Back to Journals » International Journal of Women's Health » Volume 15
Describing the Patient Journey of Women with Claims for Uterine Fibroids and Heavy Menstrual Bleeding Using a Commercial Database (2011–2020)
Authors Agarwal SK , Stokes M, Kung T, Tilney R, Lickert C
Received 17 June 2023
Accepted for publication 26 September 2023
Published 16 October 2023 Volume 2023:15 Pages 1561—1575
DOI https://doi.org/10.2147/IJWH.S420612
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Sanjay K Agarwal,1 Michael Stokes,2 Tiffany Kung,3 Rong Tilney,2 Cassandra Lickert3
1UC San Diego, La Jolla, CA, USA; 2Evidera, St. Laurent, Quebec, Canada; 3Myovant Sciences, Inc (now known as Sumitomo Pharma America, Inc), Marlborough, MA, USA
Correspondence: Cassandra Lickert, Sumitomo Pharma America, Inc, 4 Waterford Drive, Marlborough, MA, 01752, USA, Tel +1 (708) 214-1007, Email [email protected]
Introduction: This retrospective database claims analysis describes the clinical characteristics and treatment patterns of commercially insured United States women with uterine fibroids (UF) and heavy menstrual bleeding (HMB).
Methods: Women age 18– 55 years with an incident UF diagnosis (index date) between 1/1/2012 and 12/31/2019 and ≥ 1 claim for HMB (UF-HMB), were identified from the Optum® Clinformatics® database. Outcomes included clinical characteristics, pharmacologic therapy use, and surgeries/procedures. Regression models were used to identify factors associated with time to post-diagnosis hormonal therapy and hysterectomy.
Results: A total of 85,428 women had UF-HMB (mean [SD] age, 43.7 [6.4] years). The median follow-up was 3.2 years. After HMB, the most common symptoms were pelvic pressure/pain (27.6%) and backache (17.5%). Within 6 months of UF diagnosis, 40.2% of patients had received only pharmacologic therapy; 25.5% had received no treatment; 24.3% had a hysterectomy, and 10.0% had other procedures. By the end of follow-up, 50.0% had received a hysterectomy. Multiple factors were predictive of a higher likelihood of receiving hormonal therapy (geographic region, infertility, pre-index pregnancy) or hysterectomy (older age, prior hormonal treatment, specific bulk symptoms, White race).
Conclusion: Within 6 months of UF diagnosis, fewer than one-half of women with UF-HMB had received hormonal therapy, one-quarter received no treatment, and one-quarter had received a hysterectomy or another gynecologic procedure. Patients who received a hysterectomy were more likely to be older, White, and to have bulk symptoms.
Keywords: uterine fibroids, leiomyoma, heavy menstrual bleeding, menorrhagia
Introduction
Uterine fibroids (UF) are common, hormone-sensitive benign, uterine tumors that affect at least 70–80% of all women by age 50.1–3 UF incidence increases with age until menopause,1 with a mean age at diagnosis of 40.4 years.4 In the United States (US), UF are most prevalent in African American women.1,3 The majority of patients with UF are asymptomatic, and their condition is identified during routine clinical examination or imaging.5 Other women are diagnosed because they experience symptoms associated with UF,2,3,6 most commonly heavy menstrual bleeding (HMB), with or without anemia.4,5,7,8 Women with UF also frequently experience bulk symptoms, including pelvic pain/pressure, urinary and bowel symptoms, and leg and lower back pain.4,5,7,8
A number of drugs have been used to treat symptomatic UF: gonadotropin-releasing hormone (GnRH) analogs, other hormonal therapies (aromatase inhibitors, contraceptives, selective progesterone receptor modulators), nonsteroidal anti-inflammatory drugs (NSAIDs), and tranexamic acid.5,7 Until recently, available pharmaceuticals have primarily addressed bleeding, but not bulk symptoms.3 The US Food and Drug Association recently approved 2 new oral therapies for the management of HMB associated with UF, including elagolix (approved May 2020) and relugolix combination therapy (May 2021), both GnRH antagonists with add-back hormonal treatment.9,10 Relugolix combination therapy has also been shown in Phase 3 trials to reduce pain and bulk symptoms of UF.11–13
Multiple surgical and other procedural options exist for UF, including hysterectomy, myomectomy, uterine artery embolization (UAE), and endometrial ablation.14,15 Surgical procedures reduce HMB and decrease uterine mass to provide bulk symptom relief but are not the preferred choice for all patients.3 In the US, hysterectomy is by far the most common procedure used to treat UF.14 A large US retrospective database analysis (2010–2015) found that, among commercially insured and Medicaid patients, hysterectomy accounted for 68–76% of initial UF-related surgeries.14 Similarly, a recent claims analysis (2010–2019) of commercial patients found that, in the first year following UF diagnosis, hysterectomy accounted for 62.5% of all UF-related procedures in women with UF and HMB (UF-HMB).16
With the availability of new oral therapies with the potential to alter how UF is managed, it is important to have real-world benchmarks for patient treatment patterns and clinical outcomes. Indeed, aside from the clinical research programs for elagolix and relugolix combination therapy,11,17 limited clinical data have been published in this disease space since 2015. The objective of this retrospective claims database analysis was to describe clinical characteristics and treatment patterns (drug therapy and hysterectomy) of commercially insured women with medical claims for UF-HMB over the last decade.
Materials and Methods
Study Design and Data Source
Women from the Optum® Clinformatics® (Optum) database, age 18–55 years, with an initial UF diagnosis between January 1, 2012, and December 31, 2019, and ≥1 claim for HMB, were identified. The Optum database contains comprehensive, de-identified longitudinal data for >180 million commercial health plan enrollees, with data availability from January 1, 2011, (initiation of study database) through December 31, 2020, (end of study database). The database includes information on patient demographics, diagnoses, and procedures performed during outpatient and inpatient visits.
This research was not subject to the US Department of Health and Human Services (HHS) Common Rule requirements or institutional review board (IRB) review. Codified at 45 Code of Federal Regulations (C.F.R.) Part 46, the Common Rule includes requirements for IRB review to ensure adequate protection of human subjects. However, in this case, research was conducted using protected health information (PHI) that had been de-identified in compliance with the HHS Privacy Rule’s requirements, codified at 45 C.F.R. § 164.514(a)–(c). All data in the Optum Research Database were obtained from covered entities that permitted this PHI de-identification for use in Optum research studies. Throughout the process, patient privacy was preserved, and researchers complied strictly with all applicable Health Insurance Portability and Accountability Act data management rules and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Patient consent was not required for this retrospective study.
Study Population
To be included, patients were required to have a UF diagnosis on ≥2 outpatient claims ≥30 days apart or 1 inpatient claim and ≥1 medical claim (outpatient or inpatient) for HMB, irrespective of its temporal relationship to the UF diagnosis. See Figure S1 for study schema and diagnostic codes. The index date was the date of the first UF diagnosis claim. Patients had to have ≥1 year of continuous pre- and post-index–date enrollment, or for patients who underwent hysterectomy within 1 year of index, continuous post-index enrollment until the date of hysterectomy. Patients with evidence of pre-index hysterectomy were excluded. Patient follow-up began on the index date and continued until death, disenrollment, hysterectomy, or end of study database, whichever occurred first.
Pre-Index Measures
Patients’ demographic and clinical characteristics were collected for the 12-month pre-index period. This included age, race/ethnicity, geographic location, payer, health plan type, and Charlson Comorbidity Index (CCI) (all obtained at time of UF diagnosis); time of HMB diagnosis relative to UF diagnosis; and comorbidities/conditions, including those related to women’s health and bulk symptoms (see Table S1 for diagnostic codes). Pre- and post-index, information was also collected regarding pharmacologic therapies of interest for UF, including hormonal treatments (contraceptives, GnRH agonists and antagonists, aromatase inhibitors, selective estrogen receptor modulators, selective progesterone receptor modulators, and non-contraceptive steroids [oral danazol or intravenous estradiol or progesterone]) and other primary treatments (anti-fibrinolytics and analgesics [acetaminophen, NSAIDs, opioids]). Medication use was identified based on outpatient prescription dispensation, with relevant National Drug Code (NDC) codes, as appropriate.
Post-Index Outcomes
Pharmacotherapy patterns were ascertained from pre-index through the time of hysterectomy or end of follow-up, whichever occurred first. Treatment patterns were analyzed over 6-month intervals (ie, no treatment, pharmacologic treatment only, hysterectomy ± other procedures or pharmacotherapy, and surgeries/procedures other than hysterectomy ± pharmacotherapy). Additionally, specific treatment pathways with hormonal contraceptives were tracked for up to 3 lines of therapy (ie, switches of up to 2 additional hormonal contraceptives) in a patient subset that received post-index hormonal contraceptives (with ≥24 months of follow-up) or a hysterectomy within 24 months of the index date. For hormonal contraceptives, discontinuation was defined as a gap of ≥60 days with no prescription refills. A switch occurred when a new hormonal contraceptive was initiated prior to discontinuation of the previous hormonal contraceptive. Patients who remained on their initial hormonal contraceptive without switching or discontinuing <60 days before the end of follow-up were defined as not switching. For analyses of broader hormonal therapy regimens or medication classes, a gap of ≥90 days with no prescription fills signified treatment discontinuation (because refill cycles for these regimens are generally longer than for contraceptive hormones).
The post-index occurrence of surgeries/procedures for UF was also measured, including hysterectomy. See Table S2 for a full list and relevant identifying claims codes.
Statistical Analyses
Demographics, clinical characteristics, pharmacotherapy use, and the occurrence of surgical procedures were summarized using descriptive statistics. Kaplan–Meier (KM) curves were used to examine the time from index date to hysterectomy. Cox proportional hazard regression models were constructed to determine factors associated with hormonal treatment or hysterectomy; variables included age, race, geographic region, CCI, comorbidities, and bulk symptoms. Patients with pre-index hormone therapy were excluded from the model that examined time to hormonal treatment. The model examining hysterectomy included prior hormone therapy as a time-varying covariate. Hazard ratios (HRs) and 95% confidence intervals (CIs) were reported for each main effect. Data were analyzed using the SAS version 9.4.
Results
Demographic and Clinical Characteristics
A total of 299,416 women with a UF diagnosis were identified; after applying selection criteria, 85,428 patients with UF-HMB were included in the study (Table 1). The mean (SD [median]) duration of the follow-up was 44.5 (27.7 [38.0]) months or 3.7 years.
 |
Table 1 Patient Attrition |
Table 2 shows demographic characteristics for the study cohort at the time of UF diagnosis, and pre-index clinical characteristics. The mean (SD) patient age was 43.7 (6.4) years. Most were White (46,139 [54.0%]), one-fifth (20.2%) were African American, and the largest proportion resided in the US South (40,321 [47.2%]). Most women were diagnosed with HMB in the year prior to (35,385 [41.4%]) or the 6 months following their UF diagnosis (17,208 [20.1%], inclusive of index). Common women’s health issues were endometriosis (4324 [5.1%]), pregnancy (pre-index; 4143 [4.8%]), and uterine polyps (3643 [4.3%]). Other prevalent comorbidities were hypertension (18,059 [21.1%]), hyperlipidemia (16,415 [19.2%]), fatigue (15,325 [17.9%]), urinary tract infection (11,777 [13.8%]), obesity (11,398 [13.3%]), and anemia (3734 [4.4%)]. Post-index anemia prevalence (3460 [4.1%]) was similar to pre-index. One-half of patients (42,603 [49.8%]) had ≥1 bulk symptom, most commonly pelvic pressure/pain (23,570 [27.6%]) and backache (14,950 [17.5%]).
 |
Table 2 Patient Demographic and Clinical Characteristics at Index |
Treatment Patterns
In the 6 months following UF diagnosis (N = 85,428), 21,809 (25.5%) of patients received no treatment; 34,314 (40.2%) received only pharmacologic therapy; 8578 (10.0%) received procedures other than hysterectomy; and 20,727 (24.3%) had a hysterectomy (Figure 1). During the 6–12 months post-UF diagnosis (N = 81,760), 35,327 (43.2%) patients did not receive any treatment and 39,991 (48.9%) received only pharmacologic therapy. In the >18-24-month post-UF diagnosis (N = 70,350), 48.0% of patients did not receive any treatment, and 48.0% received only pharmacologic treatment.
 |
Figure 1 Patient Treatment Patterns Through 24 Months. Abbreviation: UF, uterine fibroid. |
The most common therapies prescribed prior to UF diagnosis (pre-index) were contraceptive hormones (16,007 [18.7%]), opioids (7969 [9.3%]), NSAIDs (7155 [8.4%]), and non-contraceptive steroid hormones (6336 [7.4%]) (Figure 2). Post-index, the most common therapies prescribed were NSAIDs (29,072 [34.0%]), opioids (28,518 [33.4%]), contraceptive hormones (27,038 [31.7%]), and non-contraceptive steroid hormones (13,377 [15.7%]).
 |
Figure 2 UF-related Pharmacotherapy Use Before and After Initial UF Diagnosis. Abbreviations: GnRH, gonadotropin-releasing hormone; NSAID, non-steroidal anti-inflammatory drug; UF, uterine fibroid. |
Figure S2 shows the use of initial post-index hormone therapy, stratified by hormone therapies used in the 3 months prior to UF diagnosis (pre-index). Regardless of the type of initial post-index hormone therapy used (N = 31,850), 65.0% (20,709/31,850) of patients were not receiving any pharmacologic treatment prior to diagnosis, while the remainder were using either contraceptive hormones (25.5%), contraceptive hormones plus non-contraceptive steroid hormones (5.9%), non-contraceptive steroid hormones (3.3%), or GnRH agonists (0.1%). When broken down by specific post-index hormone therapy, most patients were either not using any pre-index pharmacologic therapy (59.5–75.1%) or were using the same form of hormone therapy as observed post-index (21.6–38.8%).
Table 3 shows patterns of contraceptive hormone use in patients who initiated a contraceptive hormone post-index and had ≥24 months of follow-up (n = 19,908, 23.3%). The average duration of use was 284 days. Of these patients, 17,918 (90.0%) discontinued contraceptive hormone use after 1 agent (16,024 [80.5%]) or 2 different contraceptive hormones (1894 [9.5%]). Only 2.5% of women were exposed to a third contraceptive hormone. After discontinuing their initial contraceptive hormone (n = 16,024), patients most commonly re-started contraceptive hormone therapy (4965 [30.1%]), received a hysterectomy (3438 [21.5%]) or started other steroid hormones (2641 [16.5%]) (Table 4).
 |
Table 3 Mean Time (Days) on Post-Index Contraceptive Hormone Therapy |
 |
Table 4 Subsequent Therapies Received by Patients Who Discontinued Initial Post-Index Contraceptive Hormones |
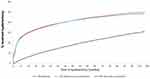
Figure 3 shows the KM analysis of time to hysterectomy. At 12 and 24 months of follow-up, 29.5% and 35.0% of all patients had received a hysterectomy. At the end of post-index follow-up, 50.0% of patients had received a hysterectomy. Among patients who had not received a pre-index surgery/procedure, 30.2% and 35.6% had received a hysterectomy at 12 and 24 months. Among patients who did have a pre-index surgery/procedure, 6.3% and 10.9% had received a hysterectomy at 12 and 24 months. For patients with a pre-index surgery/procedure (n = 4002), the mean (SD) time from first procedure to hysterectomy was 17.4 (18.8) months.
Multivariate Analyses
Figure 4A shows the results of Cox proportional hazards models examining the time to hormonal therapy initiation. Demographic characteristics associated with a lower likelihood of initiating hormonal therapy (HR [95% CI]) were older age (30–44 years: 0.54 [0.50–0.59]; 45–55 years: 0.36 [0.33–0.39]; both P<0.0001) and Black race (0.92 [0.89–0.96]; P<0.0001). Clinical characteristics associated with a lower likelihood of initiating hormonal therapy (HR [95% CI]) were higher CCI (CCI 2: 0.80 [0.75–0.86]; CCI 3+: 0.76 [0.70–0.83]; P<0.0001 for all); presence of uterine polyps (0.90 [0.83–0.97]; P=0.007); abdominal distention (0.88 [0.80–0.97]; P=0.0125); and increased abdominal girth (0.69 [0.63–0.74]; P<0.0001). The following were significantly associated with a higher likelihood (HR [95% CI]) of initiating hormonal therapy: geographic region (South: 1.07 [1.02–1.12]; West: 1.15 [1.09–1.21]; P=0.0036 and P<0.0001, respectively); infertility (1.80 [1.67–1.94]; P<0.0001); and pre-index pregnancy at any time (1.22 [1.15–1.29]; P<0.0001).
Figure 4B shows the results of Cox proportional hazards models examining time to hysterectomy. Demographic characteristics associated with a shorter time to hysterectomy (HR [95% CI]) were increasing age (30–44 years: 5.60 [4.68–6.71]; 45–55 years: 6.42 [5.39–7.69]; both P<0.0001) and geographic region (Midwest: 2.26 [2.16–2.36]; South: 2.03 [1.95–2.12]; West: 1.78 [1.70–1.86]; all P<0.0001). Clinical characteristics associated with a shorter time to hysterectomy (HR [95% CI]) were higher CCI (CCI 1: 1.05 [1.02–1.08]; CCI 2: 1.10 [1.05–1.16]; P=0.0016 and P<0.0001, respectively); use of post-index hormonal therapy (3.67 [3.56–3.77]; P<0.0001); increased abdominal girth (1.58 [1.51–1.66]; P<0.0001); adenomyosis (1.48 [1.34–1.63]; P<0.0001); pelvic pressure/pain (1.24 [1.21–1.27]; P<0.0001); presence of uterine polyps (1.15 [1.10–1.21]; P<0.0001); and endometriosis (1.11 [1.05–1.17]; P=0.0001). Some demographic and clinical characteristics were significantly associated with a longer time to hysterectomy (HR [95% CI]): Race (Black: 0.86 [0.83–0.88]; other: 0.79 [0.77–0.82]; both P<0.0001); leg pain (0.96 [0.92–0.99]; P=0.0143); abdominal distention (0.85 [0.79–0.91]; P<0.0001); infertility (0.32 [0.28–0.36]: P<0.0001); and any pre-index pregnancy (0.30 [0.27–0.33]; P<0.0001).
Discussion
This retrospective analysis of claims data updates our understanding of the characteristics and treatment journey of commercially insured US patients with UF-HMB diagnosed over the past decade (2011–2019). Most women with UF-HMB (97.8%) were between 30 and 55 years of age, with incidence evenly distributed between age categories of 30–44 and 45–55 years. These results are similar to age-proportional distributions reported by epidemiologic research from 2003,1 and to a recent commercial retrospective claims analysis conducted using a different database.16 In this analysis, just under one-half of patients with UF-HMB resided in the Southern part of the US. This is proportionally similar to UF geographic distribution reported in US administrative claims research from 1999 to 2004,18 2000–2010,19 and 2010–2015.14 Finally, the majority (54.0%) of patients with UF-HMB in the current study were White, while African American women made up only 20.2% of the cohort, suggesting that African American women were underrepresented in this database.20,21
The patient symptomatology and comorbid conditions observed in this study reflect the humanistic burden of UF-HMB in the US. Overall, one-half of patients experienced bulk symptoms in addition to HMB. The most frequently reported were pelvic pressure/pain, experienced by approximately 1 in 4 patients (27.6%); backache, experienced by nearly 1 in 5 (17.5%); and urinary symptoms and/or leg pain, experienced by 1 in 10 (9.9% and 9.7%). Also, noteworthy is the high rate of opioid use after UF diagnosis (33.4%), indicative of a substantial experienced pain burden. This pattern of symptomatology, including pelvic pressure and/or pain as the second-most prevalent UF symptom (after HMB), is supported by data from a systematic literature review covering 2000 to 2013;22 2012 data from a US cross-sectional survey (N = 59,411);23 and a 2010–2019 US retrospective analysis of the IQVIA PharMetrics® Plus database (N = 66,313).16
In the current study, 5% of the patients had comorbid endometriosis or fertility issues, and 4% had uterine polyps. Approximately 4% had anemia prior to their UF-HMB diagnosis. Post-diagnosis, this percentage remained the same. Although one might expect anemia claims to increase following a UF-HMB diagnosis, this was not the case, possibly due to under-reporting or patients receiving pre-index anemia treatment. Previous research confirms the association between UF and these women’s health conditions.23–26 Other comorbidities common in women with UF-HMB in this study and prior research were depression, diabetes, hyperlipidemia, hypertension, and obesity.23,27,28 However, patients from the 2012 cross-sectional US survey had higher self-reported rates of endometriosis (16.5%), infertility (8.6%), and polyps (7.6%) than the current analysis.23
The US treatment patterns and pathways identified in this study point to an unmet need for noninvasive, effective therapies that address the underlying pathophysiology of symptomatic UF. Despite experiencing a substantial disease burden, one-quarter of women with UF-HMB were not treated in the 6 months following UF diagnosis. This was the case even though, in this same 6-month post-index period, one-third of these patients were subsequently diagnosed with HMB. Following UF diagnosis, the primary treatments prescribed were contraceptive hormones and hysterectomy. After initial contraceptive hormone therapy, switching or adding other contraceptive hormone therapies was not typical. Instead, discontinuation was common (80.5%) and occurred within a short period (~7 months). Interestingly, of those who discontinued their initial contraceptive hormone and were treated with a subsequent therapy, nearly one-third (30.1%) restarted a contraceptive hormone and one-fifth (21.5%) had a hysterectomy.
With respect to hysterectomy, one-quarter of women with UF-HMB received this surgery within 6 months of UF diagnosis (patients with pre-index hysterectomy were excluded). At 12 months of follow-up, 29.5% of patients with UF-HMB had received a hysterectomy; this proportion increased to 35.0% at 2 years and 50.0% at the end of follow-up. Hysterectomy rates were lower in women with prior procedures, suggesting that a prior procedure may prevent hysterectomy in some women. While the treatment patterns observed were largely similar to those seen in other, recent US retrospective analyses,14,29 this high hysterectomy rate soon after UF diagnosis is notable, and additional research is warranted to understand why so many women undergo hysterectomies in the 6 months after UF-HMB diagnosis. One possibility is age, as uterine-sparing procedures may not be a priority for older women. In a multivariate analysis, women in older age groups (30–44 and 45–55 years) were 6–7 times more likely to undergo hysterectomy than younger patients (18–29 years). Similarly, in a 2007–2018 US retrospective commercial database claims analysis, 81% of 52,270 women with UF-HMB who underwent hysterectomy were 39–51 years, whereas 59% of 3693 women who had a myomectomy were <40 years.29 Another likelihood is that some patients who received hysterectomy preferred to have this surgery. In a 2020–2022 survey of 67 women (mean [SD] age 46.2 [7.5] years; 57% White; 100% no prior hysterectomy) treated for UF at an urban, outpatient clinic, 35% preferred hysterectomy over myomectomy for a number of reasons that included improved emotions/mood, quality of life, identity/body image, relationship with partner, and sexuality.30
Race may also be a factor in hysterectomy frequency. In this study, White women were significantly more likely than Black women and women of other races to receive a hysterectomy in the 6 months following diagnosis. Similar findings were observed in a 2021 US questionnaire-based cohort study (N = 2337) that evaluated White (n = 1141) and Black (n = 1196) women age 18–54 years as part of the Comparing Options for Management: Patient-Centered Results for UF treatment registry. White women had a higher hysterectomy rate than Black women (43.6% versus 32.2%). The role of race in treatment choice was statistically significant when evaluated using logistic regression.31
The 2008 American College of Obstetricians and Gynecologists (ACOG) clinical management guidelines for symptomatic UF in place during this study also provide an explanation for the high frequency of hysterectomy following UF diagnosis. While these guidelines emphasized alternatives to hysterectomy, they also indicated that available medical therapies provided only short-term symptomatic relief and/or temporary fibroid size reduction, and that there was a high crossover rate to surgical approaches, including hysterectomy. The guidelines did not address the role of individualized management but did emphasize the need to consider treatment safety and efficacy.32 Therefore, the treatment patterns observed in this study may be reflective of outdated clinical management guidelines.
According to the updated 2021 ACOG guidelines, insufficient comparative evidence exists to offer recommendations for first-line medical therapy in patients with UF. Therefore, individualized medical management, based on patient-specific symptoms and their severity, should be used to guide treatment rather than a prespecified clinical sequencing algorithm. ACOG also underscores the importance of engaging patients in shared decision-making that takes their long- and short-term therapeutic goals into account.3
Treatment guidelines for patients with UF have evolved over the past 15 years. In particular, the updated guidelines reflect the availability of a new medication class (GnRH antagonists with hormonal add-back therapy) suitable for up to 24 months of use to treat UF-associated HMB, pain, and/or bulk symptoms.3,9,10 With ACOG guidelines recently updated and the introduction of this pharmacologic class, treatment trends are likely to change to incorporate shared decision-making and increased treatment options. Clinician education regarding these updates, as well as ongoing research regarding treatment patterns, is warranted.
Study Limitations
This retrospective, descriptive study used medical and pharmacy claims data. Consequently, caution is warranted with respect to drawing conclusions about causality or inferences regarding the medical decision-making processes underpinning treatment choices. Furthermore, claims data are not collected specifically for research and are subject to gaps, potential coding variance and errors. There is no standard approach among clinicians regarding the best approaches to coding patient encounters (ie, whether to code for diagnosis with symptomatology, diagnosis only, and/or diagnosis in addition to separate claims for each symptom). As such, this study will not capture all symptoms reported by patients during medical visits. It is also not feasible to confirm that the symptom claims recorded in this analysis were related to UF, as other conditions may have caused the symptoms.
Similarly, because NDC codes are not associated with a specific diagnosis, patients may have been prescribed drugs for reasons other than UF-HMB, leading to an inflated drug treatment rate. Conversely, some hormonal contraceptives may have been absent from claims data in cases where patients paid for prescriptions out-of-pocket; this could have led to an underestimate of drug treatment. Furthermore, although efforts were made to limit the study population to women with recently diagnosed UF and HMB, patients could have received a UF diagnosis or incurred HMB claims in the years prior to 2011. Last, it should be noted that, from the physician perspective, changing medication from one hormonal contraceptive to another might not be considered a true therapeutic switch. Therefore, the treatment pathways for prescribed hormonal contraceptives in this study might not align with physician experience.
These findings can be generalized to US insured women with UF-HMB age 55 years and younger. Findings cannot be generalized to the overall US population because this study primarily includes data for commercially insured patients with limited government-funded insurance plans (Medicare) and may have excluded self-insured individuals. Pre-menopausal women age >55 years were also excluded, which limits the ability to generalize study results to an older population. Additionally, women trying to conceive during the study period may not have been candidates for hormonal options and hysterectomy, and may account for some women who received no treatment. Finally, African Americans were likely underrepresented in this study,20,21 which is a commonly reported issue in the literature,3,33,34 and may impact the treatment patterns identified. In the current analysis, this underrepresentation is due to the study’s commercial insurance focus; a higher proportion of African American than White patients receives Medicaid or other public insurance.20 Other ethnic groups that were not well represented in this study were Hispanic, Asian, and Native American populations.
Conclusion
In this analysis, fewer than one-half of women with UF-HMB received hormonal therapy within 6 months of UF diagnosis. In the same time frame, one-quarter of these patients received no treatment, and one-quarter had a hysterectomy or another gynecologic procedure. Among women who initiated contraceptive hormones post-index, discontinuation was common, but switching or adding other contraceptive hormones was not. Patients who received a hysterectomy were more likely to be older, White, and to have bulk symptoms. Additional research is needed to understand the factors driving these treatment patterns, as well as how new therapeutic agents may impact future treatment patterns.
Abbreviations
ACOG, American College of Obstetricians and Gynecologists; CCI, Charlson comorbidity index; CPT, Current Procedural Terminology; GnRH, gonadotropin-releasing hormone; HCPCS, Healthcare Common Procedure Coding System; HMB, heavy menstrual bleeding; ICD, International Classification of Diseases; KM, Kaplan Meier; MRI, magnetic resonance imaging; NDC, National Drug Code; NSAIDs, nonsteroidal anti-inflammatory drugs; UAE, uterine artery embolization; UF, uterine fibroids.
Data Statement
The data that support the findings of this study are property of Evidera; restrictions apply to the availability of these data, which were used under license and were therefore only available during the conduct of the study.
Acknowledgments
The authors would like to thank Robert Dufour for his assistance in developing this project and reviewing the manuscript. Medical writing support was provided by Caitlin Rothermel MA, MPH of MedLitera as overseen by Simcoe Consultants, Inc, and funded by Myovant Sciences GmbH, in collaboration with Pfizer, Inc.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all of these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
This work was supported by Sumitomo Pharma Switzerland GmbH, in collaboration with Pfizer, Inc., and conducted by Evidera.
Disclosure
SKA is a consultant to Myovant (now known as Sumitomo Pharma America, Inc)/Pfizer and AbbVie as well as a member of the AbbVie speakers’ bureau. MS is an employee of Evidera, which received consulting fees from Myovant (now known as Sumitomo Pharma America, Inc) for this study. TK was an employee of Myovant Sciences Inc (now known as Sumitomo Pharma America, Inc). RT was an employee of Evidera. CL is an employee of Myovant Sciences Inc (now known as Sumitomo Pharma America, Inc). The authors report no other conflicts of interest in this work.
References
1. Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1):100–107. doi:10.1067/mob.2003.99
2. Stewart EA, Cookson CL, Gandolfo RA, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501–1512. doi:10.1111/1471-0528.14640
3. American College of Obstetricians & Gynecologists. Management of symptomatic uterine leiomyomas: ACOG practice bulletin, number 228. Obstet Gynecol. 2021;137(6):e100–e115. doi:10.1097/AOG.0000000000004401
4. Zimmermann A, Bernuit D, Gerlinger C, Schaefers M, Geppert K. Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC Women's Health. 2012;12:6. doi:10.1186/1472-6874-12-6
5. De La Cruz MS, Buchanan EM. Uterine fibroids: diagnosis and treatment. Am Fam Physician. 2017;95(2):100–107.
6. Evans P, Brunsell S. Uterine fibroid tumors: diagnosis and treatment. Am Fam Physician. 2007;75(10):1503–1508.
7. Lewis TD, Malik M, Britten J, San Pablo AM, Catherino WH. A comprehensive review of the pharmacologic management of uterine leiomyoma. Biomed Res Int. 2018;2018:2414609. doi:10.1155/2018/2414609
8. Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114. doi:10.2147/IJWH.S51083
9. MYFEMBREE®. Prescribing information. Myovant Sciences Inc; 2021. Available from: https://www.myovant.com/wp-content/uploads/2023/01/Approved-MYFEMBREE-PI-and-PPI_27January2023.pdf.
10. ORIAHNN. Prescribing information. AbbVie Inc; 2020. Available from: https://www.rxabbvie.com/pdf/oriahnn_pi.pdf.
11. Al-Hendy A, Lukes AS, Poindexter AN, et al. Treatment of uterine fibroid symptoms with relugolix combination therapy. N Engl J Med. 2021;384(7):630–642. doi:10.1056/NEJMoa2008283
12. Al-Hendy A, Stewart EA, Venturella R, Hunsche E, Zhao X, Lukes AS. Relugolix combination therapy improves bulk symptoms of uterine fibroids* through 24 week treatment. presented at: society of Endometriosis and Uterine Disorders (SEUD) Annual Congress. Athens: Greece; 2022.
13. Stewart EA, Lukes AS, Venturella R, et al. Relugolix combination therapy for uterine leiomyoma-associated pain in the LIBERTY randomized trials. Obstet Gynecol. 2022;139(6):1070–1081. doi:10.1097/AOG.0000000000004787
14. Bonine NG, Banks E, Harrington A, Vlahiotis A, Moore-Schiltz L, Gillard P. Contemporary treatment utilization among women diagnosed with symptomatic uterine fibroids in the United States. BMC Womens Health. 2020;20(1):174. doi:10.1186/s12905-020-01005-6
15. Stewart EA, Laughlin-Tommaso SK, Catherino WH, Lalitkumar S, Gupta D, Vollenhoven B. Uterine fibroids. Nat Rev Dis Primers. 2016;2:16043. doi:10.1038/nrdp.2016.43
16. McKain L, Edsall K, Dufour R, Lickert C. Treatment patterns in patients with uterine fibroids with and without a diagnosis of heavy menstrual bleeding: results from a large U.S. claims database. J Womens Health. 2022;32(3):332–340. doi:10.1089/jwh.2022.0056
17. Schlaff WD, Ackerman RT, Al-Hendy A, et al. Elagolix for heavy menstrual bleeding in women with uterine fibroids. N Engl J Med. 2020;382(4):328–340. doi:10.1056/NEJMoa1904351
18. Lee DW, Ozminkowski RJ, Carls GS, Wang S, Gibson TB, Stewart EA. The direct and indirect cost burden of clinically significant and symptomatic uterine fibroids. J Occup Environ Med. 2007;49(5):493–506. doi:10.1097/JOM.0b013e31805f6cf2
19. Fuldeore M, Yang H, Soliman AM, Winkel C. Healthcare utilization and costs among women diagnosed with uterine fibroids: a longitudinal evaluation for 5 years pre- and post-diagnosis. Curr Med Res Opin. 2015;31(9):1719–1731. doi:10.1185/03007995.2015.1069738
20. Artiga S, Latoya H, Orgera K, Damico A. Health coverage by race and ethnicity, 2010–2019. Kaiser Family Foundation. Available from: https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/.
21. United States Census Bureau. Quick facts. Available from: https://www.census.gov/quickfacts/US.
22. Soliman AM, Yang H, Du EX, Kelkar S, Winkel C. A systematic literature review of comorbidities and symptoms among uterine fibroids patients between 2000 and 2013. Value Health. 2016;19(2016):A172.
23. Fuldeore MJ, Soliman AM. Patient-reported prevalence and symptomatic burden of uterine fibroids among women in the United States: findings from a cross-sectional survey analysis. Int J Women's Health. 2017;9:403–411. doi:10.2147/IJWH.S133212
24. Uimari O, Jarvela I, Ryynanen M. Do symptomatic endometriosis and uterine fibroids appear together? J Hum Reprod Sci. 2011;4(1):34–38. doi:10.4103/0974-1208.82358
25. Freytag D, Gunther V, Maass N, Alkatout I. Uterine fibroids and infertility. Diagnostics. 2021;11:8. doi:10.3390/diagnostics11081455
26. Kinay T, Ozturk Basarir Z, Firtina Tuncer S, Akpinar F, Kayikcioglu F, Koc S. Prevalence of endometrial polyps coexisting with uterine fibroids and associated factors. Turk J Obstet Gynecol. 2016;13(1):31–36. doi:10.4274/tjod.36043
27. Faerstein E, Szklo M, Rosenshein NB. Risk factors for uterine leiomyoma: a practice-based case-control study. II. Atherogenic risk factors and potential sources of uterine irritation. Am J Epidemiol. 2001;153(1):11–19. doi:10.1093/aje/153.1.11
28. Charles H, Groenwald M. Comorbid medical conditions in women undergoing uterine artery embolization for symptomatic uterine fibroids and adenomyosis. J Vasc Interv Radiol. 2013;24(4):S152. doi:10.1016/j.jvir.2013.01.381
29. Wang A, Wang S, Owens CD, Vora JB, Diamond MP. Health care costs and treatment patterns associated with uterine fibroids and heavy menstrual bleeding: a claims analysis. J Women's Health. 2022;31(6):856–863. doi:10.1089/jwh.2020.8983
30. Duyar S, Tsai S, Milad MP, Chaudhari A. Attitudes and beliefs about hysterectomy in patients with uterine fibroids. J Minim Invasive Gynecol. 2023. doi:10.1016/j.jmig.2023.05.012
31. Wegienka G, Stewart EA, Nicholson WK, et al. Black women are more likely than white women to schedule a uterine-sparing treatment for leiomyomas. J Women's Health. 2021;30(3):355–366. doi:10.1089/jwh.2020.8634
32. American College of Obstetricians & Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112:387–400. doi:10.1097/AOG.0b013e318183fbab
33. Jacoby VL, Fujimoto VY, Giudice LC, Kuppermann M, Washington AE. Racial and ethnic disparities in benign gynecologic conditions and associated surgeries. Am J Obstet Gynecol. 2010;202(6):514–521. doi:10.1016/j.ajog.2010.02.039
34. Laughlin-Tommaso SK, Jacoby VL, Myers ER. Disparities in fibroid incidence, prognosis, and management. Obstet Gynecol Clin North Am. 2017;44(1):81–94. doi:10.1016/j.ogc.2016.11.007
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.