Back to Journals » Infection and Drug Resistance » Volume 16
Development and Validation of a Nomogram to Predict Significant Liver Inflammation in Patients with Chronic Hepatitis B
Authors Jiang S, Wang J, Zhang Z, Zhan J, Xue R, Qiu Y, Zhu L, Zhang S, Pan Y, Yan X, Chen Y, Li J, Liu X, Zhu C, Huang R, Wu C
Received 30 April 2023
Accepted for publication 26 July 2023
Published 7 August 2023 Volume 2023:16 Pages 5065—5075
DOI https://doi.org/10.2147/IDR.S417007
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Suling Jiang,1,* Jian Wang,2,3,* Zhiyi Zhang,4,* Jie Zhan,1 Ruifei Xue,1 Yuanwang Qiu,5 Li Zhu,6 Shaoqiu Zhang,2 Yifan Pan,1 Xiaomin Yan,2 Yuxin Chen,3,7 Jie Li,1– 4 Xingxiang Liu,8 Chuanwu Zhu,6 Rui Huang,1– 4 Chao Wu1– 4
1Department of Infectious Diseases, Nanjing Drum Tower Hospital Clinical College of Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China; 2Department of Infectious Diseases, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, Jiangsu, People’s Republic of China; 3Institute of Viruses and Infectious Diseases, Nanjing University, Nanjing, Jiangsu, People’s Republic of China; 4Department of Infectious Diseases, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Nanjing, Jiangsu, People’s Republic of China; 5Department of Infectious Diseases, The Fifth People’s Hospital of Wuxi, Wuxi, Jiangsu, People’s Republic of China; 6Department of Infectious Diseases, The Affiliated Infectious Diseases Hospital of Soochow University, Suzhou, Jiangsu, People’s Republic of China; 7Department of Laboratory Medicine, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, Jiangsu, People’s Republic of China; 8Department of Clinical Laboratory, Huai’an No. 4 People’s Hospital, Huai’an, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chao Wu, Department of Infectious Diseases, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, No. 321 Zhongshan Road, Nanjing, Jiangsu, 210008, People’s Republic of China, Tel +86-25-83105890, Fax +86-25-83307115, Email [email protected] Rui Huang, Department of Infectious Diseases, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, No. 321 Zhongshan Road, Nanjing, Jiangsu, 210008, People’s Republic of China, Email [email protected]
Background: Noninvasive diagnosis of liver inflammation is important for patients with chronic hepatitis B (CHB). This study aimed to develop a nomogram to predict significant liver inflammation for CHB patients.
Methods: CHB patients who underwent liver biopsy were retrospectively collected and randomly divided into a development set and a validation set. The least absolute shrinkage and selection operator regression and logistic regression analysis were used to select independent predictors of significant liver inflammation, and a nomogram was developed. The performance of nomogram was assessed by receiver operating characteristic (ROC) curves, calibration curves and decision curve analysis (DCA).
Results: A total of 1019 CHB patients with a median age of 39.0 years were included. Alanine aminotransaminase (ALT, P = 0.018), gamma-glutamyl transpeptidase (P = 0.013), prothrombin time (P < 0.001), and HBV DNA level (P = 0.030) were identified as independent predictors of significant liver inflammation in the development set. A model namely AGPD-nomogram was developed based on the above parameters. The area under the ROC curve in predicting significant inflammation was 0.765 (95% CI: 0.727– 0.803) and 0.766 (95% CI: 0.711– 0.821) in the development and validation sets, which were significantly higher than other indexes. The AGPD-nomogram had a high predictive value in patients with normal ALT. Moreover, the nomogram was proven to be clinically useful by DCA.
Conclusion: A visualized AGPD-nomogram which incorporated routine clinical parameters was proposed to facilitate the prediction of significant liver inflammation in CHB patients. This nomogram had high accuracy in the identification of significant liver inflammation and would be a useful tool for the better management of CHB patients, especially for those with normal ALT.
Keywords: chronic hepatitis B, liver inflammation, prediction, nomogram, alanine aminotransferase
Introduction
Chronic hepatitis B virus (HBV) infection is a global public health challenge, which is one of the leading causes of cirrhosis and hepatocellular carcinoma (HCC). Approximately 250 million people are currently being infected with HBV despite the use of vaccines and nucleosides or nucleoside analogues for several years.1,2 More than 800,000 people worldwide die from liver diseases caused by HBV infection annually, of which cirrhosis and HCC account for 52% and 38%, respectively.3 In patients with chronic hepatitis B (CHB), HBV persists with dynamic variations in hepatocellular injury with inflammation activity.4 Antiviral treatment can alleviate hepatic inflammation and reduce the development of cirrhosis and HCC.2,5,6
The identification of liver inflammation grade is conducive to risk prediction and therapeutic decisions, especially for those with normal alanine aminotransaminase (ALT). According to the international CHB guidelines, CHB patients with moderate-to-severe inflammation and/or fibrosis are recommended to receive antiviral treatment.2,6 Liver biopsy (LB) is the most direct and accurate evaluation tool for liver histological inflammation and fibrosis. However, it is invasive with adverse risks, and not available in resource-limited settings. Furthermore, only a small section can lead to sampling errors.7,8 Several non-invasive measures for assessing liver fibrosis were developed as alternatives to LB, including aspartate aminotransaminase (AST) to platelet ratio (APRI), fibrosis-4 score (FIB-4) and gamma-glutamyl transpeptidase (GGT) to platelet ratio (GPR), which have been validated with relatively high accuracy in distinguishing liver fibrosis.9–11 However, few non-invasive indicators are available to reflect liver inflammation in CHB patients.
Clinically, serum biomarkers including ALT and AST are commonly used to assess liver inflammation activity in patients with CHB.2,6 Serum ALT level has always been regarded to be closely associated with liver injury, whereas numerous studies have reported that ALT failed to be consistent with the severity of liver damage.12–14 Increasing evidence suggested that CHB patients with normal ALT levels may exist significant liver injury which is an indication for antiviral therapy.15–17 Actitest is a non-invasive diagnostic tool for the liver inflammation activity in patients with chronic viral hepatitis with a satisfactory accuracy.18,19 However, this score contains six indicators (ALT, bilirubin, GGT, alpha-2-macroglobulin, haptoglobin, apolipoprotein-A1), and some indicators are not commonly used in clinical practice, which limit its clinical application.18–20 In addition, other non-invasive predictors such as golgi protein 73, hepatitis B core antibody, and red blood cell distribution width were reported to be associated with liver inflammation activity in patients with chronic liver diseases.21–23 However, the predictive values of these indicators need to be validated in CHB patients.
Given the lack of a safe and convenient approach, exploring a non-invasive predictive model reflecting liver inflammation activity will greatly facilitate the clinical management of CHB, especially for patients with normal ALT. Therefore, in the present study, we established a novel predictive model for significant liver inflammation in CHB patients.
Methods
Patients
A total of 1019 consecutive CHB patients who underwent liver biopsy were retrospectively included between April 2004 and October 2020 at four hospitals in Jiangsu, China. Chronic HBV infection is defined as positive for serum HBV surface antigen (HBsAg) over 6 months. The exclusion criteria were as follows: concurrent with any cause of liver diseases (including other viral hepatitis, non-alcoholic fatty liver disease, alcoholic liver diseases, autoimmune liver disease, decompensated cirrhosis, HCC, syphilis and human immunodeficiency virus), or insufficient clinical data.
Clinical and Laboratory Data Collection
We reviewed the medical records of all patients. The demographic information such as age and gender and laboratory data such as platelet (PLT), total bilirubin (TB), albumin (ALB), globulin (GLB), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP) and gamma-glutamyl transpeptidase (GGT) were collected. The results of laboratory tests within two weeks of liver biopsy were recorded.
Liver Biopsy
Liver pathology in patients with chronic HBV infection was conducted to determine the degrees of inflammation and fibrosis. An ultrasound-guided liver biopsy was performed on each patient. Liver tissues were obtained using 16-G biopsy needle and treated with formalin and embedded in paraffin. Liver inflammation was graded by experienced pathologists using the Scheuer scoring system as follows: G0 (no inflammation); G1 (inflammatory but no liver damage); G2 (focal necrosis or acidophil bodies); G3 (severe focal cell damage); and G4 (fusion necrosis). G ≥ 2 and G ≥ 3 were defined as significant inflammation and advanced inflammation, respectively.6
Statistical Analysis
Continuous variables were presented as the median and interquartile range (IQR). Categorical variables were shown as frequencies and percentages. Patients were randomly divided into a development set and a validation set with a ratio of 7:3 by a computer-generated randomization schedule. The Wilcoxon-Mann–Whitney test, Student’s t-test or Chi-square test were used to examine differences between groups. The predictors of significant liver inflammation were selected using the least absolute shrinkage and selection operator (LASSO) regression. Subsequently, the selected variables were incorporated into a multivariate logistic regression model. Finally, the model was presented as a nomogram, built on the likelihood of significant inflammation. Decision curve analysis (DCA), calibration curve, and receiver operating characteristic (ROC) curve were used to validate the nomogram’s accuracy and value. Statistics were considered significant at a two-sided P < 0.05. The data analysis was performed using R software (version 4.2.0, http://www.r-project.org/).
Results
Patient Characteristics
A total of 1019 patients were included in the final analysis and were randomly divided into two sets: a development set containing 713 patients and a validation set containing 306 patients. The clinical characteristics of development and validation sets are summarized in Table 1. The median age of patients was 39.0 (IQR: 32.0, 47.0) years old and 665 (65.3%) patients were male. The median levels of ALT, GGT and HBV DNA were 40.0 (IQR: 25.0, 79.0) U/L, 27.0 (IQR: 17.0, 60.0) U/L and 4.98 (IQR: 3.08, 7.00) log10 IU/mL, respectively. There were no significant differences in age, gender ratio or serological parameters between the two sets except for serum AST, ALT and grades of hepatitis activity. The AST and ALT levels were higher in the development set. The distribution of inflammation grades was as follows: 209 (29.3%) patients with non-significant inflammation (G0-1) and 504 (70.7%) patients with significant inflammation (G2-4) in the development set; 117 (38.2%) patients with non-significant inflammation (G0-1) and 189 (61.8%) patients with significant inflammation (G2-4) in the validation set.
 |
Table 1 Clinical Features of Patients in the Development Set and Validation Set |
Comparison of Clinical Features of Patients with and without Significant Liver Inflammation in the Development Set
The median age (39.0 years vs 40.0 years, P = 0.276), red blood cell distribution width (RDW) (12.4% vs 12.3%, P = 0.214), and albumin (ALB) (43.4 g/L vs 43.7 g/L, P = 0.378) were comparable between patients with and without significant inflammation. The proportions of male (68.3% vs 60.3%, P = 0.041) and HBeAg positivity (52.2% vs 30.1%, P < 0.001) were higher in patients with significant inflammation than those of patients without significant inflammation. Patients with significant inflammation had higher median levels of total bilirubin (TB, 16.1 μmol/L vs 13.2 μmol/L, P < 0.001), globulin (GLB, 28.3 g/L vs 27.3 g/L, P < 0.001), ALT (53.5 U/L vs 27.7 U/L, P < 0.001), AST (39.0 U/L vs 25.0 U/L, P < 0.001), alkaline phosphatase (ALP, 76.0 U/L vs 67.0 U/L, P < 0.001), GGT (37.5 U/L vs 19.0 U/L, P < 0.001), prothrombin time (PT, 13.6 s vs 12.8 s, P < 0.001), international normalized ratio (INR, 1.08 vs 1.00, P < 0.001) and HBV DNA level (5.44 log10 IU/mL vs 3.51 log10 IU/mL, P < 0.001), while lower levels of platelets (PLT, 161.0 ×109/L vs 192.0 ×109/L, P < 0.001) compared to patients with non-significant liver inflammation (Table 2).
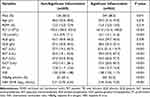 |
Table 2 Comparison of Clinical Features Between Patients with and without Significant Liver Inflammation in the Development Set |
Development of a Nomogram for Predicting Significant Inflammation
In the development set, the LASSO regression was performed to determine the most significant predictors and 10 variables were selected with an optimal lambda (Figure 1). These parameters were included in multivariate regression analysis to estimate the odds ratio (OR) and 95% confidence interval (CI), ultimately including four variables in the model: ALT (OR = 1.000, 95% CI 1.001–1.009, P = 0.018), GGT (OR = 1.010, 95% CI 1.001–1.013, P = 0.013), PT (OR = 1.380, 95% CI 1.192–1.588, P<0.001), and HBV DNA levels (OR = 1.170, 95% CI 1.015–1.352, P = 0.030) (Table S1). These independently associated risk factors were included to build a simple-to-use risk estimation nomogram, namely AGPD-nomogram, which is freely available online at https://ndth-zzy.shinyapps.io/AGPD-nomogram/ (Figure 2). We can calculate the total points on a vertical line from each variable to the point axis and obtain the diagnostic probability of significant inflammation in CHB patients.
Comparison of Predictive Accuracy Between the AGPD-Nomogram and Other Parameters
We compared the performance of AGPD-nomogram and other parameters in predicting significant inflammation (Figure 3, Table 3). The AUROCs of AGPD-nomogram were 0.765 (95% CI: 0.727–0.803) and 0.766 (95% CI: 0.711–0.821) in development and validation sets, with optimal cut-off values of 18.813 and 21.134, respectively. In the development set, the AGPD-nomogram showed higher AUROC than ALT (0.725, 95% CI: 0.685–0.764, P = 0.021), GGT (0.722, 95% CI: 0.682–0.761, P = 0.026), PT (0.684, 95% CI: 0.641–0.727, P < 0.001) and HBV DNA (0.630, 95% CI: 0.582–0.677, P < 0.001). Similarly, in the validation set, the AGPD-nomogram also had higher AUROC than ALT (0.690, 95% CI: 0.630–0.750, P = 0.008), GGT (0.707, 95% CI: 0.649–0.765, P = 0.031), PT (0.678, 95% CI: 0.615–0.740, P < 0.001) and HBV DNA (0.627, 95% CI: 0.560–0.694, P < 0.001). In both sets, ALT and GGT were comparably superior to either PT or DNA load in detecting significant inflammation (Figure 3A and B). As shown in Figure 3C and D, the AGPD-nomogram was calibrated by the Hosmer–Lemeshow test and the calibration plot, using a 500-bootstrap analysis, which yielded a nonsignificant statistic and indicated that sound agreement between the nomogram predicted and actual probability of significant inflammation in both development set (P = 0.389) and validation set (P = 0.454).
 |
Table 3 Diagnostic Accuracy of Different Indicators for the Prediction of Significant Inflammation in the Development Set and Validation Set |
Moreover, the decision curve analysis indicated the feasibility of the nomogram for generating valuable predictions and displayed a higher net benefit compared to the other four indexes. When the threshold probability exceeds 28% in the DCA analysis, the use of AGPD-nomogram to predict significant liver inflammation confers greater benefits than the “treat all” and the “treat none” schemes (Figure 3E and F).
The Correlations Between Nomogram and Liver Inflammation Grades
The correlations between AGPD-nomogram scores and liver inflammation grades were analyzed by Spearman’s rank correlation coefficient analysis. Correlation analysis suggested that there was a significantly positive association between the AGPD-nomogram scores and liver inflammation grades in CHB patients both in the development set (r = 0.55, P < 0.001) and the validation set (r = 0.55, P < 0.001). The AGPD-nomogram scores increased with the aggravation of liver inflammation (Figure S1A and S1B). Patients with significant liver inflammation exhibited notably higher AGPD-nomogram scores than those without significant liver inflammation in both development set and validation set (Both P < 0.001) (Figure S1C and S1D).
AGPD-Nomogram and ALT for Estimating Significant Liver Inflammation in Patients with Normal ALT
We explored the performance of AGPD-nomogram for estimating significant liver inflammation in patients within the upper limit of normal (ULN) of ALT suggested by the American Association for the Study of Liver Diseases (AASLD) recommendation (35 U/L in males and 25 U/L in females), East Asia expert opinion (30 U/L in males and 19 U/L in females), and the European Association for the Study of the Liver (EASL) recommendation (40 U/L).2,6,24 322 patients (45.2%) and 171 patients (55.9%) had normal ALT levels (<40 U/L) in the development set and validation set, respectively. Using the ULN of ALT was 40 U/L, the proportions of significant liver inflammation were 55.9% and 49.7% in the development set and validation set, respectively. In the development set, the AGPD-nomogram had an AUC of 0.703 (95% CI: 0.622–0.783) for predicting significant liver inflammation. The optimal cut-off value was 17.622, with a sensitivity of 81.8% and a specificity of 53.2%. Notably, the predictive accuracy was better than that of serum ALT (AUC: 0.608, 95% CI: 0.521–0.695, P = 0.039). Similarly, the AGPD-nomogram showed higher predictive performance with an AUC of 0.803 (95% CI: 0.707–0.898) compared to serum ALT (AUC: 0.546, 95% CI: 0.434–0.659, P < 0.001) in the validation set. In addition, using ALT ULN of 35/25 U/L (male/female), the model showed a slightly higher AUC (0.692 vs 0.597, P = 0.084) with ALT in the development set while higher AUC than ALT (0.827 vs 0.597, P = 0.005) in the validation set. With regard to ALT ULN of 30/19 U/L (male/female), the nomogram had comparable AUC compared to ALT in the development set (0.643 vs 0.610, P = 0.620) and validation set (0.803 vs 0.633, P = 0.129) (Figure S2, Table S2).
Discussion
In this study, we developed and validated a non-invasive, clinical–based nomogram for the prediction of liver inflammation in CHB patients. Incorporating the clinical risk factors into an easy-to-use nomogram facilitates the individualized prediction of the severity of liver inflammation.
Accurate evaluation of liver inflammation grade is of great clinical importance for making therapeutic decisions in CHB patients, especially for patients with normal ALT. Although serum ALT is commonly used as a noninvasive indicator of liver injury, the correlation of ALT with liver inflammation grade is not satisfactory in CHB patients.25 In our study, 55.9% and 49.7% of patients with normal ALT in the development set and validation set had significant liver inflammation. Previous studies also found a high proportion of significant liver inflammation in CHB patients with normal ALT.23,26,27 Chen et al developed a non-invasive model for predicting liver inflammation in patients with CHB. However, this is a single-center study and the model only showed a moderate accuracy.28 Similar AAGP model was reported by Li et al, which contained age, ALT, GGT, and PLT to predict liver inflammation activity in patients with CHB, while the small sample size and single-center design limit the clinical application for this model.29
In the present study, LASSO regression analysis was used to screen variables, which can effectively reduce the data dimension in high-dimensional data analysis and ensure the simplicity and stability of the model. We developed a complex logistic regression formula in the form of an intuitive and simple nomogram. This AGPD-nomogram showed a better performance and a larger net benefit in screening patients with significant inflammation than ALT, GGT, PT, and HBV DNA separately, which was also verified in the validation set. Moreover, the AGPD-nomogram scores were positively correlated with liver inflammation grades in both the development set and validation set.
The AGPD-nomogram contains four independent risk factors for significant hepatic inflammation: ALT, PT, GGT and HBV DNA levels. Serum ALT level is the most commonly used indicator of liver inflammation activity.30 Previous reports showed the value of GGT as a marker of liver injury. Elevated GGT levels can be caused by most liver diseases.31,32 PT has been reported as an independent predictor of significant inflammation in CHB patients in previous studies.28 The prolonged PT may be associated to the reduction of coagulation factors as well as the fibrinogen synthesis, reflecting the synthetic capacity of the hepatocytes during liver damage.33,34 HBV DNA is the marker for viral replication, and its level is directly proportional to the progression to cirrhosis.35 Serum HBV DNA levels are also associated with liver inflammation.36 Our previous study demonstrated that patients with CHB with moderate serum HBV DNA levels had a high risk of significant inflammation.36 The AGPD-nomogram including the above-mentioned parameters had significantly higher predictive values of significant liver inflammation than the above parameters alone in patients with CHB, especially for patients with normal ALT. Nomogram is an intuitive graphical presentation of complex statistical model, which can help physician evaluates the likelihood of a clinical event and formulate individualized strategy of diagnosis and treatment.37 In this study, we examined common clinical indicators by LASSO regression analysis and constructed the AGPD-nomogram, which presented high discrimination and well-fitted calibration. Importantly, development set and validation set showed consistent performance and higher accuracy than ALT, GGT, PT, and HBV DNA.
Limitations
We acknowledge that there are several limitations. First, it is a retrospective study which might lead to selection bias. Second, this nomogram was verified internally, and external validation is needed. Third, the predictive value of AGPD-nomogram for disease progression and long-term outcomes of CHB patients remains not yet clear due to the lack of follow-up data.
Conclusion
We established a nomogram-based model for CHB patients which was validated with promising performance in the identification of significant liver inflammation. This nomogram would be a useful tool for better management of CHB patients, especially for those with normal ALT. However, further prospective studies are needed to validate the diagnostic value of the AGPD-nomogram.
Abbreviations
HBV, hepatitis B virus; CHB, chronic hepatitis B; HCC, hepatocellular carcinoma; LB, liver biopsy; HBeAg, hepatitis B e antigen; RDW, red blood cell distribution width; PLT, platelet; TB, total bilirubin; ALB, albumin; GLB, globulin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; GGT, gamma-glutamyl transpeptidase; PT, prothrombin time; INR, International normalized ratio; IQR, interquartile range; OR, odds ratio; ROC, receiver operating characteristic; DCA, decision curve analysis.
Data Sharing Statement
The data that support the study findings are available upon reasonable request from the corresponding authors ([email protected] or [email protected]).
Ethical Considerations
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and was approved by the Institutional Review Board at Nanjing Drum Tower Hospital (IRB number: 2008022). A waiver of informed consent was granted because all data were retrospectively collected, and all clinical and laboratory data were used anonymously.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, took part in drafting, revising or critically reviewing the article, gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from Nanjing Medical Science and Technique Development Foundation (JQX21002, YKK21067 and QRX17121), Natural Science Foundation of Jiangsu Province (BK20211004), and Clinical Trials from the Affiliated Drum Tower Hospital, Medical School of Nanjing University (2022-LCYJ-MS-07 and 2021-LCYJ-PY-43).
Disclosure
All authors declare that they have no competing interests in this study.
References
1. Nguyen MH, Wong G, Gane E, et al. Hepatitis B virus: advances in prevention, diagnosis, and therapy. Clin Microbiol Rev. 2020;33(2):e00046–19.
2. Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Clin Liver Dis. 2018;12(1):33–34. doi:10.1002/cld.728
3. Brody H. Hepatitis B. Nature. 2022;603(7903):S45. doi:10.1038/d41586-022-00811-2
4. Bengsch B, Chang KM. Evolution in our understanding of hepatitis b virus virology and immunology. Clin Liver Dis. 2016;20(4):629–644. doi:10.1016/j.cld.2016.06.001
5. Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10(1):1–98. doi:10.1007/s12072-015-9675-4
6. Lampertico P, Agarwal K, Berg T; European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67(2):370–398. doi:10.1016/j.jhep.2017.03.021
7. Kramvis A, Chang KM, Dandri M, et al. A roadmap for serum biomarkers for hepatitis B virus: current status and future outlook. Nat Rev Gastroenterol Hepatol. 2022;19(11):727–745. doi:10.1038/s41575-022-00649-z
8. Rockey DC, Caldwell SH, Goodman ZD, et al. Liver biopsy. Hepatology. 2009;49(3):1017–1044. doi:10.1002/hep.22742
9. Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518–526. doi:10.1053/jhep.2003.50346
10. Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology. 2007;46(1):32–36. doi:10.1002/hep.21669
11. Lemoine M, Shimakawa Y, Nayagam S, et al. The gamma-glutamyl transpeptidase to platelet ratio (GPR) predicts significant liver fibrosis and cirrhosis in patients with chronic HBV infection in West Africa. Gut. 2016;65(8):1369–1376. doi:10.1136/gutjnl-2015-309260
12. Seto WK, Lai CL, Ip PP, et al. A large population histology study showing the lack of association between ALT elevation and significant fibrosis in chronic hepatitis B. PLoS One. 2012;7(2):e32622. doi:10.1371/journal.pone.0032622
13. Chao DT, Lim JK, Ayoub WS, et al. Systematic review with meta-analysis: the proportion of chronic hepatitis B patients with normal alanine transaminase ≤ 40 IU/L and significant hepatic fibrosis. Aliment Pharmacol Ther. 2014;39(4):349–358. doi:10.1111/apt.12590
14. Wang J, Xia J, Yan X, et al. The gamma-glutamyl transpeptidase to platelet ratio predicts liver inflammation in chronic hepatitis B with normal or mildly elevated alanine transaminase. Clin Res Hepatol Gastroenterol. 2020;44(6):913–922. doi:10.1016/j.clinre.2020.01.011
15. Teng J, Du Y, Visalath P, et al. A noninvasive model discriminating significant histological changes in treatment-naive chronic hepatitis B patients with normal ALT. Virol J. 2023;20(1):7. doi:10.1186/s12985-023-01963-x
16. Zhao XA, Wang J, Wei J, et al. Gamma-glutamyl transpeptidase to platelet ratio predicts liver injury in hepatitis B e antigen-negative chronic hepatitis b patients with normal alanine aminotransferase. J Clin Transl Hepatol. 2022;10(2):247–253. doi:10.14218/JCTH.2021.00151
17. Duan M, Chi X, Xiao H, et al. High-normal alanine aminotransferase is an indicator for liver histopathology in HBeAg-negative chronic hepatitis B. Hepatol Int. 2021;15(2):318–327. doi:10.1007/s12072-021-10153-2
18. Pokorska-śpiewak M, Kowalik-Mikołajewska B, Aniszewska M, et al. Non-invasive evaluation of the liver disease severity in children with chronic viral hepatitis using FibroTest and ActiTest - comparison with histopathological assessment. Clin Exp Hepatol. 2017;3(4):187–193. doi:10.5114/ceh.2017.71079
19. Yakoob R, Bozom IA, Thandassery RB, et al. Noninvasive biomarkers FibroTest and ActiTest versus liver biopsy in chronic hepatitis C patients: the middle east experience. Ann Gastroenterol. 2015;28(2):265–270.
20. Uyar C, Akcam FZ, Ciris M, et al. Comparison of FibroTest-ActiTest with histopathology in demonstrating fibrosis and necroinflammatory activity in chronic hepatitis B and C. Indian J Pathol Microbiol. 2010;53(3):470–475. doi:10.4103/0377-4929.68281
21. Yao M, Wang L, Wang J, et al. Diagnostic value of serum golgi protein 73 for liver inflammation in patients with autoimmune hepatitis and primary biliary cholangitis. Dis Markers. 2022;2022:4253566. doi:10.1155/2022/4253566
22. Xu WS, Qiu XM, Ou QS, et al. Red blood cell distribution width levels correlate with liver fibrosis and inflammation: a noninvasive serum marker panel to predict the severity of fibrosis and inflammation in patients with hepatitis B. Medicine. 2015;94(10):e612. doi:10.1097/MD.0000000000000612
23. Yao K, Wang J, Wang L, et al. Association of anti-HBc and liver inflammation in HBeAg-negative chronic hepatitis B virus-infected patients with normal ALT and detectable HBV DNA. J Med Virol. 2022;94(2):659–666. doi:10.1002/jmv.27327
24. Kao JH, Hu TH, Jia J, et al. East Asia expert opinion on treatment initiation for chronic hepatitis B. Aliment Pharmacol Ther. 2020;52:1540–1550.
25. Chang X, Wang J, Chen Y, et al. A novel nomogram to predict evident histological liver injury in patients with HBeAg-positive chronic hepatitis B virus infection. EBioMedicine. 2021;67:103389. doi:10.1016/j.ebiom.2021.103389
26. Zhou J, Wang FD, Wang ML, et al. Antiviral therapy for chronic HBV infection with persistently normal alanine aminotransferase: controversy and consensus. Front Med. 2021;8:717125. doi:10.3389/fmed.2021.717125
27. Zhang L, Yang L, Gao Y, et al. Nomogram for evaluating obvious liver inflammation in treatment-naïve HBeAg positive chronic hepatitis B virus infection patients with normal ALT. Virulence. 2023;14(1):2158710. doi:10.1080/21505594.2022.2158710
28. Chen S, Huang H. Clinical non-invasive model to predict liver inflammation in chronic hepatitis B with alanine aminotransferase ≤ 2 upper limit of normal. Front Med. 2021;8:661725. doi:10.3389/fmed.2021.661725
29. Li Q, Zhou Y, Huang C, et al. A novel diagnostic algorithm to predict significant liver inflammation in chronic hepatitis B virus infection patients with detectable HBV DNA and persistently normal alanine transaminase. Sci Rep. 2018;8(1):15449. doi:10.1038/s41598-018-33412-z
30. Gui HL, Wang H, Yang YH, et al. Significant histopathology in Chinese chronic hepatitis B patients with persistently high-normal alanine aminotransferase. J Viral Hepat. 2010;17 Suppl 1:44–50. doi:10.1111/j.1365-2893.2010.01270.x
31. Myers RP, Ratziu V, Imbert-Bismut F, et al. Biochemical markers of liver fibrosis: a comparison with historical features in patients with chronic hepatitis C. Am J Gastroenterol. 2002;97(9):2419–2425. doi:10.1111/j.1572-0241.2002.05997.x
32. Eminler AT, Irak K, Ayyildiz T, et al. The relation between liver histopathology and GGT levels in viral hepatitis: more important in hepatitis B. Turk J Gastroenterol. 2014;25(4):411–415. doi:10.5152/tjg.2014.3693
33. Kim SU, Han KH, Park JY, et al. Liver stiffness measurement using FibroScan is influenced by serum total bilirubin in acute hepatitis. Liver Int. 2009;29(6):810–815. doi:10.1111/j.1478-3231.2008.01894.x
34. Wang CY, Deng Y, Li P, et al. Prediction of biochemical nonresolution in patients with chronic drug-induced liver injury: a large multicenter study. Hepatology. 2022;75(6):1373–1385. doi:10.1002/hep.32283
35. Yuen MF, Chen DS, Dusheiko GM, et al. Hepatitis B virus infection. Nat Rev Dis Primers. 2018;4:18036. doi:10.1038/nrdp.2018.36
36. Liu J, Wang J, Yan X, et al. Presence of liver inflammation in Asian patients with chronic hepatitis B with normal ALT and detectable HBV DNA in absence of liver fibrosis. Hepatol Commun. 2022;6(4):855–866. doi:10.1002/hep4.1859
37. Kattan MW, Scardino PT. Evidence for the usefulness of nomograms. Nat Clin Pract Urol. 2007;4(12):638–639. doi:10.1038/ncpuro0968
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



