Back to Journals » Nature and Science of Sleep » Volume 14
COVID-19 Related Emotional Stress and Bedtime Procrastination Among College Students in China: A Moderated Mediation Model
Received 29 April 2022
Accepted for publication 2 August 2022
Published 22 August 2022 Volume 2022:14 Pages 1437—1447
DOI https://doi.org/10.2147/NSS.S371292
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Yuhong Deng,1 Baojuan Ye,1 Qiang Yang2
1Center of Mental Health Education and Research, School of Psychology, Jiangxi Normal University, Nanchang, People’s Republic of China; 2School of Education, Jiangxi Normal University, Nanchang, People’s Republic of China
Correspondence: Baojuan Ye, Email [email protected]
Purpose: Although bedtime procrastination is prevalent during the COVID-19 pandemic, little is known about the relationship between COVID-19 related emotional stress and bedtime procrastination. Therefore, we investigated the correlation between COVID-19 related emotional stress and bedtime procrastination and examined the mediating role of negative affect and the moderating role of rumination among Chinese college students.
Methods: A multicenter, cross-sectional, and quantitative research was conducted in China from August 11, 2021, to August 27, 2021, during the COVID-19 pandemic. The sampling method used in the study is the convenience sampling method. A total of 913 college students (aged 18– 24 years) participated and completed online self-reported questionnaires. Their levels of COVID-19 related emotional stress, negative affect, rumination, and bedtime procrastination were measured by the Coronavirus Stress Measure, the Depression Anxiety Stress Scale, the Ruminative Responses Scale, and the Bedtime Procrastination Scale, respectively. The data were analyzed using Pearson correlations and moderated mediation analysis.
Results: COVID-19 related emotional stress was positively associated with bedtime procrastination. Meanwhile, the association could be mediated by negative affect (Effect = 0.33, Boot 95% CI = [0.26, 0.39]) and moderated by rumination (Effect = 0.05, Boot 95% CI = [0.03, 0.07]) through its moderation in the link between COVID-19 related emotional stress and negative affect. This indicated that the mediation effect of negative affect was stronger in college students with high levels of rumination than in those with low levels of rumination.
Conclusion: The findings of this study shed light on a correlation between COVID-19 related emotional stress and bedtime procrastination. Moreover, this study suggests that interventions could be targeted at alleviating negative affect and rumination to reduce the bedtime procrastination of college students with high levels of COVID-19 related emotional stress.
Keywords: COVID-19, emotional stress, bedtime procrastination, negative affect, rumination
Introduction
The novel coronavirus disease 2019 (COVID-19) pandemic has severely disrupted daily life around the world.1 Stress has been ubiquitous due to uncertainty about the future, health concerns, social isolation, home-schooling, and financial hardship.2,3 Combined with strict social distancing rules in many countries around the world, these multiple stressors have had tremendous impacts on mental health and sleep.4–6 Surveys conducted in several countries since the beginning of the pandemic, have reported an increased risk of post-traumatic stress disorder, fear, anxiety, and depression in different populations.7–12 Sleep problems in response to the COVID-19 pandemic are high in prevalence,13,14 as are psychological symptoms. Problems included poorer sleep quality, increased insomnia symptoms, and delayed bedtime and wake times,15,16 which were most common among women,17 youth,18 and individuals with poor social support and high pandemic-related stress.19
COVID-19 is a health threat identified as a significant stressor threatening individuals’ physical and mental health around the world.20–22 It is confirmed that perceived stress is a major obstacle to sleep,23,24 and sleep can be affected when exposed to unpredictable or uncontrollable stressors.25–27 According to the ego-depletion theory, prolonged exposure to stress would adversely affect individuals’ subsequent performance of self-regulatory behaviors, leading to procrastination.28–31 As a sleep-related procrastination, bedtime procrastination is defined as “going to bed later than intended while no external circumstances are accountable for doing so”.32 Bedtime procrastination turns out to be highly prevalent after the outbreak of COVID-19,33 having a significant effect on daytime fatigue,32 as well as the experience of insufficient sleep.34 Moreover, bedtime procrastination correlates with preclinical depressive symptoms of college students, which can be used to predict the occurrence of clinical depressive symptoms.35 A survey across different continents conducted during the pandemic exhibited that 89.8% of participants were going to bed after 10 p.m. on weekdays compared to 57.1% respectively before the pandemic, with these proportions being higher on weekends.36 Also, a study conducted during the pandemic revealed that participants went to bed, on average,1 h 13 min later on weekdays and 31 min later on weekends.15 Despite the prevalence of bedtime procrastination during the pandemic, there is no study in the literature on the linkage between COVID-19 related emotional stress and bedtime procrastination. Based on the ego-depletion theory and empirical evidence, we can therefore hypothesize a positive correlation between COVID-19 related emotional stress and bedtime procrastination (Hypothesis 1).
Studies have reported that COVID-19 related emotional stress can trigger mild to severe levels of psychosocial issues, such as depression, anxiety, and somatization.20,22,37,38 From the perspective of the stress response mechanism, individuals stimulated by stress may elicit relevant emotional responses.39 Expectedly, empirical studies have demonstrated that stress is positively related to negative affect.40,41 Moreover, negative affect is a harmful factor for sleep disorders.42 According to the internalization of conflicts model, negative affect leads to a high level of emotional arousal, which in turn provokes physiological hyper-arousal and causes the failure to fall asleep.43 As a sleep problem, bedtime procrastination has been found to be associated with negative affect.44,45 Based on the above, COVID-19 related emotional stress may correlate with negative affect, which in turn correlates with bedtime procrastination. Therefore, we hypothesized that negative affect would mediate the association between COVID-19 related emotional stress and bedtime procrastination (Hypothesis 2).
Rumination refers to the tendency of dwelling on one’s distress and its potential causes and consequences without any positive changes,46 which is a maladaptive response mode and a negative personal trait.47 The organism-environment interaction model indicates that the impact of environmental factors on individual’s psychosocial and social adaptation is affected by individual personality traits,48 that is, individual’s psychosocial and social adaptation is the result of the interaction between environmental factors and individual traits. In addition, the response style theory suggests that compared with low ruminators, high ruminators tend to repetitively think about the causes and potential adverse consequences of stressful events they encounter in life and fail to take constructive actions to tackle with, which increases the possibility of stressful life events triggering the negative affect such as anxiety and depression.49–51 Specifically, compared with individuals with low levels of rumination, individuals with high levels of rumination are more likely to repeatedly think before sleep after a stressful experience, which deepens the negative impact of stress-induced negative emotional responses. Numerous researches have confirmed the view of the organism-environment interaction model and response style theory. For example, studies have found that compared with low ruminators, the effect of negative life events on negative affect is stronger in high ruminators.52 As rumination intensifies the impact of the stressful events on negative affect, the adverse effects of COVID-19 related emotional stress may be more significant in students with high rumination. Therefore, we hypothesized that the impact of COVID-19 related emotional stress on negative affect was moderated by rumination, and the mediating effect was stronger in students with high levels of rumination when compared to those with low levels of rumination (Hypothesis 3).
Bedtime procrastination is a relatively new concept. Thus, literature on this topic is scarce. To our knowledge, few of the published studies have tried to explore the relationship between COVID-19 related emotional stress and bedtime procrastination. Considering its high prevalence and adverse outcomes, exploring the occurrence mechanism of bedtime procrastination is crucial for prevention and intervention. Thus, the purpose of the current study was to explore the psychological mechanism between COVID-19 related emotional stress and bedtime procrastination among Chinese college students. We aimed to test whether negative affect would mediate the relation between COVID-19 related emotional stress and bedtime procrastination, and whether the relationship between COVID-19 related emotional stress and negative affect was moderated by rumination. Better solutions to the sleep problems of college students with high levels of COVID-19 related emotional stress may be implied by answering the research questions of our study. The relations are illustrated in Figure 1.
 |
Figure 1 The proposed moderated mediation model. |
Materials and Methods
Procedure
The research is cross-sectional and quantitative research. Participants were recruited from different universities in different regions of China such as Jiangxi, Hunan, Anhui province, etc. The research was conducted from August 11, 2021 to August 27, 2021, during the COVID-19 pandemic. The sampling method used in the study is the convenience sampling method. We collected primary data on the Questionnaire Star (an online survey platform) by disseminating questionnaires to participants through the WeChat or QQ groups (online social media platforms). As the majority of the population was home isolated, students participated in the survey from various regions of China. The inclusion criteria for participants were as follows: 1) college students; 2) using social media; 3) they volunteer to participate in the study. A total of 936 students were initially approached. After excluding unqualified samples (eg, answering regularly, such as responding “1” to all items; failing an attention check question), we finally collected 913 valid questionnaires with an effective response rate of 97.54%. Because only completed responsive questionnaires could be recorded, there were no missing data. The survey was approved by the Research Ethics Committee of the Jiangxi Normal University of China (The ethics review approval code is IRB-JXNU-PSY-2020002). All participants signed informed consents online prior to participating in the study and were informed that their personal information would be confidential. Participation in this study was entirely voluntary and participants could exit the survey at any time. Thus, no compensation was given to them. This study complied with the Declaration of Helsinki.
Participants
A total of 913 Chinese college students (M age = 19.72, SD = 1.24, range = 18–24, 54% female) were included in this study. The participants consisted of 217 (23.77%) freshmen, 391 (42.83%) sophomores, 237 (25.96%) juniors, and 68 (7.44%) seniors. The sample size required for a study depends on many factors. Fritz and MacKinnon provided researchers with sample size requirements for various combinations of parameters in the single mediator model, and they showed that if small mediated effects are to be detected, the sample size requirement is 462 for bias-corrected bootstrap test.53 Considering that the moderated mediation model in this paper is more complex than the simple mediation model, we use a larger sample size in this study. Using G*Power 3.1,54 a post hoc power analysis revealed that the sample size of this study was adequate to attain a power of 1 (effect size = 0.25, α = 0.05).
Materials
Coronavirus Stress Measure
The Chinese version55 of the Coronavirus Stress Measure56 was used to assess COVID-19 related emotional stress. The scale consists of 5 items (eg, “How often have you been upset because of the COVID-19 pandemic?”). All items were measured on a 5-point Likert scale (0 = never, 4 = always), and higher total scores indicate higher levels of COVID-19 related emotional stress. In the present study, the Cronbach’s alpha of the scale was 0.96.
Depression Anxiety Stress Scale
The Chinese version57 of the Depression Anxiety Stress Scale58 was used to assess participants’ levels of negative affect.59 The scale contains 21 items (eg, “I found it hard to wind down.”). All items were measured on a 4-point Likert scale (0 = never, 3 = often or always), and higher total scores indicate higher levels of negative affect. In the present study, the Cronbach’s alpha of the scale was 0.98.
Ruminative Responses Scale
The Chinese version60 of the Ruminative Responses Scale46 was used to assess participants’ levels of rumination. It consists of 22 items (eg, “Think ‘why do I have problems other people don’t have’?”). All items were measured on a 4-point Likert scale (1 = never, 4 = always), and higher total scores indicate higher rumination. In the present study, the Cronbach’s alpha of the scale was 0.98.
Bedtime Procrastination Scale
The Chinese version61 of the Bedtime Procrastination Scale32 was used to assess participants’ propensity to unnecessarily delay their bedtimes. The scale consists of 9 items (eg, “I go to bed later than I would like to”) and all items were measured on a 5-point Likert scale (1 = never, 5 = always). Responses to all items were averaged, and higher total scores indicate more bedtime procrastination behaviors. In the present study, the Cronbach’s alpha of the scale was 0.80.
Statistical Analyses
First, descriptive statistics and Pearson correlations analyses were conducted to investigate the correlation between COVID-19 related emotional stress, negative affect, rumination, and bedtime procrastination. Second, we used Model 4 of the Hayes PROCESS macro to examine the mediation effect of negative affect. Bootstrapping (5000 bootstrap samples) with 95% confidence intervals (CIs) was conducted to test the significance of indirect effects.62 The 95% CIs did not include zero, indicating a significant effect. Third, Model 7 of the Hayes PROCESS macro was used to test whether rumination moderated the mediation process. The 95% CIs did not include zero, indicating a significant moderation effect. Finally, simple slope tests were performed to demonstrate the interaction patterns, and significant moderation effects were probed at plus and minus one standard deviation from the mean of the predictor variables. All variables were standardized prior to being analyzed and all data were analyzed using SPSS Statistics 22.0.
Result
Preliminary Analysis
Descriptive statistics and Pearson correlations among the study variables are presented in Table 1. As expected, COVID-19 related emotional stress was positively correlated with bedtime procrastination and negative affect. Rumination was positively associated with negative affect. Therefore, hypothesis 1 was supported.
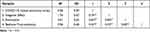 |
Table 1 Descriptive Statistics and Correlations of Study Variables |
Mediation Analysis
Hypothesis 2 assumed that negative affect would mediate the relation between COVID-19 related emotional stress and bedtime procrastination. To test this hypothesis, we used Model 4 of the PROCESS macro.62 Table 2 showed that COVID-19 related emotional stress was positively related to bedtime procrastination (β = 0.44, p < 0.001) and negative affect (β = 0.72, p < 0.001) after controlling for gender. When controlling for COVID-19 related emotional stress, negative affect was positively related to bedtime procrastination (β = 0.45, p < 0.001). Bootstrapping indicated that the mediation effect of negative affect was significant (ab = 0.33, Boot SE = 0.03, Boot 95% CI = [0.26, 0.39]), and it accounted for 73.95% of the total effect. Taken together, negative affect mediated the relationship between COVID-19 related emotional stress and bedtime procrastination. Hence, hypothesis 2 was supported.
 |
Table 2 Testing the Mediation Effect and the Moderated Mediation Effect of COVID-19 Related Emotional Stress on Bedtime Procrastination |
Moderated Mediation Analysis
Hypothesis 3 proposed that the relationship between COVID-19 related emotional stress and negative affect would be moderated by rumination. To test this hypothesis, we used Model 7 of the PROCESS macro.62 Controlling for gender, Table 2 showed the interaction between COVID-19 related emotional stress and rumination. Results showed a significant, positive interaction between COVID-19 related emotional stress and rumination on negative affect (β = 0.05, p < 0.001), suggesting that rumination moderated the effect of COVID-19 related emotional stress on negative affect. Figure 2 showed the interaction effect graphically. Simple slope tests showed that, COVID-19 related emotional stress were positively associated with negative affect for both students with low (Z = −1, βsimple = 0.25, t = 9.03, p < 0.001) and high (Z = 1, βsimple = 0.35, t = 16.74, p < 0.001) levels of rumination, but the correlation was significantly stronger in the latter.
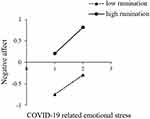 |
Figure 2 The moderation effect of rumination. |
The bias-corrected percentile bootstrap analysis further indicated that rumination moderated the mediating effect. For college students with high rumination, the indirect effect of negative affect on COVID-19 related emotional stress and bedtime procrastination association was stronger (β = 0.15, SE = 0.02, Boot 95% CI= [0.12, 0.19]) than those with low rumination (β = 0.11, SE = 0.02, Boot 95% CI = [0.07, 0.15]). Thus, hypothesis 3 was supported.
Discussion
This study explored the relationship between COVID-19 related emotional stress and bedtime procrastination in college students and tested the internal mechanism of formation and deterioration. The results showed that COVID-19 related emotional stress was not only directly related to bedtime procrastination, but also indirectly correlated with bedtime procrastination by the mediating variable of negative affect, and the indirect effect of this model was moderated by rumination. Further, the mediation effect of negative affect was stronger for those students with higher levels of rumination than for those with lower levels of rumination. During the pandemic crises, international research revealed several negative effects of the lockdown on mental health and were associated with emotional strains such as stress, fear, depression, and anxiety, as well as sleep disturbance.2,10,12,36,63,64 Similarly, results from Chinese studies indicated that the COVID-19 outbreak engendered anxiety, depression, sleep disturbances, and other psychological issues.65 With the impact of the COVID-19 pandemic on negative affect and bedtime procrastination of Chinese college students, the present findings supported these suggestions from the literature and highlight that the COVID-19 outbreak is a common risk factor for mental health and sleep problems across different populations and contexts.14,66–69
The Relationship Between COVID-19 Related Emotional Stress and Bedtime Procrastination
First, the study found that COVID-19 related emotional stress was related to bedtime procrastination. It was consistent with existing research, indicating that lockdown was associated with later bedtime across different continents.36 This was also in line with a study noting that bedtime procrastination was affected by people’s daily stress.70 In the same vein of the ego-depletion theory, controlling emotions may deplete the pool of internal limited cognitive resources, so a high level of stress may predict subsequent poor self-regulatory behavior,71,72 and procrastination is a typical behavioral outcome of those who are unwilling to exercise self-control and tend to choose short-sighted, short-term benefits over long-term ones.73–76 Why do people engage in more bedtime procrastination after a stressful day? According to the so-called ego-depletion theory, there are two plausible explanations. While most people know the importance of getting enough sleep, short-term motives may discourage them from going to bed on time. For instance, as the uncertainty about the future and the treatment of the virus has brought great stress to people, students may want to have some “me time” before bedtime and relax from the day.70 When experiencing high levels of COVID-19 related emotional stress, students may have a greater need to recover from the stressful day, and therefore relaxing activities are prolonged into the evening. An alternative explanation was that students do not have enough resources to start the aversive evening routine after a stressful day,77 leading to bedtime procrastination. It may seem paradoxical that some students want to relax or recover at the end of a stressful day but delay going to bed. After all, sufficient sleep seems to be the best way to actually relax and recover. From this perspective, bedtime procrastination does not seem to be a highly functional strategy. Hence, effective prevention and intervention strategies are necessary to mitigate college students’ susceptibility to bedtime procrastination behaviors.
The Mediating Effect of Negative Affect
Besides, the mediation results of this study suggested that negative affect partially mediated the relationship between COVID-19 related emotional stress and bedtime procrastination, indicating that excessive COVID-19 related emotional stress induced strong negative affect, which in turn tended to more bedtime procrastination. This result was consistent with the findings of existing research, indicating that the COVID-19 pandemic has major impacts on mental health and sleep,2 and confirmed the stress response mechanism which suggests that stress can cause dramatic changes in emotion which in turn trigger health problems, including sleep.78–80 Some researchers have explained the relationship between stress and negative affect from the perspective of attention. When individuals are stimulated by stress, they tend to produce mind wandering, which is a spontaneous shift of attention from dealing with the primary task at hand to processing irrelevant information.81 According to prior research, mind wandering can increase anxiety, depression, worry, and other negative affect,40,41,82 and those adverse outcomes directly result in sleep problems.83,84
It should be noted that the relationship between negative affect and bedtime procrastination was significant in our study. This finding was consistent with previous studies85 and the internalization of conflicts model.43 Individuals with high levels of negative affect focus more on short-term goals that benefit them immediately than long-term goals that bring them delayed rewards.86 More specifically, instead of pursuing the long-term benefits of going to bed on time, they are eager to deal with the current negative affect. Therefore, they may divert their attention to activities that make them feel happy (eg, playing online games, watching videos, and chatting with friends) and delay bedtime.87 In this case, bedtime procrastination can be seen as a way to deal with negative affect.45,88
Interestingly, we found that the mediating effect of negative affect accounted for 73.95% of the total effect, which was stronger than the direct effect from COVID-19 related emotional stress to bedtime procrastination. This suggests that negative affect as a variable, has a more direct and important influence when examining the effect of COVID-19 related emotional stress on bedtime procrastination.
The Moderating Effect of Rumination
Furthermore, the current results demonstrated that rumination moderated the relationship between COVID-19 related emotional stress and negative affect in students. Specifically, compared with students with low levels of rumination, individuals with high levels of rumination were more likely to experience negative affect when exposed to COVID-19 related emotional stress. This result supported the organism-environment interaction model,48 indicating that environmental factors (eg, COVID-19 related emotional stress) and individual traits (eg, rumination) have a superposition effect on psychosocial and social adaptation, also known as the “aggravation effect”, that is, negative personality traits (eg, rumination) aggravate the negative impact of adverse environmental factors (eg, COVID-19 related emotional stress) on individual’s psychosocial and social adaptation. This can be explained by the response style theory of rumination.49 According to the theory, when experiencing stress, individuals with high rumination tend to repeatedly think about the stressful event, its causes and potential adverse consequences, which aggravates the stress-related negative affect. Rumination is not conducive to the adoption of positive coping strategies, and it makes individuals in the long-term adverse impact of stressful events and the erosion of stress emotions, which harms individual’s psychosocial and social adaptation, such as inducing negative affect. On the contrary, individuals with less rumination tend to focus their attention on the current states or feelings and tend to adopt positive coping strategies, which not only helps them to properly deal with stressful life events, but also reduces the possibility of the negative impact of stressful life events on negative affect. Thus, rumination may function as a catalyst in the relation between COVID-19 related emotional stress and negative affect. Individuals with high rumination are more likely to experience negative affect when suffering from COVID-19 related emotional stress.
Limitations and Implications for Practice
Despite the important implications, the present study had its methodological limitations. First, the measure of the data relied on subjective reports completely, which may be prone to bias though high reliability and validity of the selected scales. For example, participants could have given responses that included a tendency to either underreport or overreport socially desirable attitudes. Thus, to address this problem, future studies should use multiple assessment techniques to investigate the relationships between the study variables. Second, the present study employed a cross-sectional design, thus, we cannot ascertain a causal relationship between the variables. Subsequent researches using longitudinal or experimental designs need to be adopted which may have the potential to explore the causal implications of the relations among COVID-19 related emotional stress, negative affect, rumination, and bedtime procrastination.
Our study showed that COVID-19 related emotional stress and rumination should be considered as important risk factors in prevention and intervention programs for bedtime procrastination. Unfortunately, COVID-19 is highly contagious, making it an uncontrollable source of stress for many people.89 In this context, it is necessary to select the content of public information carefully, avoid messages that may increase stress, and carry out health promotion to reduce the level of stress in society during the pandemic. In terms of rumination, it can be reduced by changing the poor cognitive and emotional reaction patterns.90,91 Therefore, college students can mitigate the adverse effects of COVID-19 related emotional stress by reducing rumination through targeted learning and training. Meanwhile, a highlighted finding in our study that negative affect mediated the relationship between COVID-19 related emotional stress and bedtime procrastination may imply some new solutions to the sleep problems. That is, prevention and intervention programs for sleep problems can partially consider reducing the negative affect to help college students with high levels of rumination attain more and better sleep. On this basis, we recommend Cognitive Behavioral Techniques (CBTs), which is a type of self-regulation intervention that can be used in these prevention and intervention programs. Cognitive Behavioral Techniques include cognitive reappraisal, response modulation, and mindfulness-based techniques. It has been well established that these techniques can help college students with high levels of rumination relieve their negative affect.92 According to a study, a four-week program of mindfulness exercises, including body scan, breath awareness, and loving-kindness meditation exercises, achieved great success in reducing ruminative thoughts and anxiety before sleep.93 Therefore, people experiencing high levels of stress during the COVID-19 pandemic can employ Cognitive Behavioral Techniques to mitigate negative affect and thus reduce bedtime procrastination behaviors.
Conclusion
In a nutshell, this study explored how COVID-19 related emotional stress may be related to bedtime procrastination among Chinese college students. The results showed that negative affect served as one mechanism linking COVID-19 related emotional stress to bedtime procrastination. Further, the interaction effect provided a positive implication showing that COVID-19 related emotional stress may be coupled with rumination to further reinforce students’ negative affect while promoting bedtime procrastination. The present study provides some initial avenues for future interventions that help people get more of the sleep they need during the COVID-19 pandemic. The new findings not only explained the mechanism of bedtime procrastination during the COVID-19 pandemic, but also revealed feasible approaches to reduce bedtime procrastination for college students.
Acknowledgments
Thanks to everyone who helped during the research.
Funding
This study was funded by the National Natural Science Foundation of China (72164018), National Social Science Fund Project (BFA200065), Jiangxi Social Science Foundation Project (21JY13), Jiangxi’ Key Research Base Project of Humanities and Social Sciences (JD20068), and Science and Technology Research Project of Jiangxi’ Department of Education (GJJ200306).
Disclosure
All authors report no conflicts of interest in this work.
References
1. Klaiber P, Wen JH, DeLongis A, Sin NL. The ups and downs of daily life during COVID-19: age differences in affect, stress, and positive events. J Gerontol B-Psychol. 2021;76(2):e30–e37. doi:10.1093/geronb/gbaa096
2. Morin CM, Bjorvatn B, Chung F, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45. doi:10.1016/j.sleep.2021.07.035
3. Okely AD, Kariippanon KE, Guan HY, et al. Global effect of COVID-19 pandemic on physical activity, sedentary behaviour and sleep among 3-to 5-year-old children: a longitudinal study of 14 countries. BMC Public Health. 2021;21(1):940. doi:10.1186/s12889-021-10852-3
4. Ornell F, Borelli WV, Benzano D, et al. The next pandemic: impact of COVID-19 in mental healthcare assistance in a nationwide epidemiological study. Lancet Reg Health Am. 2021;4:100061. doi:10.1016/j.lana.2021.100061
5. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatr. 2020;66(4):317–320. doi:10.1177/0020764020915212
6. Xie M, Tang YG, Zhu L, et al. Childhood Trauma and Mental Health Status in General Population: a Series Mediation Examination of Psychological Distress in COVID-19 Pandemic and Global Sleep Quality. Front Psychiatry. 2021:12782913. doi:10.3389/fpsyt.2021.782913
7. Berberoglu B, Koc N, Boyacioglu H, et al. Assessment of dental anxiety levels among dental emergency patients during the COVID-19 pandemic through the Modified Dental Anxiety Scale. Dent Med Probl. 2021;58(4):425–432. doi:10.17219/dmp/139042
8. Brulhart M, Klotzbucher V, Lalive R, Reich SK. Mental health concerns during the COVID-19 pandemic as revealed by helpline calls. Nature. 2021;600(7887):121–126. doi:10.1038/s41586-021-04099-6
9. Guessoum SB, Lachal J, Radjack R, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020:291113264. doi:10.1016/j.psychres.2020.113264
10. Melissa Flores-Quispe B, Alejandro Ruiz-Reyes R, Antonio Leon-Manco R, Agudelo-Suarez A. Preventive measures for COVID-19 among dental students and dentists during the mandatory social isolation in Latin America and the Caribbean in 2020. Dent Med Probl. 2022;59(1):5–11. doi:10.17219/dmp/142033
11. Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuro-Psychoph. 2021;109110236. doi:10.1016/j.pnpbp.2020.110236
12. Wieckiewicz M, Danel D, Pondel M, et al. Identification of risk groups for mental disorders, headache and oral behaviors in adults during the COVID-19 pandemic. Sci Rep. 2021;11(1):10964. doi:10.1038/s41598-021-90566-z
13. Petrov ME, Pituch KA, Kasraeian K, et al. Impact of the COVID-19 pandemic on change in sleep patterns in an exploratory, cross-sectional online sample of 79 countries. Sleep Health. 2021;7(4):451–458. doi:10.1016/j.sleh.2021.05.007
14. Fila-Witecka K, Malecka M, Senczyszyn A, et al. Sleepless in Solitude-Insomnia Symptoms Severity and Psychopathological Symptoms among University Students during the COVID-19 Pandemic in Poland. Int J Environ Res Public Health. 2022;19(5):2551. doi:10.3390/ijerph19052551
15. Socarras LR, Potvin J, Forest G. COVID-19 and sleep patterns in adolescents and young adults. Sleep Med. 2021;83:26–33. doi:10.1016/j.sleep.2021.04.010
16. Yuksel D, McKee GB, Perrin PB, et al. Sleeping when the world locks down: correlates of sleep health during the COVID-19 pandemic across 59 countries. Sleep Health. 2021;7(2):134–142. doi:10.1016/j.sleh.2020.12.008
17. Emodi-Perlman A, Eli I, Uziel N, et al. Public Concerns during the COVID-19 Lockdown: a Multicultural Cross-Sectional Study among Internet Survey Respondents in Three Countries. J Clin Med. 2021;10(8):1577. doi:10.3390/jcm10081577
18. Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi:10.1016/j.sleep.2020.05.011
19. Li D-J, Ko N-Y, Chen Y-L, et al. COVID-19-Related Factors Associated with Sleep Disturbance and Suicidal Thoughts among the Taiwanese Public: a Facebook Survey. Int J Environ Res Public Health. 2020;17(12):4479. doi:10.3390/ijerph17124479
20. Bhuiyan AKMI, Sakib N, Pakpour AH, Griffiths MD, Mamun MA. COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence from media reports. Int J Ment Health Ad. 2021;19(6):2110–2115. doi:10.1007/s11469-020-00307-y
21. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/s0140-6736(20
22. Satici B, Saricali M, Satici SA, Griffiths MD. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int J Ment Health Ad. 2020;1–12. doi:10.1007/s11469-020-00305-0
23. Akerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, Kecklund G. Predicting sleep quality from stress and prior sleep - A study of day-to-day covariation across six weeks. Sleep Med. 2012;13(6):674–679. doi:10.1016/j.sleep.2011.12.013
24. Eliasson AH, Kashani M, Mayhew M, Ude A, Hoffman J, Vernalis M. Reducing perceived stress improves sleep quality: a longitudinal outcomes study. Chest. 2010;138(4):913A. doi:10.1378/chest.10417
25. Hefez A, Metz L, Lavie P. Long-term effects of extreme situational stress on sleep and dreaming. Am J Psychiatry. 1987;144(3):344–347. doi:10.1176/ajp.144.3.344
26. Mellman TA, David D, Kulick-Bell R, Hebding J, Nolan B. Sleep disturbance and its relationship to psychiatric morbidity after Hurricane Andrew. Am J Psychiatry. 1995;152(11):1659–1663. doi:10.1176/ajp.152.11.1659
27. Tempesta D, Curcio G, De Gennaro L, Ferrara M. Long-term impact of earthquakes on sleep quality. PLoS One. 2013;8(2):e55936. doi:10.1371/journal.pone.0055936
28. Cohen S. Aftereffects of stress on human performance and social behavior: a review of research and theory. Psychol Bull. 1980;88(1):82–108. doi:10.1037/0033-2909.88.1.82
29. Hagger MS, Wood C, Stiff C, Chatzisarantis NLD. Ego depletion and the strength model of self-control: a meta-analysis. Psychol Bull. 2010;136(4):495–525. doi:10.1037/a0019486
30. Glass DC, Siger JE, Friedman LN. Psychic cost of adaptation to an environmental stressor. J Pers Soc Psychol. 1969;12(3):200–210. doi:10.1037/h0027629
31. Inzlicht M, Schmeichel BJ. What is ego depletion? Toward a mechanistic revision of the resource model of self-control. Perspect Psychol Sci. 2012;7(5):450–463. doi:10.1177/1745691612454134
32. Kroese FM, De Ridder DTD, Evers C, Adriaanse MA. Bedtime procrastination: introducing a new area of procrastination. Front Psychol. 2014;5:611. doi:10.3389/fpsyg.2014.00611
33. Meng D, Zhao Y, Guo J, et al. Time Perspective and Bedtime Procrastination: the Role of the Chronotype-Time Perspective Relationship. Nat Sci Sleep. 2021;13:1307–1318. doi:10.2147/nss.S313157
34. Kroese FM, Evers C, Adriaanse MA, de Ridder DTD. Bedtime procrastination: a self-regulation perspective on sleep insufficiency in the general population. J Health Psychol. 2016;21(5):853–862. doi:10.1177/1359105314540014
35. Guo J, Meng D, Ma X, Zhu L, Yang L, Mu L. The impact of bedtime procrastination on depression symptoms in Chinese medical students. Sleep Breath. 2020;24(3):1247–1255. doi:10.1007/s11325-020-02079-0
36. Kaditis AG, Ohler A, Gileles-Hillel A, et al. Effects of the COVID-19 lockdown on sleep duration in children and adolescents: a survey across different continents. Pediatr Pulm. 2021;56(7):2265–2273. doi:10.1002/ppul.25367
37. Arslan G, Yildirim M. Coronavirus stress, meaningful living, optimism, and depressive symptoms: a study of moderated mediation model. Aust J Psychol. 2021;73(2):113–124. doi:10.1080/00049530.2021.1882273
38. Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiat. 2020;7(6):468–471. doi:10.1016/s2215-0366(20
39. Mason MF, Brown K, Mar RA, Smallwood J. Driver of discontent or escape vehicle: the affective consequences of mindwandering. Front Psychol. 2013;4:477. doi:10.3389/fpsyg.2013.00477
40. Deng YQ, Li S, Tang YY. The relationship between wandering mind, depression and mindfulness. Mindfulness. 2014;5(2):124–128. doi:10.1007/s12671-012-0157-7
41. Killingsworth MA, Gilbert DT. A wandering mind is an unhappy mind. Science. 2010;330(6006):932. doi:10.1126/science.1192439
42. Ong AD, Kim S, Young S, Steptoe A. Positive affect and sleep: a systematic review. Sleep Med Rev. 2017;35:21–32. doi:10.1016/j.smrv.2016.07.006
43. Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14(4):227–238. doi:10.1016/j.smrv.2009.10.007
44. Kadzikowska-Wrzosek R. Self-regulation and bedtime procrastination: the role of self-regulation skills and chronotype. Pers Individ Dif. 2018;128:10–15. doi:10.1016/j.paid.2018.02.015
45. Sirois FM, Nauts S, Molnar DS. Self-compassion and bedtime procrastination: an emotion regulation perspective. Mindfulness. 2019;10(3):434–445. doi:10.1007/s12671-018-0983-3
46. Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol. 1991;100(4):569–582. doi:10.1037/0021-843x.100.4.569
47. Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008;3(5):400–424. doi:10.1111/j.1745-6924.2008.00088.x
48. Lerner RM, Lerner JV, Almerigi J, Theokas C. Dynamics of Individual←→ Context Relations in Human Development: a Developmental Systems Perspective. J Med. 2006;1:548.
49. Conway M, Csank PA, Holm SL, Blake CK. On assessing individual differences in rumination on sadness. J Pers Assess. 2000;75(3):404–425. doi:10.1207/s15327752jpa7503_04
50. Olatunji BO, Naragon-Gainey K, Wolitzky-Taylor KB. Specificity of rumination in anxiety and depression: a multimodal meta-analysis. Clin Psychol-Sci Pr. 2013;20(3):225–257. doi:10.1111/cpsp.12037
51. Roelofs J, Huibers M, Peeters F, Arntz A. Effects of neuroticism on depression and anxiety: rumination as a possible mediator. Pers Individ Dif. 2008;44(3):576–586. doi:10.1016/j.paid.2007.09.019
52. Moberly NJ, Watkins ER. Ruminative self-focus, negative life events, and negative affect. Behav Res Ther. 2008;46(9):1034–1039. doi:10.1016/j.brat.2008.06.004
53. Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007;18(3):233–239. doi:10.1111/j.1467-9280.2007.01882.x
54. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:10.3758/brm.41.4.1149
55. Ye B, Wang R, Liu M, Wang X, Yang Q. Life history strategy and overeating during COVID-19 pandemic: a moderated mediation model of sense of control and coronavirus stress. J Eat Disord. 2021;9(1):1–12. doi:10.1186/s40337-021-00514-5
56. Arslan G, Yildirim M, Tanhan A, Bulus M, Allen K-A. Coronavirus stress, optimism-pessimism, psychological inflexibility, and psychological health: psychometric properties of the Coronavirus Stress Measure. Int J Ment Health Ad. 2021;19(6):2423–2439. doi:10.1007/s11469-020-00337-6
57. Gong X, Xie XY, Xu R, Luo YJ. Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chin J Clin Psychol. 2010;18(4):443–446. doi:10.16128/j.cnki.1005-3611.2010.04.020
58. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–343. doi:10.1016/0005-7967(94
59. Nanthakumar S, Bucks RS, Skinner TC, et al. Assessment of the Depression, Anxiety, and Stress Scale (DASS-21) in untreated obstructive sleep apnea (OSA). Psychol Assess. 2017;29(10):1201–1209. doi:10.1037/pas0000401
60. Han X, Yang HF. Chinese version of Nolen-Hoeksema ruminative responses scale (RRS) used in 912 college students: reliability and validity. Chin J Clin Psychol. 2009;17(5):550–551. doi:10.16128/j.cnki.1005-3611.2009.05.028
61. Ma X, Zhu L, Guo J, Zhao Y, Fu Y, Mu L. Reliability and validity of the Bedtime Procrastination Scale in Chinese college students. Chin J Clin Psychol. 2021;29(4):717–720. doi:10.16128/j.cnki.1005-3611.2021.04.011
62. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford publications; 2017.
63. Ammar A, Trabelsi K, Brach M, et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study. Biol Sport. 2021;38(1):9–21. doi:10.5114/biolsport.2020.96857
64. Veer IM, Riepenhausen A, Zerban M, et al. Psycho-social factors associated with mental resilience in the Corona lockdown. Transl Psychiat. 2021;11(1):67. doi:10.1038/s41398-020-01150-4
65. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288112954. doi:10.1016/j.psychres.2020.112954
66. Ara T, Rahman MM, Hossain MA, Ahmed A. Identifying the Associated Risk Factors of Sleep Disturbance During the COVID-19 Lockdown in Bangladesh: a Web-Based Survey. Front Psychiatry. 2020;11580268. doi:10.3389/fpsyt.2020.580268
67. Dondi A, Fetta A, Lenzi J, et al. Sleep disorders reveal distress among children and adolescents during the Covid-19 first wave: results of a large web-based Italian survey. Ital J Pediatr. 2021;47(1):130. doi:10.1186/s13052-021-01083-8
68. Saadeh H, Saadeh M, Almobaideen W, et al. Effect of COVID-19 Quarantine on the Sleep Quality and the Depressive Symptom Levels of University Students in Jordan During the Spring of 2020. Front Psychiatry. 2021:12605676. doi:10.3389/fpsyt.2021.605676
69. Zerbini G, Taflinger S, Reicherts P, Kunz M, Sattler S. Perceived risk of COVID-19 exposure and poor COVID-19 prognosis impair sleep: the mediating and moderating roles of COVID-19-related anxiety and knowledge. J Sleep Res. 2022;e13569. doi:10.1111/jsr.13569
70. Bernecker K, Job V. Too exhausted to go to bed: implicit theories about willpower and stress predict bedtime procrastination. Brit J Psychol. 2020;111(1):126–147. doi:10.1111/bjop.12382
71. Inzlicht M, Bartholow BD, Hirsh JB. Emotional foundations of cognitive control. Trends Cogn Sci. 2015;19(3):126–132. doi:10.1016/j.tics.2015.01.004
72. Maier SU, Makwana AB, Hare TA. Acute stress impairs self-control in goal-directed choice by altering multiple functional connections within the brain’s decision circuits. Neuron. 2015;87(3):621–631. doi:10.1016/j.neuron.2015.07.005
73. Ariely D, Wertenbroch K. Procrastination, deadlines, and performance: self-control by precommitment. Psychol Sci. 2002;13(3):219–224. doi:10.1111/1467-9280.00441
74. Howell AJ, Watson DC, Powell RA, Buro K. Academic procrastination: the pattern and correlates of behavioural postponement. Pers Individ Dif. 2006;40(8):1519–1530. doi:10.1016/j.paid.2005.11.023
75. Klassen RM, Krawchuk LL, Rajani S. Academic procrastination of undergraduates: low self-efficacy to self-regulate predicts higher levels of procrastination. Contemp Educ Psychol. 2008;33(4):915–931. doi:10.1016/j.cedpsych.2007.07.001
76. Ozer BU, O’Callaghan J, Bokszczanin A, Ederer E, Essau C. Dynamic interplay of depression, perfectionism and self-regulation on procrastination. Br J Guid Counc. 2014;42(3):309–319. doi:10.1080/03069885.2014.896454
77. Nauts S, Kamphorst BA, Sutu AE, Poortvliet R, Anderson JH. Aversive bedtime routines as a precursor to bedtime procrastination. Eur Health Psychol. 2016;18(2):80–85.
78. Epel ES, Crosswell AD, Mayer SE, et al. More than a feeling: a unified view of stress measurement for population science. Front Neuroendocrinol. 2018;49:146–169. doi:10.1016/j.yfrne.2018.03.001
79. Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150–170. doi:10.1037/0022-3514.48.1.150
80. Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986;50(5):992–1003. doi:10.1037/0022-3514.50.5.992
81. An YY, Xu W. Haze and perceived stress aggravate fatigue: from ecological transients when evaluating evidence. Chin J Clin Psychol. 2017;25(6):1130–1133. doi:10.16128/j.cnki.1005-3611.2017.06.029
82. Poerio GL, Totterdell P, Miles E. Mind-wandering and negative mood: does one thing really lead to another? Conscious Cogn. 2013;22(4):1412–1421. doi:10.1016/j.concog.2013.09.012
83. Cheung T, Yip PSF. Lifestyle and depression among Hong Kong nurses. Int J Environ Res Public Health. 2016;13(1):135. doi:10.3390/ijerph13010135
84. Kirwan M, Pickett SM, Jarrett NL. Emotion regulation as a moderator between anxiety symptoms and insomnia symptom severity. Psychiatry Res. 2017;254:40–47. doi:10.1016/j.psychres.2017.04.028
85. Myrick JG. Emotion regulation, procrastination, and watching cat videos online: who watches Internet cats, why, and to what effect? Comput Human Behav. 2015;52:168–176. doi:10.1016/j.chb.2015.06.001
86. Sirois F, Pychyl T. Procrastination and the priority of short‐term mood regulation: consequences for future self. Soc Personal Psychol Compass. 2013;7(2):115–127. doi:10.1111/spc3.12011
87. Exelmans L, Van den Bulck J. Self-control depletion and sleep duration: the mediating role of television viewing. Psychol Health. 2018;33(10):1251–1268. doi:10.1080/08870446.2018.1489048
88. Pychyl TA, Sirois FM. Procrastination, emotion regulation, and well-being. Procrastination, health, and well-being. Academic Press. 2016;1:163–188.
89. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monitor. 2020;26:e923549. doi:10.12659/msm.923549
90. Cohen N, Mor N, Henik A. Linking executive control and emotional response: a training procedure to reduce rumination. Clin Psychol Sci. 2015;3(1):15–25. doi:10.1177/2167702614530114
91. Querstret D, Cropley M. Assessing treatments used to reduce rumination and/or worry: a systematic review. Clin Psychol Rev. 2013;33(8):996–1009. doi:10.1016/j.cpr.2013.08.004
92. Grecucci A, Messina I, Amodeo L, et al. A dual route model for regulating emotions: comparing models, techniques and biological mechanisms. Front Psychol. 2020;11:930. doi:10.3389/fpsyg.2020.00930
93. Hassirim Z, Lim ECJ, Lo JC, Lim J. Pre-sleep cognitive arousal decreases following a 4-week introductory mindfulness course. Mindfulness. 2019;10(11):2429–2438. doi:10.1007/s12671-019-01217-4
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
