Back to Journals » Journal of Pain Research » Volume 17
Current Status of Cognition and Clinical Practice of Refractory Cancer Pain in Shanghai: A Questionnaire Survey
Authors Zhang J , Ma K, Yan J, Pan P, Yin J, Lin F, Chen H, Zhao W, Chen M, Zhang Z, Liu M, Gu X, Liao X , Zhang C, Cheng W
Received 19 December 2023
Accepted for publication 4 April 2024
Published 9 April 2024 Volume 2024:17 Pages 1413—1422
DOI https://doi.org/10.2147/JPR.S452605
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amitabh Gulati
Jing Zhang,1,2 Ke Ma,3 Jun Yan,4 Pingsheng Pan,5 Jiangshan Yin,6 Fuqing Lin,7 Hui Chen,8 Weiwei Zhao,1,2 Menglei Chen,1,2 Zhe Zhang,1,2 Minghui Liu,1,2 Xiaoli Gu,1,2 Xinghe Liao,1,2 Chenyue Zhang,1,2 Wenwu Cheng1,2
1Department of Integrated Therapy, Shanghai Cancer Center, Fudan University, Shanghai, People’s Republic of China; 2Department of Oncology, Shanghai Medical College, Fudan University, Shanghai, People’s Republic of China; 3Department of Pain Medicine, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 4Department of Oncology, Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences, Shanghai, People’s Republic of China; 5Department of Oncology, Fangta Hospital of Traditional Chinese Medicine in Songjiang District, Shanghai, People’s Republic of China; 6Department of Oncology, Fudan University Shanghai Cancer Center, Minhang Branch, Shanghai, People’s Republic of China; 7Department of Anaesthesiology, Shanghai Tenth People’s Hospital, Tongji University School of Medicine, Shanghai, People’s Republic of China; 8Department of Anesthesiology and Perioperative Medicine, Shanghai Fourth People’s Hospital Affiliated to Tongji University School of Medicine, Shanghai, People’s Republic of China
Correspondence: Wenwu Cheng, Email [email protected]
Purpose: This study aimed to assess the current status of clinical practice of refractory cancer pain (RCP) among a sample of physicians specializing in cancer pain management in Shanghai.
Methods: From 2019 to 2021, a questionnaire survey was conducted among physicians engaged in diagnosis and treatment of cancer pain through the questionnaire WJX network platform in Shanghai, China.
Results: A total of 238 responses participated in the survey. This survey reports physicians’ understanding and incidence rate of breakthrough cancer pain (BTCP). The choice of analgesics and satisfaction of analgesic effect were investigated. We also investigated doctors’ knowledge of the diagnostic criteria for RCP and their tendency to choose analgesics. Oral immediate-release morphine and intravenous or subcutaneous morphine injection have been the common treatment approach for transient cancer pain exacerbations. The main barriers to pain management are lack of standardized treatment methods for RCP, lack of knowledge related to RCP, and single drug dosage form. Doctors believe the most necessary measures to improve the current situation of poor cancer pain control include improving medical staff’s understanding and treatment techniques for RCP, updating treatment techniques and methods, and improving the configuration of drug types in medical institutions. Clinicians expect to improve understanding and treatment techniques through systematic training.
Conclusion: Despite multiple available analgesic measures, the treatment of RCP remains challenging. Improving the understanding of medical staff towards RCP, improving treatment techniques, and increasing the accessibility of multiple drug types are important ways to improve the satisfaction of cancer pain management in the future.
Keywords: refractory cancer pain, breakthrough cancer pain, pain management, opioid drugs
Background
According to the International Agency for Research on Cancer (IARC) of the World Health Organization (WHO), there were 19.29 million new cancer cases worldwide in 2020, with 4.57 million new cases in China.1 More than half of cancer patients experience moderate-to-severe pain, and part of them felt that their cancer pain treatment is inadequate. Refractory cancer pain (RCP) has been described as persistent pain related to cancer or its treatment. RCP is difficult to respond to standard treatment with opioid drugs and co-analgesics.2 However, there is no standard definition recognized by international experts. The lack of international consensus on the definition of RCP in clinical practice may contribute to failures in pain management. According to reports, 10–20% of cancer patients suffer from RCP. RCP has become a thorny problem faced by both doctors and patients.3 RCP usually persists longer than three months and is associated with significant physical, psychosocial, and social implications. Poor pain control can result in increased healthcare costs, extended hospital stays, increased patient suffering, and decreased patient satisfaction. The reasons for poor pain control not only include the nature of the patient’s cancer pain itself but also include doctors’ insufficient perception of RCP, improper drug selection, and a lack of drug types, which have a significant impact on the effectiveness of pain relief. A generally accepted understanding of RCP is essential for future treatment. Medical staff should take the lead in implementation of evidence-based pain management strategies, to decrease patient suffering, decrease healthcare costs, and improve quality of life.
In order to gain insight into the current status of standardized treatment for RCP in Shanghai, we independently designed a survey questionnaire on the diagnosis and treatment status of RCP. We conducted a survey on medical staff engaged in oncology and related fields in Shanghai. The primary objective of the survey is to review and summarize the progress in the diagnosis and treatment of RCP. The secondary objective of the survey is to propose implementation suggestions for the management of RCP based on this. Our study reflects the current management status of RCP and provides a basis for improving cancer pain treatment.
Methods
Study Design
A questionnaire of 29 questions was developed about RCP. The detailed content is provided in the Supplementary Material 1. Wenwu Cheng, the leader of the expert group of Shanghai Alliance for Refractory Cancer Pain, directed the design of the questionnaire. Members of expert group of Shanghai Alliance for Refractory Cancer Pain participated in developing the relevant questions for questionnaire. They have been engaged in clinical diagnosis and treatment of cancer pain for more than ten years and have rich clinical experience. We sent questionnaires to oncologists, pain specialists (PSs), palliative care specialists (PCSs), general practitioners (GPs), and geriatric specialists (GSs) engaged in cancer pain treatment in Shanghai, China, and collected data reported by physicians from 2019 to 2021. A total of 238 physicians from multiple medical centers voluntarily filled out our questionnaire, which took an average of 506 seconds to complete. All participants have voluntarily provided information and given informed consent. All participants are informed that all survey information will be kept absolutely confidential and personal privacy will never be disclosed. Our study is a non-interventional study (a questionnaire survey) and has been performed in accordance with the principles stated in the Declaration of Helsinki. Our study has been granted an exemption by the ethics committee of the Institutional Review Board of Shanghai Cancer Center, Fudan University.
The questionnaire consists of three parts. The first part is about the general situation of medical personnel, including name and category of hospital, working years, professional title, department categories, number of cancer pain patients, etc. The second part is related knowledge and treatment management of breakthrough cancer pain (BTCP), including general knowledge, drug use, and efficacy evaluation of BTCP. The third part is to investigate the general knowledge of RCP and analyze the causes of poor pain control, especially the diagnosis, treatment habits, and expected improvements in RCP management. The electronic version of the questionnaire is distributed and recycled through WJX and WeChat network platform.
Statistical Analysis
We used descriptive statistical data, including percentages, to describe the characteristics of participants and their responses to the questionnaire. The average comprehensive score of the ranking questions is automatically calculated by the questionnaire star rating system based on the ranking of all respondents’ options. It reflects the comprehensive ranking of the options, and the higher the score, the higher the comprehensive ranking. The option average comprehensive score = (Σweight×frequency)/number of respondents. The weight is determined by the order in which the options are arranged.
Results
Characteristics of Physicians
Among the physicians surveyed by the questionnaire, 23 (9.66%) come from cancer specialist hospitals, 92 (38.66%) work in tertiary levels of general hospitals, 67 (28.15%) work in secondary levels of general hospitals, and 56 (23.53%) work in primary levels of general hospitals. About half of the physicians who responded to the survey come from oncology department. About 39.5% of physicians come from departments with more than 40 open beds. Most physicians have more than 10 years of experience in cancer pain treatment, and 95 (39.92%) of them have senior professional title. The specific characteristics of responders are listed in Table 1. According to clinicians’ recollection, 123 (51.68%) report that they treat more than 10 cancer pain patients per month on average. Regarding the proportion of patients receiving sufficient analgesia, 9 (3.78%) chose “100%”, 102 (42.86%) chose “>80%”, 83 (34.87%) chose “50%−80%”, 33 (13.87%) chose “20%−50%”, and 11 (4.62%) considered “≤20%”. In addition, 90.34% of physicians report that 1–5 patients receiving analgesic treatment every month were diagnosed with RCP (Table 1).
 |
Table 1 Characteristics of Physicians |
General Knowledge of BTCP
The definition of BTCP is described as “a brief pain attack that occurs on a relatively well-controlled baseline pain background”. The typical intensity of BTCP attacks is moderate to severe, with rapid onset (minutes) and relatively short duration (median of 30 minutes).4 Most physicians (209/87.82%) participating in the survey provided the best option on the definition of BTCP, indicating that physicians engaged in cancer pain diagnosis and treatment in Shanghai have a comprehensive understanding of BTCP. The reported prevalence variability is dependent on the definitional criteria and ranges from approximately 40% to 80%.5 The physicians in our survey are required to reported the proportion range of BTCP among the analgesic patients they treated. A total of 109 (45.8%) of them reported incidence rate of 25% and below, 36 (15.13%) reported incidence rate of 75%–50%, 36 (15.13%) of them reported incidence rate of 75%–50%, and 6 (2.52%) reported 100–75% (Table 2).
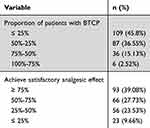 |
Table 2 Quantitative Results of Survey Responses About BTCP |
When it comes to BTCP, rescue medicines should be used. Opioids are the preferred drugs for exacerbating cancer pain.6,7 Oral morphine is usually recommended as a first-line treatment for moderate to strong cancer pain, and oral oxycodone or oral hydromorphone is an effective alternative.8,9 For severe cancer pain that requires rapid relief, parenteral approaches should be used, and intravenous administration can provide the most immediate effect.9 Patients can also use patient-controlled analgesic devices to administer parenteral opioids.10 According to our survey, “oral morphine immediate-release tablets” and “intravenous or subcutaneous morphine injection” are the most recognized options for clinicians to treat BTCP (Figure 1). Due to the strong neurotoxicity of pethidine hydrochloride, WHO has explicitly proposed that pethidine hydrochloride should not be used as a treatment for moderate-to-severe cancer pain. We found that 6.72% of clinicians still choose to use pethidine hydrochloride. We further investigated the level of satisfaction of physicians with pain relief effects, and found that only 39.08% of them believed that their patients had achieved satisfactory analgesic effect, while 33.91% chose less than 50% satisfied (Table 2). These data indicate that we still need to further standardize the rational use of analgesic drugs.
 |
Figure 1 Therapeutic measures commonly used in the treatment of patients with BTCP (multiple choices available). |
General Knowledge and Treatment Management of RCP
Cancer pain belongs to a mixed type of pain, characterized by both nociceptive and neuropathic pain. The main mechanisms of pain caused by tumors or treatment are as follows: 1) Direct damage to sensory nerves; 2) Tumor and surrounding inflammatory cells release inflammatory factors such as tumor necrosis factor-α etc; 3) Invasion and destruction of blood vessels causing ischemia, invasion of hollow organs causing obstruction, or invasion of parenchymal organs causing excessive capsule tension. The continuous growth of tumors causes acute pain to persist and is prone to peripheral or (and) central sensitization. According to our survey, 208 (87.39%) physicians consider “refractory pain has a complex condition and poor drug efficacy” as a common factor for poor pain control in cancer pain patients. More than 50% of physicians also choose “limited drug options”, “worried about drug addiction” and “inadequate patient education” (Figure 2).
 |
Figure 2 Factors of poor pain control in cancer pain patients (multiple choices available). |
At present, there is no unified global definition and diagnostic criteria for RCP. In China, the diagnosis of RCP usually needs to meet the following criteria: 1) Continuous pain digital score ≥4 points and/or the number of BTCP ≥ 3 times per day; 2) Following relevant cancer pain treatment guidelines, patients may experience unsatisfactory pain relief and/or intolerable adverse reactions after 1–2 weeks of treatment with opioid drugs alone or in combination with adjuvant analgesics. In order to perceive the general knowledge of physicians about RCP and treatment practice, we have set up relevant questions about RCP. Only 37.39% of physicians believe that they fully grasp the relevant knowledge of RCP. About 59.24% expressed partial understanding and 3.36% reported not clear. Among those surveyed, 70.17% of physicians informed that they have been trained in knowledge related to RCP. Regarding the multiple-choice question for diagnosing RCP, only 64 physicians (26.89%) selected all 4 options we provided. About 92.44% of them chose “moderate to severe pain caused by the tumor itself or factors related to tumor treatment, with unsatisfactory pain relief and/or intolerable adverse reactions after 1–2 weeks of standardized drug treatment”; 35.71% of them chose “after standardized drug treatment, the pain has been basically relieved, but the adverse reactions are intolerable”; 58.82% of them chose “failure to alleviate pain and/or intolerable adverse reactions after standardized drug treatment”; 63.87% of them chose “continuous pain digital score ≥4 points and/or number of BTCP ≥ 3 times/day”; 3 (1.26%) physicians chose “unclear” (Figure 3). We further inquire which of the following clinical situations can be considered as RCP. The options and selection scale are listed in Figure 4. Due to the unclear standard definition, doctors have inconsistent perspectives of the clinical scenarios of RCP. These results indicate that clinicians have not yet formed a unified understanding of RCP in clinical practice.
 |
Figure 3 Options and selection scale of the question “Which of the following situations do you think may be diagnosed as RCP” (multiple choices available). |
 |
Figure 4 Options and selection scale of the question “Which of the following situations belongs to RCP” (multiple choices available). |
The common clinical types of RCP include cancerous neuropathic pain, cancerous visceral pain, bone metastatic cancer pain, and BTCP. A total of 121 (50.84%) physicians recognized all 4 types above. The selection ratios for individual options are listed in Table 3. All doctors agree that effective analgesic measures are “highly necessary” or “necessary” for patients with RCP. Oral medication is the most common treatment method, followed closely by systemic administration combined with local treatment and patches (Table 3).
 |
Table 3 Quantitative Results of Survey Responses About RCP |
We require doctors to sequence the factors we provided that hinder effective management of RCP. Based on the ranking of each option by all respondents, we calculated a comprehensive priority score for each option, which reflects the importance of these factors from high to low (Table 4). The main barriers to pain management are lack of standardized treatment methods for RCP, lack of knowledge related to RCP, and a single drug dosage form. For another ranking question, “In order to improve the current situation of unsatisfactory cancer pain relief, what do you think is the most needed improvement at this stage?”, doctors believe that the most necessary measures to improve the current situation of poor cancer pain relief include improving medical staff’s understanding and treatment techniques for RCP, updating treatment techniques and methods, and improving the configuration of drug types in medical institutions (Table 5). We further require the surveyed doctors to select the training content options based on their needs. Clinicians expect to improve treatment methods and management of RCP through systematic training. In addition, pharmacological characteristics and rational drug selection of analgesic drugs are placed in an important position (Figure 5).
 |
Table 4 Comprehensive Priority Score for Factors That Hinder Optimal Pain Management of RCP |
 |
Table 5 Comprehensive Priority Score for the Most Needed Measures to Improve the Current Situation of Unsatisfactory Cancer Pain Relief |
 |
Figure 5 Options and selection scale of the knowledge that doctors hope to acquire through RCP training (multiple choices available). |
We care about the next step of treatment for cancer pain patients after receiving initial treatment. We asked the physicians surveyed the following question: “Among the patients currently diagnosed and treated, where will patients with RCP go in the later stages?” More than 60% of physicians choose “refer to a hospital department with specialized treatment techniques” and “receive treatment in their own hospital or undergraduate department” (Figure 6). Regarding the role of family participation in controlling cancer pain, 98.74% physicians in our survey believe that the diagnosis and treatment of RCP requires the participation of family members. Only 1.26% believe that family participation is not essential.
 |
Figure 6 Options and selection scale of patients’ subsequent treatment (multiple choices available). |
Discussion
The physicians in our research have long-term experience in clinical practice of cancer pain. They are often troubled by RCP. Although we currently have multiple methods to achieve rapid pain relief, the satisfaction with RCP treatment still needs to be improved. The characteristics that make cancer pain difficult to control include young age, neuropathic pain, incident pain, psychological distress, previous use of opioids, high tolerance, history of addiction and cognitive impairment.11 According to reports, patients with mixed-type pain, high severity of pain, daily use of opioids, and poor emotional health have a poorer prognosis for cancer pain.11 Our survey shows that the complex condition of refractory pain and poor drug efficacy are the main factors for poor pain control in cancer patients. In addition to factors related to the patient’s pain nature, over 50% of physicians believe that other important factors leading to poor pain control are as follows: inadequate patient education, limited drug options, and concern about drug addiction.
A questionnaire survey reported four barriers in a Chinese general hospital in 2001. The main barriers to optimal management of cancer pain were inadequate assessment, excessive supervision of opioid drug prescriptions, insufficient knowledge of pain management, and a lack of access to potent analgesics.12 Breuer et al conducted an anonymous survey of medical oncologists to evaluate their attitudes, knowledge, and practices related to cancer pain management in the United States. The most important clinician-related barrier to pain management is physicians' reluctance to prescribe opioids and perceived excessive supervision.13 In our survey, doctors also ranked the importance of factors that hinder effective management of RCP. The top three barriers are lack of standardized treatment methods for RCP, lack of knowledge related to RCP, and a single drug dosage form.
The drug treatment of BTCP is supplemented with rapid-release opioid drugs on the basis of sustained release of opioids. In China, oral immediate-release morphine plays a leading role in the treatment of explosive pain. However, due to the peak analgesic activity occurring approximately 1 h after intake, patients can also choose to achieve rapid pain relief through non-gastrointestinal pathways such as subcutaneous or intravenous injection.
For patients with RCP, opioid therapy is the cornerstone and usually requires a combination of non-steroidal drugs and/or adjuvant analgesics based on different mechanisms of cancer pain. It is generally not recommended to use two or more opioid drugs simultaneously. Opioid drug conversion or a change in route of administration is required in the following cases: 1) pain control, but the patient experiences intolerable adverse reactions; 2) The satisfactory analgesic effect was not achieved by increasing the dosage, but the adverse reactions increased. In recent years, the development of various minimally invasive interventional treatment technologies has provided an effective solution for the treatment of RCP. Commonly used technologies include patient-controlled analgesia pump technology, nerve damage surgery, percutaneous vertebroplasty, radioactive particle implantation, and intrathecal drug infusion system implantation.
Although clinical physicians have extensive experience in cancer pain treatment, about a quarter of them perceive that the ideal treatment effect has not been achieved. From the answers to the ranking questions shown in Tables 4 and 5, lack of knowledge and treatment methods related to RCP among medical personnel is an urgent problem to be solved in clinical practice. Limitations in oncologists’ knowledge and practice in pain management may be contributing to the substantial unmet needs of cancer patients.
This study reflects the current management status of RCP through a questionnaire survey of oncology-related professionals in Shanghai, China, in order to promote the development of standardized treatment of cancer pain and chronic disease management. Chinese medical personnel have accumulated experience in pain relief practices, and the overall treatment level of cancer pain has significantly improved. However, the diagnosis and treatment of RCP remains a weak point in China, and there are still many areas that need improvement. We propose improvements in the following aspects: Accelerate the establishment of a professional team for cancer pain treatment; Strengthen the training of physicians and improve the treatment level for RCP; Ensure the long-term supply of analgesics through policies and systems.
Disclosure
The authors declare no competing interests in this work.
References
1. Wild CP, Weiderpass E, Stewart BW. World cancer report: cancer research for cancer prevention. Lyon, France: International Agency for Research on Cancer; 2020. Available from: https://publications.iarc.fr/586.
2. Currow DC, Spruyt O, Hardy J. Defining refractory pain in cancer for clinicians and researchers. J Palliat Med. 2012;15(1):5–6. doi:10.1089/jpm.2011.0326
3. Hardy J, Quinn S, Fazekas B, et al. Double-blind, placebo-controlled study to assess the efficacy and toxicity of subcutaneous ketamine in the management of cancer pain. J Clin Oncol. 2012;30(29):3611–3617. doi:10.1200/JCO.2012.42.1081
4. Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence, and characteristics. Pain. 1990;41(3):273–281. doi:10.1016/0304-3959(90)90004-W
5. Deandrea S, Corli O, Consonni D, Villani W, Greco MT, Apolone G. Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. J Pain Symptom Manage. 2014;47(2):57–76. doi:10.1016/j.jpainsymman.2013.02.015
6. Davies AN, Elsner F, Filbet MJ, et al. Breakthrough cancer pain (BTcP) management: a review of international and national guidelines. BMJ Support Palliat Care. 2018;8(3):241–249. doi:10.1136/bmjspcare-2017-001467
7. World Health Organization. WHO Guidelines for the Pharmacological and Radiotherapeutic Management of Cancer Pain in Adults and Adolescents. Geneva: World Health Organization; 2018.
8. Fallon M, Giusti R, Aielli F, et al. Management of cancer pain in adult patients: ESMO clinical practice guidelines. Ann Oncol. 2018;29(Suppl 4):iv166–iv191. doi:10.1093/annonc/mdy152
9. George B, Minello C, Allano G, Maindet C, Burnod A, Lemaire A. Opioids in cancer-related pain: current situation and outlook. Support Care Cancer. 2019;27(3):3105–3118. doi:10.1007/s00520-019-04828-8
10. Nijland L, Schmidt P, Frosch M, et al. Subcutaneous or intravenous opioid administration by patient-controlled analgesia in cancer pain: a systematic literature review. Support Care Cancer. 2019;27(1):33–42. doi:10.1007/s00520-018-4368-x
11. Fainsinger RL, Nekolaichuk CL. A “TNM” classification system for cancer pain: the Edmonton Classification System for Cancer Pain (ECS-CP). Support Care Cancer. 2008;16(6):547–555. doi:10.1007/s00520-008-0423-3
12. Yu S, Wang XS, Cheng Y, Yang J, Cleeland CS. Special aspects of cancer pain management in a Chinese general hospital. Eur J Pain. 2001;5(Suppl A):15–20. doi:10.1053/eujp.2001.0274
13. Breuer B, Fleishman SB, Cruciani RA, Portenoy RK. Medical oncologists’ attitudes and practice in cancer pain management: a national survey. J Clin Oncol. 2011;29(36):4769–4775. doi:10.1200/JCO.2011.35.0561
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
