Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Developing Appropriate Pulmonary Rehabilitation Services in Sri Lanka: Assessment of People Living with COPD and Healthcare Providers in Urban and Semi Urban Areas in Sri Lanka
Authors Perera ACH , Jayamaha AR , Jones AV , Yusuf ZK , Wijayasiri KDCU, Amarasekara T , Seneviratne A, Miah R, Barton A, Steiner MC , Wimalasekara SW, Orme MW , Singh SJ
Received 21 April 2021
Accepted for publication 24 January 2022
Published 25 March 2022 Volume 2022:17 Pages 631—641
DOI https://doi.org/10.2147/COPD.S316555
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Richard Russell
A Chamilya H Perera,1,2 Akila R Jayamaha,1,2 Amy V Jones,1,3 Zainab K Yusuf,1,3 KDC Upendra Wijayasiri,4 Thamara Amarasekara,5 Anthony Seneviratne,6 Ruhme Miah,1,3 Andy Barton,1 Michael C Steiner,1,3 Savithri W Wimalasekara,7 Mark W Orme,1,3,* Sally J Singh1,3,*
1Department of Respiratory Science, University of Leicester, Leicester, UK; 2Faculty of Nursing, KIU, Colombo, Sri Lanka; 3Centre for Exercise and Rehabilitation Science, NIHR Leicester Biomedical Research Centre-Respiratory, University Hospitals of Leicester NHS Trust, Leicester, UK; 4National Hospital of Sri Lanka, Colombo, Sri Lanka; 5Faculty of Allied Health Sciences, University of Sri Jayewardenepura, Nugegoda, Sri Lanka; 6Primary Care Respiratory Group, Colombo, Sri Lanka; 7Faculty of Medical Sciences, University of Sri Jayewardenepura, Nugegoda, Sri Lanka
*These authors contributed equally to this work
Correspondence: A Chamilya H Perera, Email [email protected]
Introduction: Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, corresponding to 5% of all deaths globally, with more than 90% occurring in low- and middle-income countries (LMIC). Pulmonary Rehabilitation (PR) is a routine clinical service for COPD management, often used in western countries. At present, there is no formal PR in Sri Lanka; a culturally appropriate programme is required that considers the views of adults living with COPD and healthcare providers (HCPs) who would be involved in the referral or delivery of PR.
Purpose: The study assessed the attitudes and preferences of Sri Lankan adults living with COPD and attitudes and barriers of HCPs making PR referrals to inform an appropriate PR programme.
Methodology: A descriptive cross-sectional study was conducted with the ethical clearance of Colombo south teaching hospital ERC committee (ERC Application No. 674), among adults living with COPD and HCPs in Colombo district, Sri Lanka. Adults living with COPD were enrolled August 2018–December 2018 using systematic random sampling from Colombo South Teaching Hospital and were assessed using a pre-tested interviewer administered questionnaire. HCPs were recruited from Colombo South Teaching Hospital and Jaffna Teaching Hospital between August 2018 and November 2018 and assessed using self-administered questionnaire.
Results: Responses from 138 adults living with COPD (53% male, 52% aged ≥ 60 years) and 277 HCPs were collected. The majority of adults living with COPD were interested in participating in PR (80%) and would prefer PR to be delivered in a supervised, group-based, setting with hospital-based (49%). Adults living with COPD were mostly (73%) willing to spend between 30 minutes and 2 hours per day for PR-related activities. Among HCPs, 234 (83%) were nurses, 29 (11%) were hospital doctors and 14 (4%) were family physicians. The majority of HCPs stated that they were unsure about referring adults with COPD for PR (86%) and 61% stated considerable uncertainty regarding the availability of resources for PR. Nearly half of the HCPs (45%) felt they were not adequately prepared to refer adults living with COPD to PR programmes. Most HCPs (92%) reported that PR is worthwhile for COPD management.
Conclusion: Adults living with COPD in Sri Lanka are willing to attend PR and would prefer group-based programmes delivered in hospitals, under the supervision of qualified personnel. Awareness about PR is poor and there is a lack of readiness to refer to PR amongst HCPs. There is an urgent need to train HCPs on PR and develop effective referral strategies to support PR uptake and delivery for adults living with COPD in Sri Lanka.
Keywords: pulmonary rehabilitation, opinion, patients, healthcare providers
Introduction
Chronic obstructive pulmonary disease (COPD) is a common preventable and treatable disease condition which accounts for 5% of all deaths globally. More than 90% of COPD deaths occurring in lower and middle income countries (LMIC) and it is the third leading cause for deaths worldwide.1 The most recent estimate of COPD prevalence in South Asia was 6.3% with a prevalence in Sri Lanka of 10.5%,2 demonstrating COPD is a significant burden to both patients and healthcare services.
When managing COPD, there are several treatment options available in Sri Lanka, which include smoking cessation and pharmacological treatment such as bronchodilators, inhaled corticosteroids and influenza and pneumococcal vaccinesSame time options for disease self-management are limited. Pulmonary Rehabilitation (PR) is an established and effective intervention that is low cost and high impact, proven to reduce the disability associated with lung disease, and is supported by the highest level of research evidence3 PR is a highly recommended intervention by many international bodies2 and brings together HCPs from many disciplines offering supervised exercise training and disease education, supporting people to manage their own disease.4,5 There remains an unmet need for PR in low resource settings6 and few trials of PR have been conducted.7 At present, there is no established PR programme available in Sri Lankan healthcare settings. Therefore, there is an urgent need in introducing a culturally adopted PR programme for Sri Lankan adults with COPD. In preparation for this it is very important to get the opinions of adults living with COPD about their requirements and preferences for PR. Patients with COPD as the recipients of PR should feel it is an achievable target. When planning a PR programme, it should be patient centered and HCPs should be competent in its delivery. HCPs are important to increase the awareness of PR as well as to deliver PR for adults living with COPD.8 Thus, it is important to obtain the views of adults living with COPD on how they would prefer to have PR and the most suitable way of delivering PR. Further it is essential to understand the challenges faced by HCPs in referring patients for PR and the needs of HCPs in delivery of PR in the local setting. Health care providers are stakeholders who offer PR to suitable candidates. As HCPs refer patients for PR, they should have a very good understanding of the referral criteria and processes by which a referral can be made. Otherwise it will not be possible to embed PR into routine care. Also, patients are beginning to believe in and expect active engagement of the HCP during the process of initiating and conducting the PR programme.9 When considering the above factors as an initial step of developing culturally adopted PR it is very important to get the input of adults living with COPD and health care providers. To support the development and practice of PR in Sri Lanka, an exploration of the service users’ needs and requirements is necessary, alongside those of the health care professionals likely to recommend and refer to PR.
Accordingly, this study aimed to assess, (i) attitudes for adults living with COPD to participate in PR (ii) their preference regards the structure of PR (specifically the delivery mode and time commitment) and (i) attitudes and (ii) barriers of HCPs to make potential referrals for PR.
Materials and Methods
Study Design
The study was conducted as two separate cross-sectional surveys. Survey one evaluated the attitudes and opinions of adults living with COPD on PR and survey two was conducted with HCPs who would likely refer adults to PR or deliver PR. This study has been registered with the ISRCTN (ISRCTN58273367) and is reported in accordance with the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines. Ethics approval for the study was obtained prior to data collection from Colombo South hospital, Sri Lanka (ERC Application No. 674) ethics review committee and permission was obtained from relevant authorities. This study was conducted in accordance with the Declaration of Helsinki.
Study Setting
Data collection for survey one occurred at the Chest Clinic of Colombo South Teaching Hospital, Sri Lanka, during a four month time period in 2018. Data for survey two was collected at Colombo South Teaching Hospital and Jaffna Teaching Hospital which is the main hospital in the Northern province of Sri Lanka; data was collected from August – November 2018.
Participants and Recruitment
The inclusion criteria for adults were adults aged 18 years old and above, a confirmed diagnosis of COPD based on GOLD (Global Initiative for Obstructive Lung Disease) criteria,10 had regularly attended the clinic for more than for 6 months’ prior to the recruitment period, free from an exacerbation at the time of participation, and ability to complete the survey in Sinhala, Tamil or English. Participants were recruited by a clinic nursing officer from the Central Chest Clinic at Colombo South Teaching Hospital, using a systematic random sampling method (every fifth patient was included in the sample, originating from the seventh patient). The clinic nursing officer was blinded to the study and participants were selected from the clinic registration book. HCPs were eligible to participate if they worked at Colombo South Teaching hospital or Jaffna Teaching Hospital and were directly involved in the care of adults with COPD. A convenient sampling method was used for the selection of HCPs. The sample was consisted of 234 (84%) nurses, 29 (11%) hospital doctors and 14 (5%) family physicians who were directly involved in the care of respiratory disease patients.
Both surveys for adults living with COPD and HCPs were distributed as paper copies after providing all the relevant information and obtaining written informed consent by protecting the anonymity of the participants. Survey questionnaires were provided to participants by the four research team members in the participants’ preferred language. The participants were recognized only from the identification number given by the researchers and privacy and confidentiality were fully enforced during the data collection process.
Variables
The primary outcome measures for the study was how their breathing problem effected their paid and unpaid work and level of activity, their preference regards the structure of PR as mode of delivery and acceptable time commitment. For HCPs, the survey examined responsibilities of caring for COPD patients, availability of PR, potential barriers to referring to PR, assessed the infrastructure available and their capacity to refer adults living with COPD. Both surveys used for data collection are provided as Supplementary Material A and B.
Data Collection
The patient survey was conducted using an interviewer administered questionnaire with details of personal characteristics, how their breathing problem was effected on paid and unpaid work and level of activity, their preference regards the structure of PR as mode of delivery and acceptable time commitment. The data collection of HCPs was conducted using a self-administered questionnaire which included questions about the role of the HCP in the management of COPD patients, availability of PR and referral process.
Both questionnaires were developed in English as part of the National Institute of Health Research (NIHR) Global Health Research Group on Respiratory Rehabilitation (Global RECHARGE, 17/63/20), with contributions from clinicians and researchers from several LMICs and the UK. Surveys were translated into Sinhala and Tamil languages, then back-translated as part of validity checking. Both survey questionnaires were pretested by 10 participants from each group and public involvement (PPI) prior to data collection. Minor modifications such as changes to wording were made in accordance with the PPI feedback. A formal sample size calculation was not conducted, as the study was exploratory.
Data Analysis
Data were reported as frequencies and percentages (%), means (standard deviation, (SD) as appropriate. No inferential statistics were used due to the descriptive nature of the study. Data were analyzed using Microsoft Excel and IBM SPSS (version 25). The free text questions included in surveys were analyzed using autonomous qualitative counting, whereby participants’ responses were counted and grouped together based on similarity.
Results
One hundred and sixty-four adults living with COPD were invited to take part in the study, of which 140 were eligible (as they have fulfilled the eligibility criteria) and 138 completed the survey. Two survey reports were removed as they were incomplete.Four hundred and twenty-six HCPs were invited to participate, of which 277 completed the survey. Out of the eligible 286 HCPs 277 survey questionnaires were completed in full and 9 had missing details. (Figure 1).
 |
Figure 1 Recruitment flow diagram. |
Participant Characteristics
Most adults living with COPD self-reported their sex as male, were aged ≥60 years, not in employment and did not use technology (83%) (Table 1).
 |
Table 1 Participant Characteristics (n=138) |
The most common professional job categories of HCPs were nursing officers 234 (84%), hospital doctor 29 (11%), and family physician 14 (5%). The most common responsibilities of the staff were diagnosing (68%), primary care (55%), medication checks (55%), inpatient treatment (52%), admission prevention (51%), oxygen therapy (50%), urgent assessments (45%), on-going management (40%) and prescribing (15%).
Responses of Adults Living with COPD
For the majority of respondents 80% reported a breathing problem affected their ability to carry out unpaid work, 53% were affected in their ability to carry out paid work, and 88% reported missing at least a day of work because of breathing problems. When asked about their ability to keep up with peers when walking, 57% reported that they were unable to do so and that breathing problems prevented (87%) from being as physically active as they would like. Half of participants reported being unable to visit friends or family as often as they would like due to breathing problems and overall, 89% reported that their breathing problems bothered them (Supplementary material B, Question No. 5–11).
Eighty percent of participants stated they would be interested in participating in a treatment to reduce breathlessness and increase their physical activity. Reasons for not being interested in such a treatment were: being satisfied with current breathing and activity levels (16%), concerned about the monetary cost of treatment (2%), no time to spend on treatment (1%), or currently using alternative treatment (1%) (Supplementary material B, Question No. 12a).
Participants preferred structure of PR (mode of delivery and how long participants would be willing to spend on PR) is provided in Table 2. (Supplementary material B, Question No. 12b, 12c).
 |
Table 2 Preference Regards the Structure of a PR Programme Among Adults Living with COPD (n=138) |
Responses of HCPs
Most HCPs reported believing PR to be “worthwhile”, with 92% (n=255) answering “Yes, very much”, 5% (n=13) answering “Yes, a little”, 2% (n=6) answering “No” and 1% (n=3) “unsure”. Also around 40% of the HCPs mentioned that they are having a PR programme in there clinical setting. when asked to elaborate on their responses using the free-text options, HCPs mentioned that it as similar to the exercise programmes.
With regards to the opinions of the staff on referring to PR (Figure 2), more than 50% strongly agreed and agreed that difficulties in referring patients could be overcome and are open to enabling new ways and would like to receive outcomes of PR referral.
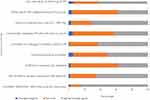 |
Figure 2 HCPs opinions on referring to Pulmonary Rehabilitation Data presented as a percentage of those that strongly disagree, disagree and agree/strongly agreed. |
Regarding the patient based factors that may impact PR referral (Figure 3), HCPs most frequently reported that they would recommend adults with COPD to PR that have low exercise tolerance (84% strong influence) and have increased shortness of breath (83% strong influence). They have provided considerable level of free text evidence also for confirm this referral reasons such as minimizing the drug dependency of most of the patients and preference for change in routine lifestyle.
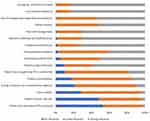 |
Figure 3 Patient-based factors influencing decision to refer to PR, with influence graded as no, some or strong influence. Data presented as a percentage. |
Data were also collected from the HCPs regarding factors affecting to the referral process, their knowledge and their workload that may influence their decision to refer a patient to PR (Figure 4). Thirty one percent of the HCPs (n= 87) stated an unawareness of how to make PR referrals would strongly influence their actions, and 69% (n = 194) stated a difficult referral process would have some influence in their decision to refer to PR.
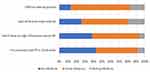 |
Figure 4 Referrer and referral process-based Factors influencing decision to refer to PR, with influence graded as no, some or strong influence. Data presented as a percentage. |
When asked about the main reasons for making referrals of patients to PR, health care providers mentioned that patient’s breathing difficulties, low exercise capacity and difficulty in doing their normal physical activity were the main reasons. Also, when HCPs were asked about improving referrals and uptake of PR, the majority of them emphasized the need to increase resources (78%) and develop clear referral procedures (71%).
Discussion
In this paper, we explored the views of adults living with COPD and HCPs towards PR, including their preferred mode of delivery and time commitment. There was a very high interest amongst adults living with COPD in participating in PR, with a clear preference for hospital-based supervised programmes and were prepared to dedicate between 30 minutes and 2 hours per day. Despite the vast majority of HCPs reporting that PR is worthwhile for COPD management, almost half felt inadequately prepared to conduct referrals, with much uncertainty as to how this would fit into their job role and the resources available to them. The present study highlights a high demand and need for PR in Sri Lanka but also clearly identifies a lack of a clear pathway and resources to implement effective referral processes. Education, training and dedicated resources for referral are needed if PR is to become part of routine care for people living with COPD in Sri Lanka.
Our observation that adults living with COPD would prefer hospital-based PR is in slight contrast to a systematic review of PR trials in LMIC, which identified 13 trials of which 5 were conducted in hospital settings compared with 7 conducted as home-based programmes.7 No trials identified in this systematic review were conducted in Sri Lanka. It may be that people living with COPD preferred hospital-based PR because PR is a very new concept for people in Sri Lanka. Therefore, at least in the earlier stages of developing PR, it is perhaps unsurprising that patients preferred having PR under the supervision of trained medical professional. The same systematic review7 identified that home-based PR using inexpensive equipment may be more suitable for the rural areas with limited resources and poor transport facilities. This is likely to be particularly helpful in Sri Lanka too as most of these patients who are attend COPD clinics are retired elderly people who have issues with transportation and expenses. Health care providers seem to share a similar point of view.11 The current study was conducted around urban and semi urban areas in Sri Lanka. When compared to the rural areas, they have considerable level of resources and facilities for transportation. Therefore, facilitates wise traveling to the hospitals is less of a barrier to these individuals, except to the elderly patients who more often need support of another person to travel out of home. Level of income and the capacity of expenses can also affect this. One of the main issues regarding initiation of PR and adherence to the program is poor attendance due to limited access to transport and a lack of perceived benefits.12 Even though that the similar study conducted in Uganda have given the similar findings as 66% of the participants were preferred in group, supervised, hospital-based programme.13 This also might be due to the unavailability of resources and different cultural expectations of people same as Sri Lankan setting.
Also, as a cultural practice in Sri Lankan settings, face to face interview with the medical professionals is the most preferred way of getting treatments. Hence conducting PR in the hospital setting under the supervision of medical person fits with our urban population of patients and, when implemented, should make PR more attractive and appealing to attend.
There was a contradiction between the low usage of technology (including internet) among the participants (17%) and the number of participants reporting a web-based programme as a preferred mode of PR delivery (31%). As most of the participants were aged over 60 years, these conflicting findings may be because patients can rely on the help of their children and grandchildren who are more frequent and more competent users of technology. As this study was conducted before the COVID 19 pandemic, we can now reasonably expect our patients to be more familiar with communication technology, online education platforms and other technology-based activities. During the COVID-19 pandemic there has been a great influence on telehealth services as the Ministry of Health have developed mobile applications to expand telehealth services in Sri Lanka.14 There has been a very high demand in using digital technologies in Sri Lankan healthcare over the past year, including video-based communication platforms especially for the health and education delivery during the pandemic. As with other observations, this influence on development of technology usage has been very important to maintain doctor-patient relationship.15 Therefore, it might be that digital PR programme could have a future for PR delivery, such as part of a menu of PR options, for people living with COPD in Sri Lanka. Our experience and conversations with patients since completing the survey would suggest the overwhelming preference for group- and hospital-based PR remains.
The majority of HCPs reported PR as worthwhile, however they also identified a number of barriers to referring patients to PR. In particular, they reported a lack of resources for PR referral. Lack of hospital capacity and trained health care providers are the major barrier for setting up a PR programme.16 When conducting a PR programme there are urgent requirements in several physical resources as well as human resources. In relation to the physical resources, exercise equipment, walking aids and spaces and audio visual equipment may having the high necessity and as the main human resource requirement well trained physiotherapists and other medical persons are needed. However, providing PR within existing infrastructure and using incumbent health professionals in the hospitals will be an initial step in managing this issue within low resources17 Also, in the current study an important finding was that most of the HCPs mentioned that there is no clear referral system in place. Therefore, there is a vital need in make the referral process more efficient. There was a very specific unsureness regarding most of the concerns in referral procedure. Without timely information and robust and clear referral procedures, it is unreasonable to expect PR to be implemented as part of usual care in a cost-effective manner that is appealing to patients.18
Some HCPs reported uncertainty as to the value of PR despite the unequivocal evidence of its benefit3 and its inclusion in national and international guidelines (ERS/ATS, BTS, etc.).19 This highlights the need for education programmes for HCPs on PR, its benefits and making suitable referrals. By doing this, HCP referrers will be better equipped to explain these benefits to patients which will in turn increase the chances of patients attending PR services regularly. Lack of knowledge on PR among HCPs and not having established common guidelines to making referrals has become the major concern in relevant to the lack of progress in PR.16 In providing this education and awareness it will be significant to use the help of the well trained and well-known resource persons like clinic consultants, physiotherapists and nurses, conducting practical workshops, education sessions, including involving policy makers to facilitate adoption within routine healthcare. At government level, making PR part of standard COPD care through financial incentives and improving information flow regarding the referrals and services among HCPs and spreading information over the general public may give more influence on the expansion of PR.20
Our study has some limitations which must be considered when interpreting findings. The current study recruited adults living with COPD in the urban and semi urban Colombo areas and it cannot be assumed that adults living in different settings require the same support or would prefer the same structure of PR services. People living with other chronic respiratory diseases may have different preferences and it would also be helpful to supplement these findings with in-depth qualitative approaches.21 However, we can be confident these findings are likely to facilitate wider adoption of appropriately designed PR across Sri Lanka and possibly other areas of South Asia, complimenting other advances in this area such as standardizing PR outcome measures22 and growing evidence of feasibility and effectiveness of PR in low resource settings.23
Conclusion
People living with COPD in Sri Lanka are willing to attend PR and would prefer group-based programs delivered in hospitals, under the supervision of qualified personnel. Despite growing interest in PR in Sri Lanka, South Asia and low resource settings globally, awareness of HCPs in our study about PR was poor, including its benefits, and there is a lack of readiness for referrals to PR amongst HCPs. The lack of readiness is related to both the resource limitations as well as the lack of understanding of potential referrers about PR. There is an urgent need to train HCPs on appropriate referral to PR for adults living with COPD in Sri Lanka. PR services in Sri Lanka should be designed around the preferences of adults living with COPD and future work should continue to develop PR by actively involving the people it is intended to benefit.
Acknowledgments
We acknowledge all the participants who shared their valuable details with us, as well as directors and all the health care professionals at Colombo South Teaching Hospital and Jaffna teaching hospital. We would like to acknowledge Dr. Jonathan Fuld, Addenbrookes Hospital, UK, who allowed us to modify his original survey questionnaire and who was part of the team that designed the HCW survey questionnaire for this study.
Funding
This research was funded by the National Institute for Health Research (NIHR) (17/63/20) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK Department of Health and Social Care.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO report. Chronic Respiratory Disease: burden of COPD. Herd; 2016. Available from: http://www.who.int/respiratory/copd/burden/en/.
2. Amarasiri L, Gunasinghe W, Sadikeen A, et al. The prevalence of Chronic Obstructive Pulmonary Disease (COPD) in Sri Lanka: outcomeof the BOLD study. Epidemiol Eur Respir Soc; 2017;1:PA1212.
3. Mccarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2015:2. doi:10.1002/14651858.CD003793.pub3
4. Nici L, Donner C, Wouters E, et al. American thoracic society/European respiratory society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173(12):1390–1413. doi:10.1164/rccm.200508-1211ST
5. Corhay JL, Dang DN, Van Cauwenberge H, Louis R. Pulmonary rehabilitation and copd: providing patients a good environment for optimizing therapy. Int J COPD. 2013;9:27–39. doi:10.2147/COPD.S52012
6. Singh SJ, Halpin DMG, Salvi S, Kirenga BJ, Mortimer K. Exercise and pulmonary rehabilitation for people with chronic lung disease in LMICs: challenges and opportunities. Lancet Respir Med. 2019;7(12):1002–1004. doi:10.1016/S2213-2600(19)30364-9
7. Habib GM, Rabinovich R, Divgi K, et al. Systematic review of clinical effectiveness, components, and delivery of pulmonary rehabilitation in low-resource settings. npj Prim Care Respir Med. 2020;30:1. doi:10.1038/s41533-020-00210-y
8. Meis JJM, Bosma CB, Spruit MA, et al. A qualitative assessment of COPD patients’ experiences of pulmonary rehabilitation and guidance by healthcare professionals. Respir Med. 2014;108(3):500–510. doi:10.1016/j.rmed.2013.11.001
9. Halding AG, Wahl A, Heggdal K. “Belonging”. “Patients” experiences of social relationships during pulmonary rehabilitation. Disabil Rehabil. 2010;32(15):1272–1280. doi:10.3109/09638280903464471
10. GOLD. Global Initiative for Chronic Obstructive. Glob Obstr Lung Dis GOLD. 2018:1–44. http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Apr2.pdf.
11. Alsubaiei M, Cafarella P, Frith P, McEvoy R, Effing T. Factors influencing management of chronic respiratory diseases in general and chronic obstructive pulmonary disease in particular in Saudi Arabia: an overview. Ann Thorac Med. 2018;13(3):144. doi:10.4103/atm.ATM_293_17
12. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8(2):89–99. doi:10.1177/1479972310393756
13. Katagira W, Jones AV, Orme MW, et al. Identifying appropriate delivery of and referral to pulmonary rehabilitation in Uganda: a survey study of people living with chronic respiratory disease and health care workers. Int J COPD. 2021;16:2291–2299. doi:10.2147/COPD.S314849
14. Kulatunga GG, Hewapathirana R, Marasinghe RB, Dissanayake VHW. A review of Telehealth practices in Sri Lanka in the context of the COVID-19 pandemic. Curr Practice. 2020;11(1):8–19.
15. Vargo D, Zhu L, Benwell B, Yan Z. Digital technology use during COVID-19 pandemic: a rapid review. Hum Behav Emerg Technol. 2021;3(1):13–24. doi:10.1002/hbe2.242
16. Alsubaiei ME, Cafarella P, Frith P, McEvoy R, Effing T. Barriers for setting up a pulmonary rehabilitation program in the Eastern Province of Saudi Arabia. Ann Thorac Med. 2016;11(2):121–127. doi:10.4103/1817-1737.180028
17. Jenkins S, Hill K, Cecins NM. State of the art: how to set up a pulmonary rehabilitation program. Respirology. 2010;15(8):1157–1173. doi:10.1111/j.1440-1843.2010.01849.x
18. Milner SC, Boruff JT, Beaurepaire C, Ahmed S, Janaudis-Ferreira T. Rate of, and barriers and enablers to, pulmonary rehabilitation referral in COPD: a systematic scoping review. Respir Med. 2018;137:
19. Singh SJ, ZuWallack RL, Garvey C, et al. Learn from the past and create the future: the 2013 ATS/ERS statement on pulmonary rehabilitation. Eur Respir J. 2013;42(5):1169–1174. doi:10.1183/09031936.00207912
20. Johnston KN, Young M, Grimmer KA, Antic R, Frith PA. Barriers to, and facilitators for, referral to pulmonary rehabilitation in COPD patients from the perspective of Australian general practitioners: a qualitative study. Prim Care Respir J. 2013;22(3):319–324. doi:10.4104/pcrj.2013.00062
21. Jayamaha AR, Perera CH, Orme MW, et al. Protocol for the cultural adaptation of pulmonary rehabilitation and subsequent testing in a randomised controlled feasibility trial for adults with chronic obstructive pulmonary disease in Sri Lanka. BMJ Open. 2020;10(11):1–11. doi:10.1136/bmjopen-2020-041677
22. Orme MW, Free RC, Manise A, et al. Global RECHARGE: establishing a standard international data set for pulmonary rehabilitation in low- and middle-income countries. J Glob Health. 2020;10(2):2. doi:10.7189/JOGH.10.020316
23. Bickton FM, Fombe C, Chisati E, Rylance J. Evidence for pulmonary rehabilitation in chronic respiratory diseases in sub-Saharan Africa: a systematic review. Int J Tuberc Lung Dis. 2020;24(10):991–999. doi:10.5588/IJTLD.19.0526
 © 2022 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a
Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
© 2022 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a
Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
