Back to Journals » Infection and Drug Resistance » Volume 16
Comparison of Epidemiological Characteristics Between ESBL and Non-ESBL Isolates of Clinically Isolated Escherichia coli from 2014 to 2022: A Single-Center Study
Authors Zhang W , Wang Q, Zhang L, Wu J, Liu J, Lu C, Wang X, Zhang Z
Received 14 April 2023
Accepted for publication 1 August 2023
Published 9 August 2023 Volume 2023:16 Pages 5185—5195
DOI https://doi.org/10.2147/IDR.S414079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Suresh Antony
Wei Zhang,1,2,* Qing Wang,3,* Liru Zhang,4,* Jiangxiong Wu,5 Jinlu Liu,2 Cheng Lu,2 Xinsheng Wang,1 Zhihua Zhang6
1Central Laboratory, The First Affiliated Hospital of Hebei North University, Zhangjiakou, Hebei, People’s Republic of China; 2Microbiology Laboratory, The First Affiliated Hospital of Hebei North University, Zhangjiakou, Hebei, People’s Republic of China; 3Clinical Laboratory, State Key Laboratory of Complex Severe and Rare Diseases, Beijing, People’s Republic of China; 4Clinical Laboratory, Zhangjiakou Wanquan District Hospital, Zhangjiakou, Hebei, People’s Republic of China; 5Inspection Center, Qujing No.1 People’s Hospital, Affiliated Qujing Hospital of Kunming Medical University, Qujing, Yunnan, People’s Republic of China; 6Department of Respiratory and Critical Care Medicine, The First Affiliated Hospital of Hebei North University, Zhangjiakou, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhihua Zhang, Department of Respiratory and Critical Care Medicine, The First Affiliated Hospital of Hebei North University, Zhangjiakou, 36 Changqing Road, Qiaoxi District, Zhangjiakou City, Hebei Province, People’s Republic of China, Tel +86-03138043503, Fax +86-1088326317, Email [email protected] Xinsheng Wang, Central Laboratory, The First Affiliated Hospital of Hebei North University, Zhangjiakou, 36 Changqing Road, Qiaoxi District, Zhangjiakou City, Hebei Province, People’s Republic of China, Email [email protected]
Purpose: This single-center study aims to investigate the epidemiological characteristics of clinically isolated Escherichia coli from 2014 to 2022.
Methods: In vitro drug sensitivity of E. coli to 20 antibiotics was examined using the microbroth dilution method. A total of 7580 clinical E. coli strains were isolated from 2014 to 2022, among which 56.9% were identified as extended spectrum beta-lactamase-producing strains. The data were analyzed using the software WHONET5.6 and the R language platform.
Results: Over the study period, carbapenem resistance rates increased by more than 50% (2022 [1.34%] vs 2014 [0.8%]) and the annual number of isolates showed an upward trend (1264 in 2022 vs 501 in 2014). Drug resistance rates were the highest for penicillin (75– 85%) and lowest for imipenem (1%). The resistance rate of strains isolated from male patients and sputum was found to be higher than that of female patients and urine, except for quinolones (p < 0.05). The drug resistance rates from high to low were penicillins (75– 85%), tetracycline (64%), quinolones (64– 67%), sulfamethoxazole (59.3%), cephalosporins (22– 72%), aztreonam (34%), chloramphenicol (21%), amikacin (2.8%), colistin (1.4%), meropenem (1.1%), and imipenem (1%). Urine, sputum, and blood accounted for 51%, 16.6%, and 10.6% of the samples, respectively. A greater number of female patients were included more than male patients (4798[63.3%] vs 2782[26.7%]). Patients aged 50– 80 accounted for 64.2% of those surveyed.
Conclusion: Carbapenems remain the optimal choice for treating extended spectrum beta-lactamase-producing E. coli infections (sensitivity rate: 98%). Colistin (87.7%) and amikacin (87%) exhibited good antibacterial activities against carbapenem-resistant E. coli. Long-term and continuous epidemiological surveillance of E. coli can facilitate the development of preventive strategies and control policies.
Keywords: antibiotic resistance, bacteria, ESBL, carbapenems, cephalosporin, quinolones
Introduction
Escherichia coli (E. coli) is a common bacterium that can cause a wide range of infections in humans, including urinary tract infections, bloodstream infections, and gastrointestinal infections. Over the years, the emergence and spread of extended-spectrum β-lactamase (ESBL)-producing E. coli strains have become a significant concern in clinical settings.1–3 ESBLs are enzymes that confer resistance to a broad range of β-lactam antibiotics, including penicillins, cephalosporins, and monobactams.4,5
Understanding the epidemiological characteristics of ESBL-producing E. coli isolates is crucial for effective infection control and antibiotic stewardship. Previous studies have reported an increasing prevalence of ESBL-producing E. coli, highlighting the need for continuous monitoring of drug susceptibility patterns and the identification of risk factors associated with ESBL production.5–7
In addition to drug susceptibility, the sex ratio and age distribution of patients infected with ESBL-producing E. coli may provide valuable insights into the epidemiology and clinical management of these infections. Differences in susceptibility patterns and patient demographics could influence treatment decisions, infection control measures, and the development of targeted interventions.6
Therefore, this single-center study aims to compare the epidemiological characteristics between ESBL and non-ESBL isolates of clinically isolated E. coli from 2014 to 2022. By examining trends in drug susceptibility over time, sex ratio, and age distribution, we aim to provide a comprehensive understanding of the changing landscape of ESBL-producing E. coli infections. This knowledge will contribute to the development of effective strategies for infection control and antibiotic management, ultimately improving patient outcomes.
Materials and Methods
Research Program
For nine years (January 1, 2014 to December 31, 2022), a total of 40,116 clinical bacterial strains were isolated at the First Affiliated Hospital of Hebei North University (Zhangjiakou, Hebei Province, China), of which 8224 were identified as E. coli. After excluding 644 duplicate samples from the same patient, 7580 strains were isolated and included in the study (Figure 1). The separation and drug resistance rates and their trends, MIC50/90 values, and sector distribution were investigated. Research plan and ideas can be found in Figure 1.
 |
Figure 1 Outline of the research program followed in this study. |
Sample Collection
Clinical isolates of Escherichia coli were collected from various sources, including urine, blood, sputum, and wound specimens, from January 2014 to December 2022. Clinical samples were inoculated onto Columbia blood and MacConkey agar plates (Autobio, Zhengzhou City, Henan Province, China) and incubated at 35°C for 24 h. The isolates were obtained from both inpatients and outpatients who visited the hospital during this period.
Identification and Confirmation of Escherichia Coli
All isolates were initially identified as Escherichia coli using conventional microbiological techniques, including colony morphology, Gram staining, and the automated bacterial identification system (PhoenixTM100, BD, New Jersey, USA).
Drug Susceptibility Testing
Drug susceptibility testing was performed using the broth microdilution method according to the guidelines provided by the Clinical and Laboratory Standards Institute (CLSI). The source of the drug susceptibility plates and reagents used in this study was Becton Dickinson Company (BD, New Jersey, USA). The following antimicrobial agents were tested: amoxicillin-clavulanate; ampicillin/sulbactam; piperacillin; piperacillin/tazobactam; moxifloxacin; aztreonam; cephazolin; ceftazidime; cefotaxime; cefepime; imipenem; meropenem; colistin; sulfamethox-azole; chloramphenicol; gentamicin; amikacin; ciprofloxacin; levofloxacin; tetra-cycline. Pseudomonas aeruginosa ATCC27853 and E. coli ATCC25922 were used as quality control strains.
ESBL and CRE Detection
Extended-spectrum beta-lactamase (ESBL) production was determined using the double-disc synergy test, as recommended by the CLSI guidelines. The reference source for ESBL detection was Clinical and Laboratory Standards Institute M100-S30.8 ESBLeco is defined when the MIC of cefotaxime is ≥16μg/mL and the MIC of amoxicillin/clavulanic acid is ≤8μg/mL, or when the MIC of ceftazidime is ≥4μg/mL and the MIC of amoxicillin/clavulanic acid is ≤8μg/mL. NESBLeco is defined when the MIC of cefotaxime is ≤4μg/mL or the MIC of ceftazidime is ≤1μg/mL.
Carbapenem-resistant Enterobacteriaceae (CRE) detection was performed using the modified Hodge test, following the CLSI guidelines. The reference source for CRE detection was Clinical and Laboratory Standards Institute M100-S30.8 The MIC for imipenem and meropenem in CReco were ≥4 μg/mL and ≥4 μg/mL, respectively.
Statistical Analysis and Data Visualisation
The results were presented as frequencies and percentages for categorical variables. WHONET 5.6 software was used to perform raw data statistics. Statistical analysis was performed using R software (V4.2.1, SAS Institute, Inc., Cary, NC). The drug resistance rates were compared using an independent sample T-test, Welch’s t-test, or Mann–Whitney U-test, and data visualisation was performed using the ggplot2 package [3.3.6]. p <0.05 (*) was considered statistically significant; p <0.01 (**) and p <0.001 (***) were considered highly significant. Drawio software (V20.8.10, JGraph Ltd, Northampton, England) was used to produce a flowchart (Figure 1). Origin 2021 software (OriginLab, Northampton, UNITED STATES) was used to visualise changes in drug resistance rates and MIC frequency data.
Limitations
This study has several limitations, including its retrospective design, which may introduce selection bias. Additionally, the findings of this single-center study may not be generalizable to other healthcare settings.
Results
Clinical Characteristics
The number of female patients exceeds that of males (4798vs.2782), and the median age of females is higher than that of males (Median [IQR] [64 (19) vs 63 (39)], p <0.05). The median age of patients with NESBL, ESBL, and CRE infections was compared. The ESBL group had a lower median age than the NESBL group (Median [IQR] [61 (36) vs 64 (22)], p<0.01), while the CRE group had a higher median age than the NESBL group (Median [IQR] [67 (22) vs 64 (22), p>0.05). Additionally, the CRE group had a higher median age than the ESBL group (Median [IQR] [67 (22) vs 61 (36)], p<0.05) (Table 1). Patients are divided into four groups based on age (<18, 18–40, 41–60, >60), with the 18–40 group having the lowest proportion (4%) and the >60 group having the highest proportion (59.0%). Among patients with NESBL, ESBL, and CRE infections, the NESBL group had the highest proportion of female patients (68.9%), while the CRE group had the lowest proportion of female patients (45%). The departments with the highest rates of bacterial isolation are Neurology (12.7%), Urology (11.3%), and ICU (8.0%), while the sample types with the highest rates of bacterial isolation are urine (50.6%), sputum (17.4%), and blood (11.4%) (Table 1).
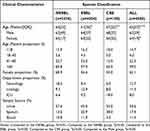 |
Table 1 Clinical Characteristics of Different Bacterial Species |
The top two departments with NESBLeco, ESBLeco, and CReco were urology (12.87%) and ICU (9.19%), neurology (17.98%) and endocrinology (14.55%), and ICU (18%) and neonatology (10%), respectively (Table S1).
Urine (51.0%, 3866/7580), sputum (16.6%, 1255/7580), and blood (10.6%, 801/7580) were the top three samples (Figure 2A). Over the nine-year period, the proportion of isolates from urine increased and sputum decreased, whereas that of blood remained unchanged (Figure 2B).
 |
Figure 2 Clinical distribution characteristics of E. coli. (A and B) Sample distribution characteristics. (C and D) Number of strains isolated/year. |
The annual number of E. coli isolates in our hospital (501 vs 1264) and number per 100,000 inpatients in the institution (107 vs 180) increased compared to that of the initial population (Figures 2C and D).
Drug Sensitivity Characteristics
Most penicillins and their enzyme inhibitors quinolones and cephalosporins have high resistance rates in E. coli, with values ranging from 50 to 85%. In the present study, resistance rates for carbapenem, colistin, and amikacin were low, ranging from 1 to 3% (Figure 3A). Over nine years, drug resistance rates of penicillin and its enzyme inhibitors, cephalosporins, tetracycline, and sulfamethoxazole have shown a slow downward trend. The drug resistance rate of third-generation cephalosporins neared 60%, except in 2021 (51.7%). The drug resistance rate of carbapenems increased significantly by more than 50% (0.8% vs 1.34%). Resistance rates of quinolones and chloramphenicol showed a slow upward trend (Figures 3B–G, Table S2).
 |
Figure 3 (A) The overall resistance rate of E. coli. (B–G) Changes in annual drug resistance rates. |
Overall, imipenem, meropenem, and amikacin showed the highest sensitivity to E. coli (>97%), and penicillin and its enzyme inhibitors were less sensitive (<18%) (Table 2).
 |
Table 2 Susceptibility of Escherichia Coli to 20 Types of Antibiotics |
NESBLeco showed more than 98% sensitivity to cephalosporins, carbapenems, colistin, and amikacin (Table S3). For NESBLeco, some antibiotics in the same class showed higher resistance (ampicillin [67.7%] vs piperacillin [50.8%], p <0.05; amoxicillin/clavulanate [66.6%] and ampicillin/sulbactam [61.5%] vs piperacillin/tazobactam [3.8%], p <0.05; gentamicin [37.55%] vs amikacin [0.6%], p <0.05), whereas others did not (imipenem [0.1%] vs meropenem [0.2%], p >0.05; ciprofloxacin [53.7%] vs levofloxacin [49.6%], p >0.05) (Table S3, Figure 4).
For ESBLeco, the antibacterial activities of imipenem, meropenem, colistin, and amikacin were very high (>95%) while those of penicillin and its enzyme inhibitor were low (<10%) (Table S4). Within the same class of antibiotics, some had higher rates of resistance (ampicillin [97.6%] vs piperacillin [94%], p <0.05; amoxicillin/clavulanate [83.9%] and ampicillin/sulbactam [87.4%] vs piperacillin/tazobactam [21.3%], p <0.05; gentamicin [49.4%] vs amikacin [4.4%], p <0.05), whereas others showed no difference (imipenem [1.8%] vs meropenem [1.8%], p >0.05; ciprofloxacin [77.3%] vs levofloxacin [74.3%], p >0.05) (Table S4, Figure 4).
CReco was only highly sensitive to amikacin and colistin (>87%), whereas its sensitivity to the other tested antibiotics was low (< 45%) (Table S5).
Strains isolated from sputum and men showed higher rates of resistance to multiple antibiotics than those isolated from urine and women, respectively (p <0.05) (Table 3).
 |
Table 3 Antibacterial Resistance Rates for Different Samples and Genders |
Compared with ESBLeco and NESBLeco, CReco had higher MIC values for antibiotics with the highest frequency, except for amikacin and colistin (Figure S1).
Discussion
E. coli, a gram-negative bacterium, is one of the microorganisms most closely associated with humans. They colonise the digestive tracts of humans and animals and play an important role in public health, cell engineering, and animal husbandry. This study discussed the clinical characteristics of E. coli. In global infectious diseases, E. coli is one of the most important pathogens causing human death.9–11 Our results showed that middle-aged people (41–60 years old) and older adults (>60 years old) accounted for a higher proportion of the patient population than teenagers and adults (<40 years old). Our research results indicate that Escherichia coli (E. coli) infection is associated with age, particularly being more common in the elderly and infants. In fact, the elderly and infants are among the high-risk populations for E. coli infection. The immune system of the elderly may be weakened due to aging, while the immune system of infants may not have fully developed, making them more susceptible to E. coli infection.
In this study, urinary tract infections accounted for more than half of the total number (51%), and majority of infected patients were women (63.3%), similar to that observed in Algeria.12 Urinary tract infections can be classified as asymptomatic bacteriuria, acute cystitis, and pyelonephritis. Transient febrile urinary tract infections are usually caused by toxic E. coli. Furthermore, pregnant women are prone to urinary tract infections and have an increased risk of death.13,14 In a study in Ethiopia, 41% of urinary tract infections in pregnant women were caused by E. coli.15 Urinary tract infection (UTI) is a common infectious disease, especially among children around the age of one. Escherichia coli is one of the most common pathogens, which can enter the bladder through the urethra and cause infection. Interestingly, in this age group, girls have a higher incidence of UTIs than boys. Therefore, gender is an important consideration when evaluating UTIs in children. The higher incidence of UTIs in girls may be related to anatomical differences and hormonal factors. Girls have a shorter urethra and it is closer to the anus, making it easier for bacteria to enter the urethra and further infect the bladder. In addition, girls have hormonal differences, especially before puberty, with lower estrogen levels, which may weaken the protective barrier of the urethral mucosa and increase the risk of infection.
Drug-resistant bacteria, especially multidrug-resistant bacteria, pose a major public health challenge. Antibiotic resistance is often associated with changes in binding targets, hydrolase production, and overexpression of drug efflux pumps.16,17 Drug resistance genes can be horizontally transmitted between different bacteria through genetic mobile elements, resulting in an increasingly serious drug resistance problem.18–20 Antibiotic-resistant bacteria cause higher in-hospital mortality and total hospital costs than susceptible strains.21 However, timely and effective antibiotic treatment is likely to result in treatment costs for patients with bloodstream infections caused by ESBLeco that are no higher than those caused by NESBLeco.22 The separation rate of ESBLeco varies greatly among different countries and regions in the world (4.5–41%), but is mostly lower than 10%.23 The eastern coastal regions and major cities in China are high-risk areas for ESBL-producing Escherichia coli (ESBL-EC) infections. The healthcare institutions and densely populated areas in these regions are more prone to the occurrence and transmission of ESBL-EC. Furthermore, there is an increasing trend in the clinical isolation of ESBL-EC in China, posing challenges to clinical treatment and public health.24 Therefore, it is necessary to strengthen prevention and control measures. The overuse of antibiotics has also led to E. coli strains from cows, pigs, and chickens developing resistance to most antibiotics, and these resistant bacteria have even been isolated from wastewater.25–27 This study revealed a concerning finding - The annual average separation rate of ESBLeco in our test region (Zhangjiakou, Hebei Province, China) was alarmingly high at 56.9%, significantly surpassing the global average. Between 2013 and 2021, third-generation cephalosporins emerged as the most commonly used antimicrobial agents in Chinese tertiary and secondary hospitals, accounting for approximately one-third of the total antimicrobial consumption.28 This statistic indirectly highlights the correlation between antibiotic usage and the emergence of drug-resistant bacteria. These findings emphasize the urgent need for effective strategies to combat antimicrobial resistance and promote responsible antibiotic stewardship in healthcare settings.
This study showed that the annual average separation rate of ESBLeco was 56.9%, much higher than the world average level. This may be due to the high frequency and quantity of third-generation cephalosporins used in our test region (Zhangjiakou, Hebei Province, China), which should be of concern to health and epidemic prevention departments. The prevalence of CReco is less than 1%, as reported by 24 large bacterial resistance surveillance organisations worldwide, with the exception of the Central and Eastern European Antimicrobial Resistance Surveillance Program and the Philippine Antimicrobial Resistance Surveillance Program.23 The prevalence of CReco in our region in 2022 was 1.34%, being lower than that of CReco (2.65%) and carbapenem-resistant Klebsiella pneumoniae isolated from Hebei Province, China (14.6%).29,30 This is slightly higher than the global average, but it should be noted that it increased by 67.5% when compared with results from 2014 (1.34% vs 0.8%). CReco was defined as an “urgent threat” by the World Health Organisation and changes in its prevalence are of great concern.
Among E. coli strains isolated from women in the Washington community, patients older than 50 had higher rates of antibiotic-resistant strains than those younger than 19.31 In this study, for most of the tested antibiotics, the resistance rates of strains isolated from men and sputum were higher than those of women and urine; however, quinolones showed the opposite trend (p <0.05) (Table 2). Levofloxacin-resistant E. coli isolated from Africa, Europe, Asia, and Latin America causes more than twice as many urinary tract infections as respiratory infections.32 Different medication habits for different populations or infection sites may lead to dissimilarities in bacterial resistance rates.
ESBL and CRE are two common multidrug-resistant strains of Escherichia coli. The increasing prevalence of these strains in clinical settings poses significant challenges to public health and clinical practice. Firstly, the multidrug resistance of ESBL and CRE strains makes the treatment of infections more difficult. Traditional antibiotics have lost their effectiveness against these strains, leading to complex and time-consuming treatment of infections.7 Secondly, ESBL and CRE strains spread rapidly and are easily transmitted within healthcare facilities. These strains can be transmitted to other patients and healthcare workers through contact, airborne transmission, and food transmission, increasing the risk of infection.33 This poses a threat to public health, especially in high-risk environments such as healthcare facilities and long-term care facilities. By strengthening monitoring and reporting, implementing strict infection control measures, rationalizing antibiotic use, enhancing education and training, and strengthening international cooperation, we can effectively address this issue and protect public health.
Conclusions and Future Directions
Understanding the evolution of E. coli resistance and antimicrobial activity of different types of drugs are crucial for making policy decisions, especially for infection control programs. Data gaps exist in many underdeveloped regions, and pathogen microbiology laboratories and data collection capabilities must be enhanced to improve our understanding of this important human pathogen. Bacterial genotyping has made a great contribution to the epidemiology of drug-resistant bacteria, and it should gradually become the mainstream monitoring method to be implemented.
Data Sharing Statement
The first author may provide data that supports the results of the report upon reasonable request.
Ethical Considerations
This study was approved by the Institutional Review Board/Ethics Committee of the First Affiliated Hospital of Hebei North University (No. K2019147). Patient confidentiality was strictly maintained throughout the study, and all data were anonymized and securely stored.
Informed Consent Statement
Patient consent was waived due to the retrospective and non-invasive nature of this observational study.
Acknowledgments
Thank our colleagues Wang Na and Wang Teng for their help in data statistics. We would like to thank Editage (www.editage.cn) for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the Natural Science Foundation of Hebei Province and S&T Program of Hebei (No. C2022405023), Hebei Provincial Health Commission Key Science and Technology Research Program (No. 20210702,20190904 and 20180843), and Zhangjiakou Key R&D Program Project Big Health and Biomedical Project (No. 2121098D). Hebei Provincial Health Commission Government Funded Clinical Medicine Talent Training Project (2021, Innovative team for precise diagnosis and treatment of fungal infections in the northwest region of Hebei Province).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Barrios H, Garza-Ramos U, Mejia-Miranda I, et al. ESBL-producing Escherichia coli and Klebsiella pneumoniae: the most prevalent clinical isolates obtained between 2005 and 2012 in Mexico. J Glob Antimicrob Resist. 2017;10:243–246. doi:10.1016/j.jgar.2017.06.008
2. Chong Y, Shimoda S, Shimono N. Current epidemiology, genetic evolution and clinical impact of extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae. Infect Genet Evol. 2018;61:185–188. doi:10.1016/j.meegid.2018.04.005
3. Martischang R, François P, Cherkaoui A, et al. Epidemiology of ESBL-producing Escherichia coli from repeated prevalence studies over 11 years in a long-term-care facility. Antimicrob Resist Infect Control. 2021;10(1):148. doi:10.1186/s13756-021-01013-7
4. McDonald KL, Garland S, Carson CA, et al. Measures used to assess the burden of ESBL-producing Escherichia coli infections in humans: a scoping review. JAC Antimicrob Resist. 2021;3(1):dlaa104. doi:10.1093/jacamr/dlaa104
5. Onduru OG, Mkakosya RS, Aboud S, Rumisha SF. Genetic determinants of resistance among ESBL-producing enterobacteriaceae in community and hospital settings in East, Central, and Southern Africa: a systematic review and meta-analysis of prevalence. Can J Infect Dis Med Microbiol. 2021;2021:5153237. doi:10.1155/2021/5153237
6. Karlowsky JA, Lob SH, DeRyke CA, et al. Prevalence of ESBL non-CRE Escherichia coli and Klebsiella pneumoniae among clinical isolates collected by the SMART global surveillance programme from 2015 to 2019. Int J Antimicrob Agents. 2022;59(3):106535. doi:10.1016/j.ijantimicag.2022.106535
7. Kawamura K, Nagano N, Suzuki M, Wachino JI, Kimura K, Arakawa Y. ESBL-producing Escherichia coli and its rapid rise among healthy people. Food Saf. 2017;5(4):122–150. doi:10.14252/foodsafetyfscj.2017011
8. CLSI. Performance standards for antimicrobial susceptibility testing. In: Clinical and Laboratory Standards Institute.
9. Stoll BJ, Puopolo KM, Hansen NI, et al. Early-onset neonatal sepsis 2015 to 2017, the rise of Escherichia coli, and the need for novel prevention strategies. JAMA Pediatr. 2020;174(7):e200593. doi:10.1001/jamapediatrics.2020.0593
10. Flannery DD, Edwards EM, Puopolo KM, Horbar JD. Early-onset sepsis among very preterm infants. Pediatrics. 2021;148(4). doi:10.1542/peds.2021-052456
11. Murray CJL, Ikuta KS, Sharara F; Collaborators AR. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi:10.1016/s0140-6736(21)02724-0
12. Ait-Mimoune N, Hassaine H, Boulanoir M. Bacteriological profile of urinary tract infections and antibiotic susceptibility of Escherichia coli in Algeria. Iran J Microbiol. 2022;14(2):156–160. doi:10.18502/ijm.v14i2.9180
13. Kalinderi K, Delkos D, Kalinderis M, Athanasiadis A, Kalogiannidis I. Urinary tract infection during pregnancy: current concepts on a common multifaceted problem. J Obstet Gynaecol. 2018;38(4):448–453. doi:10.1080/01443615.2017.1370579
14. Tullus K, Shaikh N. Urinary tract infections in children. Lancet. 2020;395(10237):1659–1668. doi:10.1016/s0140-6736(20)30676-0
15. Chelkeba L, Fanta K, Mulugeta T, Melaku T. Bacterial profile and antimicrobial resistance patterns of common bacteria among pregnant women with bacteriuria in Ethiopia: a systematic review and meta-analysis. Arch Gynecol Obstet. 2022;306(3):663–686. doi:10.1007/s00404-021-06365-4
16. Lopatkin AJ, Bening SC, Manson AL, et al. Clinically relevant mutations in core metabolic genes confer antibiotic resistance. Science. 2021;371(6531). doi:10.1126/science.aba0862
17. Arbab S, Ullah H, Wang W, Zhang J. Antimicrobial drug resistance against Escherichia coli and its harmful effect on animal health. Vet Med Sci. 2022;8(4):1780–1786. doi:10.1002/vms3.825
18. Partridge SR, Kwong SM, Firth N, Jensen SO. Mobile genetic elements associated with antimicrobial resistance. Clin Microbiol Rev. 2018;31(4). doi:10.1128/CMR.00088-17
19. Poirel L, Madec JY, Lupo A, et al. Antimicrobial Resistance in Escherichia coli. Microbiol Spectr. 2018;6(4). doi:10.1128/microbiolspec.ARBA-0026-2017
20. Van Boeckel TP, Pires J, Silvester R, et al. Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science. 2019;365(6459). doi:10.1126/science.aaw1944
21. Iskandar K, Rizk R, Matta R, et al. Economic burden of urinary tract infections from antibiotic-resistant Escherichia coli among hospitalized adult patients in lebanon: a prospective cohort study. Value Health Reg Issues. 2021;25:90–98. doi:10.1016/j.vhri.2021.03.001
22. Wang N, Zhan M, Liu J, et al. Prevalence of carbapenem-resistant Klebsiella pneumoniae infection in a Northern Province in China: clinical characteristics, drug resistance, and geographic distribution. Infect Drug Resist. 2022;15:569–579. doi:10.2147/idr.S347343
23. Diallo OO, Baron SA, Abat C, Colson P, Chaudet H, Rolain JM. Antibiotic resistance surveillance systems: a review. J Glob Antimicrob Resist. 2020;23:430–438. doi:10.1016/j.jgar.2020.10.009
24. Liu Y, Zhu M, Fu X, et al. Escherichia coli causing neonatal meningitis during 2001–2020: a study in Eastern China. Int J Gen Med. 2021;14:3007–3016. doi:10.2147/ijgm.S317299
25. Goulart DB, Mellata M. Escherichia coli mastitis in dairy cattle: etiology, diagnosis, and treatment challenges. Front Microbiol. 2022;13:928346. doi:10.3389/fmicb.2022.928346
26. Yu D, Ryu K, Zhi S, Otto SJG, Neumann NF. Naturalized Escherichia coli in wastewater and the co-evolution of bacterial resistance to water treatment and antibiotics. Front Microbiol. 2022;13:810312. doi:10.3389/fmicb.2022.810312
27. Zhou W, Lin R, Zhou Z, et al. Antimicrobial resistance and genomic characterization of Escherichia coli from pigs and chickens in Zhejiang, China. Front Microbiol. 2022;13:1018682. doi:10.3389/fmicb.2022.1018682
28. Wushouer H, Zhou Y, Zhang W, et al. Inpatient antibacterial use trends and patterns, China, 2013–2021. Bull World Health Organ. 2023;101(4):248–261b. doi:10.2471/blt.22.288862
29. Zhang W, Li Z, Wang N, et al. Clinical distribution characteristics of 1439 carbapenem-resistant Escherichia coli strains in china: drug resistance, geographical distribution, antibiotic MIC50/90. Infect Drug Resist. 2021;14:4717–4725. doi:10.2147/idr.S334283
30. Wang Y, Xiao T, Zhu Y, et al. Economic burden of patients with bloodstream infections caused by extended-spectrum β-lactamase-producing Escherichia coli. Infect Drug Resist. 2020;13:3583–3592. doi:10.2147/idr.S271230
31. Frisbie L, Weissman SJ, Kapoor H, et al. Antimicrobial resistance patterns of urinary Escherichia coli among outpatients in Washington State, 2013–2017: associations with age and sex. Clin Infect Dis. 2021;73(6):1066–1074. doi:10.1093/cid/ciab250
32. Stone GG, Hackel MA. Antimicrobial activity of ceftazidime-avibactam and comparators against levofloxacin-resistant Escherichia coli collected from four geographic regions, 2012–2018. Ann Clin Microbiol Antimicrob. 2022;21(1):13. doi:10.1186/s12941-022-00504-8
33. McDanel J, Schweizer M, Crabb V, et al. Incidence of Extended-Spectrum β-Lactamase (ESBL)-producing Escherichia coli and Klebsiella infections in the United States: a systematic literature review. Infect Control Hosp Epidemiol. 2017;38(10):1209–1215. doi:10.1017/ice.2017.156
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

