Back to Journals » Clinical Ophthalmology » Volume 16
Descriptive Analysis of Footplate Position After Myopic Implantable Collamer Lens Implantation Using a Very High-Frequency Ultrasound Robotic Scanner
Authors Zaldivar R , Zaldivar R, Adamek P, Quintero G, Cerviño A
Received 12 October 2022
Accepted for publication 17 November 2022
Published 5 December 2022 Volume 2022:16 Pages 3993—4001
DOI https://doi.org/10.2147/OPTH.S393223
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Roger Zaldivar,1 Roberto Zaldivar,1 Pablo Adamek,1 Gabriel Quintero,1 Alejandro Cerviño2
1Instituto Zaldívar, Mendoza, Argentina; 2Department of Optics & Optometry & Vision Sciences, University of Valencia, Valencia, Spain
Correspondence: Alejandro Cerviño, Department of Optics & Optometry & Vision Science, University of Valencia, C / Dr. Moliner, 50. Burjassot, Valencia, 46100, Spain, Tel +34 963 544 852, Email [email protected]
Purpose: To assess the position of the haptics of the implantable collamer lens (ICL) in myopic eyes using a high-frequency ultrasound robotic scanner.
Methods: This was a prospective, single-arm, observational study carried out at the Instituto Zaldivar SA (Mendoza, Argentina) in a sample of 52 eyes who have been submitted to successful ICL implantation prior to enrollment. Images of the eyes were obtained using a very-high frequency digital ultrasound robotic scanner (VHFDU) to establish the position of the ICL in the posterior chamber and its relation to the ciliary sulcus. New parameters for lens position analysis were also described.
Results: In 81% of cases (42 eyes), the ICL rests on the ciliary body (CB) in both temporal and nasal sides, being slightly lower than 6% (3 eyes) those that rest on the sulcus in both sides, with significant correlations between ICL position and vault values (p< 0.05). Cases in which the ICL position was CB-CB yielded central vault values across the whole range determined within the sample, but most of the eyes where the ICL rests on both the sulcus in one side and the CB in the other yield greater central vault values. Correlation was significant between ICL position and retroposition distance on the temporal side (Spearman’s rho − 0.487, p< 0.001). A significant but weaker correlation was also found between ICL position and retroiridian space (p< 0.05).
Conclusion: ICL for myopia footplates tend to locate outside of the sulcus in a significant percentage of patients after successful implantation. VHFDU assessment in eyes implanted with an ICL to properly study the lens footplate position and posterior anatomical relations provides important additional information besides post-surgery vault.
Keywords: myopia, implantable collamer lens, ultrasound biometry, high-frequency, ciliary sulcus
Introduction
Phakic intraocular lenses (pIOL) have been extensively used for the correction of different degrees of myopia and astigmatism. Specifically, one of the most widely pIOL used is the Implantable Collamer Lens (ICL, Staar Surgical Inc, Monrovia, CA, USA), which has shown stable visual and refractive outcomes and low adverse event rates with their central port designs.1–3 One of the most important parameters to be assessed when this lens is implanted is the measurement of the lens vault. ICL size choice, usually based on preoperative measurements such as white-to-white (WTW) and anterior chamber depth (ACD), is critical to avoid low or high vault values.
Among these measures, sulcus-to-sulcus (STS) distance seems to be a critical measure for ICL size selection, and can be performed using high-resolution ultrasound biomicroscopy (UBM), enabling a more reliable ICL vault assessment compared to conventional WTW measurements.4,5 UBM can provide valuable anatomical information allowing detailed assessment of ICL when implanted and imaging of the ciliary body.6 This instrument allows a comprehensive evaluation of the ICL position, including optical zonal, bilateral haptics and its relationship to other structures such as the iris, the crystalline lens, zonules and the ciliary body. In this sense, many authors have evaluated the anatomical position of the ICL and its relationship to adjacent ocular structures using different UBM devices, with conflicting results.7–10
Thus, given the heterogeneity of the description provided by previous studies on the ICL position, the aim of the present study was to further explore and describe the position of the haptics of ICLs for myopia using a very high-frequency digital ultrasound robotic scanner (VHFDU) after successful ICL implantation, and propose new metrics that could be useful for position analysis.
Methods
This study included 52 eyes from 33 patients (mean age of 31±5 years old, ranging from 22 to 42) with myopia (24 female) who were implanted with an ICL for myopia at the Instituto Zaldivar (Mendoza, Argentina) between 2013 and 2022. The V4c model ICL was implanted in all eyes with sizes of 12.60 (4% of cases), 13.20 mm (78.7% of cases) and 13.70 mm (17.3%). Descriptive statistics of the sample are summarized in Table 1. The study was approved by the Ethical Review Board of the Institute and adhered to the tenets of the Declaration of Helsinki.
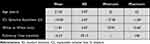 |
Table 1 Descriptive Statistics of the Sample Included in the Study |
Inclusion criteria comprised patients submitted to successful ICL implantation surgery for myopia, with or without associated astigmatism. Patients with previous eye surgeries were not included in the analysis. Preoperative measures included uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction spherical equivalent (MRSE), slit-lamp biomicroscopy and intraocular pressure measurement. WTW and ACD were determined with a slit-scanning tomography system (Orbscan II, Bausch & Lomb).
Implantable Collamer Lens (ICL)
The Visian ICL is a phakic lens made from collamer, a flexible, hydrophilic and biocompatible material with a plate-haptic design and a central convex/concave optical zone. ICL lenses are foldable, allowing for posterior chamber injection through a microscopic incision of 3.5 mm or smaller. When properly placed, the ICL should be positioned completely within the posterior chamber between the iris and crystalline lens with support on the ciliary sulcus. The V4c model ICL includes a central hole (diameter 0.36 mm) to increase aqueous humour perfusion and reduce the risk of secondary cataract.
Surgical Procedure
The Visian ICL (STAAR Surgical, Nidau, Switzerland) V4c model for myopia was used. Toric ICL and Bioptic technique (sequential or delayed) were performed in eyes with significant astigmatism. In those with mild astigmatism, Limbal Relaxing Incisions (LRI) were carried out. All the ICLs in the sample analyzed were implanted along the horizontal axis. Topical anesthesia was used in all the surgeries, which were carried out by the same experienced surgeon (RZ). WTW was manually determined under the microscope before surgery to confirm previous measures obtained with the topographer. In toric ICL implantation cases, a technician marked the references for proper axis placement at slit lamp once in the operating room (OR). A temporal main incision of 3.2 mm and just one paracentesis at 8 or 2 o’clock were performed for drug delivery. Intracameral phenylephrine 1.5% and lidocaine 1% were injected to achieve pupil dilatation and avoid pain. Ophthalmic viscosurgical device (OVD) (Ocucoat®– 2% hydroxypropyl methylcellulose solution by Bausch and Lomb) and the ICL were injected into the anterior chamber using the manufacturer injector cartridge. An OVD reinforcement was necessary before the four haptics were tucked under the iris through the main incision with the help of the Zaldivar ICL Manipulator® (Asico LLC, Westmont, IL, USA). Finally, OVD was removed using a coaxial irrigation aspiration, moxifloxacine 2% was injected and wounds were gently hydrated. Intracameral miotics were not used in any case. After surgery, a single acetazolamide 250 mg tablet was orally administered to decrease intraocular pressure. Antibiotic (Vigamox® moxifloxacine 5 mg/mL), corticosteroid (Pred Forte® Prednisolone Acetate 10 mg/mL) and anti-inflammatory (Nevanac® Nepafenac 1 mg/mL) were administered topically 4 times a day for 1 week and then progressively reduced for 1 month. Topical ocular hypotensive (Alphagan®P Brimonidine 0.2%) was also applied twice for 1 month.
Position Metrics
The ArcScan Insight 100 (ArcScan Inc. Golden, Colorado) VHFDU was used postoperatively to determine lens haptic and footplate position, as well as several other metrics. This instrument has been shown repeatable and accurate for imaging and measurements in the anatomy of the eye, particularly for precision imaging behind the iris for better ICL sizing.9–12
The VHFDU device was operated by an experienced examiner. Topical anesthesia was obtained by instillation of Proparacaine prior to measurement acquisition. Participants were sitting upright, with undilated pupils, and looking at a fixation light to get pupil centration. A correct adjustment of the device against the patient’s eye is important as the receptacle is filled with balanced saline solution (BSS). Several scans were obtained from each participant to ensure visibility of structures and allow determination of ICL position and metrics.
The metrics included ICL vault at the center, temporal and nasal. Both temporal and nasal vault were determined at the edge of the ICL optical zone. Also, the retroposition distance, defined as the distance parallel to the optical axis from the iris pigment epithelium to the anterior surface of the lens as close to the ciliary body as possible, was measured both nasally and temporally. The retroiridian space, defined as the distance parallel to the optical axis, and tangent to the ciliary body, from the iris pigment epithelium to the anterior zonule, was also measured both nasally and temporally. Figure 1 displays both the retroposition (A) and retroiridian space (B) metrics on an image as an example.
 |
Figure 1 Image description of retroposition distance (A) and retroiridian space (B) metrics measured with the ArcScan Insight 100 VHFDU. |
The ICL haptic and footplate position was determined by assessing the location of the ICL edge with respect to the eye sulcus in both nasal and temporal side (Figure 2). According with this observation, the positioning was classified as:
- Sulcus–sulcus (S-S): both sides of the lens are resting on the sulcus.
- Ciliary body–ciliary body (CB-CB): both sides of the lens are resting on the ciliary body.
- Sulcus–ciliary body or ciliary body–sulcus (S-CB or CB-S): one of the sides rests on the sulcus while the other one rests on the ciliary body.
 |
Figure 2 Images showing the ICL plate resting on the sulcus (A) and the ciliary body (B). |
Data Analysis
Descriptive statistics were used to quantitatively summarize data using mean values, standard deviations and range. Non-parametric Spearman correlation analysis was carried out to assess the relationship between ICL position and the different metrics determined. Boxplots were also obtained to represent the distribution of the metrics values for the different ICL positions observed. Statistical analysis was carried out using SPSS v25.0 (SPSS Inc., Chicago, IL, USA) and Microsoft Excel for Mac v16.41 (Microsoft Co., Redmond, WA, USA). Significance level was set at p<0.05.
Results
In almost 81% of cases (42 eyes), the ICL rests on the ciliary body in both temporal and nasal sides, being slightly lower than 6% (3 cases) those that rest on sulcus in both sides. Out of the 7 cases (13%) in which the ICL rests on the ciliary body in one side and the sulcus in the other, in 5 of them it was the temporal side the one that rested on the sulcus. Seventeen eyes out of the 52 had a toric lens implanted, however no relationship was found with footplate position. Non-parametric correlation analysis shows significant correlations between ICL position and vault values (Spearman’s rho values were 0.425, 0.305 and 0.527 for central, nasal and temporal vault values, respectively, with p-values of 0.002, 0.028 and <0.001, respectively). Table 2 shows the descriptive statistics of the metrics obtained from the ArcScan Insight 100. Figure 3 shows the frequency distribution of the different ICL positions across the sample.
 |
Table 2 Descriptive Statistics of the Metrics Obtained from the ArcScan Insight 100 VHFDU |
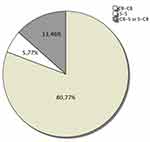 |
Figure 3 Pie chart depicting the frequencies, as percentage, of each of the ICL positions found in the sample. |
Cases in which ICL position was CB-CB yielded central vault values across the whole range determined within the sample, and no difference can be seen against those with S-S position, but most of the eyes where the ICL rests on both the sulcus in one side and the ciliary body in the other yield greater central vault values compared to those where the ICL rests on the ciliary body in both sides. Correlation was also significant between ICL position and the retroposition distance, from the iris to the ICL, on the temporal side (Spearman’s rho −0.487, p<0.001). Figure 4 displays the boxplot distribution of central vault values measured according to ICL position.
 |
Figure 4 Boxplot distribution of central vault values measured for the different ICL positions. |
Figure 5 displays the boxplot distribution of the retroiridian space for the eyes with different ICL positioning, showing that most of the eyes where the ICL rests on the ciliary body, the distance is greater than in those cases where the lens rests on the sulcus or combining sulcus and ciliary body. A significant but weaker correlation was also found between ICL position and retroiridian space (Spearman’s rho values were −0.334 and −0.290 for nasal and temporal values, with p-values of 0.015 and 0.037, respectively).
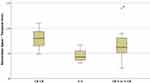 |
Figure 5 Boxplot distribution of temporal retrodistance for the different ICL positions. |
Discussion
The ideal phakic position should have the optical zone centered on the pupil, and both haptics on the sulcus while maintaining a vault value within the ideal range (250−750 μm), which is commonly found in the numerous clinical studies published to date although values vary broadly across studies (see Montés-Micó et al for a review).3
The in vivo positional analysis of the ICL has been previously studied using different devices. Elshafei et al7 in 2016, after analyzing 142 myopic eyes using the Paradigm UBM (Paradigm Medical Industries, Salt Lake City, UT, USA), found that the lens haptics could be imaged resting in the ciliary sulcus in 78.87% of eyes and at least one haptic rested on the lens periphery and zonules in 21.12% of eyes. They described that the overall iris configuration was flat in 62.76% of eyes with central anterior convexity in at least one quadrant in 28.87% of eyes and peripheral iris bombe in at least one quadrant in 8.45% of eyes. They also found that the contact between the ICL and the posterior surface of the iris was present in all eyes and considered that this contact was unrelated to increased vault. This contact was limited to the central third of the iris in 78 eyes and extended more peripherally in 64 eyes. In another study carried out by Zhang et al8 in 2018 using the Compact Touch STS UBM (Quantel Medical, France) in a sample of 72 high myopes (134 eyes) submitted to ICL implantation, they reported a high variability in lens position, with footplates in the ciliary sulcus in 21.6% of cases, on top of the ciliary body in 2.2% of cases, in the ciliary process in 12.7% of cases, under the ciliary body in 10.4% of cases, and into the ciliary body in 32.1% of cases. They found that although the haptics located on various positions postoperatively, almost each group vault with different positions of the haptics was within normal range, with more than half of the eyes (64.9%) displaying an ideal vault value. They also noticed that the inappropriate location of the haptics (not in ciliary sulcus) might be one of the factors influencing the vault values by observing the position of the ICL and haptics by means of recording UBM images in various situations.
Reinstein et al9, using the Arscan Insight100 VHFDU, analyzed the position of the footplate on a sample of 30 eyes 3 months after ICL implantation. They reported the footplates as resting just anterior to the zonules flexing up toward the sulcus (zonule position) in 48.3% of cases, inserted into the ciliary body in 49.2%, and inserted directly into the sulcus in 2.5% of cases. They indicated that the VHFDU enabled them to ensure that in the physiological state, there was no contact between the ICL and the crystalline lens in any eye, including for very high myopic ICL lenses where the thickest ICL portion is in the mid-periphery behind the iris and thus invisible to OCT B-scan imaging. As indicated the anatomical placement of the footplates may play a role on the variability of lens vault for a particular eye. As shown by Zhang et al.8 ICLs could have a combination of ≥2 of positions (ie one footplate in on top and one footplate under the ciliary body), and Reinstein et al9 found 6 eyes (20%) to have this combination. They suggested that may be reasonable to consider that a higher ICL vault would be associated with more anterior insertion. This is discussed by the same authors, indicating that the final resting position of the ICL is another variable likely to be adding to the noise of vault prediction.10
VHFDU assessment carried out in the present study allowed the direct observation of the ICL in situ and the analysis of the footplate position across the horizontal meridian. The classification suggested according to the footplate position was described considering the position on both footplates across the horizontal meridian, and considering the lack of objective landmarks, into the sulcus on both sides, the ciliary body on both sides, or mixed. The most remarkable finding was that less than 6% of eyes (3 cases) had the ICL footplates resting on the sulcus on both sides, considering that all surgeries analyzed were clinically successful. Also, two parameters were introduced in the present study, the retroposition distance and the retroiridian space. The first quantifies the position of the lens from anatomical structures, which might be useful for in situ assessment of ICL position. The second parameter would define an anatomical metric that could be useful for determining ocular characteristics influencing footplate position after ICL implantation and could, therefore, be potentially useful for future ICL sizing calculation using VHFDU-determined metrics. Significant correlations were found between these new metrics and footplate position. Given the low number of cases in which the footplates were located at the sulcus, further studies analyzing ICL position in larger samples of eyes across the refractive spectra including these new parameters would be needed in order to determine which anatomical parameters as determined by VHFDU would be useful for newer and more precise lens sizing calculations. This would allow increasing current knowledge on what to expect regarding ICL positioning in successful ICL implantation depending on the patient characteristics. The use of intraoperative optical coherence tomography13–16 to check the vault and angle anatomy during the surgery might help achieving more consistent ICL positioning.10
One limitation of the present analysis is the possible impact of including both eyes in most of the patients. In fact, out of the 3 eyes that had the expected S-S footplate position, 2 correspond to the same patient, highlighting even more the low incidence of cases in which the lens is located at the expected position. Further analysis over larger samples of eyes, and covering the different refractive error ranges, would also allow specifying landmarks on the images provided by VHFDU systems and describe a more detailed objective classification of footplate position.
Conclusions
ICL for myopia footplates tend to locate outside of sulcus in a significant percentage of patients after successful implantation. Analysis of large cohorts of patients with VHFDU are needed to further explore the reasons behind it. The use of VHFDU in eyes implanted with ICL to properly study the lens footplate position and posterior anatomical relations provides important additional information besides post-surgery vault, particularly in those eyes with low and excessive values.
Abbreviations
ICL, Implantable collamer lens; VHFDU, Very high-frequency digital ultrasound robotic scanner; OVD, Ophthalmic viscosurgical device; S, Sulcus, CB, Ciliary body.
Data Sharing Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted according to the tenets of the Declaration of Helsinki. This study was approved by the Institutional Review Board of the Instituto Zaldivar. Informed consent was obtained from all the patients prior to enrollment.
Acknowledgments
The authors would like to thank Dr. Gastón Rodríguez-Granillo for the useful feedback and helpful comments and suggestions for the preparation of the manuscript.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was performed at the Instituto Zaldivar. No external funding was received for this work.
Disclosure
Prof. Alejandro Cerviño declares research and consulting contracts with AST Products Inc. and Essilor International SA. Dr. Roger Zaldivar declares research and consulting contracts with Staar Surgical. The rest of the authors declare that they have no competing interests. None of the authors has a proprietary or financial interest in any of the instruments mentioned.
References
1. Packer M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clin Ophthalmol. 2016;10:1059–1077. doi:10.2147/OPTH.S111620
2. Packer M. The implantable collamer lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427–2438. doi:10.2147/OPTH.S188785
3. Montés-Micó R, Ruiz-Mesa R, Rodríguez-Prats JL, Tañá-Rivero P. Posterior-chamber phakic implantable collamer lenses with a central port: a review. Acta Ophthalmol. 2021;99:288–301. doi:10.1111/aos.14599
4. Choi KH, Chung SE, Chung TY, Chung ES. Ultrasound biomicroscopy for determining visian implantable contact lens length in phakic IOL implantation. J Refract Surg. 2007;23:362–367. doi:10.3928/1081-597X-20070401-08
5. Kojima T, Yokoyama S, Ito M, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153(4):632–7, 7 e1. doi:10.1016/j.ajo.2011.06.031
6. Warjri GB, Senthil S. Imaging of the Ciliary Body: a Major Review. Semin Ophthalmol. 2022;37(6):711–723. doi:10.1080/08820538.2022.2085515
7. Elshafei AM, Genaidy MM, Moharram HM. In vivo positional analysis of implantable collamer lens using ultrasound biomicroscopy. J Ophthalmol. 2016;2016:4060467. doi:10.1155/2016/4060467
8. Zhang X, Chen X, Wang X, Yuan F, Zhou X. Analysis of intraocular positions of posterior implantable collamer lens by full-scale ultrasound biomicroscopy. BMC Ophthalmol. 2018;18(1):114. doi:10.1186/s12886-018-0783-5
9. Reinstein DZ, Vida RS, Archer TJ. Visual outcomes, footplate position and vault achieved with the visian implantable collamer lens for myopic astigmatism. Clin Ophthalmol. 2021;15:4485–4497. doi:10.2147/OPTH.S330879
10. Reinstein DZ, Archer TJ, Vida RS, Piparia V, Potter JG. New sizing parameters and model for predicting postoperative vault for the implantable collamer lens posterior chamber phakic intraocular lens. J Refract Surg. 2022;38(5):272–279. doi:10.3928/1081597X-20220302-01
11. Reinstein DZ, Archer TJ, Silverman RH, Coleman DJ. Accuracy, repeatability, and reproducibility of Artemis very high-frequency digital ultrasound arc-scan lateral dimension measurements. J Cataract Refract Surg. 2006;32:1799–1802. doi:10.1016/j.jcrs.2006.07.017
12. Reinstein DZ, Archer TJ, Silverman RH, Rondeau MJ, Coleman DJ. Correlation of anterior chamber angle and ciliary sulcus diameters with white-to-white corneal diameter in high myopes using Artemis VHF digital ultrasound. J Refract Surg. 2009;25:185–194.
13. Titiyal JS, Kaur M, Sahu S, Sharma N, Sinha R. Real-time assessment of intraoperative vaulting in implantable collamer lens and correlation with postoperative vaulting. Eur J Ophthalmol. 2017;27:21–25. doi:10.5301/ejo.5000818
14. Torbey J, Mehanna CJ, Abdul Fattah M, Awwad ST. Comparison of intraoperative vs postoperative optical coherence tomography measurement of implantable collamer lens vaulting. J Cataract Refract Surg. 2020;46(5):737–741. doi:10.1097/j.jcrs.0000000000000119
15. Zaldívar R, Adamek P, Zaldívar R, Domínguez MS, Cerviño A. Intraoperative versus postoperative vault measurement after implantable collamer lens implantation in a large cohort of patients. J Refract Surg. 2021;37(7):477–483. doi:10.3928/1081597X-20210405-03
16. Zaldivar R, Zaldivar R, Adamek P, Cerviño A. Intraoperative adjustment of implantable collamer lens vault by lens rotation aided by intraoperative OCT. J Cataract Refract Surg. 2022;48(9):999–1003. doi:10.1097/j.jcrs.0000000000000915
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
