Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Correlation Between Neck Circumference and Gestational Diabetes
Authors Li X, Bai L, Niu Z , Lu Q
Received 12 October 2023
Accepted for publication 21 December 2023
Published 23 December 2023 Volume 2023:16 Pages 4179—4185
DOI https://doi.org/10.2147/DMSO.S439413
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Xiaojing Li,1 Liwei Bai,2 Ziru Niu,3 Qiang Lu3
1Department of Obstetrics, First Hospital of Qinhuangdao, Qinhuangdao, Hebei, 066000, People’s Republic of China; 2Department of Obstetrics, Qinhuangdao Hospital for Maternal and Child Health, Qinhuangdao, Hebei, 066000, People’s Republic of China; 3Department of Endocrinology, First Hospital of Qinhuangdao, Qinhuangdao, Hebei, 066000, People’s Republic of China
Correspondence: Qiang Lu, Department of Endocrinology, First Hospital of Qinhuangdao, Qinhuangdao, Hebei, 066000, People’s Republic of China, Tel +86-13933909066, Email [email protected]
Purpose: The objective of this study was to explore whether neck circumference can serve as an early predictor of the risk of Gestational Diabetes (GDM).
Patients and Methods: A total of 318 singleton pregnant women who underwent routine prenatal examinations at Qinhuangdao Maternal and Child Health Hospital from September 2017 to September 2020 were selected and categorized into the GDM group and the normal glucose tolerance group (NGT) based on the results of the oral glucose tolerance test (OGTT) conducted during the second trimester. The general information and laboratory test results were compared and analyzed. Inter-group comparison was conducted using the t-test, and multivariate logistic regression analysis was employed to analyze the independent risk factors of GDM. The predictive threshold of various indicators for GDM occurrence during pregnancy was determined using the subject’s work curve.
Results: The GDM group exhibited significantly higher levels of pre-pregnancy weight, pre-pregnancy BMI, neck circumference, waist circumference, hip circumference, triglycerides (TG), uric acid (UA), TG/HDL-C ratio, and waist-hip ratio compared to the NGT group. Additionally, HDL cholesterol (HDL-C) levels were significantly lower in the GDM group, and blood glucose levels at each point of the OGTT were markedly higher compared to the NGT group (P< 0.05). Multivariate logistic regression analysis revealed that neck circumference (OR=1.239, P< 0.001) and early pregnancy TG (OR=1.842, P< 0.001) were independent risk factors for GDM. The receiver operating characteristic analysis demonstrated that the optimal critical value of neck circumference for predicting GDM was 32.6 cm, with a sensitivity of 50% and specificity of 74.3%.
Conclusion: The neck circumference during early pregnancy was found to be related to GDM, and the predictive cutoff point of 32.6 cm for neck circumference could be employed as a simple index to predict GDM in early pregnancy.
Keywords: neck circumference, gestational diabetes, obesity, predictive indicators
Introduction
Currently, the global standardized prevalence rate of GDM stands at 14.0%, making it one of the most common complications during pregnancy.1 Gestational Diabetes (GDM) not only adversely affects pregnancy outcomes but also escalates the long-term risk of complications for both mothers and offspring, including obesity, diabetes, cardiovascular diseases, and other ailments.2,3 This situation has placed a significant burden on both individual and public health.
Neck circumference (NC), a straightforward and practical anthropometric measure, offers insights into upper body fat distribution. Mounting evidence underscores the strong association between NC and metabolic disorders like metabolic syndrome, diabetes, and fatty liver.4 A study has demonstrated a close link between neck circumference and insulin resistance, predicting the risk of metabolic abnormalities with greater simplicity and less variability than other obesity indicators.5,6 Given that obesity is a notable risk factor for GDM, scant research has been conducted on the connection between neck circumference and Gestational Diabetes, both domestically and internationally. Neck circumference has the potential to emerge as a traditional obesity assessment parameter surpassing waist circumference and the Waist-Hip Ratio. Moreover, it presents itself as a novel marker for predicting diabetes risk during pregnancy.7 This article retrospectively scrutinizes the routine prenatal and clinical data of 318 pregnant women, aiming to unearth the association between neck circumference and early-pregnancy (8–12 weeks) GDM occurrences. Furthermore, it assesses the clinical utility of neck circumference as an early predictor of GDM risk.
Materials and Methods
Research Object
A total of 318 pregnant women aged between 21 and 40 years (mean age: 29.12±4.55 years) were selected from Qinhuangdao Maternal and Child Health Hospital for routine prenatal examinations from September 2017 to September 2020. Inclusion criteria encompassed single pregnancies with complete first-trimester data, including measurements of neck circumference, waist circumference, hip circumference, as well as results from the 75g oral glucose tolerance test (OGTT) conducted at 24–28 weeks of gestation. Exclusion criteria comprised autoimmune diseases (including systemic lupus erythematosus, rheumatoid arthritis, primary Sjögren syndrome), chronic hypertension, heart diseases, thyroid disorders, diabetes, severe liver or kidney diseases (including intrahepatic cholestasis of pregnancy, autoimmune hepatitis, nephrotic syndrome chronic, glomerulonephritis, IgA nephropathy), etc. This study was approved by the Ethics Committee of Qinhuangdao First Hospital and the Ethics Committee of Qinhuangdao Maternal and Child Health Hospital with the ethics approval number 2021Q088. Patient consent was not required by the Ethics Committee due to the retrospective nature of the study and the anonymity of the data.
Data Collection
Data were collected, including maternal age, height, pre-pregnancy weight, systolic and diastolic blood pressure, neck circumference, waist circumference, hip circumference, and levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transpeptidase (GGT), uric acid (UA), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) during the first trimester (8–12 weeks of gestation). Pre-pregnancy body mass index (BMI) was calculated. Blood glucose results from OGTT at 0 hours, 1 hour, and 2 hours during the second trimester (24–28 weeks of gestation) were recorded.
Diagnostic Criteria and Grouping
In accordance with the diagnostic criteria established by the International Association of Diabetes and Pregnancy Study Groups (IADPSG),8 GDM was diagnosed among pregnant women who had not received a diabetes diagnosis prior to or during the first trimester of pregnancy. The 75g oral glucose tolerance test (OGTT) was conducted during the period of 24–28 weeks of gestation. Blood glucose levels were measured during fasting and at 1 hour and 2 hours after glucose administration. Specifically, GDM diagnosis was confirmed if any of the following criteria were met: fasting blood glucose level (FPG) ≥5.1 mmol/L, blood glucose level at 1 hour after glucose administration (1hPG) ≥10.0 mmol/L, or blood glucose level at 2 hours after glucose administration (2hPG) ≥8.5 mmol/L.
The study population was divided based on OGTT outcomes into two groups: (1) the normal glucose tolerance gestation (NGT) group, 218 people; and (2) the gestational diabetes mellitus (GDM) group, which comprised patients whose blood glucose levels met the aforementioned diagnostic criteria for GDM, 100 people.
Statistical Analysis
Statistical analysis was performed using SPSS 25.0 software. Normally distributed measurement data were presented as X ± s. The t-test was utilized for inter-group comparisons of continuous variables, while the χ2 test was employed for categorical data. Multivariate logistic regression analysis, with no observed multicollinearity among included independent variables, was conducted to identify independent risk factors for GDM. The predictive capacity of neck circumference in relation to GDM was evaluated using the receiver operating characteristic (ROC) curve, with the area under the curve (AUC) calculated. The optimal predictive threshold was established based on the maximal Youden index. A significance level of P < 0.05 was considered statistically significant.
Results
Comparison of the Clinical Data in the Various Groups
Table 1 illustrates the comparison of clinical data among different groups. No statistically significant differences were observed in age, systolic blood pressure, diastolic blood pressure, ALT, AST, GGT, TC, and LDL-C between the two groups (P>0.05).
 |
Table 1 Comparison of Baseline Characteristics of Subjects in the GDM and NGT Groups [ |
Pregnant women in the GDM group exhibited significantly higher values for pre-pregnancy weight, pre-pregnancy BMI, waist circumference, hip circumference, neck circumference, and waist-to-hip circumference ratio when compared to the NGT group (P<0.05). Additionally, levels of TG, HDL-C, TG/HDL-C ratio, and UA were notably elevated in the GDM group relative to the NGT group (P<0.05). Furthermore, levels of OGTT at 0 hours, 1 hour, and 2 hours in the second trimester were markedly higher in the GDM group with statistical significance (P<0.05).
Regression Analysis of Risk Factors for GDM
To comprehensively assess risk factors associated with GDM, both with and without GDM as the dependent variable, the statistically significant factors identified in Table 1—namely, pre-pregnancy weight, pre-pregnancy BMI, neck circumference, waist circumference, hip circumference, waist-to-hip ratio, FPG, 1hPG, 2hPG, TG, UA, and HDL-C—were considered as independent variables. Univariate logistic regression analysis was conducted, revealing that pre-pregnancy BMI, neck circumference, waist circumference, hip circumference, waist-to-hip ratio, TG, HDL-C, TG/HDL-C ratio, and UA emerged as risk factors for GDM (P<0.05, Table 2).
 |
Table 2 Univariate Logistic Regression Analysis of the Risk Factors Associated with GDM |
To discern the independent risk factors for GDM, the presence or absence of GDM was designated as the dependent variable. Subsequently, the statistically significant risk factors (pre-pregnancy BMI, neck circumference, waist-to-hip ratio, UA, TG, HDL-C, TG/HDL-C ratio) from Table 2, which were identified through diagnosis of multicollinearity, were included in a multivariate logistic regression analysis. Based on the P<0.05 criteria, only neck circumference (OR=1.223, P=0.000) and early pregnancy TG (OR=1.889, P=0.000) were confirmed as independent risk factors for GDM (refer to Table 3).
 |
Table 3 Results of Binary Logistic Regression Analysis of Different Influencing Factors and GDM Relationships |
Prediction Cut-off Point of Neck Circumference in the Assessment of Diabetes in Pregnancy
The assessment of GDM utilized a ROC curve analysis, where gestational diabetes constituted the outcome variable, and neck circumference served as the test variable. The area under the ROC curve for neck circumference was computed as 0.636 (95% CI: 0.569 ~ 0.704). The optimal threshold for neck circumference was established at 32.60 cm, demonstrating a sensitivity of 50% and a specificity of 74.3% (Figure 1).
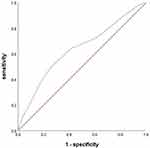 |
Figure 1 The ROC curve of NC for predicting GDM risk. |
Discussion
The diagnosis of gestational diabetes mellitus relies on the oral glucose tolerance test (OGTT) administered during the 24–28 weeks of the second trimester. However, prior to OGTT screening, pregnant women at a high risk of GDM often display elevated blood glucose trends.9 Moreover, the timing of GDM diagnosis is closely proximate to delivery, affording minimal opportunity for intervention in at-risk pregnant women. Early interventions such as dietary adjustments and exercise can significantly mitigate GDM risk.10 Therefore, it becomes pivotal to identify GDM high-risk groups using accessible and efficacious indicators. Swift and effective interventions can then be initiated at the onset of medical care during pregnancy. Considering the physiological transformations during pregnancy, conventional metrics like BMI, waist circumference, and waist-to-hip ratio might not be apt for prognosticating the risk of gestational obesity and GDM. Notably, overseas studies11 have demonstrated that pregnant women with a neck circumference exceeding 33.5cm exhibit elevated odds of developing GDM, with neck circumference emerging as an autonomous predictor of GDM. A meta-analysis of literature underscores that an augmented neck circumference corresponds to a markedly increased likelihood of gestational diabetes mellitus (GDM). The neck circumference of GDM-afflicted patients surpasses that of the control cohort, and neck circumference maintains a substantial association with adverse pregnancy outcomes.12 In our investigation, we ascertained that the neck circumference of the gestational diabetes mellitus group markedly exceeded that of the normal control group (P < 0.01). Regression analysis unveiled pre-pregnancy BMI, neck circumference, waist circumference, hip circumference, waist-to-hip ratio, TG, HDL-C, TG/HDL-C ratio, and UA as GDM risk factors (P < 0.05). Multivariate regression analysis further elucidated that solely neck circumference and TG stood as independent risk factors for GDM. This implies that neck circumference holds its own regardless of BMI, waist circumference, and waist-to-hip ratio. Notably, the dynamic modifications in waist circumference and waist-to-hip ratio, often adopted obesity indicators, throughout pregnancy due to increased uterine size could potentially distort the assessment of obesity or overweight during gestation.
The precise etiology of GDM remains elusive; however, it is widely acknowledged that insulin resistance coupled with diminished functionality of islet beta cells constitutes the principal pathophysiological foundation. Novel research by Pries et al3 has revealed that neck circumference, examined in non-pregnant individuals, has the potential to mirror the subcutaneous adipose tissue of the upper body. This adipose reservoir could be distinctive and is associated with insulin resistance and cardiovascular risk. Concurrently, Scovronec et al13 discovered a positive correlation between neck circumference and fasting insulin concentration, C-peptide concentration, as well as insulin resistance index (HOMA-IR) assessed via the homeostasis model. Remarkably, among obese patients, neck circumference emerged as a more potent predictor of insulin resistance compared to standard anthropometric indicators. Another investigation14 underscored the positive association between neck circumference and insulin resistance in women with polycystic ovary syndrome (PCOS), thus suggesting the potential utility of neck circumference in forecasting insulin resistance risk in PCOS patients. Substantial evidence suggests that overweight and obesity autonomously heighten the risk of GDM. Furthermore, pre-pregnancy overweight and obesity accentuate insulin resistance, thereby elevating the susceptibility to GDM.15 Our investigation exhibited significant disparities in neck circumference, pre-pregnancy weight, BMI, waist circumference, and waist-to-hip ratio between the GDM and NGT groups. Consonantly, a separate study16 unveiled positive correlations between neck circumference and body weight, waist circumference, and body mass index. Employing ROC curve analysis, our study ascertained a critical neck circumference value of 35.70 cm for predicting GDM, accompanied by a sensitivity of 51.4% and specificity of 81.2%. This underpins the reliability and efficacy of neck circumference at 16 weeks as an indicator for predicting gestational diabetes mellitus. Indeed, neck circumference serves as a novel marker for assessing GDM risk. Research conducted in southern China17 has demonstrated that escalating neck circumference independently contributes to GDM risk early in pregnancy. A neck circumference ≥33.8 cm emerges as the optimal threshold for identifying GDM, with a sensitivity of 68.04% and specificity of 59.12%. In a foreign context,18 neck circumference ≥34.3 cm forecasts GDM in Iranian pregnant women, with a sensitivity of 53% and specificity of 66%. Our findings, establishing a predictive threshold of 32.6 cm for neck circumference in early pregnancy, mirror a sensitivity of 52% and specificity of 75%. This signifies the capacity of neck circumference to reasonably anticipate GDM risk. Our outcomes align with both domestic and international studies, reflecting congruence in sensitivity and specificity. It’s noteworthy that the optimal definition of neck circumference for GDM prediction varies across nations and ethnicities, potentially owing to inter-group differences in body proportions within the same ethnicity. Hence, the most suitable neck circumference criterion for GDM prognosis should be calibrated based on the racial specificity.
Insulin resistance (IR) significantly contributes to the onset and progression of GDM. The hyperinsulinemic euglycemic clamp (HEC), while considered the gold standard for IR assessment, remains primarily suited for fundamental research due to its cost and time intensiveness. Similarly, the Homeostasis Insulin Model Assessment of Insulin Resistance Index (HOMA-IR), contingent on fasting insulin levels, lacks suitability for extensive population application. In recent years, simpler IR evaluation indicators like TG/HDL-C and the triglyceride-glucose index (TyG) have presented diversified options for IR assessment. Multiple studies19,20 have affirmed that metrics such as TG/HDL-C and the TyG index aptly identify high-risk cohorts for metabolic disorders including IR and diabetes. Research outcomes21 have further affirmed the effectiveness of the TG/HDL-C ratio prior to 24 weeks of pregnancy as an indicator for GDM risk identification. Chinese research indicates that TG/HDL-C and TyG in early pregnancy stand as robust indicators for predicting GDM, amenable to early assessment.22 Notably, our study revealed markedly elevated TG/HDL-C in the GDM group, suggesting exacerbated IR within the GDM cohort. These insights accentuate that neck circumference could potentially surpass waist circumference and waist-to-hip ratio as an IR indicator during pregnancy. Consequently, we infer that neck circumference offers a fresh and efficacious avenue for early pregnancy screening of GDM high-risk groups.
Conclusions
Several limitations warrant consideration in our study. Insulin levels were not assessed, and the steady-state insulin model could not be utilized for IR index evaluation. Although neck circumference was considered, the study did not undertake an assessment of insulin resistance and islet beta cell function during pregnancy. Furthermore, the study sample was derived from a single hospital, with the limited case numbers constituting another study drawback.
Neck circumference, a straightforward measure of obesity, holds simplicity and minimal variability, rendering it an effective clinical screening and GDM prediction indicator. It capacitates early identification of GDM high-risk groups, thereby facilitating proactive and rational dietary and exercise management during pregnancy. This intervention effectively forestalls GDM incidence, promotes positive maternal and infant outcomes, and mitigates various adversities. In conclusion, the application of neck circumference to predict GDM is of great significance for early identification of high-risk groups of GDM, improvement of long-term outcomes of mothers and offspring, strengthening of early life management, and reduction of adult chronic diseases.
Abbreviations
GDM, gestational diabetes mellitus; NGT, normal glucose tolerance group; OGTT, oral glucose tolerance test; ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyl transpeptidase; UA, uric acid; TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; NC, neck circumference; WC, waist circumference; WHR, waist-to-hip circumference ratio; HC, hip circumference; SBP, systolic pressure; DBP, diastolic pressure; BMI, body mass index; IADPSG, International Association of Diabetes and Pregnancy Study Groups; FPG, fasting blood glucose level; ROC, Generate the Receiver Operating Characteristic; HOMA-IR, insulin resistance index; IR, Insulin resistance; PCOS, polycystic ovary syndrome; HEC, hyperinsulinemic euglycemic clamp; TyG, triglyceride-glucose index.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki. This study was approved by the Ethics Committee of Qinhuangdao First Hospital and the Ethics Committee of Qinhuangdao Maternal and Child Health Hospital with the ethics approval number 2021Q088. Patient consent was not required by the Ethics Committee due to the retrospective nature of the study and the anonymity of the data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang H, Li N, Chivese T, et al. IDF Diabetes Atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by International Association of Diabetes in Pregnancy Study Group’s Criteria. Diabet Res Clin Pract. 2022;183:109050. doi:10.1016/j.diabres.2021.109050
2. Sweeting A, Wong J, Murphy HR, Ross GP. A clinical update on gestational diabetes mellitus. Endocr Rev. 2022;43(5):763–793. doi:10.1210/endrev/bnac003
3. Preis SR, Massaro JM, Hoffmann U, et al. Neck circumference as a novel measure of cardiometabolic risk: the Framingham Heart study. J Clin Endocrinol Metab. 2010;95(8):3701–3710. doi:10.1210/jc.2009-1779
4. Ebrahimi H, Mahmoudi P, Zamani F, Moradi S. Neck circumference and metabolic syndrome: a cross-sectional population-based study. Prim Care Diabetes. 2021;15(3):582–587. doi:10.1016/j.pcd.2021.02.002
5. Mendes CG, Barbalho SM, Tofano RJ, et al. Is neck circumference as reliable as waist circumference for determining metabolic syndrome? Metab Syndr Relat Disord. 2021;19(1):32–38. doi:10.1089/met.2020.0083
6. Luo Y, Ma X, Shen Y, et al. Neck circumference as an effective measure for identifying cardio-metabolic syndrome: a comparison with waist circumference. Endocrine. 2017;55(3):822–830. doi:10.1007/s12020-016-1151-y
7. KhushBakht D, Mazhar S, Bhalli A, Rashid A, Khan K, Jahanzaib U. Correlation between neck circumference and gestational diabetes mellitus and associated risk factors during pregnancy. Cureus. 2018;10(5):e2699. doi:10.7759/cureus.2699
8. Metzger BE, Gabbe SG, Persson B, Lowe LP, Dyer AR, Oats JJ, Buchanan TA; International Association of D, Pregnancy Study Groups Consensus P. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi:10.2337/dc09-1848
9. Scholtens DM, Kuang A, Lowe LP, et al. Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study (HAPO FUS): maternal glycemia and childhood glucose metabolism. Diabetes Care. 2019;42(3):381–392. doi:10.2337/dc18-2021
10. Wang C, Wei Y, Zhang X, et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol. 2017;216(4):340–351. doi:10.1016/j.ajog.2017.01.037
11. Ghorbani A, Hashemipour S, Mohammadi Z, Zohal M, Lalooha F. Appropriate neck/waist circumference cut-off points for gestational diabetes prediction in Iranian pregnant women: the baseline analysis of the Qazvin maternal and neonatal metabolic study (QMNMS), Iran. Diabetes Metab Syndr. 2022;16(8):102579. doi:10.1016/j.dsx.2022.102579
12. Heslehurst N, Ngongalah L, Bigirumurame T, et al. Association between maternal adiposity measures and adverse maternal outcomes of pregnancy: systematic review and meta-analysis. Obes Rev. 2022;23(7):e13449. doi:10.1111/obr.13449
13. Scovronec A, Provencher A, Iceta S, et al. Neck circumference is a better correlate of insulin resistance markers than other standard anthropometric indices in patients presenting severe obesity. Obes Res Clin Pract. 2022;16(4):307–313. doi:10.1016/j.orcp.2022.07.005
14. Chen Y, Zheng X, Ma D, et al. Neck circumference is a good predictor for insulin resistance in women with polycystic ovary syndrome. Fertil Steril. 2021;115(3):753–760. doi:10.1016/j.fertnstert.2020.07.027
15. Peng Y, Han N, Su T, et al. Gestational weight gain and the risk of gestational diabetes mellitus: a latent class trajectory analysis using birth cohort data. Diabet Res Clin Pract. 2021;182:109130. doi:10.1016/j.diabres.2021.109130
16. Hancerliogullari N, Kansu-Celik H, Asli Oskovi-Kaplan Z, Kisa B, Engin-Ustun Y, Ozgu-Erdinc AS. Optimal maternal neck and waist circumference cutoff values for prediction of gestational diabetes mellitus at the first trimester in Turkish population; a prospective cohort study. Gynecol Endocrinol. 2020;36(11):1002–1005. doi:10.1080/09513590.2020.1750003
17. Li P, Lin S, Cui J, Li L, Zhou S, Fan J. First trimester neck circumference as a predictor for the development of gestational diabetes mellitus. Am J Med Sci. 2018;355(2):149–152. doi:10.1016/j.amjms.2017.09.012
18. Barforoush TS, Ghadimi R, Pahlevan Z, Ahmadi N, Delavar MA. The relationship between neck circumference and gestational diabetes mellitus in Iranian women. Clin Diabetes Endocrinol. 2021;7(1):22. doi:10.1186/s40842-021-00136-5
19. Zhou M, Zhu L, Cui X, et al. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance but not of beta cell function in a Chinese population with different glucose tolerance status. Lipids Health Dis. 2016;15:104. doi:10.1186/s12944-016-0270-z
20. Young KA, Maturu A, Lorenzo C, et al. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance, beta-cell function, and diabetes in Hispanics and African Americans. J Diabetes Complicat. 2019;33(2):118–122. doi:10.1016/j.jdiacomp.2018.10.018
21. Liu PJ, Liu Y, Ma L, et al. The predictive ability of two triglyceride-associated indices for gestational diabetes mellitus and large for gestational age infant among Chinese pregnancies: a preliminary cohort study. Diabetes Metab Syndr Obes. 2020;13:2025–2035. doi:10.2147/DMSO.S251846
22. Dos Santos-Weiss IC, Rea RR, Fadel-Picheth CM, et al. The plasma logarithm of the triglyceride/HDL-cholesterol ratio is a predictor of low risk gestational diabetes in early pregnancy. Clin Chim Acta. 2013;418:1–4. doi:10.1016/j.cca.2012.12.004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

