Back to Journals » Infection and Drug Resistance » Volume 16
Development and Validation of a Nomogram for Predicting Tigecycline-Related Coagulopathy: A Retrospective Cohort Study
Authors Li Z , Zeng Q, Xu S , Li Y, Tang T , Shi J, Song X , He W , Chen L , Liu G , Gao B , Zheng J, Huang L , Chen M, Jiang S
Received 23 September 2022
Accepted for publication 16 January 2023
Published 24 January 2023 Volume 2023:16 Pages 423—434
DOI https://doi.org/10.2147/IDR.S388438
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Zhaolin Li,1,* Qiaojun Zeng,1,* Shuwan Xu,2,* Yuewei Li,1 Tiantian Tang,1 Jianting Shi,1 Xueming Song,1 Wenman He,1 Liang Chen,1 Guirong Liu,1 Boying Gao,3 Jianming Zheng,4 Linjie Huang,1 Ming Chen,1 Shanping Jiang1
1Department of Pulmonary and Critical Care Medicine, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, People’s Republic of China; 2Department of Cardiology, the Eighth Affiliated Hospital, Sun Yat-sen University, Shenzhen, People’s Republic of China; 3Breast Tumor Center, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, People’s Republic of China; 4Cardiovascular Medicine Department, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shanping Jiang; Ming Chen, Department of Pulmonary and Critical Care Medicine, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Yan-jiang Xi Road 107, Guangzhou, 510120, People’s Republic of China, Tel +86-20-81332441, Email [email protected]; [email protected]
Background: Although tigecycline is an effective drug against drug-resistant bacteria, it demonstrated a higher all-cause mortality than comparator antibiotics and a high incidence of coagulation disorders which can be accompanied by severe bleeding. At present, a predictive model for tigecycline-related coagulopathy is not readily available, and the prognostic value of coagulopathy in tigecycline-administered patients has not been elucidated. In this paper, we investigate the association between tigecycline-related coagulopathy and in-hospital mortality to develop a nomogram for the prediction of tigecycline-related coagulopathy.
Methods: This retrospective cohort study includes 311 adults prescribed with tigecycline from 2018 to 2020. The primary cohort and validation cohort were constructed by dividing the participants in a ratio of 7:3. The endpoint is tigecycline-related coagulopathy, defined as a condition with no abnormality in coagulation prior to tigecycline application but developed the following symptoms upon prescription: activated partial thromboplastin time (APTT) extended by > 10 s than the upper limit of normal (ULN), prothrombin time (PT) prolonged for > 3 s than the ULN or reduced serum level of fibrinogen to < 2.0 g/L. A predictive nomogram based on logistic regression was subsequently constructed.
Results: Tigecycline intake for over 7 days, combined other antibiotics, initial PT, initial fibrinogen and estimated glomerular filtration rate (eGFR), are independent prognostic factors of tigecycline-related coagulopathy. The primary and validation cohort each has an area under the receiver operating characteristic curve (AUC) of 0.792 (0.732– 0.851) and 0.730 (0.629– 0.832) for nomogram, respectively. Furthermore, the fitted calibration curve illustrated adequate fit of the model, while the decision curve analysis demonstrated good clinical value. Survival curves showed a high mortality rate among patients with tigecycline-related coagulopathy.
Conclusion: This nomogram exhibited helpful clinical value in predicting tigecycline-related coagulopathy that could reduce the high mortality rate of patients prescribed with tigecycline.
Keywords: tigecycline, drug-resistant bacteria, coagulopathy, nomogram
Introduction
The multidrug-resistant (MDR) or extensively drug-resistant (XDR) pathogens have attracted more and more public healthcare attention due to the high mortality rate, high morbidity rate and prolonged hospitalization.1 It was estimated that antimicrobial resistance-associated deaths were as high as 1.27 million globally in 2019, among whom approximately 1 million cases were caused by the following six dominating bacteria: Acinetobacter baumannii, Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli, Staphylococcus aureus and Streptococcus pneumoniae.2 Additionally, Acinetobacter baumannii showed a very high carbapenem resistance rate (97%) in patients with ventilator-associated pneumonia in a clinical research conducted in Greece, Italy and Spain. At the same time, almost two-thirds of isolated strains were XDR or even pan-drug resistant.3 With the high incidence and mortality rates of drug-resistant bacteria becoming increasingly concerning, the application of certain antimicrobial agents against MDR or XDR bacterial pathogens is becoming the focal point in clinical practice.
Tigecycline, the first glycylcycline antibiotic, is a 9-t-butylglycylamido derivative of minocycline.4 Tigecycline and colistin are effective therapies for MDR and XDR, especially against Acinetobacter spp. and carbapenem-resistant Enterobacterales.4–6 However, previous randomized controlled trials (RCT) showed that tigecycline has a higher all-cause mortality than comparator antibiotics,7 although the exact reason remains unclear. Meanwhile, the impact of adverse reactions on the efficacy of tigecycline treatment is inevitable. Despite gastrointestinal reactions being recognized as the most common side effects,8 tigecycline-associated coagulation disorders are gaining the attention of physicians nowadays. Hypofibrinogenemia, increased activated partial thromboplastin time (APTT), prolonged prothrombin time (PT) and increased international normalized ratio (INR) have incidence rates of nearly 50% during the administration of tigecycline according to previous studies.9–12 About 11.3% of the patients with tigecycline-associated hypofibrinogenemia were reported to suffer from severe bleeding.13 Prior studies revealed that age, gender, tigecycline dosage and course, baseline fibrinogen level and renal insufficiency may be relevant to the risk factors of hypofibrinogenemia associated with tigecycline.13–15 However, those aforementioned risk factors are not good predictors of tigecycline-related coagulopathy. Besides, the prognostic value of coagulation dysfunction in patients administered with tigecycline has not been elucidated.
In this present study, we developed a nomogram as well as validating it to predict tigecycline-related coagulopathy based on the clinical records of patients prescribed with tigecycline. Furthermore, the association between coagulation dysfunction and in-hospital mortality among patients receiving tigecycline therapy was also investigated.
Method
Participants
A retrospective cohort study was conducted based on a protocol approved by the Ethics Review Board of Sun Yat-sen Memorial Hospital (Guangzhou, China, IRB number SYSEC-KY-KS-2022-009). This study includes adult patients who were prescribed with tigecycline for over 48 hours in Sun Yat-sen Memorial Hospital. The time span is from April 1st, 2018 to July 31st, 2020. Patients without information on coagulation indexes before or during tigecycline intake are excluded. Abnormalities in coagulation function or the occurrence of bleeding events before tigecycline prescription are also part of the exclusion criteria. A flow chart presents the inclusion and exclusion process (Figure 1). The upper normal limits (ULN) of PT and APTT in our laboratory are 14.4 s and 35 s, respectively. Tigecycline-related coagulopathy is defined as a condition with no abnormality in coagulation prior to tigecycline application but meets any of the following conditions for coagulation disturbance during drug administration: PT prolonged for >3 s than the ULN, APTT extended by >10 s than the ULN or serum level of fibrinogen <2.0 g/L. A total of 311 observations were selected for the investigation. The primary cohort and validation cohort were constructed by dividing the participants in a ratio of 7:3. The nomogram was built with the primary cohort and validated with the validation cohort.
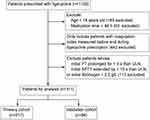 |
Figure 1 Study flow chart. Abbreviations: PT, prothrombin time; ULN, upper limit of normal; APTT, activated partial thromboplastin time. |
Research Information Collection
The following information was collected within 10 days before tigecycline use: demographic data (age, gender, body mass index, in-hospital time, surgery, prescription department, smoke and alcohol abuse), comorbidity (abdominal tumor, pancreatitis, hypertension, coronary heart disease (CHD), apoplexy, diabetes, transplantation and source of infection), treatment (medication time, initial dose and cumulative dose of tigecycline, combined use of other antibiotics, glucocorticoid, ventilator use, anticoagulation or antiplatelet therapy, occurrence of tigecycline-related coagulopathy and in-hospital mortality), coagulation index (PT, INR, fibrinogen, APTT, plasma prothrombin activity (PTA) and D-dimer before tigecycline prescription) and lab results (blood routine examination, electrolyte, liver and kidney function). During tigecycline administration, all information on coagulation indexes was collected. The last measured coagulation indexes during the administration were regarded as the coagulation index level after prescription and displayed as the median [IQR] before being subsequently compared with initial coagulation indexes (Figure 2).
Statistical Method
The R (Vienna, Austria, ver. 4.1.0) software was used for statistical computation. The missing covariates were less than 10% and were filled by multiple imputation. The continuous variables of normal distribution and non-normal distribution are expressed as mean ± SD and median [IQR], respectively. The categorical variables are denoted as number (percentage). The comparison of continuous data is based on Student’s t-test or the Wilcoxon rank sum test, whereas the comparison of categorical data is based on the chi-square test. For the purpose of developing a predictive model for the occurrence of tigecycline-related coagulopathy, a two-way stepwise logistic regression procedure was applied in the primary cohort based on Akaike information criterion to screen all biologically plausible variables for significant variables that meets general medical knowledge in univariate analysis. The variables identified were then entered into a multivariate logistic analysis. A two-sided p < 0.05 is considered statistically significant.
A nomogram was constructed based on results of the multivariable logistic analysis. We evaluated the performance of nomogram by adjusting its clinical value, calibration and discrimination.16 The receiver operating characteristic curve (ROC) was applied to evaluated the predictive capacity of the prediction model by calculating the area under the curve (AUC). The fitted logistic calibration curve was used to analyze consistency between the actual state and the nomogram. Decision curve analysis (DCA) was applied to quantify the standardized net benefits at different threshold probabilities for assessing the clinical value of the predictive model. Additionally, the 30-day survival probability of both the primary and validation cohorts were compared between the patients with tigecycline-related coagulopathy and the non-coagulopathy patients on the survival curves, respectively.
Result
Baseline of the Primary and Validation Cohorts
A total of 311 individuals who met the inclusion criteria were divided into the primary cohort (n = 217) and the validation cohort (n = 94). The mean ages of the patients in the primary cohort and validation cohort were 58.36 ± 15.28 and 59.61 ± 16.98 years, respectively (p > 0.05). Males accounted for 62.7% in the primary cohort and 59.6% in the validation cohort (p > 0.05). The medication time and cumulative dose of tigecycline of the both cohorts showed no significant difference. The median in-hospital time of all patients was 33 days, while the medication time of tigecycline was 1–2 weeks. Cumulative dose of tigecycline can generally reach 0.8–1.8 g in the total course of treatment. In total, 78.8% of the patients were prescribed tigecycline in combination with other antibiotics (the summaries for the prescription department, pathogen, type of infection and antibiotics used in combination are visualized in Figures S1–S4). The median medication time when tigecycline-related coagulopathy occurred was 2 days, with an interquartile range of 1–4 days. Tigecycline-related coagulopathy has an incidence rate of around 50% in both cohorts. Bleeding events during tigecycline medication were observed in 24 patients, accounting for 7.9% within the sample population, whereas the in-hospital mortality rate was 19%. There was no significant difference in the baseline variables between the primary and validation cohorts (all p > 0.05) (Table 1).
 |
Table 1 Comparison of Baseline Between the Primary Cohort and Validation Cohort |
Variation of Coagulation Indexes Before and After Tigecycline Prescription
Figure 2 demonstrates the variation of coagulation indexes in all patients. The level of PT, APTT and INR rose while the level of fibrinogen fell significantly after tigecycline prescription (all p < 0.001). The changes of the above indexes suggest that patients tend to bleed more easily after prescription.
Predicting Factors of Tigecycline-Related Coagulopathy
General demographics, comorbidities, coagulation indexes, lab results and treatments of the primary cohort were further examined using the stepwise logistic regression model to predict tigecycline-related coagulopathy. In the univariate analysis, the following variables were found to be associated with tigecycline-related coagulopathy: age, diabetes, the course of tigecycline medication over 7 days, cumulative dose of tigecycline, combined use with other antibiotics, initial PT, initial APTT, initial fibrinogen and eGFR. The following factors were identified to be independent prognostic factors of tigecycline-related coagulopathy in the multivariate logistic regression analysis: the course of tigecycline medication over 7 days, combined use with other antibiotics, initial PT, initial fibrinogen and eGFR (each p < 0.05) (Table 2). The detailed process of logistic regression can be checked in Tables S1–S4.
 |
Table 2 Univariate and Multivariate Logistic Regression Analysis for the Risk Factors of Tigecycline-Related Coagulopathy in the Primary Cohort |
Establishment of a Nomogram
A predictive nomogram for tigecycline-related coagulopathy was established with the predictive factors gained from the multivariable logistic model. The nomogram was constructed using each of the independent predicting variables with weighted score. The score of combined antibiotics usage, medication over 7 days, baseline PT, eGFR and baseline fibrinogen ranges from 0 to 1, 0 to 1, 9.5 to 16.5, 240 to 0 and 10 to 2, respectively. A score of 35 points was identified as the highest total score. The scale of tigecycline-related coagulopathy probability ranges from 0.95 to 0.1. A higher total score in the nomogram represents a higher incidence of tigecycline-related coagulopathy (Figure 3).
Evaluation of the Nomogram
The predictive capacity of the nomogram was 0.792 (0.732–0.851) in the primary cohort and 0.730 (0.629–0.832) in the validation cohort according to the AUC (Figure 4). The fitted logistic calibration curve illustrated adequate fit of the predictive model for tigecycline-related coagulopathy in both cohorts (Figure 5). The net benefit obtained from the nomogram was 0.90 and 0.77 based on threshold probabilities for the primary cohort and validation cohort, respectively, as demonstrated by the decision curve analysis (Figure 6).
The Association Between Coagulopathy and Mortality
To further analyze the association between tigecycline-related coagulopathy and in-hospital mortality, a log rank test based on survival curves was performed in both the primary and validation cohorts. The survival curves showed that patients with tigecycline-related coagulopathy under tigecycline prescription have a higher incidence of mortality (p < 0.05, log rank test) (Figure 7).
 |
Figure 7 Survival analysis for the primary and validation cohort. Note: (A and B) demonstrate the survival curve in the primary cohort and validation cohort, respectively. |
Discussion
In this study, a nomogram constructed on the basis of clinical characteristics as screened by the logistic regression model included cumulative dose, combined use with antibiotics, initial PT, initial fibrinogen and eGFR to predict tigecycline-related coagulopathy. As evaluated by the AUC, calibration curve as well as DCA, this model exhibits sound predictive performance. Furthermore, the survivor curves revealed that patients suffering from tigecycline-related coagulopathy possess a higher risk of mortality. To our knowledge, this is the first model for predicting tigecycline-related coagulopathy.
Tigecycline, the first glycyl-tetracycline drug, obtained approval from the Food and Drug Administration (FDA) in June 2005 before entering the Chinese market in November 2011. The antibacterial spectrum of tigecycline covers Gram-positive bacteria, Gram-negative bacteria, atypical pathogens as well as anaerobic bacteria. Despite inactivity against proteus spp. and Pseudomonas aeruginosa, tigecycline exhibits powerful antibacterial activity against MDR and XDR, including the methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococci (VRE), carbapenem-resistant Enterobacterales, extended-spectrum β-lactamase-producing Enterobacterales and MDR Acinetobacter spp.17–22 Tigecycline is recommended for community-acquired pneumonia, complicated intra-abdominal infections and complicated skin or soft tissue infections caused by sensitive bacteria, with its indications still rapidly expanding.
As the use of tigecycline increases, the side effects that it brings should be paid more attention as well. Based on information obtained from the FDA from 2004 to 2009, common adverse reactions associated with tigecycline include gastrointestinal effects, pancreatitis, hypoglycemia and liver injury.23 Since the first case of tigecycline-induced hypofibrinogen was reported back in 2010,24 tigecycline-related coagulopathy has attracted widespread attention. Subsequently, several case reports about coagulation disorders induced by tigecycline were published.25–32 However, the accurate incidence of coagulopathy remains uncertain. A study based on the FDA adverse event reporting system (FAERS) database revealed that around 15% of patients prescribed with tigecycline developed coagulation disorder identified by Medical Dictionary for Regulatory Activities terms (V22.0).33 The previous definitions of tigecycline-related coagulation disorder were not unified. Previous studies revealed that more than half of the patients who had undergone tigecycline therapy were presented with hypofibrinogen.13–15 Moreover, the PT, APTT and INR were often applied for the research indicators to explore coagulopathy induced by tigecycline.12,13,34 Cui et al summarized that tigecycline-induced coagulopathy usually manifests as prolongation of the prothrombin time and activated partial thromboplastin time and a reduction in the fibrinogen level.9 In this study, the occurrence rate of coagulation dysfunction, defined as hypofibrinogen, increased APTT or increased PT, was around 50%. Differences in the incidence of various forms of coagulopathy are probably due to differences in definition and population.
Prior studies indicate that coagulopathy occurs within 2 weeks of tigecycline prescription, while the coagulation indicators could be restored several days after tigecycline withdrawal.13,33 Besides, the incidence of bleeding in patients with coagulation dysfunction was documented to be approximately 10%.15,33 This present study yielded highly similar results, where coagulopathy was shown to develop at a median of 2 days, and 7.9% of the patients involved in this study developed bleeding. Some researchers speculate that coagulopathy was associated with increased consumption or impaired synthesis of fibrinogen.35 The liver is an important organ in synthesizing coagulation factors. Yet, liver function was hardly associated with coagulopathy as assessed by the logistic regression analysis in our study. In addition, the direct effect of tigecycline on coagulation function was not observed in vitro.36 Therefore, other investigators inferred that it is likely for tigecycline to indirectly impact the fibrinogen level via suppressing the synthesis of interleukin-6 which has been proven to stimulate the expression of fibrinogen.15 However, the underlying mechanism needs to be further elucidated.
In this present study, the risk factors of tigecycline-related coagulopathy as screened by a multivariable logistic model include cumulative dose of tigecycline, combined antibiotics, initial PT, initial fibrinogen and eGFR, all of which resonates with previous studies.13–15 A predictive model for coagulopathy in the use of tigecycline was further constructed via the integration of relevant risk factors, and the model exhibits satisfactory performance as evaluated by the AUC, calibration curve as well as DCA. Nevertheless, the impact of tigecycline-related coagulopathy on survival outcome is still poorly studied. Herein, the association between coagulopathy and mortality was further evaluated (the potential causes for the higher mortality of patients with tigecycline-related coagulopathy can be checked in Tables S5 and S6). Patients with tigecycline-related coagulation dysfunction have a higher risk of mortality, thus implying the importance of a coagulation index monitor.
Several limitations to this study must, however, be mentioned. First, selection bias is inevitable in a retrospective study. The effect of tigecycline has not been studied in patients with coagulation disorder before prescription. Second, this is a single-center study with small sample size, which may affect the accuracy of the prediction model. Furthermore, the definition of coagulopathy in this study includes the changes of PT, APTT and fibrinogen, irrespective of coagulation markers such as plasmin–α2-antiplasmin complex, thrombin–antithrombin-III complex and so on. Finally, validation from external database is currently absent for the nomogram.
Conclusion
In conclusion, a novel nomogram was constructed on the basis of relevant independent risk factors to predict the occurrence of tigecycline-related coagulopathy. This model possesses the potential as a useful tool in clinical practice, and is thus worthy of further scrutiny. Finally, tigecycline-related coagulopathy was also found to be associated with higher mortality, making it essential to monitor the occurrence of coagulation.
Data Sharing Statement
The data of this study can be obtained from the corresponding authors with reasonable requirement.
Ethics Approval
The whole process of this study is based on the Declaration of Helsinki. This study was conducted in concordance with a protocol approved by the Ethics Review Board of Sun Yat-sen Memorial Hospital, Sun Yat-sen University (No. SYSEC-KY-KS-2022-009). Informed consents were obtained from all enrolled individuals.
Funding
This study is supported by grants from the National Natural Science Foundation of China (No. 82071804 and No. 81700033) and Guangzhou Science and Technology Program Key Project (No. 202102020429).
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter Baumannii and Pseudomonas Aeruginosa in Health Care Facilities. Geneva: World Health Organization; 2017.
2. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi:10.1016/S0140-6736(21)02724-0
3. Nowak J, Zander E, Stefanik D, et al. High incidence of pandrug-resistant Acinetobacter baumannii isolates collected from patients with ventilator-associated pneumonia in Greece, Italy and Spain as part of the MagicBullet clinical trial. J Antimicrob Chemother. 2017;72(12):3277–3282. doi:10.1093/jac/dkx322
4. Karageorgopoulos DE, Falagas ME. Current control and treatment of multidrug-resistant Acinetobacter baumannii infections. Lancet Infect Dis. 2008;8(12):751–762. doi:10.1016/S1473-3099(08)70279-2
5. Rodríguez-Baño J, Gutiérrez-Gutiérrez B, Machuca I, Pascual A. Treatment of infections caused by extended-spectrum-beta-lactamase-, Ampc-, and carbapenemase-producing Enterobacteriaceae. Clin Microbiol Rev. 2018;31(2). doi:10.1128/CMR.00079-17
6. Ni W, Han Y, Zhao J, et al. Tigecycline treatment experience against multidrug-resistant Acinetobacter baumannii infections: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;47(2):107–116. doi:10.1016/j.ijantimicag.2015.11.011
7. McGovern PC, Wible M, El-Tahtawy A, Biswas P, Meyer RD. All-cause mortality imbalance in the tigecycline Phase 3 and 4 clinical trials. Int J Antimicrob Agents. 2013;41(5):463–467. doi:10.1016/j.ijantimicag.2013.01.020
8. Tasina E, Haidich AB, Kokkali S, Arvanitidou M. Efficacy and safety of tigecycline for the treatment of infectious diseases: a meta-analysis. Lancet Infect Dis. 2011;11(11):834–844. doi:10.1016/S1473-3099(11)70177-3
9. Cui N, Cai H, Li Z, Lu Y, Wang G, Lu A. Tigecycline-induced coagulopathy: a literature review. Int J Clin Pharm. 2019;41(6):1408–1413. doi:10.1007/s11096-019-00912-5
10. Leng B, Xue YC, Zhang W, et al. Analysis of the effect of tigecycline on coagulation function. Chem Pharm Bull. 2019;67(3):258–264. doi:10.1248/cpb.c18-00844
11. Zhang Q, Zhou S, Zhou J. Tigecycline treatment causes a decrease in fibrinogen levels. Antimicrob Agents Chemother. 2015;59(3):1650–1655. doi:10.1128/AAC.04305-14
12. Akdağ D, Işıkgöz-Taşbakan M, Pullukcu H, Sipahi H, Sipahi OR. Tigecycline versus INR increase; more than expected? Expert Opin Drug Saf. 2020;19(3):335–337. doi:10.1080/14740338.2020.1723546
13. Hu J, Xiao Y-H, Zheng Y, Lai Y-X, Fang X-L, Fang Q. Clinical characteristics and risk factors of tigecycline-associated hypofibrinogenemia in critically ill patients. Eur J Clin Pharmacol. 2020;76(7):913–922. doi:10.1007/s00228-020-02860-w
14. Liu J, Yan Y, Zhang F. Risk factors for tigecycline-associated hypofibrinogenemia. Ther Clin Risk Manag. 2021;17:325–332. doi:10.2147/TCRM.S302850
15. Zhang Q, Wang J, Liu H, Ma W, Zhou S, Zhou J. Risk factors for tigecycline-induced hypofibrinogenemia. J Clin Pharm Ther. 2020;45(6):1434–1441. doi:10.1111/jcpt.13250
16. Alba AC, Agoritsas T, Walsh M, et al. Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA. 2017;318(14):1377–1384. doi:10.1001/jama.2017.12126
17. Brink AJ, Bizos D, Boffard KD, et al. Guideline: appropriate use of tigecycline. S Afr Med J. 2010;100(6 Pt 2):388–394. doi:10.7196/SAMJ.4109
18. Rodvold KA, McConeghy KW. Methicillin-resistant Staphylococcus aureus therapy: past, present, and future. Clin Infect Dis. 2014;58(Suppl 1):S20–27. doi:10.1093/cid/cit614
19. Bender JK, Cattoir V, Hegstad K, et al. Update on prevalence and mechanisms of resistance to linezolid, tigecycline and daptomycin in enterococci in Europe: towards a common nomenclature. Drug Resist Updat. 2018;40:25–39. doi:10.1016/j.drup.2018.10.002
20. Durante-Mangoni E, Andini R, Zampino R. Management of carbapenem-resistant Enterobacteriaceae infections. Clin Microbiol Infect. 2019;25(8):943–950. doi:10.1016/j.cmi.2019.04.013
21. Morosini MI, García-Castillo M, Coque TM, et al. Antibiotic coresistance in extended-spectrum-beta-lactamase-producing Enterobacteriaceae and in vitro activity of tigecycline. Antimicrob Agents Chemother. 2006;50(8):2695–2699. doi:10.1128/AAC.00155-06
22. Karaiskos I, Lagou S, Pontikis K, Rapti V, Poulakou G. The “Old” and the “New” Antibiotics for MDR gram-negative pathogens: for whom, when, and how. Front Public Health. 2019;7:151. doi:10.3389/fpubh.2019.00151
23. Kadoyama K, Sakaeda T, Tamon A, Okuno Y. Adverse event profile of tigecycline: data mining of the public version of the U.S. Food and Drug Administration adverse event reporting system. Biol Pharm Bull. 2012;35(6):967–970. doi:10.1248/bpb.35.967
24. Pieringer H, Schmekal B, Biesenbach G, Pohanka E. Severe coagulation disorder with hypofibrinogenemia associated with the use of tigecycline. Ann Hematol. 2010;89(10):1063–1064. doi:10.1007/s00277-010-0911-7
25. Rossitto G, Piano S, Rosi S, Simioni P, Angeli P. Life-threatening coagulopathy and hypofibrinogenemia induced by tigecycline in a patient with advanced liver cirrhosis. Eur J Gastroenterol Hepatol. 2014;26(6):681–684. doi:10.1097/MEG.0000000000000087
26. Sabanis N, Paschou E, Gavriilaki E, Kalaitzoglou A, Vasileiou S. Hypofibrinogenemia induced by tigecycline: a potentially life-threatening coagulation disorder. Infect Dis. 2015;47(10):743–746. doi:10.3109/23744235.2015.1043942
27. Giryes S, Azzam ZS, Ismael-Badarneh R, Krivoy N, Berger G. Severe coagulation disorder and thrombocytopenia associated with tigecycline - case report and review of literature. Curr Drug Saf. 2017;12(1):7–9. doi:10.2174/1574886311666160920090714
28. McMahan J, Moenster RP. Tigecycline-induced coagulopathy. Am J Health Syst Pharm. 2017;74(3):130–134. doi:10.2146/ajhp150894
29. Wu X, Zhao P, Dong L, Zhang X. A case report of patient with severe acute cholangitis with tigecycline treatment causing coagulopathy and hypofibrinogenemia. Medicine. 2017;96(49):e9124. doi:10.1097/MD.0000000000009124
30. Wu P-C, Wu -C-C. Tigecycline-associated hypofibrinogenemia: a case report and review of the literature. IDCases. 2018;11:56–57. doi:10.1016/j.idcr.2018.01.003
31. Akalay S, Vanassche T, De Munter P. Tigecycline-induced life-threatening coagulopathy in a patient with a Mycobacterium abscess: a case report and step-by-step diagnostic approach. Acta Clin Belg. 2021;76(5):410–414. doi:10.1080/17843286.2020.1747197
32. Fan Q, Huang W, Weng Y, Xie X, Shi Z. Hypofibrinogenemia induced by high-dose tigecycline-case report and review of literature. Medicine. 2020;99(43):e22638. doi:10.1097/MD.0000000000022638
33. Guo M, Liang J, Li D, et al. Coagulation dysfunction events associated with tigecycline: a real-world study from FDA adverse event reporting system (FAERS) database. Thromb J. 2022;20(1):12. doi:10.1186/s12959-022-00369-z
34. Wang D, Lin C, Gu C, Wu Y, Wang S. Tigecycline-associated coagulopathy: a single-center retrospective analysis. Pharmacology. 2022;107(9–10):524–536. doi:10.1159/000525380
35. Treml B, Rajsic S, Hell T, Fries D, Bachler M. Progression of fibrinogen decrease during high dose tigecycline therapy in critically ill patients: a retrospective analysis. J Clin Med. 2021;10(20):4702. doi:10.3390/jcm10204702
36. Brandtner A, Bachler M, Fries D, et al. Tigecycline interferes with fibrinogen polymerization independent of peripheral interactions with the coagulation system. Antibiotics. 2020;9(2):84. doi:10.3390/antibiotics9020084
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





