Back to Journals » Nutrition and Dietary Supplements » Volume 12
Determinants of Nutritional Edema Among Under-Five Children with Severe Acute Malnutrition Admitted to Health Facilities at Gedeo Zone: Unmatched Case–Control Study
Authors Hussen Kabthymer R , Yacob T, Tenkolu G
Received 13 November 2019
Accepted for publication 15 February 2020
Published 26 February 2020 Volume 2020:12 Pages 49—56
DOI https://doi.org/10.2147/NDS.S238403
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gary Johanning
Robel Hussen Kabthymer, 1 Terefe Yacob, 2 Girma Tenkolu 1
1School of Public Health, Dilla University, Dilla, Ethiopia; 2Hulla Primary Hospital, Hulla, Ethiopia
Correspondence: Robel Hussen Kabthymer
Dilla University, P.O. Box - 419, Dilla, Ethiopia
Tel +251913575702 Email [email protected]
Purpose: To assess the determinants of nutritional edema among under-five children with severe acute malnutrition admitted in health facilities at Gedeo zone, southern Ethiopia, 2018.
Patients and Methods: Institution-based unmatched case–control study was conducted on 291 (97 cases and 194 controls) children. Structured questionnaires were used to collect data. Data were entered into EpiData version 3.1 and exported to SPSS version 24. Descriptive analysis was done using the frequency tables and graphs. Bivariate and multivariate binary logistic regression analysis was used to identify independent determinants of edematous malnutrition, and P-value < 0.05 was used to declare statistical significance.
Results: Multivariable logistic regression analysis revealed that edematous malnutrition was associated with antenatal care (ANC) utilization during pregnancy (adjusted odds ratio [AOR]: 0.05, 95% confidence interval [CI], 0.02– 0.13). Childhood diarrhea within the previous two weeks before admission to health facility increases the odds of developing edema by 2.8 times as compared to those who did not develop diarrhea (AOR: 2.83, 95% CI, 1.21– 6.65).
Conclusion: The findings of this study have confirmed that ANC during pregnancy and having childhood diarrhea within the previous two weeks before admission to health facility were associated with edematous malnutrition. To prevent edematous malnutrition, mothers are encouraged to attend ANC during pregnancy, and to prevent childhood diarrhea, community awareness needs to be strengthened by giving participatory sanitation and hygiene activity.
Keywords: severe acute malnutrition, edematous malnutrition, under-five children, Ethiopia
Introduction
Acute malnutrition is caused by a decrease in food consumption or illness, resulting in bilateral pitting edema or sudden weight loss. Severe acute malnutrition (SAM) is characterized by the presence of bilateral pitting edema or mid-upper arm circumference of <11.5 cm or weight-for-height Z-score (WHZ) <-3 SD (standard deviation) or weight-for-height <70% of growth reference (World Health Organization). The clinical manifestations of SAM include marasmus (severe wasting), kwashiorkor (bilateral pitting edema), marasmic kwashiorkor (a mixed form of bilateral pitting edema and severe wasting), all forms present with protein deficiency.1–3
Edematous malnutrition is rampant in many parts of the world and is associated with a high case-fatality rate. It is associated with an increased secretion of an antidiuretic hormone that prevents the normal excretory response to water administration.4
Bilateral pitting edema (kwashiorkor) can be verified by applying pressure using the thumb on top of both feet for three seconds and if it leaves an indentation on the foot after the thumb is lifted. In most cases, anthropometric measurements and/or the presence of bilateral pitting edema confirm a clinical diagnosis of edematous malnutrition.1,2
There are two immediate causes of edematous malnutrition. The first is when a child does not have enough food to eat and the second is when a child develops an illness or infection. If the child is left untreated then death becomes inevitable.5
Edematous malnutrition is a public health problem that highly affects children in sub-Saharan Africa. At the early stages of life, it increases the risk of infection, morbidity, and mortality.6–9 Globally, more than 29 million children under the age of 5 years suffer from edematous malnutrition.10,11 Even though edematous malnutrition declined relatively during the year 1990s globally, its burden in Africa has increased.12 The prevalence of edematous malnutrition varies from 0% to 32.9%. Children in Central and South Africa were at high risk of developing edematous malnutrition.13 Children with edematous malnutrition are nine times more likely to die than children with non-edematous malnutrition.14 Ninety percent of cases occur in sub-Saharan Africa and South Asia.15,16
In developing countries, children with edematous malnutrition have a higher risk of mortality even in the absence of other medical comorbidities, and the risk of death is twice higher than non-edematous malnutrition.17
Before interventions can be planned, it is necessary to understand and identify contributing factors of edematous malnutrition in a particular setting. But there is no adequate population-based data on determinant factors of edematous malnutrition. This is due to the fact that large-scale health and nutrition surveys do not make any attempts to identify factors of edema. Case fatality, however, is very high among children hospitalized with edematous malnutrition in Ethiopia. This study intended to fill the need for better information on the determinant factors of edematous malnutrition.
Materials and Methods
Study Setting
The study was conducted in Gedeo zone, southern Ethiopia. Gedeo zone is 1 of the 14 zones in the Southern Nations, Nationalities, and Peoples’ Region (SNNPR) of Ethiopia. Gedeo zone has a total population of 1,105,813. The zone has 6 districts (Bule, Gedeb, Wonago, Kochere, Yirgachefe, and Dila zuria) and 2 administrative towns (Dila and Yirgachefe). It has 1 referral hospital, 3 primary hospitals, and 40 health centers (HCs) (Figure 1).
 |
Figure 1 Map of Gedeo zone. |
In Gedeo zone, there are 10 HCs which gives stabilization and treatment service for SAM, located in Yirgachefe (5 HCs) and Wonago (5 HCs) districts. All those 10 HCs were included in this study. The study was conducted from March 26 to May 13, 2018
Study Design
- An institution-based unmatched case–control study was conducted.
Study Populations
All selected under-five children with SAM admitted to health facilities in the Gedeo zone during the study period.
Inclusion Criteria
- Case: under-five children with edematous SAM (bilateral pitting edema) irrespective of their WHZ who were admitted in selected health facilities in Gedeo zone during the study period.
- Control: under-five children SAM (WHZ ≤−3) without bilateral pitting edema who were admitted in selected health facilities in Gedeo zone during the study period.
Exclusion Criteria
- Children who are admitted to the health center with edema other than nutritional edema (bilateral pitting edema).
Study Unit
Study unit for the study was all under-five children who were admitted with SAM (both edematous and non-edematous malnutrition) with their caregiver/mother
Sample Size Determination
The sample size was calculated through STATCAL application of Epi-Info version 7 assuming a double population proportion formula with a 95% confidence interval (CI), 80% power (1-β), and a control:case ratio of 2:1. The determinants of nutritional edema among under-five children using percentage of control assumed to be 57.2% with an odds ratio (OR) of 2.29 (family size ≥5) were assessed based on a case–control study done at Konso district, in Karat town, southern Ethiopia.5 In this study, sample size was 291 (97 cases and194 controls) with assuming a 10% nonresponse rate.
Data Collection Procedure
The questionnaire was first prepared in English and then translated to Gedeofa and Amharic and back-translated into English to check its consistency. A structured questionnaire of a Gedeoffa (local language) version was used by the data collectors.
Data were collected by four diploma nurses by face-to-face interview using the structured questionnaire.
Data Quality Assurance
The pretest was conducted in 5% (15) of the sample size in a nearby (Chichu) HC at Gedeo zone before the actual data collection. Intensive training was given to data collectors and supervisors. Data were checked daily for completeness and consistency at the site of the study by supervisors.
Data Processing and Analysis
The data were entered into EpiDATA version 3.1 software and exported to SPSS version 24 software for cleaning and analysis. A descriptive analysis was carried out for each of the variables using tables and graphs. Then, data were analyzed using bivariate and multivariate binary logistic regression. Variables with P-value <0.25 on bivariate analysis were taken as candidates for multivariate analysis. Crude and adjusted ORs with 95% CI were used. P-value ≤0.05 was used to declare statistical significance.
Dependent Variable
- Edematous malnutrition (Yes/No)
Independent Variable
- Sociodemographic and socioeconomic factors: age of the child, sex of the child, age of mother, family size, educational status of mother, educational status of father, residence urban/rural, occupational status of mother, occupational status of father, birth interval, decision-making on resource use, source of income, etc.
- Child feeding and caring practice: breastfeeding, complementary feeding, hygiene, etc.
- Health service utilization: antenatal care (ANC) utilization, deworming, immunization, etc.
- Sanitation and hygiene: the source of water supply, availability of latrine, etc.
- Childhood illness – diarrhea
Ethical Consideration
Ethical clearance was obtained from Dilla University, College of Medical and Health Science ethical review board. Permission letter was taken from the zonal health bureau and submitted to district health offices. In addition, written accent and consent was obtained from caregivers of the children.
Results
Descriptive Analysis
Sociodemographic and Socioeconomic Characteristics
In this study, a total of 291 study participants (97 cases and 194 controls) were involved resulting in a 100% response rate. The median age of the cases and controls was 25.5 (SD: 11.8) months and 22.5 (SD: 15.6), respectively. Among the cases and controls, 52 (53.6%) and 93 (47.9%) were males. Regarding the residence of the children, 95 (97.9%) of the cases and 185 (95.4%) of the controls were from rural.
Among the interviewed 291 mothers, 31 (32%) of the mothers of cases and 98 (50.5%) of the mothers of the controls were aged >25 years. In this study, majority of the households of the cases (79 ,81.4%) have family sizes greater than 5 as compared to that of of the controls 129 (66.5%).
Among mothers of the cases and controls, 79 (81.4%) and 106 (54.6%) were illiterate, respectively. Regarding occupation, the majority of the mothers of the cases (87, 89.7%) and the controls 125 (64.4%) were housewives (Table 1).
 |
Table 1 Comparison of Sociodemographic and Socioeconomic Characteristics of SAM Children with and Without Edematous Malnutrition in Gedeo Zone, SNNPR June 2018 |
Regarding birth interval, short birth interval (<24 months) is observed in 26 (26.8%) families of the cases and 95 (49%) families of the controls.
Child Feeding and Caring Practices
In this study, the prevalence of breastfeeding in a child in his/her lifetime was found in 85 (87.6%) and 181 (93.3%) of the cases and controls, respectively . Among breastfeed, 14 (14.4%) among cases and 90 (46.6%) among controls were only 2–3 times feed per day. The majority of children started complementary food between 4 and 6 months, but 8 (8.3%) among cases and 16 (8.3%) among controls were started below 4 months.
When starting the complementary feeding, children who took cow milk in both cases and controls were 34 (35%) and 71 (36.6%), respectively. Feeding the child by the bottle is 30 (30.9%) among cases and 31 (16%) among controls (Table 2). Most of the mothers among cases (85, 87.6%) and controls (165, 85.1%) wash their hands before feeding their children.
 |
Table 2 Comparison of Child Feeding and Caring Practices of SAM Children with and Without Edematous Malnutrition in Gedeo Zone, SNNPR June 2018 |
Health Service Utilization
ANC follow-ups were practiced in 20 (20.6%) of the mothers of cases and 146 (75.3%) of the mothers of control. Regarding deworming 40 (41.2%) of the cases and 68 (35%) of the controls were dewormed with in the past month. The majority of the cases (92, 94.9%) and controls (183, 94.3%) were vaccinated for their age, respectively. But only 32 (33%) among cases and 111 (57.2%) among controls were treated with measles vaccination (Table 3). Regarding vitamin A supplementation, 40 (41.2%) among cases and 131 (67.5%) among controls have taken oral vitamin A at least once.
 |
Table 3 Comparison of Health Service Utilization of SAM Children with and Without Edematous Malnutrition in Gedeo Zone, SNNPR June 2018 |
Sanitation, Hygiene and Childhood Illness
Concerning the morbidity status of the children, 63 (64.9%) of the cases and 80 (41.2%) of the controls had diarrhea 2 weeks before admission. Households that get water from protected spring are 76 (78.4%) among cases and 145 (74.7%) among controls (Table 4). The use of latrine was 79 (81.4%) households of the cases and 176 (90.7%) of the controls.
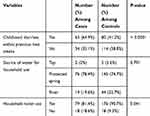 |
Table 4 Comparison of Sanitation, Hygiene and Childhood Illness of SAM Children with and Without Edematous Malnutrition in Gedeo Zone, SNNPR June 2018 |
Multivariable Analysis
Variables with P-value <0.25 in bivariate analysis were taken as candidates for multivariate analysis, which include are family size, educational status of the mother, educational status of the father, childhood diarrhea within the previous two weeks, ANC service utilization, vitamin A supplementation and household toilet use.
The variables that were significant in multiple logistic regression analysis were childhood diarrhea within the previous two weeks before admission and ANC utilization. A child who had diarrhea within the previous two weeks before admission was 2.83 (1.21–6.65) times more likely to develop edematous malnutrition than a child who had no diarrhea. Children whose mother has attended ANC during pregnancy in any frequency were 95% less likely to develop edematous malnutrition as compared to a child whose mother has not attended ANC at all (Table 5).
 |
Table 5 Significant Variables by MultivVariable Analysis to Edematous Malnutrition in Gedeo Zone, SNNPR June 2018 (Case =97, Control =194) |
Discussion
Malnutrition is one of the common causes of child death. This study revealed that having childhood diarrhea within the previous two weeks and ANC utilization of mothers during pregnancy were significant factors for edematous malnutrition.
The morbidity status of the child with diarrhea in the preceding two weeks before admission is significantly associated with edematous malnutrition of under-five children. Cases had more history of diarrhea than the controls. The odds of having nutritional edema in severely malnourished children are two times more in children who had diarrhea within the previous two weeks before admission as compared to their counterparts with no diarrhea. This result is supported by the study done in Kenya, Jomo Kenyata University that shows the child with diarrhea within the previous two weeks before the onset of edema was 2.54 times more likely to develop edematous malnutrition as compared to a child with no diarrhea.18 Another study done in Zambia indicated that the child with diarrhea two weeks before the onset of edema were 1.12 times more likely to develop edematous malnutrition than a child with no diarrhea.19 Also, a study done in southern Ethiopia (Damot Gale, Wolayita zone) indicated that a child with diarrhea within the previous two weeks before the onset was 39.5 times more likely to develop edematous malnutrition compared to a child with no diarrhea.20 Having diarrhea was highly significant to edematous malnutrition observed. This can be due to excessive loss of fluids and electrolytes, loss of appetite, lack of absorption of food in the intestine due to the high motility of the intestine during diarrhea episodes.
On the other hand, mothers not attending ANC during pregnancy have a strong association with edematous malnutrition in this study. It revealed that a child whose mother has attended ANC during pregnancy in any frequency were 95% less likely to develop edematous malnutrition as compared to a child whose mother has not attended ANC. This result supported by a study done in London that children whose mothers attented ANC during pregnancy are 43.6% times less likely to develop edematous malnutrition as compared to children whose mothers not attended ANC.13 Another study was done in Kombolcha children whose mothers attended ANC during pregnancy 11.9% times less likely to develop edematous malnutrition as compared to children whose mothers not attended ANC in any frequency.18 This can be due to when mothers attend ANC during pregnancy, they assess nutritional status. If mothers did not have good nutrition during pregnancy, it increases the risk of child edematous malnutrition afterbirth, so that antenatal visit is important to check the health status of both child and mother. ANC in the study setting is the care provided by skilled health-care professionals to pregnant women in order to ensure the best health conditions for both mother and baby during pregnancy. The components of ANC include risk identification, prevention and management of pregnancy-related or concurrent diseases, and health education and health promotion. ANC is provided during the first trimester of pregnancy.
Conclusion
Based on this study results, we can conclude that edematous malnutrition in under-five children was associated with ANC utilization and having childhood diarrhea within the previous two weeks.
Abbreviations
AOR, Adjusted odds ratio; CI, Confidence interval; ANC, Ante Natal Care; COR, Crude odds ratio; HC, Health center; MAM, Moderate acute malnutrition; OR, Odds Ratio; SAM, Severe acute malnutrition; SD, Standard deviation; SPSS, Statistical Package for the Social Sciences; SNNPR, Southern Nation Nationality and People's Region; WHZ, weight-for-height Z-score.
Ethics/Copyright
A written informed consent was taken from all caregivers, and this study is done in accordance with the Declaration of Helsinki.
Acknowledgments
The authors acknowledge Dilla University, Gedeo Zone Health Department, Wonago District and Yirgachefe District Health offices and all study participants for their cooperation.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Mr Terefe Yacob reports grants, personal fees from Dilla University during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. FANTA. Interim national guidelines for community-based management of severe acute malnutrition Ghana. 2010. Available from: https://www.fantaproject.org/countries/ghana/interim-national-guidelines-cmam.
2. WHO and UNICEF. Child growth standards and identification of severe acute malnutrition in infants and children: a joint statement by the World Health Organization and the United Nations Children's Fund. 2009. Available from: https://apps.who.int/iris/bitstream/handle/10665/44129/9789241598163_eng.pdf;jsessionid=1A3B3FBD31C8976FC94AEA30E5EEFB84?sequence=1.
3. Desormeaux J. The revitalization of the community-based management of acute malnutrition program in Haiti. 2015. Available from: https://scholarworks.gsu.edu/iph_theses/379/.
4. Ahmed T, Rahman S, Cravioto A. Oedematous malnutrition. International centre for diarrhoeal disease research, Bangladesh. Indian J Med Res. 2009;130(5):651–654.
5. Abebaw M, wanzahun G, Meseret G, Feleke G. Determinants of acute malnutrition among under-five children in Karat town public health facilities, Konso district, southern Ethiopia: a case control study. Qual Prim Care. 2017;25(4):242–252.
6. WHO. Essential nutrition actions: improving maternal, newborn, infant and young child health and nutrition. 2013 Available from: https://www.who.int/nutrition/publications/infantfeeding/essential_nutrition_actions.pdf.
7. Black RE, Victora CG, Walker SP, . Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;51:382–427.
8. Currie J, Almond D. Capital development before age five. Handbook of labor economics. Pharmaceuticals2011;4:1315–1486. doi:10.3390/ph4101315
9. Dewey KG, Begum K. Long-term consequences of stunting in early life. Matern Child Nutr. 2011;7:5–18. doi:10.1111/mcn.2011.7.issue-s3
10. UNICEF, WHO and World Bank. Joint Child Malnutrition Estimates Levels and Trends; 2012. doi:10.1094/PDIS-11-11-0999-PDN
11. UNICEF. Improving child nutrition: the achievable imperative for global progress. 2013. Available from: https://www.unicef.org/publications/index_68661.html.
12. UNICEF. Children and the Millennium Development Goals. Progress for Children a Report Card on Nutrition; 2007. doi:10.1094/PDIS-91-4-0467B
13. Frison S, Checchi F, Kerac M. Omitting edema measurement: how much acute malnutrition are we missing? Am J Clin Nutr. 2015;102(5):1176–1181. doi:10.3945/ajcn.115.108282
14. UNICEF. Tracking progress on child and maternal nutrition: a survival and development priority. 2009. Available from: https://www.unicef.org/publications/index_51656.html.
15. UNICEF, WHO, World Bank, UN Population Division. Levels and Trends in Child Mortality; 2012. doi:10.1094/PDIS-11-11-0999-PDN
16. Park SE, Kim S, Ouma C, Loha M, Wierzba TF, Beck NS. Community management of acute malnutrition in the developing world. Pediatr Gastr Nutr. 2012;15(4):210–219. doi:10.5223/pghn.2012.15.4.210
17. Roberfroid D, Hammami N, Mehta P, . Management of Oedematous Malnutrition in Infants and Children Aged >6 Months: A Systematic Review of the Evidence. Geneva, Switzerland: World Health Organization (WHO); 2013. Available from: https://biblio.ugent.be/publication/5700347.
18. Zewdie T, Abebaw D. Determinants of child malnutrition: empirical evidence from Kombolcha District of Eastern Hararghe Zone, Ethiopia. J Int Agric. 2013;52(52 4):357–372.
19. Selestine H, Seter S, Olusegun B, Peter S, Adamson SM, Emmanuel R. Demographic, cultural and environmental factors associated with frequency and severity of malnutrition among Zambian children less than five years of age. J Public Health Epidemiol. 2011;3(8):362–370.
20. Abera L, Dejene T, Laelago T. Prevalence of malnutrition and associated factors in children aged 6–59 months among rural dwellers of Damot Gale district, South Ethiopia. Int J Equity Health. 2017;16:111. doi:10.1186/s12939-017-0608-9
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
