Back to Journals » Advances in Medical Education and Practice » Volume 14
Consolidation Carnival: A Case-Based Approach to Reviewing Musculoskeletal Anatomy in an Undergraduate Medical Curriculum
Authors Bassey R , Hill RV , Nassrallah Z, Knutson S, Pinard B, Olvet DM, Rennie WP
Received 24 February 2023
Accepted for publication 29 July 2023
Published 11 August 2023 Volume 2023:14 Pages 889—897
DOI https://doi.org/10.2147/AMEP.S409797
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Rosemary Bassey, Robert V Hill, Zeinab Nassrallah, Shannon Knutson, Brian Pinard, Doreen M Olvet, William P Rennie
Department of Science Education, Donald and Barbara Zucker School of Medicine at Hofstra/ Northwell, Hempstead, NY, USA
Correspondence: Rosemary Bassey, Department of Science Education, Donald and Barbara Zucker School of Medicine at Hofstra/ Northwell, Hempstead, NY, 11549, USA, Tel +1 516 463-7504, Email [email protected]
Introduction: Recent changes in undergraduate medical curricula have resulted in time constraints that are particularly challenging, especially when students must learn large blocks of musculoskeletal anatomy content. Consequently, students have resorted to rote memorization to cope, which counteracts our established collaborative self-directed learning model.
Methods: For a 6-week musculoskeletal anatomy course, two structured case-based review sessions are described, each following the completion of two five-hour lab sessions, two on the upper extremities and two on the lower extremities. These largely self-directed review sessions consisted of 6 students rotating through 7 to 8 stations every 10 minutes where clinical cases with follow-up questions were projected on large screens. The students were expected to work collaboratively to solve the cases utilizing the prosected specimens provided and discuss the accompanying answers at the end of each case.
Results: Ninety-four per cent of the students who participated in this study agreed that the case-based review sessions provided a helpful overview of musculoskeletal anatomy content. Student performance on the open-ended, case-based musculoskeletal examination questions showed no significant difference in performance on shoulder, hand, hip, thigh, and leg questions. There was, however, a statistically significant decrease in the students’ scores on a forearm question in 2021 compared to 2019.
Conclusion: This paper describes our integrated, collaborative musculoskeletal course, including case-based review sessions, which was positively received by students as having value in reviewing the musculoskeletal content though it was not found to improve examination performance.
Keywords: musculoskeletal, anatomy, integrated curriculum, review, consolidation, evaluation
Introduction
Musculoskeletal diseases constitute approximately 20% of all primary care and emergency department visits with trauma, back pain, and arthritis being the three most reported.1,2 Unfortunately, the burden of musculoskeletal conditions is likely to become greater with every passing year due to the obesity epidemic, upsurge in incidence of road traffic accidents and the fast-growing population of the aged in the United States.3,4 Furthermore, patients with musculoskeletal disorders are managed by a wide-ranging group of providers including primary care physicians, emergency physicians, surgeons, physical medicine and rehabilitation physicians, anesthesiologists, neurologists, radiologists, rheumatologists, and physical therapists.5 The mismanagement of musculoskeletal injuries can delay treatment, ultimately resulting in long-term disability.6–8 Due to the multidisciplinary nature of musculoskeletal disorders, it is important that all physicians-in-training are provided with the requisite knowledge of musculoskeletal anatomy to properly manage patients in the clinical setting.
The past decade has seen significant changes in undergraduate medical education, with anatomy teaching at the forefront.9 Following the introduction of the integrated curriculum in medical schools, anatomy courses have undergone extensive restructuring, including reduction in teaching hours dedicated to formal anatomy education.10,11 These changes have triggered development of more pedagogies that optimize anatomy content delivery and improve learning outcomes by shifting away from rote memorization, and leaning more towards understanding of content, driven by case-based, problem-solving approaches.11–14 The implementation of mixed or multimodal learning strategies allows students to acquire knowledge from a variety of sources. This approach has become widely used in the delivery of musculoskeletal anatomy content in many US medical schools.15–17 Several studies have explored various teaching pedagogies for musculoskeletal anatomy including the use of dissection, prosections, plastic models and 3D anatomy software on students’ performance on musculoskeletal examinations.18–20 Structured exercises like yoga and Pilates to facilitate the learning of musculoskeletal anatomy have also been explored.21,22
Furthermore, the shift from discipline-based to competency-based curricula has necessitated more vertical integration of relevant clinical content into basic sciences. Hence, case-based learning (CBL) has become widely used as an interactive, inquiry-based learning method of linking theory to practice.23 Unlike problem-based learning (PBL), CBL is more structured and involves both student preparation and faculty guidance in case discussions, thereby reinforcing concepts and enhancing the critical thinking, collaborative, and communication skills of students.24 Another advantage of CBL is that it promotes self-directed learning (SDL), which is an important component of lifelong learning and therefore a vital competency in medical school curricula.25 Various studies have described the use of CBL in anatomy education through graded oral presentations designed by the first-year medical students,26 as well as the positive perception and efficacy of CBL in anatomy education compared to other teaching strategies.27–29
One important but commonly overlooked aspect is the role of structured reviews in active learning. Active review sessions are useful in helping the students to consolidate critical information, recognize gaps in their learning, and develop the thinking skills needed to approach examination questions.30 From its inception in 2008, the Zucker School of Medicine at Hofstra/Northwell (ZSOM) established an integrated curriculum founded on experiential, active small group case-based sessions and early patient interactions in the pre-clerkship years. The collaborative self-directed learning model has been one of the frameworks used to give our learners practical approaches to problem-solving. Based on this framework, we describe our 6-week musculoskeletal anatomy course including the structured case-based review sessions, which is based on the cognitivism educational theory that promotes cognitive reasoning by utilizing structured clinical cases with relevant open-ended questions.31 We coined the review sessions “Consolidation carnival” – consolidation because it is a review that aims to reinforce, and carnival because it has logistics of rotating booths and a few light-hearted circus-themed cases.
Methods
Curricular Context
Undergraduate medical education in the United States typically refers to the four years of medical school, comprising two years of pre-clerkship course work and two years of clinical clerkships. The musculoskeletal anatomy (MSK) laboratory sessions are a component of the longitudinal curriculum called “Structure” that takes place throughout the two-year pre-clerkship years at ZSOM. Structure in this context describes the amalgamation of different disciplines including gross anatomy, embryology, histology, imaging, pathology, physical diagnoses, and clinical medicine under one curricular umbrella to facilitate consolidation of normal, abnormal, and clinical interventions in learning. The design of each weekly Structure session varies depending on content but typically lasts for about five hours which consists of two-and-a-half hours rotating through four structure stations of 33 minutes each and two hours of additional complementary material such as ultrasound and physical diagnoses, with a 30-minute break in between. There are also a limited number of lecture-styled large group sessions in the Structure curriculum, notably focusing on topics in embryology and pathology.
MSK Structure Sessions
The MSK sessions occur in the fall of the second year of medical school as part of the “Interacting with the Environment” course.32 It is a 6-week curriculum consisting of 4 scheduled laboratory sessions: 2 for the upper limb (shoulder, arm, and brachial plexus in week 1; forearm and hand in week 2) and 2 for the lower limb (hip, thigh, and gluteal region in week 4; knee, ankle, leg, and foot in week 5). Interspersed between these content-rich sessions are 2 scheduled review sessions (weeks 3 and 6).
The students were provided with laboratory guides containing the goals, learning objectives, and required resources for dissection and station-based activities at least a week before each laboratory session (Appendix 1). Students were expected to prepare for each laboratory session by using the suggested text and multimedia resources to study for each station based on the learning objectives provided. Each laboratory session was split into two sections: half of the students engaged in faculty-guided cadaveric dissections for approximately two-and-a-half hours using the dissection guides and their assigned body donors. The other half of the students rotated in small groups, interacting with facilitators at four separate stations that focused on organizational principles, functional joint anatomy, radiology, and clinical applications. Table 1 shows the detailed list of MSK topics covered each week. At the conclusion of the first section, students swapped activities so that all students engaged in both dissection and station-based learning over the course of each 5-hour laboratory sessions.
 |
Table 1 Weekly Topics for the Musculoskeletal Structure Course |
Implementation
Participants
Data from second-year medical students in 2019 (N = 100) and 2021 (N = 103) were included in this study. Students were required to participate in the weekly Structure laboratory and review sessions. The review sessions were incorporated into the curriculum in 2021 and data from students in 2019 served as a historical control. Data from 2019 were used for this study in lieu of 2020 to control for any confounding variables that might exist due to the COVID-19 pandemic.
Consolidation Carnival (Case-Based Review Sessions)
In 2021, the class was split in half, with one half participating in a large group session focused on MSK clinical reasoning and the other half engaged in a case-based review session. Each half lasted for 1½ hours, after which the two groups switched so that all students participated in clinical reasoning and the case-based review session.
A figure showing the floor plan of the laboratory during the review is shown in Figure 1. Small groups of six to seven students rotated through each station. They were given 10 to 12 minutes to work on each case before rotating to the next station. At each station, a clinical vignette was presented as a single slide on a computer screen, including at least one image and a higher order, specimen-related question. A clearly prosected donor body at each station displayed the body region relevant to the corresponding vignette. Students were expected to discuss the case and identify the involved structures on the donor. They could advance the slide to reveal the answers, allowing for real-time checking of their responses. While each station was largely self-directed, there was one faculty facilitator at each station to answer questions and provide guidance. For the first review session (week 3), there were eight cases related to the upper extremities, including the shoulder, brachial plexus, arm, forearm, and hand (Appendix 2). For the second review session (week 6), there were seven cases related to the lower extremities, including the gluteal region, thigh, knee, leg, ankle, and foot (Appendix 3).
 |
Figure 1 Floor plan of the structure laboratory during review sessions. |
Historical Control
In the years prior to 2021, optional reviews were scheduled in weeks three and six. These were largely self-directed and consisted of pinned, prosected specimens displayed in the Structure laboratory with corresponding practice questions (both open-ended and multiple-choice). This “open laboratory” format allowed for interested students to identify pinned structures and answer the questions.
Evaluation
At the end of the MSK sessions, students were sent an anonymous electronic course evaluation survey. There was one question regarding the MSK review: “The [review] provided a helpful overview of key concepts from musculoskeletal structure labs”. Response to this question was based on a 5-point Likert-scale with the following anchors: 1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree. At the end of the evaluation, students were asked to provide general feedback in an open-ended format.
We analyzed academic performance on the 2019 and 2021 MSK examinations to determine if the consolidation carnival impacted students’ performance in the end-of-course summative examinations. At ZSOM, summative exams are administered as constructed-response short answer questions, each response being scored using an analytic rubric.33 There were a total of 28 questions on the exam, each ranging from 2 to 5 points for a total of 103 possible points, which was thereafter converted to percentage scores. Each question was graded by one faculty member to assure that it was graded consistently. Student responses are always anonymous, so the graders do not know the identity of the student while they are grading. The examination questions analyzed were representative of all the areas covered in structure laboratory and review sessions which included shoulder, arm, brachial plexus, forearm, hand, hip, thigh, knee, leg, and ankle.
Data were statistically evaluated using IBM SPSS Statistics (SPSS Inc., Chicago, IL, USA, Version 24.0). Figures are presented as the mean (M) and standard error of mean (SD) score for various components of the upper and lower limbs. A Student’s t-test was used to compare exam performance of the historical control group (2019 MSK exam scores) and the consolidation carnival group (2021 MSK exam scores). A p-value ≤ 0.05 was considered statistically significant.
Ethical Consideration
Ethical approval was obtained from Hofstra University Institutional Review Board. The study was approved under Exempt Review procedures of the University’s Institutional Review Board governing the use of humans as research subjects (HUIRB Approval Ref#: 20220222-SOM-BAS-1).
Results
Students’ Perception of the Consolidation Carnival
Student feedback serves as a useful basis for modifying and refining medical education, especially because the integrated medical curriculum is designed to be student-centered.34
The Consolidation carnival was made up of two case-based review sessions as part of the MSK course. Ninety-seven out of 103 students completed the post-course evaluation (94%). In response to the question asking if the consolidation carnival provided helpful overview of key concepts from the musculoskeletal structure lab, 91 respondents (94%) agreed or strongly agreed, 5 (5%) were neutral, 1 (1%) disagreed while none strongly disagreed (Figure 2). For the open-ended general feedback regarding the case-based review sessions, students expressed their satisfaction as follows:
- “I loved the consolidation carnival for MSK and thought that it was a really helpful way to assess how much I had learned from the prior sessions and what I still needed to work on”.
- “The Consolidation Carnival was a great way to go over the main takeaways from the lab”.
- “The effort that the faculty put in in helping us consolidate and review via the massive review sessions and the consolidation carnival were EXTREMELY helpful!!! If we could always have something like this during every block that would be fabulous. Thank you!!!”
- “The consolidation/review sessions were great (Carnival and final week reinforcement sessions)”.
 |
Figure 2 Student’s responses to a 5-point Likert scale survey: The “Consolidation Carnival” provided a helpful overview of key concepts from musculoskeletal structure labs. |
MSK Examination Performance
We assessed the impact of the review sessions on student learning outcomes by comparing identically-worded questions used in both 2021 and 2019 MSK examinations. Three questions focused on the upper extremities, representing shoulder and arm, forearm, and hand were selected and analyzed. The selection of the questions was based on those that were repeated in both 2019 and 2021. Table 2 shows the mean and standard deviation for upper extremity scores for each group. There was no significant difference in the students’ scores on the shoulder (t (201) = 0.94, p = 0.35) or hand question (t (201) = −1.84, p = 0.07). There was, however, a statistically significant decrease in the students’ scores on a forearm question in 2021 compared to 2019 (t (201) = 2.37, p = 0.02).
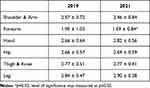 |
Table 2 Mean ± Standard Deviation of Examination Scores for Upper and Lower Extremities in 2019 and 2021 |
For the lower limb open-ended essay questions in the MSK examinations that were repeated in 2019 and 2021, three questions representing the hip, thigh and leg were selected and analyzed. Table 2 also shows the mean and standard error of mean for lower extremity scores for each group. There was no significant difference in the students’ scores on a hip (t (201) =−0.42, p=0.68), thigh (t (201) =−0.05, p=0.96) or leg question (t. (201) =−1.05, p=0.30).
Discussion
In this study, we described the consolidation carnival – a case-based review exercise designed for our musculoskeletal structure curriculum. We also assessed students’ perception and measured examination performance outcomes. Musculoskeletal anatomy, and gross anatomy in general, is an enduring challenge for medical students due to the large volume of new knowledge that must be acquired within a short time. This has caused students to resort to rote memorization which is mostly useful for short-term recall, during review for assessments, mostly without the necessary integration of fundamental concepts.35 Therefore, focus should also go into consolidation efforts described in this study, which is critical to successful learning.36 To the best of our knowledge, there is no research on the use of CBL in anatomy review sessions, hence the impetus for inclusion of structured review sessions as part of a continuous learning experience in the musculoskeletal curriculum.
The structure of the review exercise described in this study went beyond the passive method of questioning, and answers requiring repetition of facts from didactic lectures. This is in line with core definitions of CBL which involve prior knowledge, clear objectives, clinical cases, and student-led inquiry with guidance and feedback from faculty.37 In addition to the CBL approach being a student-centered, active learning style, it ensured that the students had the opportunity for (1) problem-solving and critical thinking, (2) building on existing knowledge, and (3) learning from their peers through in-depth discussions and collaboration in a low-stakes, low-stress environment.38 Additionally, the CBL approach to reviewing the MSK course fostered a deeper approach to learning the subject through application of their knowledge towards solving the cases in lieu of superficial reproduction of facts.39 The timing of the review sessions at the end of each of the extremity sections was also critical as it served as a form of retrieval practice,40 although it was not designed as a test in the traditional sense of the word, but a formative exercise. Retrieval practice based on the testing effect is an active process of learning through testing which has been shown to improve long-term retention as opposed to learning the written information from textbooks which does not involve the critical retrieval process.41 This process is often more successful soon after initial learning of the subject.40 Moreover, as memories are retrieved in these structured review sessions, they become more pliable and receptive to being updated with new knowledge, which further strengthens the memory.42
The usefulness of the consolidation carnival to the students’ overall learning experience was supported by the positive feedback received in the post-session evaluation. Our findings highlight the generally positive perception of students towards CBL as seen in other studies which compared CBL to other teaching strategies.26,28,29 The answers provided at the end of each case and immediate feedback provided by faculty through Socratic questioning during these sessions were useful in closing some knowledge gaps and further promoting self-reflection – known to have a great impact on learning.38 Besides, feedback that includes the correct answer increases learning because it helps to correct errors and helps successful memory retrieval.40 Likewise, Socratic technique is a systematic inquiry that deeply probes or explores the meaning, rationalization, or logical strength of a line of reasoning as part of the learning process.43,44 This method of inquiry is a core to successful implementation of CBL, encouraging the shift from memorizing facts to the application of independent and critical thinking skills in problem solving.23,44,45
A well-designed and integrated assessment is an important tool in determining learning outcomes and the effectiveness of an educational process.46 The students’ scores on the short, open-ended, case-based MSK examination showed no significant difference in students’ scores on the shoulder, hand, hip, thigh, and leg questions. While there was a statistically significant decrease in the students’ scores on the forearm question in 2021 compared to 2019, there was also a stability of the students’ scores in most of the examination questions in both 2019 and 2021. Previous studies have reported significantly better scores in post-tests following the implementation of CBL as a teaching strategy compared to traditional didactic methods.27 Our approach differs in that it was focused on a review session and not a primary teaching strategy. Our findings as regards examination performance bring to attention the gap that exists in understanding the relationship between revision exercises conducted in a lower stress learning environment and examination performance completed under a higher degree of stress.47
Limitations of the Study
At ZSOM, we use exclusively short essay style, open-ended questions (OEQs), even for anatomy practical exams.33 This necessitates creative wording of clinical vignettes such that some questions are similar, but not identical, from year to year. Since we chose to analyze only the questions that were identical, this reduced the number of examination questions that could be compared between the two years. Additionally, we studied the effect of this structured review session for only one body system as part of a larger, integrated course and cannot at present extrapolate these results to other courses.
Conclusion
The case-based review sessions were useful in consolidation of the MSK course, though they did not significantly improve examination performance. Their effectiveness can be attributed to the active learning approach which made learning of MSK more relevant and interest-provoking. These data and feedback will serve as an important tool to guide future strategies in improving students’ learning experience during the MSK course.
Acknowledgment
The authors thank the body donors whose generous gifts made this anatomical review session possible. We also thank Joanne Willey for sharing her expertise and guidance in the development of this manuscript. Jeff Bird and Judith Brenner provided access to assessment and evaluation data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Craton N, Matheson GO. Training and clinical competency in musculoskeletal medicine. Identifying the problem. Sports Med. 1993;15(5):328–337. doi:10.2165/00007256-199315050-00004
2. Grunfeld R, Banks S, Fox E, Levy BA, Craig C, Black K. An assessment of musculoskeletal knowledge in graduating medical and physician assistant students and implications for musculoskeletal care providers. J Bone Joint Surg Am. 2012;94(4):343–348. doi:10.2106/JBJS.J.00417
3. Woolf AD, Akesson K. Understanding the burden of musculoskeletal conditions. The burden is huge and not reflected in national health priorities. BMJ. 2001;322(7294):1079–1080. doi:10.1136/bmj.322.7294.1079
4. Initiative USBaJ. The Burden of Musculoskeletal Diseases in the United States (BMUS). Rosemont, IL: Initiative USBaJ; 2014:11.
5. Malik KM, Beckerly R, Imani F. Musculoskeletal disorders a universal source of pain and disability misunderstood and mismanaged: a critical analysis based on the U.S. model of care. Anesth Pain Med. 2018;8(6):e85532. doi:10.5812/aapm.85532
6. Guly HR. Diagnostic errors in an accident and emergency department. Emerg Med J. 2001;18(4):263–269. doi:10.1136/emj.18.4.263
7. Hallas P, Ellingsen T. Errors in fracture diagnoses in the emergency department--characteristics of patients and diurnal variation. BMC Emerg Med. 2006;6:4. doi:10.1186/1471-227X-6-4
8. Li W, Stimec J, Camp M, Pusic M, Herman J, Boutis K. Pediatric musculoskeletal radiographs: anatomy and fractures prone to diagnostic error among emergency physicians. J Emerg Med. 2022;62(4):524–533. doi:10.1016/j.jemermed.2021.12.021
9. Chapman SJ, Hakeem AR, Marangoni G, Prasad KR. Anatomy in medical education: perceptions of undergraduate medical students. Ann Anat. 2013;195(5):409–414. doi:10.1016/j.aanat.2013.03.005
10. Irby DM, Cooke M, O’Brien BC. Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad Med. 2010;85(2):220–227. doi:10.1097/ACM.0b013e3181c88449
11. Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2(6):253–259. doi:10.1002/ase.117
12. Mitchell R, Batty L. Undergraduate perspectives on the teaching and learning of anatomy. ANZ J Surg. 2009;79(3):118–121. doi:10.1111/j.1445-2197.2008.04826.x
13. Collins JP. Modern approaches to teaching and learning anatomy. BMJ. 2008;337:a1310. doi:10.1136/bmj.a1310
14. Miller SA, Perrotti W, Silverthorn DU, Dalley AF, Rarey KE. From college to clinic: reasoning over memorization is key for understanding anatomy. Anat Rec. 2002;269(2):69–80. doi:10.1002/ar.10071
15. Bergman EM, Sieben JM, Smailbegovic I, de Bruin AB, Scherpbier AJ, van der Vleuten CP. Constructive, collaborative, contextual, and self-directed learning in surface anatomy education. Anat Sci Educ. 2013;6(2):114–124. doi:10.1002/ase.1306
16. Davis CR, Bates AS, Ellis H, Roberts AM. Human anatomy: let the students tell us how to teach. Anat Sci Educ. 2014;7(4):262–272. doi:10.1002/ase.1424
17. Johnson EO, Charchanti AV, Troupis TG. Modernization of an anatomy class: from conceptualization to implementation. A case for integrated multimodal-multidisciplinary teaching. Anat Sci Educ. 2012;5(6):354–366. doi:10.1002/ase.1296
18. Peeler J, Bergen H, Bulow A. Musculoskeletal anatomy education: evaluating the influence of different teaching and learning activities on medical students perception and academic performance. Ann Anat. 2018;219:44–50. doi:10.1016/j.aanat.2018.05.004
19. Zibis A, Mitrousias V, Varitimidis S, Raoulis V, Fyllos A, Arvanitis D. Musculoskeletal anatomy: evaluation and comparison of common teaching and learning modalities. Sci Rep. 2021;11(1):1517. doi:10.1038/s41598-020-80860-7
20. Mustafa AG, Taha NR, Zaqout S, Ahmed MS. Teaching musculoskeletal module using dissection videos: feedback from medical students. BMC Med Educ. 2021;21(1):604. doi:10.1186/s12909-021-03036-5
21. Canoso JJ, Saavedra M, Pascual-Ramos V, Sánchez-Valencia MA, Kalish RA. Musculoskeletal anatomy by self-examination: a learner-centered method for students and practitioners of musculoskeletal medicine. Ann Anat. 2020;228:151457. doi:10.1016/j.aanat.2019.151457
22. McCulloch C, Marango SP, Friedman ES, Laitman JT. Living AnatoME: teaching and learning musculoskeletal anatomy through yoga and pilates. Anat Sci Educ. 2010;3(6):279–286. doi:10.1002/ase.181
23. Thistlethwaite JE, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach. 2012;34(6):e421–44. doi:10.3109/0142159X.2012.680939
24. Srinivasan M, Wilkes M, Stevenson F, Nguyen T, Slavin S. Comparing problem-based learning with case-based learning: effects of a major curricular shift at two institutions. Acad Med. 2007;82(1):74–82. doi:10.1097/01.ACM.0000249963.93776.aa
25. Eva KW, Cunnington JPW, Reiter HI, Keane DR, Norman GR. How can I know what I don’t know? Poor self assessment in a well-defined domain. Adv Health Sci Educ. 2004;9:211–224. doi:10.1023/B:AHSE.0000038209.65714.d4
26. Singh K, Bharatha A, Sa B, Adams OP, Majumder MAA. Teaching anatomy using an active and engaging learning strategy. BMC Med Educ. 2019;19(1):149. doi:10.1186/s12909-019-1590-2
27. Sangam MR, Bokan RR, Deka R, Kaur A, Deka R, Kaur A. Efficacy of Case-Based Learning in Anatomy. Cureus. 2021;13(12):e20472. doi:10.7759/cureus.20472
28. Maia D, Andrade R, Afonso J, et al. Academic Performance and Perceptions of Undergraduate Medical Students in Case-Based Learning Compared to Other Teaching Strategies: A Systematic Review with Meta-Analysis. Educ Sci. 2023;13(3):238.
29. Vedi N, Dulloo P. Students’ perception and learning on case based teaching in anatomy and physiology: an e-learning approach. J Adv Med Educ Prof. 2021;9(1):8–17. doi:10.30476/jamp.2020.87332.1304
30. Favero TG. Active review sessions can advance student learning. Adv Physiol Educ. 2011;35(3):247–248. doi:10.1152/advan.00040.2011
31. Dong H, Lio J, Sherer R, Jiang I. Some learning theories for medical educators. Med Sci Educ. 2021;31(3):1157–1172. doi:10.1007/s40670-021-01270-6
32. Ginzburg S, Brenner J, Willey J. Integration: a Strategy for Turning Knowledge into Action. Med Sci Edu. 2015;25:533–543. doi:10.1007/s40670-015-0174-y
33. Bird JB, Olvet DM, Willey JM, Brenner J. Patients don’t come with multiple choice options: essay-based assessment in UME. Med Educ Online. 2019;24(1):1649959. doi:10.1080/10872981.2019.1649959
34. Bandyopadhyay R, Biswas R. Students’ perception and attitude on methods of anatomy teaching in a medical college of West Bengal, India. J Clin Diagn Res. 2017;11(9):AC10–AC14. doi:10.7860/JCDR/2017/26112.10666
35. Radcliffe C, Lester H. Perceived stress during undergraduate medical training: a qualitative study. Med Educ. 2003;37(1):32–38. doi:10.1046/j.1365-2923.2003.01405.x
36. Yang BW, Razo J, Persky AM. Using Testing as a Learning Tool. Am J Pharm Educ. 2019;83(9):7324. doi:10.5688/ajpe7324
37. McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3. doi:10.4137/JMECD.S20377
38. van Diggele C, Burgess A, Mellis C Planning, preparing and structuring a small group teaching session. BMC Med Educ. 2020;20(Suppl 2):462. doi:10.1186/s12909-020-02281-4
39. Thistlethwaite JE. Learning and Teaching Anatomy Through Case-Based Learning (CBL). In: Chan L, Pawlina W, editors. Teaching Anatomy. Cham: Springer; 2015:125–132.
40. Roediger HL, Butler AC. The critical role of retrieval practice in long-term retention. Trends Cogn Sci. 2011;15(1):20–27. doi:10.1016/j.tics.2010.09.003
41. Bobby Z, Meiyappan K. ”Test-enhanced” focused self-directed learning after the teaching modules in biochemistry. Biochem Mol Biol Educ. 2018;46(5):472–477. doi:10.1002/bmb.21171
42. Larsen DP. Planning education for long-term retention: the cognitive science and implementation of retrieval practice. Semin Neurol. 2018;38(4):449–456. doi:10.1055/s-0038-1666983
43. Makhene A. The use of the Socratic inquiry to facilitate critical thinking in nursing education. Health SA. 2019;24:1224. doi:10.4102/hsag.v24i0.1224
44. Zare P, Mukundan J. The use of Socratic method as a teaching/learning tool to develop students’ critical thinking: a review of literature. Language India. 2015;15:256–265.
45. Kost A, Chen FM. Socrates was not a pimp: changing the paradigm of questioning in medical education. Acad Med. 2015;90:20–24. doi:10.1097/ACM.0000000000000446
46. Elshama SS. How to use and apply assessment tools in medical education? Iberoam J Med. 2020;2:351–359. doi:10.53986/ibjm.2020.0059
47. Cross S, Whitelock D, Mittelmeier J. Does the Quality and Quantity of Exam Revision Impact on Student Satisfaction and Performance in the Exam Itself?: perspectives from Undergraduate Distance Learners. In: EDULEARN16 Proceedings. IATED Academy; 2016:5052–5061.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
