Back to Journals » Journal of Pain Research » Volume 14
Comparison of the Oblique Interlaminar and Transforaminal Lumbar Epidural Steroid Injections for Treatment of Low Back and Lumbosacral Radicular Pain
Authors Choi EJ , Park SJ, Yoo YM, Yoon JU, Shin SW, Byeon GJ
Received 20 November 2020
Accepted for publication 27 January 2021
Published 15 February 2021 Volume 2021:14 Pages 407—414
DOI https://doi.org/10.2147/JPR.S293166
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Eun-Ji Choi,1,2 Soon Ji Park,1 Yeong-Min Yoo,1 Ji-Uk Yoon,1,2 Sang-Wook Shin,1,2 Gyeong-Jo Byeon1,2
1Department of Anesthesia and Pain Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Republic of Korea; 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Republic of Korea
Correspondence: Gyeong-Jo Byeon
Department of Anesthesia and Pain Medicine, Pusan National University Yangsan Hospital, Geumoro 20, Yangsan, Gyeongnam, 50612, Republic of Korea
Tel +82-55-360-2129
Fax +82-55-360-2149
Email [email protected]
Background: Transforaminal epidural steroid injections (TF-ESIs) effectively deliver small amounts of drugs to inflamed sites via the ventral epidural space. However, there is a high risk of nerve damage as the needle narrowly approaches the spinal nerve. Therefore, we devised an oblique interlaminar (OIL) approach as an alternative method. We compared the efficacy of fluoroscopic-guided OIL-ESIs with that of TF-ESIs in the management of lower back and unilateral lumbosacral radicular pain.
Materials and Methods: Sixty-six patients were randomized to receive a fluoroscopic-guided ESI either through the OIL (n = 33, group OIL) or TF (n = 33, group TF) approach. They were evaluated for effective pain relief using the visual analogue scale (VAS) and for functional improvement using the Oswestry Disability Index (ODI) and Roland Morris Disability Questionnaire (RMDQ). Other outcome measures were the presence of ventral and contralateral spread of contrast, patients’ satisfaction, and adverse events.
Results: There were no significant differences between the groups in the VAS, ODI, and RMDQ scores during the 12-week period. The differences in the ODI and RMDQ scores before and after the treatment were higher in group TF than in group OIL. The contralateral spread of contrast was higher in group OIL than in group TF. There were no significant differences in the other outcomes between the groups.
Conclusion: ESIs delivered through the OIL approach are equally effective in pain relief and functional improvement as those delivered via the TF approach in the management of low back and unilateral lumbosacral radicular pain.
Keywords: epidural analgesia, fluoroscopy, low back pain, radicular pain, steroid injection
Introduction
Epidural steroid injections (ESIs), commonly used for the treatment of low back and lumbosacral radicular pain, can be performed via interlaminar, or transforaminal (TF) approaches. The interlaminar approach has been used widely but is reported to have limited efficacy.1,2 This is probably because the drug is delivered mainly to the dorsal epidural space, whereas the ventral epidural spread is limited.3,4 The TF approach offers several advantages over the interlaminar approach, including a reduced risk of dural puncture, injection of the drug closer to the nerve root where the lesion is located, delivery of the drug to the ventral epidural space, and lesser amount of drugs required.3 However, it has been reported that several adverse effects follow the procedure. Spinal cord injury, permanent paraplegia, segmental spinal myoclonus, and increased incidence of intradiscal injection of the drug are some of them.5–7 For this reason, there is an urgent need for a technique that can offer effective drug delivery to the ventral epidural space.
Several studies have showed that an ESI delivered through the parasagittal interlaminar approach is equivalent in achieving effective pain relief and functional improvement to that delivered through the TF approach for the management of lower back and lumbosacral radicular pain. Ventral epidural spread of contrast was reported when a lateral parasagittal interlaminar approach was used at the ventrolateral side of the nerve root.8,9 Based on this approach and with reference to previous studies on various approaches,10,11 we devised a fluoroscopic-guided, alternative, oblique interlaminar (OIL) approach (Figure 1) and applied it to a patient with a difficult TF approach due to the presence of rods, pedicle screws, and bone harvests for posterior lumbar interbody fusion.12 Since our first case report, we have performed ESIs using the OIL approach instead of the TF approach in patients who visited our clinic with low back and unilateral lumbosacral radicular pain. The OIL approach showed a ventral epidural spread of the contrast and achieved effective pain relief and functional improvement in the management of low back and unilateral lumbosacral radicular pain. We speculated that the OIL approach could substitute the TF approach as the ventral epidural spread of the contrast is better than the conventional interlaminar approach. To the best of our knowledge, no previous studies have compared the OIL and the TF approaches.
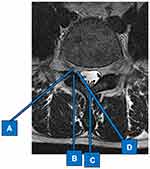 |
Figure 1 Various approaches to epidural steroid injection. (A) Transforaminal approach. (B) Parasagittal interlaminar approach. (C) Interlaminar approach. (D) Oblique interlaminar approach. |
The present study was conducted to compare the effectiveness and safety of fluoroscopic-guided OIL-ESI with that of TF-ESI in the management of low back and lumbosacral radicular pain.
Methods
Participants
The purpose of the study was explained to all patients, and written informed consent was obtained. All patients experienced lower back and unilateral lumbosacral radicular pain at the L3/L4 to L5/S1 levels. They were unresponsive to a 4-week conservative treatment with analgesics and physiotherapy. Herniation of intervertebral disc at L3/L4 to L5/S1 levels was diagnosed based on radiological findings on computed tomography or magnetic resonance imaging. Neurological signs of the patients were previously confirmed, and physical examinations such as the straight leg raise test were performed.
The exclusion criteria were as follows: low back pain with no radiating pain, a history of substance abuse or drug hypersensitivity, previous spinal surgery, a history of side effects due to steroid use, neurological deficits, bleeding tendency, and lactation and pregnancy.
Randomization was performed using computer-generated random numbers using Microsoft Excel (Microsoft Co., Redmond, WA, USA). The patients were divided into two groups. Those in group OIL (n = 33) underwent a fluoroscopic-guided OIL-ESI, and those in group TF (n = 33) underwent a fluoroscopic-guided TF-ESI.
Interventional Procedure
In both groups the needle entry point was checked under fluoroscopy. An initial AP fluoroscopic image was obtained to identify the level of the intervertebral disc and interlaminar space with the patient in a prone position and a pillow placed under the abdomen. The skin was swabbed with chlorhexidine-alcohol for sterilization. In the group OIL, a contralateral obliquely 15–30° in the caudo-cephalad direction of the fluoroscopy to achieve the “Scotty Dog” appearance of the lumbar spine. After local infiltration with lidocaine 1%, a 22-gauge, Tuohy needle (Hakko Co. Ltd., Osaka, Japan) was inserted at the level of disc pathology. The needle was advanced in a slight cephalad direction toward the most lateral part of the interlaminar opening, as indicated by the contralateral oblique projection on a plain image and a tunnel vision of the needle on fluoroscopy. The needle was inserted into the epidural space using the loss of resistance to saline technique and the oblique orientation of the needle was maintained throughout the procedure. In group TF, an ipsilateral oblique orientation of the fluoroscopy to achieve the “Scotty Dog” appearance of the lumbar spine. The needle was subsequently directed using the tunnel vision until the needle tip was in the posterior and superior aspect of the intervertebral foramen, as reviewed on lateral imaging, and in line with the pedicle on AP view.
In both groups, once the needle was in position, and after negative aspiration for cerebrospinal fluid and blood, iopamidol (Pamiray 300; Dongkook Pharm. Co. Ltd., Seoul, Korea) was injected using real-time, continuous fluoroscopy for the entire 3 mL volume of iopamidol and images were obtained in the lateral and AP projections. This was monitored to confirm the spread of contrast and to verify that no contrast medium entered the intravascular, subarachnoid, subdural, or intradiscal spaces. Lateral images were taken to evaluate the ventral epidural space. Perineural and segmental spread were also visualized in the anteroposterior view (Figure 2). After epidural space confirmation, 5 mg of dexamethasone mixed with 4 mL of 1% lidocaine was injected into the epidural space.
Immediately after the procedure, all patients were released home after taking rest at the pain clinic recovery room for about 30 minutes. Two weeks after the intervention (2nd week of the study), if there was no pain reduction of at least 50%, the same intervention was repeated at the pain clinic. After the next 2 weeks (4th week of the study), a third intervention was performed in the patients without pain reduction of at least 50%. The interventions were performed up to 4 times in the same way in each group at 0, 2, 4, and 8 weeks. Pain relief scores were recorded at the first visit and at 2, 4, 8, and 12 weeks after the procedure.
Outcome Measurements
The primary outcome of the study was the pain reduction after the procedure, assessed using the Visual Analogue Scale (VAS) at the pre-procedure, 2-, 4-, 8-, and 12-week visits. We also used the Oswestry Disability Index (ODI) and the Roland Morris Disability Questionnaire (RMDQ) (Appendix 1 and 2) and recorded the changes between the first visit and the 12-week visit. We recorded the spread patterns of the contrast medium during fluoroscopy in each procedure. We compared the spread of the contrast medium in the anterior epidural space and the unilateral or bilateral spread of contrast medium at the epidural space between the two groups. Twenty minutes after the procedure, muscle weakness and sensory abnormalities for less than 4 hours were assessed in the unilateral or bilateral lower extremities. Adverse events, such as paraplegia, nausea, vomiting, dizziness, headache, hypotension, procedure-induced hematoma, and local anesthetic toxicities were also evaluated and recorded. At the 12-week visit, the patients’ satisfaction was evaluated using a 4-point scale:13 1 (very dissatisfied), 2 (somewhat dissatisfied), 3 (somewhat satisfied), and 4 (very satisfied).
Statistical Analysis
Statistical analysis of all measurements was performed using PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, IL, USA). Continuous or categorical values were reported as mean ± standard deviation or number of patients (%), respectively. The Student’s t-test was used to compare the continuous values of the demographic data and VAS between the groups. The paired t-test was used to compare the VAS, ODI, and RMDQ scores before and after the procedure in each group. The chi-square or Fisher’s extract tests were used to compare the categorical values of the demographic data, the spread patterns of the contrast medium, possible adverse events, and patient satisfaction. P < 0.05 was considered statistically significant.
Sample Size Estimation
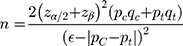
The primary outcome of the study was to compare the changes in the VAS scores between the two groups after 12 weeks. In a previous study,14 the VAS change rate (≥ 50% reduction from baseline) in the TF approach was 76.7% (pc = 0.767) and that in the parasagittal interlaminar approach was 78.1% (pt = 0.781). The estimated sample size was 33 patients per group, assuming that the clinical significance between the two groups did not differ by 30% (ϵ = 0.3), and type I (α) and type II (β) errors were 0.05 and 0.2, respectively. The sample size was calculated according to the following equation:
ϵ = 0.3, pc = 0.767, qc = 1 – pc, pt = 0.781, qt = 1 - qt,
Results
Sixty-six patients were included in the study. Seven patients refused to participate in the study. Fifty-nine patients completed the follow-up for the study duration of 12 weeks (Figure 3). Both groups were similar with respect to demographic and clinical characteristics (Table 1).
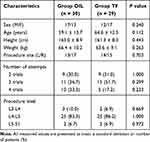 |
Table 1 Demographic Data |
In both groups, the VAS score was significantly lower two weeks after the first procedure. The mean differences (95% confidence interval) in the VAS score between the pre-procedure state and at 12 weeks were 37.3 ± 19.5 (30.065 to 44.601) in group OIL and 40.7 ± 14.9 (30.036 to 46.344) in group TF. The pain relief was within equivalence width between the two groups. There were no significant differences between the groups in the VAS score during the 12-week period (Figure 4). There were no significant differences in the ODI and RMDQ scores between the groups. The differences in the ODI and RMDQ scores between the pre-procedure state and at 12 weeks were higher in group TF than in group OIL. However, the differences were not statistically significant (Table 2).
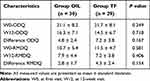 |
Table 2 The Differences in the Oswestry Disability Questionnaire (ODQ) and the Roland Morris Disability Questionnaire (RMDQ) Scores Between the First Visit and the 12-Week Visit |
The ventral epidural spread of the contrast medium was 73.3% in group OIL and 96.6% in group TF at two weeks after the procedure. Ventral epidural spread of contrast medium was lower than group TF at 2nd week visit epidural steroid injection (P = 0.013). In group OIL, the contralateral epidural spread of the contrast medium was 46.7%, 50.0%, 28.6%, and 10.0% at 0, 2, 4, and 8 weeks, respectively. In group TF, a contralateral epidural spread of the contrast medium was not shown at any visit. The contralateral epidural spread of the contrast medium was higher in group OIL than in group TF at 0, 2, and 4 weeks, respectively (P < 0.001, P < 0.001, and P = 0.035) (Table 3).
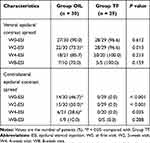 |
Table 3 Epidural Contrast Spread According to the Approaches |
There were 3 cases of paresthesia and 9 cases of motor weakness in the OIL group and 4 cases of motor weakness in the TF group. No other adverse events were found in either group. There were no significant differences in the incidence rate of adverse events after the procedure between the two groups. Complications such as hematoma, postdural puncture headache, or local anesthetic toxicity were not observed in either group.
At the 12-week visit, the patient satisfaction after the procedure was assessed. The number of patients who answered “somewhat dissatisfied” was significantly higher in group OIL than in group TF (Table 4).
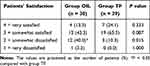 |
Table 4 Patients’ Satisfaction After the Procedure |
Discussion
The effectiveness of the ESI treatment depends on whether the steroids reach the nerve root lesion.15 Most disc herniations or nerve root compression lesions are located posterior to the vertebra; hence, it is suggested that an ESI would be more effective if delivered close to this targeted site.1 The TF-ESI is reported to be more effective than the interlaminar approach, as it allows a better ventral spread.15 However, the TF approach is associated with major complications such as paraplegia, epidural hematoma, and an intradiscal spread.16 Thus, various alternative approaches to replace the TF approach have recently been introduced. The lateral parasagittal interlaminar approach has been introduced, and it has been proved to be more effective than the midline conventional interlaminar approach and equally effective with the TF approach.9,14 Some studies introduced the OIL approach,10,11 and concluded that this approach could be an alternative to the TF approach; however, there was no direct comparison with the TF approach. Therefore, we compared the OIL-ESI to the conventional TF-ESI in the pain relief effect, safety, and contrast spread patterns.
The present study revealed that the OIL-ESI was equivalent in achieving effective pain relief to the TF-ESI in the management of low back and unilateral lumbosacral radiating pain. Similar functional improvements, including the ODI and RMDQ scores, were observed after the OIL-ESI and TF-ESI, although the OIL approach had a lower ventral epidural contrast spread at 2 weeks and a higher contralateral epidural contrast spread at 0, 2, and 4 weeks after the procedure. The results in the pain relief efficacy and adverse events rates were similar between the two groups, except for the patients’ satisfaction. The number of patients who answered “somewhat dissatisfied” was significantly higher in the OIL-ESI group than in the TF-ESI group.
We compared the clinical outcome after OIL-ESI with that after TF-ESI in patients with low back and unilateral lumbosacral radicular pain. The spread of the drug to the ventral epidural space reflects the efficacy of ESI.15 This was in fact confirmed through this and other, previous studies.1,15 Effective ventral epidural spreads have been achieved using several OIL approaches prior to our previous case report.12 There have been several studies on how well the drug is spreading to the ventral epidural space. A study evaluating the contrast flow pattern in the parasagittal interlaminar and TF approaches reported a ventral epidural spread of 100% and 75%, respectively.8 Another study investigated the ventral epidural contrast spread in the ventral interlaminar approach with placement of an epidural catheter at the ventrolateral portion of the nerve root in patients with low back and lumbar radicular pain at the L5 level.17 They reported a ventral epidural spread in all patients, concluding that lumbar ventral interlaminar ESIs can be an alternative method for ventral epidural injection. In our study, there was a 73.3–90.0% incidence of ventral epidural contrast spread with the OIL approach, whereas the ventral epidural contrast spread with the TF approach was 96.6–100.0% for all injections. The better ventral spread of the drug with these two approaches is most probably the reason for the better clinical outcomes. Our result also showed that an effective pain relief and functional improvement, including the ODI and RMDQ scores, were achieved using the OIL-ESI, and these were similar to those achieved with the TF-ESI. However, the OIL approach also showed 28.6–50.0% contralateral epidural spread, which may have caused the adverse events of paresthesia (10.0%) and motor weakness on both sides (30.0%). These results might have affected the patients’ satisfaction, as more patients who underwent OIL-ESIs answered “somewhat dissatisfied”.
The OIL approach offers a number of advantages over the TF approach. It has the advantage of clarifying the needle insertion point through the “Scotty Dog” view, and thus offers an alternative method to the transforaminal approach. In some postoperative states, the TF approach may be difficult due to the presence of rods, pedicle screws, and bone harvests for posterior lumbar interbody fusion. In addition, osteoarthritis that has developed at the superior or inferior borders of the transverse articular processes causes narrowing of the interspinous foramen. This narrowing makes it difficult to advance the needle in the TF approach. In these cases, caudal or conventional interlaminar approach can be performed; however, the OIL approach may be useful as an alternative method for effective drug delivery into the ventral epidural space.12 Another advantage of the OIL approach is that the needle is directed towards the most lateral part of the interlaminar opening; in this way, the needle tip meets the most lateral part of the sac, which is usually the nerve root lesion. Thus, the OIL approach would suffice to drive medication ventrally in the epidural space towards the interface of the exiting nerve root and the disc pathology.18,19
Complications in lumbar ESIs are extremely rare and most of them can be avoided by accurate needle placement, sterile techniques, and fluoroscopic-guided injections.20 In our study, there were no serious complications in both groups; however, some of the patients in the OIL group complained of paresthesia or motor weakness. These results can be attributed to the fact that the drug was spreading at only one level in the TF group, whereas in the OIL group, it was spreading to several levels, and even to the contra-lateral side.
This study has several limitations. First, there was no long-term follow-up; hence, the benefit of using corticosteroids via this approach for improving the long-term success could not be evaluated. Our study had only a 12-week follow-up period. Second, there was a lack of documentation of adjuvant therapies, such as individual patient exercise routines and analgesic drug therapy. Thus, additional between-group variability might have remained unadjusted. The third limitation is the utilization of a large-volume contrast and a high dose of dexamethasone. We used 3 mL of the contrast and 4 mL of a local anesthetic mixture for the injections. The same amount of contrast agent and local anesthetic was used in both groups, and therefore, the amount of injectate was high in the TF approach. In addition, more contrast medium than usual was needed to confirm its spread. The amounts of contrast and local anesthetic mixture were adopted from that used in the interlaminar approach in a previous study.21
In conclusion, ESIs delivered through the OIL approach are equivalent in achieving effective pain relief and functional improvement to those delivered through the TF approach in the management of low back and unilateral lumbosacral radicular pain. Further prospective, large scale, multi-center outcome studies are needed to prove the efficacy and safety of the OIL approach to the anterior epidural space versus the TF approach.
Ethics Approval and Consent to Participate
With the approval of the Institutional Review Board of Pusan National University Yangsan Hospital (ID 05–2015-104), 66 consecutive patients with low back and lumbosacral radicular pain, over 19 years of age, who had an American Society of Anesthesiologists physical status I and III, were assessed for study inclusion from the institute’s pain clinic from October 2015 to September 2016. The trial is registered with the Clinical Research Information Service (KCT0003557). This study was conducted in accordance with the Declaration of Helsinki.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Schaufele MK, Hatch L, Jones W. Interlaminar versus transforaminal epidural injections for the treatment of symptomatic lumbar intervertebral disc herniations. Pain Physician. 2006;9(4):361–366.
2. Lee JH, An JH, Lee S. Comparison of the effectiveness of interlaminar and bilateral transforaminal epidural steroid injections in treatment of patients with lumbosacral disc herniation and spinal stenosis. Clin J Pain. 2009;25(3):206–210. doi:10.1097/AJP.0b013e3181878f9e
3. Botwin KP, Natalicchio J, Hanna A. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective evaluation of epidurography contrast patterns and anatomical review of the epidural space. Pain Physician. 2004;7(1):77–80.
4. Weil L, Frauwirth NH, Amirdelfan K, Grant D, Rosenberg JA. Fluoroscopic analysis of lumbar epidural contrast spread after lumbar interlaminar injection. Arch Phys Med Rehabil. 2008;89(3):413–416. doi:10.1016/j.apmr.2007.08.161
5. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med. 2009;10(8):1389–1394. doi:10.1111/j.1526-4637.2009.00728.x
6. Candido KD, Katz JA, Chinthagada M, McCarthy RA, Knezevic NN. Incidence of intradiscal injection during lumbar fluoroscopically guided transforaminal and interlaminar epidural steroid injections. Anesth Analg. 2010;110(5):1464–1467. doi:10.1213/ANE.0b013e3181d6bd12
7. Wong SSC, Qiu Q, Cheung CW. Segmental spinal myoclonus complicating lumbar transforaminal epidural steroid injection. Reg Anesth Pain Med. 2018;43(5):554–556. doi:10.1097/AAP.0000000000000742
8. Candido KD, Raghavendra MS, Chinthagada M, Badiee S, Trepashko DW. A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg. 2008;106(2):638–644. doi:10.1213/ane.0b013e3181605e9b
9. Ghai B, Vadaje KS, Wig J, Dhillon MS. Lateral parasagittal versus midline interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: a double-blind, randomized study. Anesth Analg. 2013;117(1):219–227. doi:10.1213/ANE.0b013e3182910a15
10. Kraemer J, Ludwig J, Bickert U, Owczarek V, Traupe M. Lumbar epidural perineural injection: a new technique. Eur Spine J. 1997;6(5):357–361. doi:10.1007/BF01142687
11. Williams MT. The oblique interlaminar approach for fluoroscopy-guided lumbar puncture: keep the eye opened. Diagn Interv Imaging. 2014;95(6):629–632. doi:10.1016/j.diii.2014.02.010
12. Byeon GJ, Choi EJ, Choi YM, Chang EJ, Kim HJ, Kim KH. Oblique interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: a case report. Anesth Pain Med. 2017;12(4):375–380. doi:10.17085/apm.2017.12.4.375
13. Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine (Phila Pa 1976). 2000;25(24):3167–3177. doi:10.1097/00007632-200012150-00012
14. Ghai B, Bansal D, Kay JP, Vadaje KS, Wig J. Transforaminal versus parasagittal interlaminar epidural steroid injection in low back pain with radicular pain: a randomized, double-blind, active-control trial. Pain Physician. 2014;17(4):277–290.
15. Abdi S, Datta S, Lucas LF. Role of epidural steroids in the management of chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician. 2005;8(1):127–143.
16. Chang A, Ng AT. Complications associated with lumbar transforaminal epidural steroid injections. Curr Pain Headache Rep. 2020;24(11):67. doi:10.1007/s11916-020-00900-9
17. Choi YK, Barbella JD. Evaluation of epidurographic contrast patterns with fluoroscopic-guided lumbar interlaminar ventral epidural injection. Pain Pract. 2009;9(4):275–281. doi:10.1111/j.1533-2500.2009.00283.x
18. Crall TS, Gilula LA, Kim YJ, Cho Y, Pilgram T, Riew KD. The diagnostic effect of various needle tip positions in selective lumbar nerve blocks: an analysis of 1202 injections. Spine. 2006;31(8):920–922. doi:10.1097/01.brs.0000209325.52986.da
19. Stalcup ST, Crall TS, Gilula L, Riew KD. Influence of needle-tip position on the incidence of immediate complications in 2217 selective lumbar nerve root blocks. Spine J. 2006;6(2):170–176. doi:10.1016/j.spinee.2005.08.009
20. Goodman BS, Posecion LWF, Mallempati S, Bayazitoglu M. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med. 2008;1(3–4):212–222. doi:10.1007/s12178-008-9035-2
21. Furman MB, Kothari G, Parikh T, Anderson JG, Khawaja A. Efficacy of fluoroscopically guided, contrast-enhanced lumbosacral interlaminar epidural steroid injections: a pilot study. Pain Med. 2010;11(9):1328–1334. doi:10.1111/j.1526-4637.2010.00926.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.