Back to Journals » Clinical Ophthalmology » Volume 17
Visual Acuity Improvement in Low, Moderate and High Myopia After Posterior-Chamber Phakic Implantable Collamer Lens Surgery in a Large Patient Cohort
Authors Zaldivar R , Zaldivar R, Gordillo CH, Adamek P
Received 7 February 2023
Accepted for publication 11 April 2023
Published 18 April 2023 Volume 2023:17 Pages 1179—1185
DOI https://doi.org/10.2147/OPTH.S407492
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Roger Zaldivar, Roberto Zaldivar, Carlos H Gordillo, Pablo Adamek
Surgery Department, Instituto Zaldivar, Mendoza, Argentina
Correspondence: Roger Zaldivar, Instituto Zaldivar, Av. Emilio Civit 701, Mendoza, Argentina, Email [email protected]
Purpose: To compare best-corrected visual acuity (BCVA) before and after implantable collamer lens (ICL) surgery in patients with low, moderate and high myopia.
Methods: A single-centre, prospective, registry-based study involving patients with myopia who received ICLs between October 2018 and August 2020. The study population was divided into three groups of subjects with low (from 0 to − 6 D), moderate (− 6 to − 10 D) and high myopia (more than − 10 D). We analysed uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), spherical equivalent (SE), differences between BCVA pre- and 1-month postoperative, and line gain in BCVA 1 month after surgery.
Results: A total of 770 eyes belonging to 473 patients were surgically intervened during the study period, of which 692 eyes completed 1 month of postoperative follow-up and were included in the study population. At 1-month follow-up, 478 eyes (69%) achieved a BCVA of 20/20, 599 (87%) obtained 20/25 or better, and 663 (96%) had a BCVA of 20/40 or better. We identified a significant improvement in BCVA (baseline 0.15± 0.2 logMAR vs follow-up 0.07± 0.2 logMAR, p< 0.0001) and a significant reduction in SE (baseline − 9.23± 4.1 D, vs follow-up − 0.21± 0.8 D, p< 0.0001), with a significant relationship between preoperative SE and line gain (r = − 0.46, p< 0.0001). We identified a significantly higher line gain among eyes with higher degrees of myopia (low myopia 0.22± 0.69 lines compared to moderate myopia 0.56± 1.1 lines and high myopia 1.51± 1.9 lines, p< 0.0001). Notably, 99.6% of eyes with a high grade of myopia achieved improvement to a low degree (less than − 6 D) at follow-up. The safety and efficacy indexes were 0.083± 0.1 and − 0.001± 0.1, respectively.
Conclusion: In this large patient cohort, ICL surgery was related to a significant line gain in BCVA, particularly among eyes with higher degrees of myopia.
Keywords: myopia, implantable collamer lens, visual acuity, phakic intraocular lens, refractive surgery
Introduction
Of the surgical options for the treatment of patients with low-to-moderate myopia, superficial cornea operations, such as laser-assisted in-situ keratomileusis (LASIK) and photorefractive keratectomy (PRK).1–3 More recently, the introduction of small incision lenticule extraction (SMILE) has been shown to correct higher dioptre myopia;4,5 however, correcting high degrees of myopia using corneal refractive surgery can also increase the future risk of corneal ectasia.6–8 Posterior-chamber phakic implantable collamer lenses (ICLs) have emerged as an effective treatment for patients with high myopia and no significant complications, especially since the incorporation of the central hole in the V4c model.9 A recent literature review highlighted the good refractive and visual results obtained with the new V4c model of ICLs. Another excellent surgical treatment option for refractive errors is the Bioptic technique. This one was developed by one of our main authors and combine posterior ICL implantation for myopia correction and LASIK for residual myopia or astigmatism correction.10,11
However, patients with high degrees of myopia generally also have severe amblyopia and often benefit from surgery to correct the ametropia, with a greater than expected line gain and a pre- to postoperative improvement in best-corrected visual acuity (BCVA).12,13 These young patients with high myopia, sometimes accompanied by severe amblyopia, therefore represent the main candidates for ICL surgery. Furthermore, given the good safety outcomes observed with ICLs, they are an excellent indication for patients with low or moderate myopia and contraindications for corneal refractive surgery, such as medium or severe dry eye syndrome, thin cornea and subclinical keratoconus, among others.14–17 A growing number of patients with low and moderate myopia are consequently being indicated ICLs, even though their efficacy in terms of postoperative vision gain has not been proven conclusively. And to the best of our knowledge, no studies have been published to date that have explored the relationship between the degree of myopia and BCVA gain obtained from ICL surgery. As such, the aim of this study was to compare the refractive outcomes and line gains in patients with low, moderate and high myopia after they had received a phakic implantable collamer lens, model V4c.
Methods
This prospective, registry-based, observational study included all consecutive patients who received ICL surgery for myopia, with or without astigmatism, at our centre (Instituto Zaldivar, Mendoza, Argentina) between October 2018 and August 2020. Only patients with at least two full postoperative follow-ups completed at 24 hours and 1 month, plus a record of their different visual acuities were included. All patients with a history of eye diseases other than myopia and astigmatism or prior eye surgery were excluded. This observational study was approved by the institute’s ethics committee and met the requirements of the Declaration of Helsinki.
Pre- and Postoperative Measurements
Prior to the operation, we performed slit-lamp biomicroscopy and dilated eye fundus examinations, and measured the patients’ uncorrected visual acuity (UCVA), BCVA, manifest spherical equivalent refractive error (SE) and intraocular pressure (IOP) (using a Goldmann tonometer). We also measured their white-to-white (WTW) distances and anterior chamber depths (ACD) from the endothelium, the latter with an Orbscan II topography (Bausch & Lomb, Orbtek Inc., USA). In follow-up, we measured the UCVA, BCVA, SE, IOP and carried out a slit lamp examination at 1 day and 1 month postoperative.
Implantable Collamer Lens (ICL)
This study used the Visian ICL V4c model (STAAR Surgical, Monrovia CA, USA) for myopia. A toric ICL implant or the bioptics technique (sequential or delayed) was performed in eyes with significant astigmatism. Limbal relaxing incisions were applied in eyes with mild astigmatism. All the ICLs in the sample were implanted along the eye’s horizontal axis. ICLs are phakic lenses made from collamer, a flexible, hydrophilic and biocompatible material, and have a plate-haptic design and central convex/concave optical zone. ICLs can be folded and, therefore, then inserted in the posterior chamber via a corneal incision of 3.5 mm or less. When placed correctly, the ICL should be positioned entirely within the posterior chamber, between the iris and crystalline lens, resting on the ciliary sulcus. The ICL V4c model incorporates a central hole (0.36 mm in diameter) to increase aqueous humour perfusion and reduce the risk of secondary cataract.
Surgical Procedure
The same experienced surgeon (RZ) performed all the implants using topical anaesthesia. In the case of toric ICLs, a technician marked the points of reference on the slit lamp to help align the ICL correctly in the corresponding eye during surgery. A main incision of 3.2 mm was made on the temporal side and a paracentesis placed at 8 or 2 o’clock to administer medications. Intracameral phenylephrine (1.5%) and lidocaine (1%) were injected to dilate the pupil and avoid any pain. A viscoelastic solution (OcuCoat®, 2% hydroxypropylmethylcellulose solution; Bausch & Lomb) was injected, then the ICL was introduced into the anterior chamber using the manufacturer’s injector cartridge. Viscoelastic solution had to be administered for reinforcement before positioning the four haptics beneath the iris via the main incision with the aid of a Zaldivar ICL® Manipulator (Asico LLC, USA). Finally, the viscoelastic solution was withdrawn using coaxial irrigation/aspiration, 2% moxifloxacin injected and the incisions gently hydrated. Intracameral miotic agents were not used in any of the interventions. After the surgery, patients were given one acetazolamide 250 mg tablet, taken orally, to reduce the intraocular pressure. An antibiotic (moxifloxacin 5 mg/mL), corticosteroid (prednisolone acetate 10 mg/mL) and anti-inflammatory (nepafenac 1 mg/mL) were administered topically four times a day for 1 week and then reduced progressively over the next month. A topical ocular hypotensive agent (brimonidine 0.2%) was also applied twice daily for 1 month.
Definitions of Results and Between-Group Differences
The treated eyes were divided into three groups for analysis based on their preoperative SE values: low myopia (SE of 0 to −6.00 D), moderate myopia (SE of −6.00 to −10.00 D) and high myopia (SE of greater than −10 D). We used the line gain (LG), defined as the difference between each patient’s pre- and postoperative BCVA scores, in addition to the visual outcomes and postoperative SE values, to compare the results between groups. The safety (preoperative BCVA – postoperative BCVA) and efficacy indices (preoperative BCVA – postoperative UCVA) were also calculated for the overall sample. For a better analysis, the UCVA and BCVA were measured in an ophthalmologist’s office using a Snellen chart and converted to LogMAR for their statistical analysis.
Statistical Analysis
Continuous variables are reported as means ± standard deviation, while categorical variables are reported as frequencies and percentages. Between-group comparisons were carried out using paired Student’s t-test, one-way analysis of variance (ANOVA) for continuous variables and the chi-square test for categorical variables. The relationship between the preoperative SE values and line gain in BCVA was evaluated with Pearson’s correlation coefficient. Bland–Altman plots were used to express the relationship between line gain and baseline myopia. All analyses were performed with SPSS version 22.0 (Armonk, USA) software.
Results
A total of 770 myopic eyes belonging to 473 patients underwent ICL surgery between October 2018 and August 2020, of which 692 eyes (429 patients) were still in follow-up at 1 month and were included in the study. The patients included in the study had a mean age of 30.9±5.8 years.
The mean baseline UCVA was 1.69±0.4 logMAR, which, as expected, improved after the intervention to 0.15±0.2 logMAR (p<0.0001). We also observed a significant improvement in BCVA at 1-month postoperative (baseline 0.15±0.2 logMAR vs 30-days postoperative 0.07±0.2 logMAR, p<0.0001), with a mean line gain in BCVA of 0.83±1.4 (see Table 1). As expected, we identified a significant reduction in SE at the 1-month follow-up (baseline −9.23±4.1 D vs 30-days postoperative −0.21±0.8 D, p<0.0001). With respect to the refractive results stratified to the 1-month follow-up, 478 eyes (69%) achieved a BCVA of 20/20, 599 (87%) had 20/25 or better, and 663 (96%) obtained 20/40 or better; notably, the number of eyes with a BCVA of 20/20 increased from 42% preoperatively to 69% at 1 month.
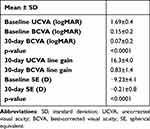 |
Table 1 Visual Acuity and Refractive Outcomes at Baseline and 1-Month Postoperative |
Furthermore, we identified a significant correlation between the preoperative SE values and the difference between pre- and postoperative BCVA (line gain) (r= −0.46, p<0.0001). The Bland–Altman plot highlights the greater line gain in eyes with a poorer preoperative BCVA (Figure 1).
 |
Figure 1 Bland–Altman plot illustrating the greater line gain among eyes with a higher baseline best-corrected visual acuity (BCVA). |
After dividing the sample into groups according to the baseline degree of myopia, we found a greater line gain among eyes with higher myopia. Specifically, the gain was 0.22±0.69 for the low myopia group, 0.56±1.1 for moderate and 1.51±1.9 for the high myopia group (p<0.0001), with 328 eyes (47%) showing an improvement on their baseline BCVA, 335 (48%) no change and only 29 (4%) were worse (Figure 2).
 |
Figure 2 Line gain according to baseline spherical equivalent (SE, in dioptres). |
Regarding the safety and efficacy indices, the former was 0.083±0.1 and the latter −0.001±0.1. We did not record any intraoperative complications or lens explantations or rotations in our sample throughout the 1-month follow-up period. Nor were there any cases of cataracts, pigment dispersion glaucoma, pupillary block or any other complications related to the ICL implant throughout the postoperative follow-up.
Discussion
Considering the given aim of the study, the main finding of our analysis was the significant line gain demonstrated by myopic patients after receiving phakic ICLs, with eyes with the highest levels of myopia obtaining the greatest benefit. It is worth noting that in a large cohort of patients implanted with phakic ICLs to treat myopia, besides the foreseeable improvements in SE and UCVA achieved with this type of intervention, we observed a vision line gain above all in eyes with higher preoperative SE values and worse BCVA scores. However, we must also consider the different anatomical characteristics of eyes with high and low myopia, for example in the fundus characteristics of high myopic patients are different comparing with low myopia patients.
The safety and effectiveness of phakic ICL surgery have already been established elsewhere, with comparable or even better results than those obtained with laser refractive surgery (LASIK, PRK).9,18–21 A few isolated studies with smaller samples, however, have reported vision line gains in patients with myopia who underwent ICL surgery.9 Of these, a paper by Ying et al indicated that 57% of patients with a preoperative myopia of 10 D or more gained 1 or more lines after ICL surgery.12 Besides confirming the safety, and the excellent refractive results with ICLs in a large patient cohort, our study has, for the first time, shown patients with higher degrees of myopia achieve better results than those with lower myopia. Bearing in mind our patients were all operated on by the same surgeon, our findings are also much less liable to surgeon bias.
The improved visual power measured in postoperative follow-up could be because the lens (of greater power in higher myopias) is closer to the fovea centralis, thus effectively magnifying the received image, very similar to that obtained with the use of contact lenses. This effect was most evident in eyes that received the ICLs with the highest powers. Therefore, whenever comparing the pre- and postoperative visual acuity, it is important to remember that all refractive surgeries produce a change in retinal image magnification.20,21 This magnification is less than unity in myopic eyes corrected with ophthalmic lenses prior to surgery. After surgery, the magnification approaches unity, so the image formed on the retina is larger. For example, an eye with a myopic error of −6.00 D corrected with ophthalmic lenses at a vertex distance of 14 mm has a magnification of around 0.9x. After ICL surgery, the image on the retina will be magnified by a factor of approximately 1.1x. Therefore, in the absence of any other related factors, visual acuity should improve slightly after myopia correction surgery, with the effect enhanced by the magnitude of the correction. At higher corrections, the greater the retinal image magnification and, in turn, the higher the visual acuity (or greater the line gain compared to preoperative values). Beyond the good results reported here, it is worth noting that a more in-depth study is required to analyse the specific causes for the improvement in BCVA in patients with higher myopia, as other factors unrelated to retinal image magnification may also have an impact.
It is important to mention that this study has certain limitations. Notably, we only measured visual acuity based on 20/20 vision on a Snellen chart (or 0.0 logMAR), so we do not know if some patients with a preoperative BCVA of 20/20 could have improved beyond this point, and patients with high myopia also tend to have severe amblyopia. What is more, we did not perform separate analyses on the datasets for patients who were and were not treated for astigmatism in addition to myopia. Another limitation to bear in mind was the short postoperative follow-up period (1 month). However, this might not be very relevant given that previous studies have suggested that any long-term visual changes in this type of patient are insignificant as they continue to obtain stable results in visual acuity tests for years.22,23 On the other hand, could be consider a limitation of this study the fact that corneal endothelial cells changes pre and postoperative were not included. Nevertheless, this aspect has been well analysed in previous studies, obtained a mild endothelial cell lost during the first postoperative year, maybe due to surgery, but there have not been ongoing chronic loss more than normal and no cases of corneal decompensation in the absence of trauma have been reported following ICL implantation.9,24,25 Finally, we would like to emphasise that the extrapolation of our conclusions to other populations, including other races or less experienced surgical teams, should be treated with precaution when obtaining similar results to ours. Also we want to point out the large number of eyes included in this study.
Conclusions
Our study, conducted in a large, “real world” cohort of patients with myopia, shows that ICL surgery yields significant postoperative line gains in visual acuity (BCVA), particularly in eyes with a high degree of myopia.
Data Sharing Statement
The datasets analysed in the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted according to the tenets of the Declaration of Helsinki. This study was approved by the Institutional Review Board of the Instituto Zaldivar. Informed consent was obtained from all the patients prior to enrolment.
Author Contributions
All authors made substantial contributions to the conception and design, data acquisition, analysis and/or interpretation; took part in drafting the article or revising it critically for significant intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by STAAR Surgical.
Disclosure
Drs. Roger and Roberto Zaldivar are consultants for STAAR Surgical. The remaining authors have no proprietary or financial interest in the materials presented herein.
References
1. Torricelli AA, Bechara SJ, Wilson SE. Screening of refractive surgery candidates for LASIK and PRK. Cornea. 2014;33(10):1051–1055. doi:10.1097/ICO.0000000000000171
2. Vestergaard AH. Past and present of corneal refractive surgery: a retrospective study of long-term results after photorefractive keratectomy and a prospective study of refractive lenticule extraction. Acta Ophthalmol. 2014;2:1–21. doi:10.1111/aos.12385
3. Luger MH, Ewering T, Arba-Mosquera S. Myopia correction with transepithelial photorefractive keratectomy versus femtosecond-assisted laser in situ keratomileusis: one-year case-matched analysis. J Cataract Refract Surg. 2016;42(11):1579–1587. doi:10.1016/j.jcrs.2016.08.025
4. Agca A, Demirok A, Yildirim Y, et al. Refractive lenticule extraction (ReLEx) through a small incision (SMILE) for correction of myopia and myopic astigmatism: current perspectives. Clin Ophthalmol. 2016;10:1905–1912. doi:10.2147/OPTH.S80412
5. Gatinel D, Weyhausen A, Bischoff M. The Percent Volume Altered in Correction of Myopia and Myopic Astigmatism With PRK, LASIK, and SMILE. J Refract Surg. 2020;36(12):844–850. doi:10.3928/1081597X-20200827-01
6. Schmitt-Bernard CF, Lesage C, Arnaud B. Keratectasia induced by laser in situ keratomileusis in keratoconus. J Refract Surg. 2000;16(3):368–370. doi:10.3928/1081-597X-20000501-12
7. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115(1):37–50. doi:10.1016/j.ophtha.2007.03.073
8. Sorkin N, Kaiserman I, Domniz Y, Sela T, Munzer G, Varssano D. Risk Assessment for Corneal Ectasia following Photorefractive Keratectomy. J Ophthalmol. 2017;2017:2434830. doi:10.1155/2017/2434830
9. Packer M. The Implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427–2438. doi:10.2147/OPTH.S188785
10. Zaldivar R, Davidorf JM, Oscherow S, Ricur G, Piezzi V. Combined posterior chamber phakic intraocular lens and laser in situ keratomileusis: bioptics for extreme myopia. J Refract Surg. 1999;15(3):299–308. doi:10.3928/1081-597X-19990501-04
11. Alfonso JF, Lisa C, Fernandez-Vega Cueto L, Fernandes P, Gonzalez-Meijome JM, Montes Mico R. Comparison of visual and refractive results of Toric Implantable Collamer Lens with bioptics for myopic astigmatism. Graefes Arch Clin Exp Ophthalmol. 2013;251(3):967–975. doi:10.1007/s00417-012-2155-9
12. Ying X, Li Y, Zhang F. Predictive factors for postoperative visual acuity improvement with ICL-V4c for ultrahigh myopia above - 10 D. Graefes Arch Clin Exp Ophthalmol. 2022;260(9):3107–3114. doi:10.1007/s00417-022-05626-5
13. Sorkin N, Varssano D, Smadja D, Klein A, Mimouni M, Rosenblatt A. Visual outcomes of laser vision correction in eyes with preoperative amblyopia. J Cataract Refract Surg. 2017;43(3):383–388. doi:10.1016/j.jcrs.2016.12.029
14. Dougherty PJ, Priver T. Refractive outcomes and safety of the implantable collamer lens in young low-to-moderate myopes. Clin Ophthalmol. 2017;11:273–277. doi:10.2147/OPTH.S120427
15. Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102(2):177–181. doi:10.1136/bjophthalmol-2017-310164
16. Pinto C, Monteiro T, Franqueira N, Faria-Correia F, Mendes J, Vaz F. Posterior chamber collamer phakic intraocular lens implantation: comparison of efficacy and safety for low and moderate-to-high myopia. Eur J Ophthalmol. 2021;11206721211012861. doi:10.1177/11206721211012861
17. Wang Q, Fan L, Zhou Q. The best choice for low and moderate myopia patients incapable for corneal refractive surgery: implantation of a posterior chamber phakic intraocular lens. Int Ophthalmol. 2022;43(2):575–581. doi:10.1007/s10792-022-02459-3
18. Packer M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clin Ophthalmol. 2016;10:1059–1077. doi:10.2147/OPTH.S111620
19. Hruba H, Vlkova E, Horackova M, Svacinova J. [Comparison of clinical results between LASIK method and ICL implantation in high myopia]. Cesk Slov Oftalmol. 2004;60(3):180–191. Czech.
20. Sanders D, Vukich JA. Comparison of implantable collamer lens (ICL) and laser-assisted in situ keratomileusis (LASIK) for low myopia. Cornea. 2006;25(10):1139–1146. doi:10.1097/ICO.0b013e31802cbf3c
21. Liu HT, Zhou Z, Luo WQ, et al. Comparison of optical quality after implantable collamer lens implantation and wavefront-guided laser in situ keratomileusis. Int J Ophthalmol. 2018;11(4):656–661. doi:10.18240/ijo.2018.04.20
22. Packer KT, Vlasov A, Greenburg DL, et al. U.S. military implantable collamer lens surgical outcomes: 11-year retrospective review. J Cataract Refract Surg. 2022;48(6):649–656. doi:10.1097/j.jcrs.0000000000000818
23. Papa-Vettorazzi MR, Guell JL, Cruz-Rodriguez JB, Moura-Coelho N, Elies D. Long-term efficacy and safety profiles after posterior chamber phakic intraocular lens implantation in eyes with more than 10 years of follow-up. J Cataract Refract Surg. 2022;48(7):813–818. doi:10.1097/j.jcrs.0000000000000848
24. Edelhauser HF, Sanders DR, Azar R, Lamielle H; Group ICLiToMS. Corneal endothelial assessment after ICL implantation. J Cataract Refract Surg. 2004;30(3):576–583. doi:10.1016/j.jcrs.2003.09.047
25. Goukon H, Kamiya K, Shimizu K, Igarashi A. Comparison of corneal endothelial cell density and morphology after posterior chamber phakic intraocular lens implantation with and without a central hole. Br J Ophthalmol. 2017;101(11):1461–1465. doi:10.1136/bjophthalmol-2016-309363
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
