Back to Journals » Journal of Pain Research » Volume 16
Comparison of Unilateral and Bilateral Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures
Authors Qiao Y , Wang X, Liu Y, Hu J, Yuan FH, Zhao ZG
Received 13 October 2022
Accepted for publication 24 May 2023
Published 30 May 2023 Volume 2023:16 Pages 1813—1823
DOI https://doi.org/10.2147/JPR.S393333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Houman Danesh
Yu Qiao,1,* Xin Wang,2,* Yi Liu,2 Jun Hu,2 Fa-Hu Yuan,1 Zhi-Gang Zhao2
1School of Medicine, Jianghan University, Wuhan, 430056, People’s Republic of China; 2Department of Spine Surgery, Wuhan Fourth Hospital, Wuhan, 430035, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhi-Gang Zhao, Department of Spine Surgery, Wuhan Fourth Hospital, Gutian 3rd Road, Jiefang Avenue, Wuhan, Hubei, 430035, People’s Republic of China, Tel +86 2768831614, Email [email protected] Fa-Hu Yuan, School of Medicine, Jianghan University, No. 8, Sanjiaohu Road, Wuhan Economic and Technological Development Zone, Wuhan, Hubei, 430056, People’s Republic of China, Tel +86 2784225149, Email [email protected]
Objective: To investigate the clinical efficacy of percutaneous kyphoplasty (PKP) with a unilateral versus bilateral approach in the treatment of osteoporotic vertebral compression fractures (OVCFs).
Methods: We retrospectively analyzed a total of 147 patients (unilateral group: 79, bilateral group: 68) with OVCFs treated with PKP at the Department of Spine Surgery, Wuhan Fourth Hospital between August 2020 and January 2022. Patients’ personal information, operation time, bone cement injection volume, as well as pre- and post-operative visual analogue scale (VAS), Oswestry disability index (ODI), anterior vertebral body height and Cobb angle were recorded.
Results: All 147 patients were successfully treated with PKP and were followed up for at least 6 months. Our results showed that the operative time was significantly shorter in the unilateral group (41.60± 5.64) minutes than in the bilateral group (66.53± 9.40) minutes, and the volume of bone cement injected was also significantly less in the unilateral group (5.27± 0.73) mL than in the bilateral group (6.87± 0.93) mL (P< 0.01). The VAS score, ODI index, vertebral height and Cobb angle at postoperative follow-up were significantly improved in both groups compared to the preoperative period (P< 0.01); However, the difference between the two groups was not statistically significant (P> 0.05). Repeat thoracic and lumbar radiographs showed cement leakage in seven cases (8.86%) in the unilateral group and five cases (7.35%) in the bilateral group, but all were asymptomatic and required no further management. During our entire follow-up period, there were five adjacent vertebral fractures in the unilateral group (6.33%) and four in the bilateral group (5.88%).
Conclusion: There was no significant difference between the two groups in terms of improvement in VAS score, ODI index, restoration of vertebral body height, and posterior convexity deformity, but unilateral puncture had the advantage of shorter operative time and less cement injection.
Keywords: osteoporotic vertebral compression fracture, percutaneous vertebroplasty, unilateral arch root approach, bilateral arch root approach, clinical outcome
Introduction
Osteoporosis is a metabolic bone disease characterized by bone loss and changes in bone microarchitecture. The prevalence of postmenopausal osteoporosis ranges from 40–60% in women aged 70 years and 60–75% in women aged 80 years and older.1 It was found that the prevalence of OP in Chinese elderly people aged 60–69 years was 32.2%, 41.9% in those aged 70–79 years and 51.8% in those aged ≥80 years; the prevalence of OP in Chinese elderly people was 37.7%, and it gradually increased with age.2 Osteoporotic vertebral compression fractures (OVCFs) due to osteoporosis are the most common type of osteoporotic fracture,3 with fractures of the thoracolumbar segment being the most common.4 OVCFs commonly occur in women over the age of 60 and can lead to debilitating pain and spinal deformities, as well as a significant reduction in quality and quantity of life and a significant financial burden.5 OVCFs are also emerging as a growing public health problem with significant socio-economic implications due to the ageing population and the severe morbidity associated with these fractures. According to The National Osteoporosis Foundation (USA), approximately 10 million people in the USA have osteoporosis and approximately 750,000 OVCFs occur each year, and the incidence of osteoporosis in China is not very different from that in Western countries.6,7 Although 2/3 of patients will gradually improve with conservative treatment,3 1/3 of fracture patients will develop chronic pain. In addition, vertebral compression fractures can also lead to height loss, kyphosis, reduced lung function, mobility, and balance impairment. Treatment of patients with OVCFs should address pain, restore vertebral height and improve kyphosis, which is of paramount importance.6
Traditional incisional repositioning internal fixation surgery is invasive with high intraoperative bleeding. However, due to osteoporosis, the grip of the pedicle screw is insufficient, which can easily cause instability of fixation and ultimately lead to treatment failure.1 Therefore, internal fixation is generally not recommended for elderly patients without symptoms of neurological compression. Rapid and effective treatment of OVCFs has therefore become clinically critical. After the first vertebroplasty was performed by Lapras et al8 in the 1980s, this opened up the minimally invasive era of the spine, developing into the first successful balloon-expandable vertebroplasty performed by Lieberman et al9 in 2001. Since then, vertebroplasty (PVP) and PKP have become by far the more commonly used minimally invasive procedures, offering improved quality of life in addition to rapid and lasting pain relief.3 In addition to the obvious advantages of PKP, such as good safety, definitive treatment results, minimal invasiveness and rapid and effective pain relief, it can also promote early mobility, reduce complications such as venous thrombosis, crushing pneumonia and pressure sores caused by bed rest, and can correct kyphosis.10
A variety of puncture approaches exist for PKP, the most common of which is the bilateral arch root approach. Previous studies have found that after artificial machine compression of the spine (T3-L5) in fresh human cadavers, vertebral body kyphoplasty was performed using a unilateral or bilateral arch root approach. The final results showed that the unilateral arch root approach to vertebral kyphoplasty was comparable to the bilateral arch root approach in terms of strength, stiffness and height restoration with similar biomechanical results.11,12 Currently, there is still clinical controversy as to whether these two surgical access methods have the same surgical outcome. This retrospective study aimed to analyze the clinical outcomes of 147 patients with OVCFs treated with PKP in our department between August 2020 and January 2022, about unilateral versus bilateral punctures.
Materials and Methods
This study was conducted in compliance with the Declaration of Helsinki and approved by the Wuhan Ethics Committee (KY2022-081-01). As the study was retrospective in design, informed consent from patients was not required. All data were collected and analyzed anonymously. The flow of this study is shown in Figure 1.
 |
Figure 1 Flow chart table for this study. |
Patient Population
In this retrospective study, 147 patients with single-segment OVCFs treated with PKP at the Department of Spine Surgery, Wuhan Fourth Hospital, Wuhan, China, between August 2020 and January 2022 were analyzed. Among them, 116 (78.91%) were female and 31 (21.09%) were male, with a mean age of 72 years (range 61–89 years). Unilateral PKP in 79 cases, 61 women and 18 men, mean 70.73 years (61–87 years). There were 68 cases of bilateral PKP, 55 women and 13 men, with a mean of 73.2 years (64–89 years).Fracture sites: T1014, T1119, T1225, L131, L228, L319, and L411. There was no statistically significant difference between the two groups in terms of gender, age, and fracture site (P > 0.05).
Inclusion and Exclusion Criteria
Inclusion criteria: (1) patients aged ≥ 60 years; (2) confirmed diagnosis of vertebral compression fracture of < 2 weeks duration; (3) T < −2.5 on BMD; (4) MRI shows compression fractures of the thoracic and lumbar spine with bone marrow oedema (injured vertebra with low signal on T1-weighted images and high signal on T2-weighted images).
Exclusion criteria: (1) secondary osteoporosis (corticosteroid, endocrine disorders, and inflammatory processes); (2) patients who cannot give informed consent or have difficulty with postoperative follow-up; (3) uncorrected coagulation disorders; (4) cachexia; (5) painless OVCFs; (6) secondary malignancy of the spine; (7) fracture resulting in neurological symptoms.
Surgical Techniques
Both groups were performed by two senior surgeons (Zhi-gang Zhao and Xin Wang) from the same treatment group in our department. All PKP operations were performed in the operating room with the ability to perform immediate decompression surgery. (1) Unilateral PKP group: The patient is placed in a prone position with 2 lateral support pads placed under the chest and pelvis to reduce pressure on the abdomen. The C-arm was adjusted so that there was no bilateral shadowing of the fractured vertebrae and the shape of the vertebral arch was symmetrical and at the same distance from the spinous process. The puncture needle is inserted on the side of the patient where the compression is more severe or where the patient’s pain is more pronounced. If there is no significant difference in pain between the two sides of the patient and the degree of compression is similar on both sides, the side that is easier for the surgeon to operate on is chosen. The puncture point is chosen to be lateral to the arch on the injured side of the vertebra (10 o’clock on the left and 2 o’clock on the right) and orthogonal to the superior border of the “cat’s eye sign” of the arch projection. The puncture needle is inserted through the puncture point at an angle of 10°-20° of decubitus. When the tip of the needle is located in the anterior and middle 1/3 of the vertebral body in the lateral image and close to or slightly above the midline of the injured vertebra in the orthodromic image, the inner core is withdrawn and the guide needle is placed. The working cannula is placed in sequence, step by step, to establish the working channel and balloon expansion system. The injection is stopped when the vertebral body is satisfactorily repositioned and/or the balloon is expanded to the upper and lower endplates of the vertebral body, and the balloon is removed. The cement is injected under fluoroscopy along the working channel with the front end of the cement injector located in the anterior 1/3 of the vertebral body at the start of the injection, with a fluoroscopic front and side view for every 0.5–0.75 mL of cement injected. If the bone cement leaks, adjust the anterior and posterior position of the cement injector in the vertebral body, generally backing off the cement injector by 1 cm and then continuing the injection. The injection is stopped when the bone cement reaches the posterior third of the vertebral body. After the bone cement has been adequately filled, the puncture needle is slowly withdrawn and the wound is sutured. (Figure 2A) (2) Bilateral PKP group: Bilateral arch puncture is performed at the same time, and the rest of the procedure remains the same as unilateral (Figure 2B).
 |
Figure 2 Schematic diagram of two surgical punctures. (A) unilateral puncture; (B) bilateral puncture. |
Postoperative Management
Routine bed rest for 4–8h after surgery. All were taken out of bed on the second day after surgery with a lumbar back brace. Salmon calcitonin and vitamin D were used postoperatively to treat osteoporosis. X-ray films were routinely performed after surgery. And Follow-up were carried out 1 day, 1 month, and 6 months after surgery (Record the patient’s VAS score, ODI score and perform a spinal X-ray).
Outcome Measurements
The duration of surgery and the amount of bone cement injected were routinely recorded for both groups. Two questionnaires, the visual analogue scale (VAS score) and the Oswestry Disability Index (ODI) were used to assess pain and function at different times before and after surgery. The patients’ VAS and ODI were recorded preoperatively, 1 day postoperatively, and 6 months postoperatively, respectively. For reasons such as the age and lifestyle of the patients, the options related to sexuality in the ODI score were excluded from this study. The ODI questionnaire, therefore, consists of a total of 9 items out of 45. ODI score is calculated as follows: Total score = (score/45) x 100%.
Patients were also routinely X-rayed preoperatively, 1d postoperatively and at each follow-up visit to record changes in anterior vertebral body height (AH) and changes in Cobb’s angle. All data were measured independently by two senior spine surgeons (Jun Hu and Yi Liu) who were not involved in the surgery, and the mean of the two surgeons’ measurements was ultimately included in the analysis.
Statistical Analysis
SPSS 26.0 software was used for statistical processing. The measurement data conforming to normal distribution were expressed as ( ). The t-test of two independent samples was used for comparison between two groups, repeated measures ANOVA was used for comparison between different time points within groups, and LSD-t-test was used for multiple comparisons. Comparisons of the count data between the two groups were made using the x2 test. P < 0.05 was considered a statistically significant difference.
). The t-test of two independent samples was used for comparison between two groups, repeated measures ANOVA was used for comparison between different time points within groups, and LSD-t-test was used for multiple comparisons. Comparisons of the count data between the two groups were made using the x2 test. P < 0.05 was considered a statistically significant difference.
Results
All 147 patients underwent successful surgery with good postoperative outcomes and all were given clinical follow-up. No deaths were reported in this study, and all patients had a one-stage preoperative incision with no complications such as venous thrombosis, pressure sores, or crushing pneumonia. Patients in both groups were followed up for at least 6 months (mean follow-up 6.8 months, range 6–8 months). There were no significant differences between the two groups in terms of age, gender, and fracture site (P>0.05), indicating that the two groups were comparable (Table 1).
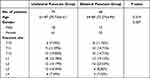 |
Table 1 Characteristics of the Study Population |
Intraoperative Measurements
As shown in Table 2, the operative time in the unilateral puncture group was (41.60 ± 5.64 min) significantly lower than that in the bilateral group (66.53 ± 9.40 min), which was statistically significant (P<0.01); the volume of bone cement injected was (5.27 ± 0.73 mL) and (6.87 ± 0.93 mL) in the unilateral and bilateral puncture groups respectively, with significant differences between the two groups (P<0.01).
 |
Table 2 Intraoperative Comparison of Unilateral and Bilateral Punctures |
Clinical Results
As shown in Figure 3, patients’ postoperative pain and ODI indices were significantly reduced in both groups after surgical treatment with PKP. After unilateral puncture PKP treatment, patients’ VAS scores decreased from 7.13 ± 1.06 preoperatively to 3.27 ± 0.80 postoperatively and to 1.27 ± 0.46 at 6 months postoperatively (P<0.01). Similarly, VAS scores for patients in the bilateral puncture group decreased from 7.07 ± 0.88 preoperatively to 3.67 ± 0.82 postoperatively and eventually became 1.13 ± 0.52 at 6-month postoperative follow-up (P<0.01). No statistical difference was found between the two groups of patients for VAS scores at all follow-ups from preoperative to postoperative (P>0.05). Similar results were found in the ODI index, which decreased from 76.87 ± 4.02 preoperatively to 21.07±1.58 at 6 months postoperatively in the unilateral puncture group (P<0.01) and from 77.47 ± 5.08 to 20.27 ± 1.87 in the double puncture group (P<0.01). However, the ODI indices between the two groups were not statistically significant at 1 day postoperatively, 1 month postoperatively, and 6 months postoperatively (P>0.05) (Table 3).
 |
Table 3 Comparison of VAS Scores and ODI in Both Groups Before and After Surgery |
 |
Figure 3 Mean preoperative and postoperative VAS scores, ODI for unilateral and bilateral groups. |
Radiological Results
All patients underwent precise unilateral and bilateral PKP under intraoperative C-arm guidance. Good surgical results were obtained with both surgical puncture routes and the bone cement was homogeneous in each case, a typical case of the procedure is shown in Figure 4. In the unilateral puncture group, the height of the anterior border of the injured vertebrae recovered from (16.45± 2.34) mm preoperatively to (20.59±2.25) mm at 6 months postoperatively, as measured by imaging indices (P<0.01). Similarly, in the bilateral puncture group, there was a recovery from (16.87±1.60) mm preoperatively to (20.89±1.60) mm postoperatively (P<0.01). The Cobb Angle was significantly improved in both groups. The preoperative Cobb Angle was (23.73±2.57) ° in the unilateral group and (24.11±1.81) ° in the bilateral group. At the end of the final follow-up, the Cobb Angle was (12.61±1.72) ° and (12.90±1.37) °, with statistical significance (P<0.01). However, there was no statistically significant comparison between the two groups (P>0.05), Table 4.
 |
Table 4 Comparison of Unilateral and Bilateral Puncture Radiographic Data |
 |
Figure 4 Intraoperative schematic diagram of a typical case of unilateral and bilateral. (a–d) are unilateral punctures; (e–h) are bilateral punctures. |
Complications
No adverse intraoperative time such as cardiovascular or cerebrovascular occurred in any of the 147 patients. Post-operative X-ray showed that 12 cases of bone cement leakage occurred, including a total of 7 cases (8.86%) in the unilateral group and 5 cases (7.35%) in the bilateral group, none of which showed clinical symptoms. There was no statistically significant difference between the two groups in terms of bone cement leakage (P>0.05). In the unilateral group, there was leakage to the anterior border of the vertebral body in 3 cases and to the intervertebral disc in 4 cases. In the bilateral group, there were 2 cases of leakage to the anterior border of the vertebral body, 1 case of leakage to the intervertebral disc and 2 cases of leakage to the extra vertebral vein. A total of 18 cases (12.24%) experienced post-operative pain due to puncture, including 3 cases in the unilateral group and 15 cases in the bilateral group (P<0.05), all of which disappeared after 1 week of heat and ultrashort wave therapy. Throughout the follow-up period, a total of nine cases of adjacent vertebral fractures occurred, five in the unilateral group (6.33%) and four in the bilateral group (5.88%), with no statistical significance in terms of recurrent fractures in either group (P>0.05). All nine patients were readmitted for PKP (readmitted patients were not included in this study).
Discussion
PKP can provide rapid pain relief and restore stability to the vertebral body.13 PKP can achieve fracture repositioning through balloon expansion, and the injection of bone cement can reduce the sensitivity of nerve endings in the vertebral body, and the heat released can also cause necrosis of nociceptive nerve endings, thus achieving pain relief, etc.14 At the same time, the stagnant blood in the injured vertebrae can be drained through the working channel, reducing the pressure in the injured vertebrae and thus reducing pain.15
There are two types of PKP: unilateral puncture and bilateral puncture. The choice of unilateral or bilateral puncture is still controversial as to how to more effectively achieve clinical outcomes, restore vertebral height, improve pain, and correct kyphotic deformity. This study aimed to retrospectively analyze the clinical outcomes of unilateral and bilateral approaches performed in our department for the treatment of OVCFs and to find that unilateral puncture and bilateral puncture resulted in the same clinical outcomes. When John et al studied the biomechanics of human cadavers, The average strength (1.40±0.38 kN) and average stiffness (0.4387±0.2095 kN/mm) of the body in the bilateral approach group showed no statistical difference from that in the unilateral approach group (1.57±0.55 kN) and average stiffness (0.6880±0.3179 kN/mm) (P>0.05). At the same time, there was no significant difference in vertebral height recovery (P>0.05).12
The Advantages of Unilateral PKP
In this study, whether unilateral PKP was used to treat OVCFs or bilateral punctures, good clinical results were achieved at 1 day and 1 month postoperatively, with significant improvements in postoperative VAS scores, ODI indices, anterior vertebral body margin height recovery and Cobb angle compared to preoperative; However, postoperative follow-up of all data revealed no statistical difference between the two groups (P>0.05), indicating that unilateral The unilateral puncture approach could achieve the same clinical results as a bilateral puncture. However, unilateral PKP has a slight advantage in terms of operative time, and reducing operative time is important in older patients with more underlying diseases. The same study by Zhang et al also confirmed that unilateral PKP can achieve the same results bilaterally and that unilateral puncture has the advantage of shorter operative time and less radiation dose.16 Our study found that the unilateral group had essentially only 2/3 of the operative time of the bilateral group, significantly reducing the time spent in the prone position and the length of intraoperative pain stimulation, which may help to reduce the probability of intraoperative cardiovascular risk in patients.17
At the same time, the amount of bone cement injected was significantly lower in the unilateral group than in the bilateral group (P <0.05). However, the two groups were identical in terms of postoperative vertebral height restoration, pain relief and correction of the kyphosis, indicating that there was no correlation between the clinical outcome of PKP for OVCFs and the amount of bone cement used, which is consistent with the findings of Berlemann et al.18 This also suggests that better clinical outcomes can be achieved as long as the bone cement possesses better dispersion in the injured spine. There is some controversy regarding the amount of bone cement injected; it has been suggested that the more adequate the dispersion of the bone cement, the better the pain relief; however, a higher amount of bone cement injected is more likely to trigger the risk of adjacent vertebral fracture and the probability of bone cement leakage.19–21 Furthermore, bone cement leakage is a common postoperative complication of PKP, which may lead to nerve compression, and stimuli such as bone cement toxicity or allergy can cause symptoms such as decreased blood pressure and dyspnoea.20,22 And, without compromising clinical outcomes, unilateral puncture requires only one set of puncture equipment, which can save patients’ hospitalization costs.23
Indications for Unilateral PKP versus Bilateral PKP
Unilateral PKP for OVCFs has the advantages of short operative time and low economic cost. Unilateral PKP is therefore recommended for older patients, those with more underlying disease, those who cannot tolerate prolonged prone positioning and those whose families are financially disadvantaged; if preoperative CT reveals a high probability of cement leakage on one side of the vertebral body, unilateral PKP from the other side is recommended; or if the fracture is asymmetrically compressed, unilateral PKP from the more severely compressed side is recommended.
Bilateral PKP is expected to be gradually replaced by unilateral PKP in the future. We believe that for the less experienced spine surgeon, unilateral PKP can be performed bilaterally if satisfactory cement dispersion is not achieved.
Points to Note During the Unilateral PKP Procedure
(1) Pre-operative CT measurement of the puncture angle and the design of the needle route can provide the best guidance for intraoperative manipulation. (2) Unilateral puncture requires a greater angle of abduction compared to bilateral puncture to get closer to the vertebral body midline. (3) Avoid damage to the joint capsule.
Surgical Complications and Their Countermeasures
The main complications of PKP surgery are bone cement leakage and fracture of the adjacent vertebral body. In this study, there were 12 cases of bone cement leakage (unilateral group: 7 cases; bilateral group: 5 cases, P>0.05), with no clinical symptoms in either group. Our experience suggests that the following measures can be taken to prevent bone cement leakage: (1) Preoperative assessment of the site and extent of rupture of the posterior wall of the injured vertebral body by CT and 3D reconstruction techniques; (2) Initially, it is recommended to inject bone cement during the extraction phase and continue to push bone cement after the initial injection has set; (3) The bone cement injection site should not be close to the posterior 1/3 of the vertebral body as far as possible to avoid the intravertebral venous system; (4) Intraoperative C-arm close monitoring of the injected bone cement. (5) Filling with a gelatin sponge before the bone cement injection can seal part of the cortical bone defect of the vertebral body and reduce the leakage of bone cement.24
Previous literature has reported vertebral re-fracture rates of 2.9–27.6% after vertebroplasty.25,26 Low bone mineral density is often considered to be the most important risk factor for recurrent fractures. Therefore, in recent years, orthopaedic surgeons have placed increasing emphasis on anti-osteoporosis treatment after OVCFs.27 Bawa et al28 conducted a clinical trial with a large sample and showed that anti-osteoporosis treatment after fracture reduced the risk of re-fracture by 40% compared to patients who did not receive this treatment. In this study, only nine patients in both groups had a re-fracture at the 6-month follow-up (unilateral group: 5; bilateral group: 4, P> 0.05). This may be related to our increased emphasis on postoperative anti-osteoporotic treatment and may also be related to the shorter follow-up period.
Limitations
There are still limitations in this study, as we only analyzed PKP treatment for single-segment OVCFs and the postoperative follow-up was only 6 months, with limitations such as insufficient follow-up time, insufficient sample size, single clinical characteristics and non-multicenter randomized controls. In the future, we will attempt to investigate the effect of multi-segmental OVCFs, the amount of cement injected into the adjacent vertebrae, and the statistical analysis in combination with multicenter randomized controls.
Conclusion
In summary, we retrospectively analyzed that unilateral and bilateral PKP for OVCFs are equally efficacious and safe. The 6-month follow-up also showed that unilateral puncture did not increase post-operative complications in patients. At the same time, unilateral PKP has the advantage of shorter operative time, less cement injection and lower financial cost than a bilateral puncture. In elderly patients with more underlying disease and who cannot tolerate prolonged prone surgery, the shorter procedure time and less painful stimulation can help to reduce intraoperative cardiovascular risk. Also, injecting less bone cement may reduce the risk of leakage to a certain extent. Unilateral PKP has proven to be clinically useful and has good economics, and these advantages will be further validated in future multi-centre clinical studies. In the future, unilateral PKP puncture is expected to become a mainstream procedure for the treatment of OVCFs.
Data Sharing Statement
All patient clinical data were obtained from the Department of Spine Surgery, Wuhan Fourth Hospital, Wuhan, China, and no data copyright issues were involved.
Ethical Approval and Consent to Participate
The study protocol was approved by the Ethics Committee of Wuhan Fourth Hospital. Informed consent was obtained from all patients before surgery after they were fully informed of the treatment procedures.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Yu Qiao and Xin Wang are co-first authors for this study. The authors declared no conflicts of interest in this work.
References
1. Tang J, Guo WC, Hu JF, Yu L. Unilateral and bilateral percutaneous kyphoplasty for thoracolumbar osteoporotic compression fractures. J Coll Physicians Surg Pak. 2019;29(10):946–950. doi:10.29271/jcpsp.2019.10.946
2. Wang Y, Tao Y, Hyman ME, Li J, Chen Y. Osteoporosis in China. Osteoporos Int. 2009;20(10):1651–1662. doi:10.1007/s00198-009-0925-y
3. Li HM, Zhang RJ, Gao H, et al. New vertebral fractures after osteoporotic vertebral compression fracture between balloon kyphoplasty and nonsurgical treatment PRISMA. Medicine. 2018;97(40):e12666. doi:10.1097/MD.0000000000012666
4. Yeni YN, Dix MR, Xiao A, Oravec DJ. Uniaxial compressive properties of human lumbar 1 vertebrae loaded beyond compaction and their relationship to cortical and cancellous microstructure, size and density properties. J Mech Behav Biomed Mater. 2022;133:105334. doi:10.1016/j.jmbbm.2022.105334
5. Carey JJ, Chih-Hsing Wu P, Bergin D. Risk assessment tools for osteoporosis and fractures in 2022. Best Pract Res Clin Rheumatol. 2022;36(3):101775. doi:10.1016/j.berh.2022.101775
6. Chen C, Wei H, Zhang W, et al. Comparative study of kyphoplasty for chronic painful osteoporotic vertebral compression fractures via unipedicular versus bipedicular approach. J Spinal Disord Tech. 2011;24(7):E62–E65. doi:10.1097/BSD.0b013e318228f470
7. Wang L, Yu W, Yin X, et al. Prevalence of osteoporosis and fracture in china: the china osteoporosis prevalence study. JAMA Netw Open. 2021;4(8):e2121106. doi:10.1001/jamanetworkopen.2021.21106
8. Lapras C, Mottolese C, Deruty R, Lapras C, Remond J, Duquesnel J. Injection percutanée de méthyl-métacrylate dans le traitement de l’ostéoporose et ostéolyse vertébrale grave (technique de P. Galibert) [Percutaneous injection of methyl-methacrylate in osteoporosis and severe vertebral osteolysis (Galibert’s technic)]. Ann Chir. 1989;43(5):371–376.
9. Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26(14):1631–1638. doi:10.1097/00007632-200107150-00026
10. Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364–376. doi:10.1016/S0140-6736(18)32112-3
11. Tohmeh AG, Mathis JM, Fenton DC, Levine AM, Belkoff SM. Biomechanical efficacy of unipedicular versus bipedicular vertebroplasty for the management of osteoporotic compression fractures. Spine. 1999;24(17):1772–1776. doi:10.1097/00007632-199909010-00004
12. Steinmann J, Tingey CT, Cruz G, Dai Q. Biomechanical comparison of unipedicular versus bipedicular kyphoplasty. Spine. 2005;30(2):201–205. doi:10.1097/01.brs.0000150831.46856.87
13. Taylor RS, Fritzell P, Taylor RJ. Balloon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J. 2007;16(8):1085–1100. doi:10.1007/s00586-007-0308-z
14. Lu Q, Gao S, Zhou M. The effect of bone cement on the curative effect of percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. Ann Palliat Med. 2021;10(10):11013–11023. doi:10.21037/apm-21-2767
15. Feng L, Feng C, Chen J, Wu Y, Shen JM. The risk factors of vertebral refracture after kyphoplasty in patients with osteoporotic vertebral compression fractures: a study protocol for a prospective cohort study. BMC Musculoskelet Disord. 2018;19(1):195. doi:10.1186/s12891-018-2123-6
16. Zhang F, Zhao QM, Ni XH, et al. Comparison of unilateral and bilateral puncture percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Neurosciences. 2021;26(3):236–241. doi:10.17712/nsj.2021.3.20200138
17. Tran I, Gerckens U, Remig J, Zintl G, Textor J. First report of a life-threatening cardiac complication after percutaneous balloon kyphoplasty. Spine. 2013;38(5):E316–E318. doi:10.1097/BRS.0b013e318281507a
18. Berlemann U, Franz T, Orler R, Heini PF. Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J. 2004;13(6):496–501. doi:10.1007/s00586-004-0691-7
19. Cheng X, Long HQ, Xu JH, Huang YL, Li FB. Comparison of unilateral versus bilateral percutaneous kyphoplasty for the treatment of patients with osteoporosis vertebral compression fracture (OVCF): a systematic review and meta-analysis. Eur Spine J. 2016;25(11):3439–3449. doi:10.1007/s00586-016-4395-6
20. He X, Li H, Meng Y, et al. Percutaneous kyphoplasty evaluated by cement volume and distribution: an analysis of clinical data. Pain Physician. 2016;19(7):495–506.
21. Ren H, Feng T, Cao J, et al. A retrospective study to evaluate the effect of dynamic fracture mobility on cement leakage in percutaneous vertebroplasty and percutaneous kyphoplasty in 286 patients with osteoporotic vertebral compression fractures. Med Sci Monit. 2022;28:e935080. doi:10.12659/MSM.935080
22. Zhang K, She J, Zhu Y, Wang W, Li E, Ma D. Risk factors of postoperative bone cement leakage on osteoporotic vertebral compression fracture: a retrospective study. J Orthop Surg Res. 2021;16(1):183. doi:10.1186/s13018-021-02337-1
23. Rebolledo BJ, Gladnick BP, Unnanuntana A, Nguyen JT, Kepler CK, Lane JM. Comparison of unipedicular and bipedicular balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a prospective randomised study. Bone Joint J. 2013;95-B(3):401–406. doi:10.1302/0301-620X.95B3.29819
24. Bhatia C, Barzilay Y, Krishna M, Friesem T, Pollock R. Cement leakage in percutaneous vertebroplasty: effect of preinjection gelfoam embolization. Spine. 2006;31(8):915–919. doi:10.1097/01.brs.0000209307.03930.38
25. Heo DH, Chin DK, Yoon YS, Kuh SU. Recollapse of previous vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int. 2009;20(3):473–480. doi:10.1007/s00198-008-0682-3
26. Yu WB, Jiang XB, Liang D, Xu WX, Ye LQ, Wang J. Risk factors and score for recollapse of the augmented vertebrae after percutaneous vertebroplasty in osteoporotic vertebral compression fractures. Osteoporos Int. 2019;30(2):423–430. doi:10.1007/s00198-018-4754-8
27. Lee BG, Choi JH, Kim DY, Choi WR, Lee SG, Kang CN. Risk factors for newly developed osteoporotic vertebral compression fractures following treatment for osteoporotic vertebral compression fractures. Spine J. 2019;19(2):301–305. doi:10.1016/j.spinee.2018.06.347
28. Bawa HS, Weick J, Dirschl DR. Anti-osteoporotic therapy after fragility fracture lowers rate of subsequent fracture: analysis of a large population sample. J Bone Joint Surg Am. 2015;97(19):1555–1562. doi:10.2106/JBJS.N.01275
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
