory Factor Analysis
Results of the exploratory factor analysis on the RHDS for patients catheterized after PTCD (initial version) were that the Kaiser–Meyer–Olkin (KMO) value = 0.839, the Bartlett’s test of sphericity test chi-square value was 8619.492, and P < 0.001, suggesting that the data were suitable for factor analysis.28,29 Subsequently, we used principal component analysis (PCA) and varimax orthogonal rotation, combined with characteristic root, scree plot, and communality, and we obtained five dimensions with the characteristic root greater than 1 as the dimensions of the scale, with 30 items, with the cumulative variance contribution rate of 74.586%. Results are shown in Tables 2, 3, and Figure 1.
 |
Table 2 Explanatory Variance of Five Domains in Factor Analysis |
 |
Table 3 Rotated Component Matrix in Factor Analysis |
 |
Figure 1 Exploratory factor scree plot. |
Reliability Analysis
The Cronbach’s α coefficient of the scale was 0.820; Cronbach’s α coefficients of dimensions are physiological status was 0.958, psychological status was 0.777, role adaptation was 0.896, social support was 0.948, and self-efficacy was 0.960.
Validity Analysis
Validity is a criterion for judging the accuracy and effectiveness of a scale, which mainly consisted of content validity and construct validity.
Content Validity
The item-content validity indexes (I-CVI) were between 0.75 and 1.00, all of which were greater than 0.700; the scale-content validity index (S-CVI) was 0.875.
Construct Validity
RHDS for patients catheterized post-PTCD included five dimensions, with a cumulative variance contribution rate of 74.586%. We analyzed the relationship between the total score of the scale and the point of each dimension, and the correlation coefficient was between 0.404 and 0.597, suggesting that the scale had good construct validity. Details are shown in Table 4.
 |
Table 4 Correlation Coefficient Between the Total Score of the Scale and the Score of Each Dimension |
Discussion
Reliability of the Scale
Reliability indicates the accuracy of the scale and its stability. In general, when the Cronbach’s α coefficient is greater than 0.8, the scale has good internal consistency.28,29 In this study, we tested the reliability of internal consistency to determine the reliability of the scale. The results showed that the Cronbach’s α coefficient of the RHDS for patients catheterized post-PTCD was 0.820, and that for each dimension was in the range of 0.777–0.960, both of which were above the standard reliability value of 0.70, suggesting that the scale had good consistency and reliability. This also suggested that researchers avoided relevant influencing factors, and having been trained, they had mastered the skills and precautions to be taken during observation and conducting qualitative interviews.
Validity of the Scale
The validity of the scale refers to the correctness of scale measurement, and the higher the validity, the higher is the accuracy of scale measurement. In this study, we evaluated the construct validity of the scale using exploratory factor analysis. As one of the common methods for evaluating construct validity, exploratory factor analysis requires that the load of each item on its factor should be greater than 0.4 and that the cumulative variance contribution rate of the extracted common factor should be greater than 50%. Validity is the degree to which the scale can correctly measure the characteristics to be measured.25 Validity is target-oriented, and each scale has its own special purpose and function. A scale with high validity is applicable to its special group and has its special purpose. Validity is the most important consideration in measurement evaluation.
Content validity refers to the applicability and representation between the scale content and items, namely, whether the content of the scale can reflect the parameters to be measured among patients discharged with catheters after PTCD of bile duct carcinoma. We mainly generated the items of RHDS for patients with bile duct carcinoma catheterized after PTCD from qualitative interviews, which were used to explore the aspects that affected the discharge readiness of patients. Pre-testing proved that items were able to accurately reflect the psychological change and condition-related experiences of patients with bile duct carcinoma catheterized after PTCD. The Delphi expert consultation ensured that the scale items complied with the objective of the study.
In clinical verification, the I-CVI of the scale items was between 0.75 and 1.00 (which was higher than 0.700); the S-CVI was 0.875 (which was higher than 0.800). This suggested that the scale had good content validity. The results of factor analysis indicated that RHDS for patients catheterized post-PTCD included five dimensions (physiological status, psychological status, role adaptation, social support, and self-efficacy), with a cumulative variance contribution rate of 74.586%. We analyzed the relationship between the total scale score and the point of each dimension, and the correlation coefficient was between 0.404 and 0.597, suggesting that the scale had good construct validity, and the different dimensions were independent and also correlated.
Scientific and Practical Significance of Scale Development
In this study, the initial item pool was generated using methods such as qualitative interviews, relevant literature analysis, and by referring to existing RHDSs based on Meleis’ Theory of Transition. Items were screened using two rounds of Delphi expert consultation and pre-tested, thus forming the initial scale for the discharge readiness of patients with bile duct carcinoma catheterized after PTCD.
After item analysis and exploratory factor analysis, we developed the RHDS consisting of 30 items in 5 dimensions for patients with bile duct carcinoma catheterized after PTCD. This included dimensions such as physiological status, psychological status, role adaptation, social support, and self-efficacy involving the four factors of Meleis’ Theory, namely, the nature of transition, conditions of transition, response mode, and nursing therapeutics. All dimensions in the scale had been included in the theoretical dimension that was originally conceived. This indicates that the theoretical model of the initial scale is reasonable.
We consider possible catheter blockage, catheter falling off, catheter displacement, and catheter infection in patients with bile duct carcinoma catheterized after PTCD after discharge, as well as the main risk links in continuing nursing such as the self-monitoring of aggravation of the disease and the improvement of self-efficacy. Accordingly, we included these relevant aspects, which were reflected in items 21 and 28–34. These items were clear, relevant, and easy to understand and observe, and were helpful in identifying these risks in patients being prepared for discharge. All these suggested that the scale was developed scientifically and was specific in its clinical evaluation.
The significance of this study is that the developed scale can be used as an assessment tool to understand the readiness of patients for discharge and return home and find out the inadequacy of patients’ discharge readiness. Therefore, suggestions for improvement could be put forward to continuously improve the quality of discharge service. Thus, the occurrence of unplanned readmissions and complications caused by improper self-care could be reduced. At the same time, the scale could be used to identify factors affecting the discharge readiness of patients wearing catheters, which provided guidance for the formulation of personalized extended care plan and the improvement of clinical nursing quality. The generalizability of the developed scale to an international audience may warrant further research in the corresponding population.
Conclusion
In this study, the scale items were screened strictly and had good validity and reliability, thus providing a quantitative evaluation tool for clinical nursing staff to assess the discharge readiness of patients catheterized post-PTCD. Yet, the study had certain limitations, and further verification of the scale needs to be done in multi-center studies.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Nantong First People’s Hospital (No: 2020YKS048). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
No external funding was received to conduct this study.
Disclosure
The authors declare that they have no competing interests.
References
1. Ricci AD, Rizzo A, Brandi G. Immunotherapy in biliary tract cancer: worthy of a second look. Cancer Control. 2020;27(3):1073274820948047. doi:10.1177/1073274820948047
2. Rizzo A, Brandi G. First-line chemotherapy in advanced biliary tract cancer ten years after the ABC-02 trial: “And Yet It Moves!”. Cancer Treat Res Commun. 2021;27:100335. doi:10.1016/j.ctarc.2021.100335
3. Viscardi G, Tralongo AC, Massari F, et al. Comparative assessment of early mortality risk upon immune checkpoint inhibitors alone or in combination with other agents across solid malignancies: a systematic review and meta-analysis. Eur J Cancer. 2022;177:175–185. doi:10.1016/j.ejca.2022.09.031
4. Rizzo A, Ricci AD, Brandi G. Durvalumab: an investigational anti-PD-L1 antibody for the treatment of biliary tract cancer. Expert Opin Investig Drugs. 2021;30(4):343–350. doi:10.1080/13543784.2021.1897102
5. Li M, Wang J, Song J, et al. Preoperative ICG test to predict posthepatectomy liver failure and postoperative outcomes in hilar cholangiocarcinoma. Bio Med Res Int. 2021;2021(4):1–8.
6. Zhu B, Fu J, Zhu XY, et al. 恶性梗阻性黄疸患者 PTCD 术后胆道感染病原学与影响因素 [Etiology and influencing factors of biliary tract infection in patients with malignant obstructive jaundice after PTCD operation]. Zhong Hua Yi Yuan Gan Ran Xue Za Zhi. 2020;30(23):3644–3648. Chinese.
7. Yin SL. Effect of PTCD and ERCP on clinical efficacy and postoperative complications in patients with malignant obstructive jaundice. Zhong Guo Xian Dai Yao Wu Ying Yong. 2020;14(20):6l–63.
8. Sahinli H, Zet A. Prognostic and predictive factors in cancer patients with obstructive jaundice treated by percutaneous transhepatic biliary drainage: a single-center experience. J Cancer Res Ther. 2020;16(8):S99–S103. doi:10.4103/jcrt.JCRT_521_19
9. Meleis AI, Sawyer LM, Im E-O, Hilfinger Messias DK, Schumacher K. Experiencing transitions: an emerging middle-range theory. Adv Nurs Sci. 2000;23(1):12–28. doi:10.1097/00012272-200009000-00006
10. Wang BH. 冠心病患者出院准备度及其影响因素调查研究 [Investigation on discharge readiness of patients with coronary heart disease and its influencing factors]. Hua Zhong Ke Ji Da Xue. 2017. Chinese.
11. Galvin EC, Wills T, Coffey A. Readiness for hospital discharge: a concept analysis. J Adv Nurs. 2017;73(11):2547–2557. doi:10.1111/jan.13324
12. Seel RT, Macciocchi S, Velozo CA, et al. The Safety Assessment Measure for persons with traumatic brain injury: item pool development and content validity. Neurorehabilitation. 2016;39(3):1–17. doi:10.3233/NRE-161369
13. Weiss ME, Piacentine LB. Psychometric properties of the readiness for Hospital Discharge Scale. J Nurs Measure. 2006;14(3):163–180. doi:10.1891/jnm-v14i3a002
14. Chen X, Zhao TY, Liu L, et al. 产妇出院准备度量表的汉化及信效度研究 [Sinicization, reliability and validity of maternal discharge readiness scale]. Hu Li Yan Jiu. 2020;34(3):407–413. Chinese.
15. Yu QS, Lu LF, Wang SY, et al. 肠造口患者出院准备度量表的编制及信效度检验 [Preparation of discharge readiness scale for enterostomy patients and test of reliability and validity]. Zhong Guo Shi Yong Hu Li Za Zhi. 2020;36(13):998–1002. Chinese.
16. Liu CX, Zhang WG, Li Y, et al. 脑卒中病人出院准备度评估量表的编制 [Preparation of discharge readiness Assessment scale for stroke patients]. Hu Li Yan Jiu. 2020;34(15):2671–2675. Chinese.
17. Crist JD, Tanner CA. Interpretation/analysis methods in hermeneutic interpretive phenomenology. Nurs Res. 2003;52(3):202. doi:10.1097/00006199-200305000-00011
18. Edward KL, Welch T. The extension of Colaizzi’s method of phenomenological enquiry. Contemp Nurse. 2011;39(2):163–171. doi:10.5172/conu.2011.163
19. Jorm AF. Using the Delphi expert consensus method in mental health research. Austr N Z J Psychiatry. 2015;49(10):887–897. doi:10.1177/0004867415600891
20. Luo H, Wang Q, Lim C, et al. Selection of Tibetan body mass index based on Delphi method. Chin J Integr Trad Western Med. 2019;39(4):441–445.
21. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. doi:10.1186/1471-2288-14-135
22. Zhang JP, Liu Y, Zhao MY, et al. 大学生阈下抑郁量表的编制及其信效度检验 [Development of subthreshold depression scale for college students and its reliability and validity test]. Xian Dai Yu Fang Yi Xue. 2019;46(23):84–86. Chinese.
23. Yue SP, Li HY, Wang Y, et al. 老年失智失能量表的编制:统计学方法在条目筛选中的运用 [Development of the senile Dementia and Disability Scale: application of statistical methods to item screening]. Zhong Guo Lao Nian Xue Za Zhi. 2020;9(40):4009–4011. Chinese.
24. Wang HP, Xiang LC, Zhang W, et al. 客观结构化临床考试信度的 Meta 分析 [A meta-analysis of the reliability of objective structured clinical tests]. Zhong Guo Xun Zheng Yi Xue Za Zhi. 2014;7:878–883. Chinese.
25. Thomas CE, Abbott G, Gastin PB, et al. Construct validity and reliability of the Talent Development Environment Questionnaire in Caribbean youth track and field athletes. PLoS One. 2020;15(1):e0227815. doi:10.1371/journal.pone.0227815
26. Chen H, Du KY, Jia GZ. 因子分析在家庭负担量表结构效度检验中的应用 [Application of factor analysis to the validity test of family Burden Scale structure]. Zhong Guo Wei Sheng Tong Ji. 2003;20(2):93–94. Chinese.
27. Li C, Xin L. 调查问卷的信度与效度的评价方法研究 [Research on evaluation method of reliability and validity of questionnaire]. Zhong Guo Wei Sheng Tong Ji. 2008;5:541–544. Chinese.
28. Shinjo M, Inoue M, Akamine I, et al. Development of an early detection scale for intimate partner violence to occur in relationships under power and control. Japan J Nurs Sci. 2021;18(1):e12369. doi:10.1111/jjns.12369
29. Adamson KA, Prion S. Reliability: measuring internal consistency using Cronbach’s α. Clin Simulat Nurs. 2013;9(5):e179–e181. doi:10.1016/j.ecns.2012.12.001
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
