Back to Journals » ImmunoTargets and Therapy » Volume 13
Comprehension of Calcitriol Levels in Pregnant Women With Latent Tuberculosis and Immune Function in their Newborns
Authors Meirina F, Sari DK , Lubis IND, Daulay RS, Yani FF , Lubis BM, Sembiring RJ, Pandia P, Rusda M, Amin MM
Received 9 October 2023
Accepted for publication 8 March 2024
Published 8 April 2024 Volume 2024:13 Pages 195—204
DOI https://doi.org/10.2147/ITT.S436765
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Michael Shurin
Fathia Meirina,1 Dina Keumala Sari,2 Inke Nadia Diniyanti Lubis,1 Rini Savitri Daulay,1 Finny Fitry Yani,3 Bugis Mardina Lubis,1 Rosita Juwita Sembiring,4 Pandiaman Pandia,5 Muhammad Rusda,6 Mustafa Mahmud Amin7
1Department of Pediatrics, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia; 2Department of Nutrition, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia; 3Department of Pediatrics, Faculty of Medicine, Universitas Andalas, Padang, Indonesia; 4Department of Clinical Pathology, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia; 5Department of Pulmonology and Respiratory, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia; 6Department of Obstetrics & Gynecology, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia; 7Department of Psychiatry, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
Correspondence: Fathia Meirina, Email [email protected]
Background: Pregnant women with latent tuberculosis infection (LTBI) may develop active tuberculosis infection and could infect their neonates, which could impair the child’s immune system due to infection-mediated immunological responses. In order to develop a preventative TB program in this study, we desired to understand the impact of calcitriol in LTBI pregnant women and immunological responses in neonates.
Patients and Methods: In three hospitals in Medan, North Sumatra, we implemented a case-control design with 84 pregnant women in their third trimester and their newborns. We determined the levels of calcitriol, cathelicidin, and interferon gamma (IFN-γ) in women between December 2021 and July 2022. These measurements were then compared to the newborns’ levels of calcitriol, cathelicidin, IFN-γ, and Toll-Like Receptor (TLR) 2. Analyses were performed using the Chi-squared and Fisher’s tests, while Spearman correlations were employed to assess for correlations.
Results: 42 pregnant women with LTBI (interferon gamma release assay (IGRA) positive) and 42 pregnant women without LTBI (IGRA negative) participated in the study. The findings demonstrated that pregnant women with LTBI were at increased risk for calcitriol deficiency (Odds Ratio (OR) = 3.667, p = 0.006), which had an impact on the calcitriol levels of their unborn children (p = 0.038). TLR2 levels and calcitriol levels were substantially associated with LTBI pregnant women and their healthy neonates (p = 0.048; p = 0.005). Cathelicidin levels in the newborns of non-LTBI pregnant women were influenced by their higher calcitriol levels (p = 0.043). Pregnant women with LTBI had higher levels of cathelicidin and IFN-γ than those without it (p = 0.03; p = 0.001).
Conclusion: Pregnant LTBI women’s calcitriol levels had an impact on the calcitriol levels of their newborns. Mother’s immunological responses and babies’ calcitriol levels affected the levels of cathelicidin, IFN-γ, and TLR2 in newborns.
keywords: pregnancy, newborns, latent tb, calcitriol, immunity
Introduction
With 230000 pediatric TB deaths reported in 2019 out of a total of 1.2 million, Children’s TB is one of the leading causes of sickness and death worldwide.1,2 Around 845,000 cases of TB were reported in Indonesia in 2020, with 28% of cases staying untreated and 34% obtaining effective therapeutic care.3 With 3% per 100.000 population of pregnant women, Indonesia has a 312/100,000 TB prevalence in 2022.4,5 Worldwide, 900 million women have LTBI, which, depending on their immune level, could develop into an active TB infection.6 The innate immune response of the host serves as the immune system’s first line of defense against all pathogens, including Mycobacterium tuberculosis, and this further triggers the adaptive immune response.1 Cathelicidin, interferon gamma (IFN-γ), and toll-like receptors (TLR) are significant mediators of the inflammatory response against M. tuberculosis.7,8 At the level of the macrophage, which is involved in cathelicidin and interferon gamma (IFN-γ) mediated activity against mycobacteria, calcitriol affects the pathogenesis of M. tuberculosis infection or illness.7
There are temporal changes in immunity throughout pregnancy, and pregnant women have a unique immunological profile compared to non-pregnant adults. Supplementing with calcitriol during pregnancy considering that calcitriol may have an impact on placental inflammation.9–11 Pregnant women’s calcitriol levels may have an impact on the fetal immune system and their children’s risk of contracting diseases.12,13 According to multiple studies, there is no direct link between calcitriol levels in pregnant women and the incidence of delivery problems such infections and atopic dermatitis in children.14,15 Another study reported that low calcitriol levels in patients with tuberculosis during pregnancy can affect the fetal immune system and increase the risk of congenital disease in neonates. This is supported by a meta-analysis study that reported low calcitriol in pregnant women will increase the risk of tuberculosis infection in children and calcitriol deficiency.7,8
In this work, we investigated the relationship between calcitriol levels in LTBI pregnant women and calcitriol levels in their newborns as well as the relationship between cathelicidin, TLR2, and IFN- levels in the newborns. We also examined the effects of cathelicidin and IFN-γ levels in LTBI pregnant women on the cathelicidin and IFN-γ levels of their neonates in order to ensure that both the children and mothers with LTBI have an adequate immune system to preventative TB activity.
Methods
Study Design
84 pregnant women in their third trimester and their newborns were involved in our case control study. The women were divided into two groups according to whether they had LTBI (IGRA-positive or -negative). Between December 2021 and July 2022, we measured calcitriol, cathelicidin, IFN-γ, and TLR2 levels for each participant. Three hospitals (Medan, North Sumatera) recruited the participants, who frequently underwent prenatal examinations and gave birth to their children there. Prior to taking part, participants gave their consent after being informed.
Participants
Participants who met the inclusion and exclusion criteria were chosen using the sequential sampling method. The inclusion criteria were third-trimester pregnant women without problems who delivered healthy newborns at term without postpartum respiratory distress. Exclusion criteria included COVID-19 infections, pregnant women with comorbidities such hypertension, diabetes mellitus, or eclampsia, bone diseases and neonates who were later found to have respiratory distress. A daily 1000 IU calcitriol supplement was given to participants by their obstetric and gynecologist specialists. Initially, 116 pregnant women in their third trimester were included in the study. However, 84 women were selected (42 in the case group and 42 in the control group) after applying the inclusion and exclusion criteria.
Statistical Analysis
For data analysis, we used IBM SPSS version 11.5 (IBM Corp., Chicago, IL, USA). Chi-squared tests were performed to examine correlations among categorical parameters. Categorical variables were shown as percentages. When the conditions for the Chi-squared test could not be met, Fisher’s tests were utilized. Kolmogorov–Smirnov test methods were originally used to assess continuous data distributions. Pearson’s parametric tests were applied to determine associations between calcitriol levels and cathelicidin, IFN-γ, and TLR2 levels in newborns. The significance level for the results was 0.05.
Sample Size and Power Calculations
To select the biggest sample size and create a representative sample from the population, we used systematic random selection. For example, 80% power and -values were determined via purposeful sampling. Investigating relationships between calcitriol and levels of cathelicidin, IFN-γ, and TLR2 was our main goal. Each two-tailed hypothesis test’s minimum sample size was calculated using significance at 0.05.
Examinations
Measurements were made twice, with the average being used. Before giving birth, ladies had blood drawn from the medial cubiti vein on either their left or right arm. Exams were performed in the Medical Faculty Integrated Laboratory at the University of North Sumatera. During birth, blood samples from the umbilical cord were collected. IGRA testing was carried out utilizing the Elispot Enzyme-linked Immunosorbent Spot Assay (Elispot), which counted spots on incubated materials and was used to classify case and control groups. Under a microscope, the specimens were examined; if five spots were present, the sample was IGRA-negative, while six spots indicated that it was IGRA-positive.
On samples from the mother and the child, enzyme-linked immunosorbent assay (ELISA) kits (DiaSorin, USA) were used to measure the calcitriol levels. Calcitriol levels in newborns were normal (>20 ng/mL), insufficient 12–20 ng/mL, and deficient (12 ng/mL).16 Insufficient levels of calcitriol in mothers were between 21 and 29 ng/mL, while inadequate levels were below 20 ng/mL. Human Cathelicidin Antimicrobial Peptide ELISA kits (Bioassay Technology Laboratory, Birmingham, UK) were used for the cathelicidin testing, and levels were expressed in ng/mL. Human IFN-γ ELISA Kits (Millipore, Sigma-Aldrich, Missouri-US) were used to measure IFN-γ levels.
We used real-time polymerase chain reaction (RT-PCR) to evaluate TLR2 in newborns. RNA was initially extracted from the umbilical cord. Then, 40 cycles of RT-PCR were performed in an RNA thermal cycler: denaturation at 50°C for 2 minutes, followed by 10 minutes at 95°C, then 15 minutes at 95°C, and finally 1 minute at 60°C. The TLR2 primers were 5’-TTGTGCCCATTGCTCTTTTCAC-3’ and 5’-TGGCATTGTCCAGTGCTTCA-3’, whereas the -actin primers were 5’-AGCCTCGCCTTTGCCGA-3’ and 5’-CTGGTGCCTGGGGCG-3’. Sigma-Aldrich (Missouri, US) was used for both the RNA isolation and the RT PCR. According to Livak et al (2001), gene expression analyses were carried out, where the higher the gene expression, the lower the delta cycle threshold (CT) value.17
Results
116 expecting mothers visited the three hospitals during the study. Twelve COVID-19 infections were confirmed, five women declined to take part, and four had preeclampsia diagnoses. 95 ladies thereby met the requirements for inclusion and gave their permission to take part. 52 of the women who underwent IGRA testing were classified as not having LTBI (IGRA-negative), while 43 were classified as having LTBI (IGRA-positive). Ten non-LTBI women dropped out of the study because they did not show up, and one non-LTBI woman dropped out because her baby died during childbirth. As a result, 84 newborns met the criterion for inclusion. According to sample estimates, the case group consisted of 42 pregnant women with LTBI and their babies, while the control group consisted of 42 pregnant women without LTBI and their newborns (Figure 1). The average gestational age was 38 to 40 weeks, and the average age of the women was 24 to 42. The majority of newborns were healthy.
 |
Figure 1 Sample estimates. |
24 LTBI pregnant women had normal calcitriol levels, 14 had insufficient calcitriol, and four had calcitriol deficiency. Pregnant women without LTBI did not have calcitriol shortages. Regardless of LTBI status, calcitriol studies in pregnant women and their neonates did not reveal any appreciable changes (Table 1).
 |
Table 1 Based on the Mother’s Calcitriol Levels, the Newborn’s Vitamin |
Pregnant women with LTBI had lower calcitriol levels than pregnant women without LTBI, although this difference was not statistically significant (p = 0.293). Of the 84 neonates, 45 had insufficient calcitriol, 33 had insufficient calcitriol, and six had appropriate levels. Six neonates born to non-LTBI pregnant women had normal levels of calcitriol, whereas newborns born to LTBI pregnant women did not. When compared to neonates from non-LTBI pregnant women, newborns from LTBI pregnant women had lower calcitriol levels, but the differences were not statistically significant (p = 0.785, Table 2).
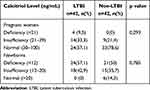 |
Table 2 Categorizes the Levels of Calcitriol in Pregnant Women and Their Newborns into LTBI Groups and Non-LTBI Groups |
LTBI was a major risk factor for calcitriol deficiency, according to LTBI risk assessments in relation to calcitriol levels in pregnant women. When compared to non-LTBI peers, pregnant women with LTBI were roughly 3.667 times more likely to be calcitriol deficient (Table 3).
 |
Table 3 The Relationship Between Calcitriol Levels in Pregnant Women and Newborns |
When statistical analyses were done on relationships between calcitriol levels in pregnant women and the LTBI status of their newborns, calcitriol levels in these women had an impact on calcitriol levels in their newborns (p = 0.038, Table 4), according to the classification of calcitriol levels in pregnant women and newborns as “normal” and “low” levels.
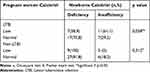 |
Table 4 The Relationship Between Low Levels of Calcitriol in Pregnant Women and Newborns |
Cathelicidin levels in newborns born to LTBI pregnant women were not significantly correlated with calcitriol levels (Table 5). However, in newborn calcitriol status assessments, a significant correlation was found between low cathelicidin levels in LTBI pregnant women and low calcitriol levels in newborns (p = 0.043, r = 0.481; Table 6). Studies found no connection between calcitriol levels in neonates born to LTBI pregnant women and newborn IFN-γ levels (p > 0.05; Table 5) or between calcitriol levels in newborns born to non-LTBI pregnant women and newborn IFN-γ levels. When comparing the outcomes depending on the calcitriol levels of the newborns, the same conclusions were reached (p > 0.05; Table 6).
 |
Table 5 The Relationship Between the Level of Calcitriol in Pregnant Women and the Levels of Tool-Like Receptor 2, Interferon Gamma, and Cathelicidin in Newborns |
 |
Table 6 The Relationship Between Calcitriol Levels in Pregnant Women and Tool-Like Receptor 2, Interferon Gamma, and Cathelicidin Levels in Newborns |
The levels of cathelicidin and calcitriol in babies delivered to LTBI pregnant women were not significantly correlate with one another (Table 5). However, in assessments of babies’ calcitriol status, a significant correlation was found between low levels of cathelicidin in LTBI pregnant women and low levels of calcitriol in neonates (p = 0.043, r = 0.481; Table 6). No significant association between calcitriol levels in neonates born to LTBI pregnant women and newborn IFN-γ levels was found in the analyses (p > 0.05; Table 5), nor were there any significant relationships between calcitriol levels in newborns born to non-LTBI pregnant women and newborn IFN-γ levels. When the newborn’s calcitriol levels were taken into account, the same outcomes were found (p > 0.05; Table 6).
When the relationships between the levels of the cathelicidin in LTBI pregnant women and the levels of the cathelicidin and TLR2 in their newborns were examined, a p value of 0.033 was produced, indicating a statistically significant relationship between the levels of the cathelicidin in LTBI pregnant women and the levels of the cathelicidin in the newborns. The correlation between the mother’s cathelicidin levels and the newborn’s cathelicidin levels was found to be 69.2% (R2 = 0.692), with a coefficient number of 1.357. IFN-γ levels in LTBI pregnant women and neonates were shown to be significantly correlated (p-value = 0.001) with one another (Table 7).
 |
Table 7 The Effects of Cathelicidin and Interferon on Expectant Mothers and Newborns |
Discussion
In our study, we found that 45.3% of the 95 pregnant women had LTBI. 32.1% (27) of the 84 pregnant women had inadequate calcitriol levels. This finding was in line with a study conducted in Indonesia in 2014, when 95% of 145 adult women were calcitriol deficient.16–19 Comparing LTBI pregnant women to non-LTBI counterparts, LTBI pregnant women exhibited lower calcitriol levels and a 3.7 times higher risk of calcitriol insufficiency. According to earlier studies, calcitriol levels in pregnant women were considerably impacted by bacterial infections,20,21 and TB-infected people had lower calcitriol levels than non-infected people.22–24 The body’s immune responses, such as cell division, proliferation, and bacterial phagocytosis, are controlled by active calcitriol metabolites that work at the cellular level to support the body’s own immune system.23,25 Increased calcitriol active metabolites aid immune cells in phagocytizing germs, which may impact calcitriol levels, as immune responses against M. tuberculosis involve both non-specific and specific natural immune systems.
Calcitriol levels in LTBI pregnant women and their babies were shown to be significantly correlated (p = 0.038). This was in line with studies from Poland, Nepal, Malaysia, and Indonesia, where nearly all neonates had calcitriol shortages and babies born to mothers with low calcitriol levels did not have adequate calcitriol levels.21,26–28 Through the transplacental pathway during intrauterine growth, maternal calcitriol levels are used to produce calcitriol for newborns. Inactive calcitriol (25(OH)D) is the primary calcitriol metabolite that crosses the placenta, and levels from the umbilical cord account for two-thirds of the mother’s calcitriol levels. As a result, the baby’s calcitriol levels may be impacted if the mother has a calcitriol shortage or insufficiency.29–31 Fetal growth and development stages make use of active calcitriol metabolites.32 According to our study, newborns receive 2/3 of their calcitriol supply from their mothers, and the high utilization of active calcitriol metabolites for fetal growth and development during the fetal period can affect the levels of inactive calcitriol in fetal blood circulation. These factors may contribute to low calcitriol levels in newborns delivered to mothers with low or normal calcitriol levels.
Cathelicidin typically increases during inflammatory processes brought on by bacterial infection and plays crucial functions in non-specific immune responses. In our study, cathelicidin mean values increased above normal limits in newborns and pregnant women with LTBI (normal range = 2.71 3.57 ng/mL). Only newborns were studied for IFN-γ levels, and those from LTBI pregnant women had greater mean IFN-γ levels than their non-LTBI counterparts (healthy neonate range = 17.5–38.5 pg/mL). The average IFN-γ levels in pregnant LTBI women were similarly higher than expected (healthy adult range = 1.4 to 1.34 pg/mL).33–36
This finding was consistent with earlier study that identified elevated cathelicidin levels in tracheal cells as a biomarker for the immune system’s ability to protect against TB and respiratory infections in neonates with acute respiratory infections. IFN-γ is a crucial cytokine in newborns; it reduces the likelihood of respiratory infections and is a cytokine of the early response to M. tuberculosis infection. Newborns’ elevated levels of cathelicidin and IFN-γ were presumably brought on by bacterial exposure during delivery. When a newborn breathes or cries for the first time, bacteria and/or viruses may enter their respiratory system, triggering normal, non-specific immune responses and raising cathelicidin and IFN-γ levels.37–40
LTBI pregnant women’s calcitriol levels did not alter the cathelicidin and IFN-γ levels in their neonates, but the newborns’ calcitriol status did affect the cathelicidin levels. Calcitriol plays immunomodulatory roles in pregnant women with LTBI and persistent infections, where immune response elements (cathelicidin and IFN-γ) are linked to the development of the child’s immune system from the time of conception. High levels of cathelicidin and IFN-γ in LTBI pregnant women suggested active immune responses that successfully fought infection. The general health of LTBI-pregnant moms and their unborn children made this clear. Mothers and newborns were in good health and showed no diseases at the time when LTBI pregnant women were hospitalized to the hospital until discharge after giving birth.
The absence of long-term participant monitoring, data on the mother’s diet and sun exposure, neonatal IGRA testing, research on the genes involved in calcitriol metabolism, and assessments of other vitamin levels and immunomodulators are only a few of the limitations of our study. Furthermore, we did not keep track of babies’ chronic cough, fever, or other TB clinical symptoms such weight loss. To develop a more thorough understanding of the connection between calcitriol levels and TLR2 expression in newborns, these approaches should be used in future studies. It is crucial to make sure that newborns receive the appropriate vaccinations and frequent growth monitoring, as was done in this study.
Future research will shed more light on the connection between calcitriol levels and TLR2 expression in newborns by examining other vitamin levels or immunomodulators, examining calcitriol metabolism genes, conducting interviews on food intake and sunlight exposure, testing newborns for IGRA, investigating calcitriol metabolism genes, and monitoring TB clinical signs. We found that even taking a 1000 IU supplement, several subjects still had calcitriol deficiencies. The right dosages for LTBI pregnant women to exert effective immune defenses may be determined by more research comparing higher calcitriol supplement dosages. Furthermore, since optimum calcitriol levels are necessary for the immune system, it is crucial to educate people about the proper levels of sunlight exposure for moms and babies.
Conclusions
Calcitriol levels in pregnant women may affect calcitriol levels and the immunological response of the neonate. It is critical for mothers and newborns to maintain adequate levels of calcitriol for a healthy immune system.
Data Sharing Statement
On reasonable request, the corresponding author will provide the datasets created during and/or analyzed during the current work.
Ethics Approval and Consent to Participate
We followed the recommendations in the Declaration of Helsinki when conducting our study. After receiving background information on the study, participants gave signed consent. If a participant disagreed with the study, they were not required to participate. On October 8th, 2021, the Universitas Sumatera Utara Ethical Committee accepted the study procedures (No. 1012/KEPK/USU/2021).
Consent for Publication
The Authors agree to publication in ImmunoTargets and Therapy.
Acknowledgments
The authors thank the hospitals, medic-paramedic teams, and participants in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Nikanfar S, Rashedi J, Poor BM, Asgharzadeh M. Vitamin D and tuberculosis patients. EC Pulmonol Respir Med. 2018;7(7):466–476.
2. Chakaya J, Khan M, Ntoumi F, Akillu E, Fatima R, Mwaba P. Global tuberculosis report 2020-reflection on the global TB burden, treatment, and prevention efforts. Int J Infect Dis. 2021;113(1):S7–S12. doi:10.1016/j.ijid.2021.02.107
3. Iskandar D, Suwantika AA, Pradipta IS, Postma MJ, van Boven M, Job FM. Clinical and economic burden of drug-susceptible tuberculosis in Indonesia: national trends 2017-19. Lancet Glob Health. 2022;11(1):e117–e125. doi:10.1016/S2214-109X(22)00455-7
4. Snow KJ, Bekker A, Huang GK, Graham SM. Tuberculosis in pregnant women and neonates: a meta-review of current evidence. Paedia Respir Rev Else. 2020;36:27–32. doi:10.1016/j.prrv.2020.02.001
5. United Nations Children’s Fund. Pediatric Tuberculosis with a Focus on Indonesia; 2022.
6. Macias CP, Monedero-Recuero I. TB or not TB? challenges in diagnosing and treating maternal and neonatal tuberculosis. Int J Tuberc Lung Dis. 2019;23(3):280–282. doi:10.5588/ijtld.18.0548
7. Aibana O, Huang C, Said A, Arnedo-Pena A, Becerra M, Bellido-Blasco JB. Vitamin D status and risk of incident tuberculosis disease: a nested case-control study, systematic review, and individual-participant data meta-analysis. PLoS Med. 2019;16(9):e1002907. doi:10.1371/journal.pmed.1002907
8. Amelin F, Yani FF, Machmud R. The role of vitamin D receptor gene FokI polymorphism, and cathelicidin in tuberculosis infection in children. Int J Appl Pharm. 2019;11(6):125–128. doi:10.22159/ijap.2019.v11s6.33575
9. Mathad JS, Bhosale R, Sangar V, Mave V, Gupte N, Kanade S. Pregnancy differentially impacts performance of latent tuberculosis diagnostics in high-burden setting. PLoS One. 2014;9(3):e92308. doi:10.1371/journal.pone.0092308
10. Naik S, Alexander M, Kumar P, Kulkarni V, Deshpande P, Yadana S. Systemic inflammation in pregnant women with latent tuberculosis infection. Front Immunol. 2021;11:587617. doi:10.3389/fimmu.2020.587617
11. Hollis BW, Wagner CL. New insights into the vitamin D requirements during pregnancy. Bone Res. 2017;5(1):17030. doi:10.1038/boneres.2017.30
12. Grant CC, Stewart AW, Scragg R, Milne T, Rowden J, Ekeroma A. Vitamin D during pregnancy and infancy and infant serum 25-hydroxyvitamin D concentration. Pediatrics. 2014;133(1):e 143–53. doi:10.1542/peds.2013-2602
13. Akhtar E, Mily A, Haq A, Al-Mahmud A, El-Arifeen S, Baqui AH. Prenatal high-dose vitamin D3 supplementation has balanced effects on cord blood Th1 and Th2 responses. Nutr J. 2016;15(1):75. doi:10.1186/s12937-016-0194-5
14. Hornsby E, Pfeffer PE, Laranjo N, Cruikshank W, Tuzova M, Litonjua AA. Vitamin D supplementation during pregnancy: effect on the neonatal immune system in a randomized controlled trial. J Allergy Clin Immunol. 2018;141(1):269–281. doi:10.1016/j.jaci.2017.02.039
15. Oktaria V, Danchin M, Triasih R, Soenarto Y, Bines JE, Ponsonby AL. The incidence of acute respiratory infection in Indonesia infants and association with vitamin D deficiency. PLoS One. 2021;16(3):e0248722. doi:10.1371/journal.pone.0248722
16. Odzemir AA, Caq Y. Neonatal vitamin D status and the risk of neonatal sepsis. Pak J Med Sci. 2019;35(2):420–425. doi:10.12669/pjms.35.2.342
17. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR anag the 2−ΔΔCT method. Methods. 2001;25(4):402–408. doi:10.1006/meth.2001.1262
18. Zhang P, Shao L, Ma J. Toll-like receptors 2 and 4 predict new onset atrial fibrillation in acute myocardial infarction patients. Int Heart J. 2018;59(1):64–70. doi:10.1536/ihj.17-084
19. Sari DK, Alrasyid D, Nurindrawaty H, Zulkifli L. Occurrence of vitamin D deficiency among women in North Sumatera, Indonesia. Mal J Nutr. 2014;20(1):63–70.
20. Owie E, Afolabi BB. Vitamin D deficiency in pregnant women and newborns in Lagos, Nigeria. J Obstetrics Gynaecol. 2018;38(5):616–621. doi:10.1080/01443615.2017.1396299
21. Oktaria V, Graham SM, Triasih R, Soenarto Y, Bines JE, Ponsonby A. The prevalence and determinants of vitamin D deficiency in Indonesian infants at birth and six months of age. PLoS One. 2020;15(10):e0239603. doi:10.1371/journal.pone.0239603
22. Yani FF, Lipoeto INI, Supriyatno B, Darwin E, Basir D. Vitamin D status in under five children with a history of close tuberculosis contact in Padang, West Sumatra. Asia Pac J Clin Nutr. 2017;26:68–72.
23. Gou X, Pan L, Tang F, Gao H, Xiao D. The association between vitamin D status and tuberculosis in children. Med J. 2018;97:35–41.
24. Patterson B, Smith D, Telford A, Tana A, Johnstone D, Davidson R. Vitamin D deficiency predicts latent TB reactivation independent of preventive therapy: a longitudinal study. Interna J Tuber Lung Dis. 2020;24(9):916–921. doi:10.5588/ijtld.19.0605
25. Deluca HF. History of the discovery of vitamin D and its active metabolites. Bonekey Rep. 2014;3:479. doi:10.1038/bonekey.2013.213
26. Wierzejska R, Jarosz M, Kleminska-Nowak M, Tomaszewska M, Sawicki W. Maternal and cord blood vitamin D status and anthropometric measurements in term newborns at birth. Front Endocrinol. 2018;9:9. doi:10.3389/fendo.2018.00009
27. Shrestha D, Budhathoki S, Pokhrel S, Sah AK, Shrestha RK, Raya GB. Prevalence of vitamin D deficiency in pregnant women and their babies in Bhaktapur, Nepal. BMC Nutr. 2019;5(1):31. doi:10.1186/s40795-019-0294-7
28. Basha MA, Majid HA, Razali N, Rashed AA, Muhammad H, Yahya A. Longitudinal vitamin D deficiency among Malaysian pregnant women and its correlation with neonatal serum 25-hydroxyvitamin D levels. Front Public Health. 2021;9:654292. doi:10.3389/fpubh.2021.654292
29. Larqué E, Morales E, Leis R, Blanco-Carnero JE. Maternal and foetal health implications of vitamin d status during pregnancy. Ann Nutr Metab. 2018;72(3):179–192. doi:10.1159/000487370
30. Rahman MM, Miah S, Tamanna S, Hosen MB, Akter T, Johra TH. Association of maternal vitamin D with neonatal vitamin D status and birth weight in urban population of Bangladesh: a cross sectional study. Acta Scien Paedia. 2020;3(12):19–26. doi:10.31080/ASPE.2020.03.0328
31. Ideraabdullah FY, Belenchia AM, Rosenfeld CS, Kullman SW, Knuth M, Mahapatra D. Maternal vitamin D deficiency and developmental origins of health and disease (DOHaD). J Endocrinol. 2019;241(2):65–80. doi:10.1530/JOE-18-0541
32. Gilani S, Janssen P. Maternal vitamin D levels during pregnancy and their effects on maternal-fetal outcomes: a systematic review. J Obstet Gynaecol Can. 2020;42(9):1129–1137. doi:10.1016/j.jogc.2019.09.013
33. Chung C, Silwal P, Kim I, Modlin RL, Jo EK. Vitamin D-cathelicidin axis: at the crossroads between protective immunity and pathological inflammation during infection. Immune Netw. 2020;20(2):e12. doi:10.4110/in.2020.20.e12
34. Majewski K, Kozlowska E, Zelechowska P, Brzezinska-Blaszczyk E. Serum concentrations of antimicrobial peptide cathelicidin LL-37 in patients with bacterial lung infections. Centr Eur J Immunol. 2018;43(4):453–457. doi:10.5114/ceji.2018.81355
35. Mouzaki A, Panagoulias I, Raptis G, Farri-Kostopoulou E. Cord blood leptin level of healthy neonates are associated with IFNγ production by cord blood T-cells. PLoS One. 2012;7(7):e40830. doi:10.1371/journal.pone.0040830
36. Sun X, Cao ZB, Zhang Y, Ishimi Y, Tabata I, Higuchi M. Association between serum 25-hydroxyvitamin D and inflammatory cytokine in healthy adults. Nutrients. 2014;6(1):221–230. doi:10.3390/nu6010221
37. Roth D, Shah R, Black R, Baqui A. Vitamin D status and acute lower respiratory infection in early childhood in Sylhet, Bangladesh. Acta Paediatr Int J Paediatr. 2010;99(3):389–393. doi:10.1111/j.1651-2227.2009.01594.x
38. Khoo A, Chai LY, Koenen HJ, Oosting M, Steinmeyer A, Zuegel U. Vitamin D3 down-regulates proinflammatory cytokine response to mycobacterium tuberculosis through pattern recognition receptors while inducing protective cathelicidin. Elsevier. 2011;55(2):294–300.
39. Acen EL, Kateete DP, Worodria W, et al. Evaluation of circulating serum cathelicidin levels as a potential biomarker to discriminate between active and latent tuberculosis in Uganda. PLoS One. 2022;17(8):e0272788. doi:10.1371/journal.pone.0272788
40. Huaman MA, Deepe GS, Fichtenbaum CJ. Elevated circulating concentrations of interferon-gamma in latent tuberculosis infection. Phatog Immun. 2016;1(2):291–300. doi:10.20411/pai.v1i2.149
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
