Back to Journals » Nature and Science of Sleep » Volume 12
Cross-Sectional Survey of Sleep Practices of Australian University Students
Authors Batten R, Liddiard K , Raynor AJ , Brown CA , Stanley M
Received 1 July 2019
Accepted for publication 25 December 2019
Published 22 January 2020 Volume 2020:12 Pages 39—48
DOI https://doi.org/10.2147/NSS.S221472
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Steven A Shea
Rachel Batten,1,* Katrina Liddiard,1,* Annette J Raynor, 1,* Cary A Brown, 2,* Mandy Stanley 1,*
1School of Medical and Health Sciences, Edith Cowan University, Joondalup, WA, Australia; 2Department of Occupational Therapy, Faculty of Rehabilitation Medicine, University of Alberta, Edmonton, AB T6G2G4, Canada
*All authors contributed equally to this work
Correspondence: Rachel Batten
School of Medical and Health Sciences, Edith Cowan University, 270 Joondalup Drive, Joondalup, WA 6027, Australia
Tel +61 8 6304 3657
Email [email protected]
Background and Aim: Sleep insufficiency is often associated with the life of a university student, yet it is well known that inadequate sleep can have a negative impact on physical and mental health and be detrimental to cognitive skills for learning. The aim of this study was to replicate a Canadian study to survey university student sleep practices, the way in which students address any sleep issues, and the students’ preferred method to receive targeted sleep information.
Methods: An anonymous on-line survey was promoted to all enrolled students at one Australian University in August 2017.
Results: In total, 601 students responded to the survey. One third indicated that they had insufficient sleep (less than 6.5 hrs). Almost two thirds reported a perception of not getting sufficient sleep. There was a significant association between the reported number of sleep hours, and the perception of high-quality sleep. Strategies to get to sleep included the use of social media which is counter to best practice in sleep hygiene.
Conclusion: The study supports the need for education about sleep health coupled with stress management to better the demands of student life.
Keywords: higher education, college, tertiary education, sleep
Introduction
Insufficient sleep is accepted by many as an apparently unavoidable part of university student life.1–5 It is questionable, however, whether students fully comprehend the negative consequences of sleep deficiency on physical wellbeing, emotional health, and their capacity for critical cognitive skills such as learning, memory, and problem-solving.1,2 In higher education students, sleep deficiency has been linked to risk-taking behaviours, depression, anxiety, and decreased self-efficacy,2,3,6 substance misuse,3 excessive alcohol and caffeine consumption,7,8 and high rates of social media use.9 Insufficient sleep has also been shown to increase the long-term risk of chronic diseases such as heart disease and diabetes,10 and is increasingly connected with neurodegenerative conditions such as dementia and Parkinson’s disease.11
Findings from the US Center for Disease Control revealed that more than one third of adults surveyed in the 2014 Behavioural Risk Factor Surveillance System indicated that they typically slept less than the recommended 7 hrs in a 24-hr period. This report suggested that public awareness of sleep is an ongoing need, and that public education should be addressed.12 The Australian Sleep Health Foundation study of sleep health in adults found that, overall, Australians’ social life, health and work effectiveness are impacted by their sleep behaviours and sleep problems.13 A 2014 study of first-year psychology students enrolled at an Australian university found that the majority reported sleeping 6–7 hrs per night or less,14 which may be a consequence of, or intensified by, the new roles and environment of higher education. Sleep habits of college students are known to be impacted by such factors as the developmental stage of life, shared housing environments, increased social and academic demands, and increased use of technology.10 However, students may also enter higher education with previous poor sleep habits or pre-existing sleep disorders (such as untreated sleep apnoea).
For some students new academic, social, financial and environmental pressures, combined with pre-existing sleep conditions and habits, may contribute to reduced resilience and overall coping. Students who are ill-informed about the relationship between sleep and cognitive ability may make poor choices and prioritize study and other activities over sufficient sleep. Unfortunately, students who sacrifice sleep actually place their ability to achieve academic success at risk.10 A number of studies have demonstrated a significant negative relationship between sleep and academic achievement, for example, in a sample of undergraduate students15 self-reported quality, and frequency, of sufficient sleep significantly predicted end-of-semester results. A multinational trial conducted across Australia, Canada and the Netherlands compared sleep risk factors and protective factors in adolescents, with reduced sleep for both Australian and Canadian participants being strongly associated with the time that students ceased use of the internet before sleep.16
Sleep deficiency is a modifiable risk factor for poor physical health, emotional distress and academic underperformance,10 yet many higher education students’ still report inadequate sleep. This may reflect a lack of understanding of the barriers that exist in seeking and achieving better sleep. The consequences of sleep deficiency in university students have a high personal and social cost; therefore, evidence-based intervention strategies are much needed. The American College Health Association-National College Health Assessment (ACHA-NCH) collects data from college/higher education students across Canada and the USA twice a year (ACHA). Although there is no comparable Australian database, it is reasonable to assume that the findings from the ACHA-NCH’s assessment of student sleep habits, insomnia, and the outcomes of sleep deficiency, provide relevant data to better understand the potential issues faced by Australian university students. For example, 22% of the Canadian students who participated in the survey in 2018 stated that sleep difficulties interfered with academic performance. Interestingly, while 33% had difficulty managing sleep problems, less than 5% reported that they were treated by a professional for insomnia. Almost two-thirds felt “tired, dragged out or sleepy” three or more days of the week, and 17% reported daytime sleepiness was a “big” or “very big” problem (ACHA-NCH).
Australia and Canada share some common historical and cultural influences and it may be that efforts to develop effective sleep interventions for higher education students can be shared. However, despite the similarities between Australia and Canada, differences in the university culture and environmental factors such as the amount of daylight hours and the climate conditions need to be considered. A greater understanding of the unique experiences of Australian university populations is therefore warranted to determine their sleep-related needs and inform any future interventions.
This study aimed to replicate the Canadian study with an Australian sample to identify students’ self-reported sleep quantity and sleep practices, preferred sources of advice for sleep problems, and students’ preferred format/medium to receive information about improving their sleep.
Materials and Methods
An anonymous online cross-sectional survey was adapted from the 2016 Canadian study17 and was administered using the commercial Fluid Survey software platform18 (acquired by Survey Monkey in Dec 2017 and no longer available). The original survey questionnaire was developed following a review of the literature which identified no existing tool to determine student sleep practices and was piloted with students and faculty for comprehension prior to use. Only minor adaptations were made for the Australian population. The study was conducted at an Australian University with a student population of just over 30,000 which included approximately 5600 international students from over 100 host countries, providing a culturally and ethnically diverse population. Participants were invited to participate through a news item that was placed on the student portal, with the news item and survey link available for 8 weeks from the beginning of August 2017. In Australia, this period represents the end of winter and the start of spring. No data were collected on the click rate to the successful completion of the survey however most students would access the student portal a number of times every day during the semester. Approval was gained from the relevant institutional Human Research Ethics committee (Approval number 12108) and was appraised as low risk. When students clicked on to the survey link they were presented with an information sheet and were asked to acknowledge consent by clicking on the link to begin answering the survey questions.
The survey gathered demographic data (age, gender, graduate/undergraduate category) and seven questions about sleep habits including usual location of sleeping, perceived hours of sleep per night (in categories 0–4.4 hrs, 4.5–6.4, 6.5–8, or more than 8 hrs), and perceived quantity of sleep (yes/no). Participants were also required to indicate using a 3-point scale (“always”—5 to7 nights/week; “often”—1 to 4 nights/week; “sometimes” <3 nights/month) how often they used a range of specified strategies, and to list any other personal strategies used to promote sleep. Free text responses were used to gather data about help-seeking behaviours for perceived sleep problems, and how they preferred to receive additional sleep information.
Data were exported to SPSS Version 23 and analysed using descriptive statistics, with Pearson chi-square statistics used to determine the associations between demographic variables and the variables related to sleep amounts, help-seeking behaviours, and self-help behaviours. The level of significance was set at p=0.05. Free text responses were analysed using content analysis19 with responses coded into categories using keywords by the first author (RB) and checked by another author (MS).
Results
A total of 601 participants (445 females, 145 males, 10 others) completed the survey with the most represented groups being undergraduate students (79%), females (74%) and those students less than 35 years old (77%). Sample demographics are presented in Table 1.
 |
Table 1 Sample Demographics |
Sleep Habits
The majority of students (92.3%) reported sleeping at their own home during the week with only 2.2% sleeping on campus (residential college), 1.2% sleeping at friend’s home and 4.3% reported sleeping at “other” locations. Participants were asked to report on their average hours of sleep per night by selecting one of four categories – less than 4.5 hrs, 4.5 to 6.4 hrs, 6.5 to 8 hrs and more than 8 hrs. The majority of the participants had between 6.5 and 8 hrs of sleep per night (56.7%), with only 10% having greater than 8 hrs per night. A large number of participants had less than 6.5 hrs, with 31% sleeping between 4.5 and 6.4 hrs per night, and an additional 2.3% sleeping less than 4.5 hrs per night. Participants were also asked to rate their perception of sleep quantity by indicating whether they perceived they had enough sleep using a yes/no response. Overall, almost two-thirds of the sample (63%) perceived that they did not get enough sleep. There was a significant association between the perception of sleep quantity and the numbers of hours of sleep that the participants reported that they slept (p < 0.01). The majority of the participants who reported sleeping more than 6.5 hrs perceived that this was enough sleep, including 45.5% of the 6.5 to 8 hrs group, and 85.0% of those who slept more than 8 hrs. Conversely, 90.9% of the 4.5 to 6.4 hr group, and 86.7% of those who had less than 4.5 hrs thought this was not enough. There was no significant association between the hours of sleep reported and the level of study (p =0.42). A summary table with a full distribution of responses is presented below in Table 2.
 |
Table 2 Sleeping Habits by Location, Amount and Perception of Quality |
Help-Seeking Behaviors
A total of 205 participants, representing 34.1% of the sample reported that they had sought help for a sleeping problem, ranging from 35.5% of those in the 6.5 to 8-hrs group, to 39.8% of those who slept between 4.5 and 6.4 hrs. There was no significant association between the number of hours of sleep and whether the participant sought help (df= 3, n =601, χ2=4.835, p=0.18). Participants were asked to indicate where they sought help and were able to choose multiple responses. The results from the people who sought help are presented in Table 3 showing that the most commonly utilized source of assistance was the doctor or general practitioner, with family, friends and colleagues also being frequently asked for assistance.
 |
Table 3 Sources of Assistance for Sleeping Problems: Reported Frequency of Sources |
Sleep Self-Help Behaviors
Participants were also asked to indicate “What, if anything, do you do to help you sleep?”, indicating whether they used this strategy, never, sometimes (less than 3 times per month), often (1 to 4 nights per week) or always (5 to 7 nights per week). Results presented in Table 4 show the number of participants who used the specific strategy at any time (Column A), which represents the sum of those who used this strategy sometimes, often or always. From this cohort of participants, the number (and percentage) of those who used the strategy “often” or “always” was calculated and presented in Column B. The percentage of participants within the anytime group who practiced the strategy always and often is then presented in Table 4, Column C. The five most popular strategies used by participants (Table 4, Column A) were reading a book, listening to music, watching television, adjusting the heat and using social media. While the range of strategies were diverse, there were some that when used, were used more regularly. These included smoking a cigarette, watching TV, taking sleep medications, using social media and using a sleep mask.
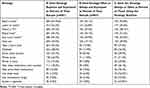 |
Table 4 Student Endorsed Sleep Strategies, Presented as Frequency and Percentage Within Total Sample, and Percentage of Those Who Used the Strategy |
There were no significant associations between the level of study and the self-help strategy adopted (p > 0.67). In terms of age, there was a significant association for a range of strategies including reading a book (df = 9, n = 601, χ2 = 17.71, p = 0.0r), music, (df = 9, n = 601, χ2 = 32.24, p < 0.01), use of social media (df = 9, n = 601, χ2 = 38.67, p < 0.01), adjusting the heating (df = 9, n = 601, χ2= 17.40, p = 0.04), use of alcohol (df = 9, n =601, χ2= 35.563, p = 0.01), and having sex (df = 9, n = 601, χ2= 27.615, p < 0.01). Figure 1 shows the percentage of participants who used each of the above strategies often or always. As shown the younger age groups tended to use music and social media more frequently whereas older students (36–45 and older than 45) tended to prefer reading a book.
 |
Figure 1 Strategies used “often or always” by hours of sleep. |
There were significant associations between the hours of sleep and taking prescribed sleep medications (df = 9, n = 601, χ2 = 21.71, p = 0.01), over the counter sleep medications (df = 9, n = 601, χ2 = 24, p < 0.01), and using alcohol (df = 9, n = 601, χ2 = 22.4, p < 0.01). Those who slept less than 4.5 hrs per night were more likely to use those strategies (see Figure 2).
 |
Figure 2 Strategies used “often or always” by age. |
Other Sleep Strategies
There were 191 text responses to the “other” category for the sleep strategy question (Table 5). Some of the responses were similar to available response options, as reported in Table 3 with some participants reporting more than one strategy. The five most popular strategies used by students in the “other” category were electronic media activity (games, reading, scrolling); changing the sleep environment (earplugs to avoid noise, darkening the room); prayer or mindfulness practice; having a warm beverage and/or snack; and using complementary and alternative medicine or diet, as shown in Table 5.
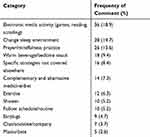 |
Table 5 Other Sleep Strategies Presented in Order of Popularity |
Perceived Need for Assistance Information and Preferred Format
The majority of participants (418/601, 69.5%) stated that they would be happy to receive information about sleep and sleep strategies. Some participants reported multiple options with a total of 436 responses recorded. The top three preferred methods identified were an email with information (273, 61.2%), a handout/booklet with the option of asking questions of the author (62, 13.9%), or a one-on-one session with a healthcare provider who knows about sleep (35, 7.8%).
Final Comments
The final question in the survey asked the question was there “Anything else you think we should know about students’ sleep?”. After excluding those responses stating that they had nothing to add and those with irrelevant content, there were 323 comments that students made about their sleep. From the content analysis there were 7 categories which are described below together with direct quotes from participants.
Stress (Academic Pressures)
More than two/thirds of the comments related to stress and the pressure associated with university work. Students commented on the impact of assignment deadlines, and exam pressures, on sleep quantity. As an example, one participant said, “The anxiety a lot of students experience in relation to studies is quite possibly a considerable contributor to poor sleep”. Respondents also commented that how much sleep they got often varied in relation to study demands. As one participant said, “When you are stressed, for instance a big paper and/or looming deadlines or exams, sleep at those times during the semester is difficult”. In addition to perceiving they did not have enough time to sleep, students also reported that thinking about assignments contributed to difficulty getting to sleep and staying asleep with comments including “the volume of reading can leave me feeling a bit overstimulated. Trying to get to sleep is not always easy, my mind is ticking over,” and, “I sometimes wake up thinking about university weekly tasks/assignments”.
Sleep as a Low Priority Amongst Competing Demands
Closely related to stress were comments about sleep being a low priority when balancing other commitments, including study, employment, social lives and family. For example, one participant stated that, “For many people, it (sleep) is not a priority but a luxury”. Another described sleep as the first casualty amongst competing demands; “Between full time study and work and other commitments, something has to give, and it’s usually sleep”. The perceived need to give up sleep to get things done was reflected in this comment; “A lot of students do all-nighters to get assignments done for deadlines”.
The need for engagement in leisure or social activities was also raised, with some students stating that they made choices which they know compromised sleep; “Social media keeps me awake! Quite often before bed people start messaging and I don’t want to miss out on a good conversation, even if I need to sleep” and
I can’t speak for others but as a mother of a 7 year old with a FIFO [fly in, fly out] husband, I find that late at night, reading in bed is the only ‘alone time’ I get. It’s precious and even though I can barely keep my eyes open and am tired, I push myself to keep reading and have that time.
The competing demand of having a young family whilst being a student was also highlighted, with comments identifying caring responsibilities for babies or young children as contributing to difficulty getting enough sleep.
Routine
Students also responded that there were several issues which impacted their ability to design routines which enabled them to get enough sleep. Inconsistency of routine as a consequence of peak study times in the semester, social activities, and employment were reported in comments such as, “[Sleep] is never consistent due to changing workload and social life”. Another wrote, “Some of us work late shifts, this can affect our sleep especially on days off when we have to adjust to a day schedule”. The timetabling of lectures and other classes was also mentioned with eight students commenting that they would prefer different class times; “Later lectures would help!” Another student commented on the combination of difficulty getting to sleep, travel to university and early class times; “I often cannot sleep until around 2AM and am required to attend 8.30AM lectures which mean I need to leave my house at around 5AM”.
Queries and Comments About Sleep Needs
A number of comments related to being tired and not getting enough sleep. In addition to this, some participants used this question to respond that they did not know how many hours they should actually be getting, or when they should be going to bed.
Physical and Mental Health
Respondents used this final question to report a range of physical and mental health conditions and related medications which they perceived significantly impacted on their sleep. While some students talked in broad terms, for example, “my mental health effects my sleep pattern and quality”, others were more specific; “I suffer from PTSD and nightmares related to that. I sometimes have to drive to uni. and attend class having had no sleep at all” and “I have type 1 diabetes and am sometime woken up during the night by hypoglycemic events which can leave me tired and sluggish in the morning”.
Sleep Environment and Exposure to Electronic Screens
A small number of comments related to the sleep environment and mentioned bedding, lighting, noise and disturbances by others as influencing their sleep, whilst others related to being lonely and “missing family”. One participant said that their sleep was impacted by being in “a crowded house or parents fighting loudly”. Another said that they needed a quiet environment to sleep in but that they often did not get this because “My roommates or flat mates come at weird times at night and most of the time this wakes me up”. Additional comments related specifically to the use of devices and screen time as potentially problematic. Comments such as “blue light in phones and other devices may cause sleep problems” suggested a level of awareness about the impact of exposure to electronic screens.
Other Factors Influencing Sleep
Remaining comments related to potential influencing factors including diet, exercise, napping, caffeine intake, and the use of mindfulness. For example, “Eating helps me to sleep better” and “Coffee! Too much coffee”.
Discussion
The key aim of this study was to better understand the sleep practices and strategies of higher education students at Edith Cowan University in Australia, the strategies used to get to sleep, and students’ preferred sources of information to help future development of targeted interventions. The study used an adapted version of the survey conducted by Brown et al17 of 1294 students at the University of Alberta, in Canada and results are similar in terms of sleep duration and strategies used by students to manage their sleep difficulties.
The results of this study are consistent with findings from similar studies outside of Australia [1–4, 10, 17]. It is evident that large numbers of tertiary students need support in addressing sleep issues, a finding which is supported by a recent sleep survey of sleep health in Australian adults,13 which found that many people, especially younger adults, sleep for much less than the average (7 hrs per night).13 Findings from the current study on the sufficiency of sleep are similar to the Adams et al study. Student participants were predominantly younger adults (91.5% under the age of 45%), and almost two thirds of these (63%) did believe they got enough sleep. In the Adams et al study, similarly high numbers of participants, in the categories under the age of 45, reported getting inadequate sleep (18–24 years 60.3%; 25–34 years 58.7%; 35–44 years 52.8%).13 The lack of sleep is a concern given the known associations between sleep, physical and emotional health and academic performance.
Respondents adopted multiple strategies for getting to sleep, some of which are supported within the literature, such as listening to music,20 adjusting the heat,21 or meditating.22 Other strategies, such as using social media, are contrary to the evidence-base,23,24 or were concerning due to their known detrimental effect on sleep and possible intermediate and long-term negative impact, such as drinking alcohol or taking recreational drugs.25–27 Some students used evidence-based environmental adjustments (for example, cooler, darker, and quieter sleep environments) however it is possible that not all students can control their sleep environment and therefore these strategies may not be accessible to them. However, the majority of students surveyed slept at home, which implies some level of control unlike many student commercial accommodation and residential settings. The survey did not ask participants to specify details such as whether they shared accommodation or sleep spaces with partners or children. Environmental issues such as noise and the presence of others were raised in the free-text responses and warrant a more detailed exploration.
The results of this Australian study showed similar results to the original Canadian study17 with regards to the top four strategies participants used for getting to sleep. In terms of other strategies used there were similarities including taking prescribed medications, using a sleep mask, using recreational drugs, and smoking cigarettes, with Canadian students being more likely to employ these strategies but major differences between the two countries with the use of white noise, or writing in a diary. The differences may be reflective of contextual differences which would need to be accounted for in any proposed interventions.
It appears that the education of students about sleep hygiene and effective strategies for getting to and staying asleep would be useful. With increased knowledge about effective strategies, there may be a decreased reliance on maladaptive strategies such as over-the-counter medication, alcohol use, and electronic device use at bedtime. It must be noted however that increased knowledge about sleep hygiene alone may not be effective as students still need to change behavior and behavioural change is not an automatic outcome of increased knowledge. For example, an Australian study of 257 undergraduate university students28 found that the likelihood of following through with planned good sleep hygiene behaviors is influenced both by students’ past behavior and their inability to refrain from responding to a range of demands including those of a social nature.
Results from this survey indicate that providing simultaneous information about stress management would be useful to increase sleep quantity. Whilst increased knowledge of sleep may be an important action out of this research, barriers to uptake of this information still exist. An Australian study of adolescents and young adults (80.5% of whom were full or part-time university students) found that participants were keen to improve their own sleep behaviour, but had seen little success in achieving this change.29 Whilst participants recognised one suitable strategy may be to minimise phone use, they reported becoming distracted by mobile phones and computers prior to sleep time. Technology use was a barrier to modification of behaviour, in particular, related to social media use and the need to maintain a social connection.29 Research evidence clearly supports that restorative sleep reduces the risk of anxiety, depression and suicidality.30,31 Supporting students' stress management through improving sleep efficiency is a positive health prevention activity that would be a useful inclusion to the suite of student well-being activities in any university.
As with all studies, this study had some limitations. The response rate was very low (2%) considering the size of the population and the method of recruitment. This study was conducted at one university in a capital city in Australia which may limit generalization to other Australian university students. The sample was comprised predominantly of under-graduate female students who were less than 35 years of age which may limit the utility of any intervention developed based on the findings from this study for graduate student populations. However, the results were very consistent with similar studies outside of Australia strongly suggesting that further development and testing of psycho-educational tools is warranted. The utility of the data was also limited by the structure of survey responses particularly in relation to categorical data on sleep duration however this was a replication study and the only amendments made to the survey before distribution were in relation to language expression to match an Australian sample.
Conclusion
Given what is already known about the strong links between inadequate sleep, poor academic performance and chronic health conditions, interventions to improve the amount of sleep for university students are required. These results suggest that there is a place for sleep interventions for university student populations drawing on the best available evidence for sleep hygiene, coupled together with broader approaches which will also empower students to better manage the stressors associated with higher education. There are a number of similarities in the sleep habits of the participants in this study and those of the earlier Canadian study. This presents an opportunity to jointly develop, and rigorously test in a suitably powered randomized control trial, psychoeducational materials with tailoring to the local contexts in terms of dissemination approach.
Data Sharing Statement
Data can be accessed at https://ro.ecu.edu.au/datasets/40/Doi:10.25958/5cc293b7045d1.
Acknowledgment
This study was supported by an internal university grant for covering the costs to publish in open access.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gaultney JF. The prevalence of sleep disorders in college students: impact on academic performance. J Am Coll Health. 2010;59(2):91–97. doi:10.1080/07448481.2010.483708
2. Hershner SD, Chervin RD. Causes and consequences of sleepiness among college students. Nat Sci Sleep. 2014;6:73. doi:10.2147/NSS.S62907
3. Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46(2):124–132. doi:10.1016/j.jadohealth.2009.06.016
4. Orzech KM, Salafsky DB, Hamilton LA. The state of sleep among college students at a large public university. J Am Coll Health. 2011;59(7):612–619. doi:10.1080/07448481.2010.520051
5. Boehm MA, Lei QM, Lloyd RM, Prichard JR. Depression, anxiety, and tobacco use: overlapping impediments to sleep in a national sample of college students. J Am Coll Health. 2016;64(7):565–574. doi:10.1080/07448481.2016.1205073
6. Augner C. Associations of subjective sleep quality with depression score, anxiety, physical symptoms and sleep onset latency in students. Cent Eur J Public Health. 2011;19(2):115–117. doi:10.21101/cejph.a3647
7. Patrick ME, Griffin J, Huntley ED, Maggs JL. Energy drinks and binge drinking predict college students’ sleep quantity, quality, and tiredness. Behav Sleep Med. 2018;16(1):92–105. doi:10.1080/15402002.2016.1173554
8. Van Reen E, Roane BM, Barker DH, McGeary JE, Borsari B, Carskadon MA. Current alcohol use is associated with sleep patterns in first-year college students. Sleep. 2016;39(6):1321–1326. doi:10.5665/sleep.5862
9. Afandi O, Hawi H, Mohammed L, et al. Sleep quality among university students: evaluating the impact of smoking, social media use, and energy drink consumption on sleep quality and anxiety. Inquiries J. 2013;5:06.
10. Owens H, Christian B, Polivka B. Sleep behaviors in traditional‐age college students: a state of the science review with implications for practice. J Am Assoc Nurse Pract. 2017;29(11):695–703. doi:10.1002/2327-6924.12520
11. Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci. 2010;11(8):589. doi:10.1038/nrn2868
12. Liu Y, Wheaton AG, Chapman D, Cunningham T, Lu H, Croft J. Prevalence of healthy sleep duration among adults - United States, 2014. Morb Mortal Wkly Rep. 2016;65:137–141. doi:10.15585/mmwr.mm6506a1
13. Adams RJ, Appleton SL, Taylor AW, et al. Sleep health of Australian adults in 2016: results of the 2016 sleep health foundation national survey. Sleep Health. 2017;3(1):35–42. doi:10.1016/j.sleh.2016.11.005
14. Lovato N, Lack L, Wright H. The napping behaviour of Australian university students. PLoS One. 2014;9(11):e113666.
15. Gomes AA, Tavares J, de Azevedo MHP. Sleep and academic performance in undergraduates: a multi-measure, multi-predictor approach. Chronobiol Int. 2011;28(9):786–801. doi:10.3109/07420528.2011.606518
16. Bartel K, Williamson P, van Maanen A, et al. Protective and risk factors associated with adolescent sleep: findings from Australia, Canada, and The Netherlands. Sleep Med. 2016;26:97–103. doi:10.1016/j.sleep.2016.07.007
17. Brown CA, Qin P, Esmail S. “Sleep? Maybe later … ” A cross-campus survey of university students and sleep practices. Educ Sci. 2017;7(3):66. doi:10.3390/educsci7030066
18. Surveys F. Online survey tools; 2016. Available from: www.fluidsurveys.com.
19. Bowling A. Research Methods in Health: Investigating Health and Health Services.
20. De Niet G, Tiemens B, Lendemeijer B, Hutschemaekers G. Music‐assisted relaxation to improve sleep quality: meta‐analysis. J Adv Nurs. 2009;65(7):1356–1364. doi:10.1111/jan.2009.65.issue-7
21. Lan L, Pan L, Lian Z, Huang H, Lin Y. Experimental study on thermal comfort of sleeping people at different air temperatures. Build Environ. 2014;73:24–31. doi:10.1016/j.buildenv.2013.11.024
22. Nagendra RP, Maruthai N, Kutty BM. Meditation and its regulatory role on sleep. Front Neurol. 2012;3:54. doi:10.3389/fneur.2012.00054
23. Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135(2):367–375. doi:10.1542/peds.2014-2306
24. Whipps J, Byra M, Gerow KG, Guseman EH. Evaluation of nighttime media use and sleep patterns in first-semester college students. Am J Health Behav. 2018;42(3):47–55. doi:10.5993/AJHB.42.3.5
25. Alamir YA, Zullig KJ, Wen S, et al. Association between nonmedical use of prescription drugs and sleep quality in a large college student sample. Behav Sleep Med. 2017;1–11.
26. Hall WD, Patton G, Stockings E, et al. Why young people’s substance use matters for global health. Lancet Psychiatry. 2016;3(3):265–279. doi:10.1016/S2215-0366(16)00013-4
27. Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–2233. doi:10.1016/S0140-6736(09)60746-7
28. Kor K, Mullan BA. Sleep hygiene behaviours: an application of the theory of planned behaviour and the investigation of perceived autonomy support, past behaviour and response inhibition. Psychol Health. 2011;26(9):1208–1224. doi:10.1080/08870446.2010.551210
29. Paterson JL, Reynolds AC, Duncan M, Vandelanotte C, Ferguson SA. Barriers and enablers to modifying sleep behavior in adolescents and young adults: a qualitative investigation. Behav Sleep Med. 2019;17(1):1–11. doi:10.1080/15402002.2016.1266489
30. Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi:10.5665/sleep.2810
31. Clarke G, Harvey AG. The complex role of sleep in adolescent depression. Child Adolesc Psychiatric Clin N Am. 2012;21(2):385–400. doi:10.1016/j.chc.2012.01.006
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
