Back to Journals » Infection and Drug Resistance » Volume 15
Clinical Comparative Evaluation of the LabTurboTM AIO® Reverse Transcription-Polymerase Chain Reaction and World Health Organization-Recommended Assays for the Detection of Emerging SARS-CoV-2 Variants of Concern
Authors Chang CK, Jian MJ, Chung HY, Lin JC, Hsieh SS, Tang S, Perng CL, Chen CW, Hung KS, Chang FY, Shang HS
Received 16 November 2021
Accepted for publication 5 February 2022
Published 22 February 2022 Volume 2022:15 Pages 595—603
DOI https://doi.org/10.2147/IDR.S349669
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Chih-Kai Chang,1,* Ming-Jr Jian,1,* Hsing-Yi Chung,1 Jung-Chung Lin,2 Shan-Shan Hsieh,1 Sheng‐Hui Tang,1 Cherng-Lih Perng,1 Chien-Wen Chen,3 Kuo-Sheng Hung,4 Feng-Yee Chang,2 Hung-Sheng Shang1
1Division of Clinical Pathology, Department of Pathology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China; 2Division of Infectious Diseases and Tropical Medicine, Department of Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China; 3Division of Pulmonary and Critical Care Medicine, Department of Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China; 4Center for Precision Medicine and Genomics, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China
*These authors contributed equally to this work
Correspondence: Hung-Sheng Shang; Feng-Yee Chang, Tel +886920713130, Fax +886287927226, Email [email protected]; [email protected]
Purpose: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent behind coronavirus disease-2019 (COVID-19). Single-plex reverse transcription-polymerase chain reaction (RT-PCR)-based assays are widely used for COVID-19 detection but exhibit decreased sensitivity and specificity in detecting the rapidly spreading SARS-CoV-2 variants; in contrast, multiplex RT-PCR reportedly yields better results. Here, we aimed at comparatively analyzing the clinical performance of the LabTurboTM AIO COVID-19 RNA testing kit, a multiplex quantitative RT-PCR kit, including a three-target (E, N1, and RNase P), single-reaction, triplex assay used for SARS-CoV-2 detection, with that of the WHO-recommended RT-PCR assay.
Materials and Methods: Residual, natural, nasopharyngeal swabs obtained from universal transport medium specimens at SARS-CoV-2 testing centers (n = 414) were collected from May to October 2021. For SARS-CoV-2 qRT-PCR, total viral nucleic acid was extracted. The limit of detection (LOD) and the comparative clinical performances of the LabTurboTM AIO COVID-19 RNA kit and the WHO-recommended RT-PCR assay were assessed. Statistical analysis of the correlation was performed and results with R2 values > 0.9 were considered to be highly correlated.
Results: The LOD of the LabTurboTM AIO COVID-19 RNA kit was 9.4 copies/reaction for the target genes N1 and E. The results obtained from 102 SARS-CoV-2-positive and 312 SARS-CoV-2-negative samples showed 100% correlation with previous WHO-recommended RT-PCR assay results.
Conclusion: Multiplex qRT-PCR is a critical tool for detecting unknown pathogens and employs multiple target genes. The LabTurboTM AIO COVID-19 RNA testing kit provides an effective and efficient assay for SARS-CoV-2 detection and is highly compatible with SARS-CoV-2 variants.
Keywords: SARS-CoV-2, COVID-19, variants of concern, COVID-19 RNA testing kit, multiplex qRT-PCR
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a member of the beta-coronavirus lineage B (B-βCoV), is spreading rapidly worldwide. This virus causes an infectious respiratory disease known as coronavirus disease-2019 (COVID-19).1,2 On January 30, 2020, the World Health Organization (WHO) declared this disease a “Public Health Emergency of International Concern”, given the serious global health crisis caused by SARS-CoV-2.3 The clinical symptoms of COVID-19 are similar to that of infections caused by influenza viruses or other common respiratory viruses.4
The ongoing global pandemic caused by multiple SARS-CoV-2 variants emerged in the Fall of 2020. These variants are more transmissible and infectious than the original strain, leading to their rapid spread.5 The SARS-CoV-2 B.1.1.7 (Alpha) variant was first detected in the United Kingdom in September 2020; its prevalence has increased in numerous counTries, including the United States and Europe.6,7 Additionally, the B.1.351 (Beta) and B.1.617 (Delta) variants were first identified in South Africa and India in December 2020, respectively. Furthermore, these variants have been associated with high mortality rates.8
SARS-CoV-2 nucleic acid testing using reverse transcription-polymerase chain reaction (RT-PCR), the gold standard for detecting acute infections9–11 was developed by Corman et al12 as recommended by the WHO and the Centers for Disease Control (CDC)13 and is used worldwide. However, some studies have reported that regular single-plex RT-PCR cannot detect SARS-CoV-2 variants, leading to decreased sensitivity and specificity of SARS-CoV-2 detection. Moreover, N, a SARS-CoV-2 target gene, was reported to show dropout or cycle threshold (Ct) value shifts in the evaluation of B.1.1.7 variants.14,15
The primer/probe sets recommended by the WHO and the CDC use identical fluorescent reporters. These require each target gene to be assayed separately, leading to high reagent consumption and low production capacity when evaluating samples in a 96-well plate. Although commercially available systems, including the Cepheid Xpert Xpress SARS-CoV-2 (Cepheid, Sunnyvale, CA), DiaSorin Simplexa (Saluggia, Italy), and Cobas 6800 (Roche Diagnostics, Indianapolis, IN), show high sensitivity and require short testing times, these require unique instruments. Therefore, more accessible assays are needed to confirm or rule out SARS-CoV-2 infection. Multiplex quantitative (q)RT-PCR assays can yield multiple results in a single test run effectively and efficiently, with decreased reagent consumption and shorter test duration. The LabTurboTM AIO COVID-19 RNA testing kit (Cat. No. Acov11240; Taigen Bioscience Corp., Taipei, Taiwan) is a commercially available, multiplex, quantitative RT-PCR kit for a three-target (E, N1, and RNase P), single-reaction, triplex assay for SARS-CoV-2 detection and is highly compatible with many other real-time PCR platforms.
Here, we evaluated the clinical performance of the LabTurboTM AIO COVID-19 RNA testing kit and determined its limit of detection (LOD) compared with current WHO-recommended qRT-PCR assays.
Materials and Methods
Clinical Specimens
Between May and October 2021, 414 residual, natural, nasopharyngeal swabs were obtained from universal transport medium specimens at SARS-CoV-2 testing centers and frozen at −80°C. The Taiwan CDC Central Laboratory confirmed that 102 original specimens tested positive for SARS-CoV-2 using the WHO-recommended RT-PCR assay,12 while the remaining 312 specimens were negative. All procedures performed in this study were approved by the Institutional Review Board of the Tri-Service General Hospital (TSGHIRB No. C202005041) registered in March 2021. Written informed consent was obtained from the patients.
RNA Extraction
Total viral nucleic acid was extracted from 300 µL of each nasopharyngeal swab in a universal transport medium and eluted in a final volume of 60 µL using the LabTurbo Virus Mini Kit (Cat. No. LVN480-300) and an automated LabTurbo 48 Compact extraction system (Taigen Bioscience Corp., Taipei, Taiwan) according to the manufacturer’s instructions. Each extracted viral RNA was stored at −80 °C until use.
SARS-CoV-2 qRT-PCR
The five different primer/probe sets and sequences used for the SARS-CoV-2 detection assays are listed in Table 1. For single-plex qRT-PCR, E and N primer/6-carboxyfluorescein (FAM)-labeled probe sets were designed for the non-coding region, as described previously12 for SARS-CoV-2 qRT-PCR. The LabTurboTM AIO COVID-19 RNA testing kit for SARS-CoV-2 multiplex qRT-PCR, containing reverse transcriptase, primer/probe mixture, and 2× PCR master mix, was utilized according to the manufacturer’s instructions. In this kit, probes for E and N1 were labeled with Hexachloro-fluorescein (HEX) and FAM fluorescent reporters, respectively. RNase P primer/Cy5-labeled probe sets (designed as quality control for RNA extraction to detect human nucleic acids) were developed by the CDC using fluorescent reporter modification and are published on the CDC website.13,16 Each 25 µL reaction mixture contained 12.5 µL of 2× PCR master mix, 2.5 µL of primer/probe mixture, 1.25 µL of reverse transcriptase, 2.75 µL of RNase-free water, and 6 µL of extracted RNA template. SARS-CoV-2 qRT-PCR was performed on a Rotor-Gene-Q real-time PCR instrument (Qiagen, Hilden, Germany) and a Roche LightCycler® 96 instrument (Roche Diagnostics, Indianapolis, IN) under the following thermocycling conditions: Reverse transcription at 55°C for 10 min and pre-denaturation at 95°C for 1 min, followed by 45 cycles of 95°C for 10s and 60°C for 15s. A Ct value of < 36 was considered a true positive while a Ct value of > 36 indicated re-testing.
 |
Table 1 Primer and Probe Sequences Used for Real-Time Reverse Transcription-Polymerase Chain Reaction (PCR) to Detect Severe Acute Respiratory Syndrome Coronavirus 2 |
SARS-CoV-2 Variants of Concern (VOC) Screening Test Using the VirSNiP Probe-Based Melting Curve Assay
Briefly, the VirSNiP SARS-CoV-2 assay17 (TIB Molbiol, Berlin, Germany) included real-time RT-PCR post-melting curve analysis to detect six spike gene mutations as follows: N501Y, H69/V70, K417N, E484K, P681R, and L452R in SARS-CoV-2 VOC. Distinguishment of SARS-CoV-2 VOCs was based on spike gene mutations detected as follows: N507Y and del H69/V70 for B.1.1.7 (Alpha variant); N507Y, E484K and K417N for B.1.351 (Beta variant); P681R and L452R for B.1.617 (Delta variant). The VirSNiP assay was performed using a LightCycler® 96 (Roche Molecular Systems, Inc.) according to the manufacturer’s instructions. Cycling conditions were as follows: Reverse transcription for 5 min at 55°C; denaturation for 5 min at 95°C; amplification for 45 cycles of 5 s at 95°C, 15s at 60°C, and 15s at 72°C, melting for 30s at 95°C, 2 min at 40°C, with a continuous temperature rise to 95°C at a 4.4°C ramp rate; a final cooling step of 30s at 40°C. Fluorescent signals were detected and analyzed with the LightCycler software 1.1.
Determination of LOD
Dilutions of SARS-CoV-2-positive clinical samples were to preliminarily assess analytical sensitivity. To determine the LOD of the LabTurboTM AIO COVID-19 RNA testing kit for both E and N1, two-fold serial dilutions of an AMPLIRUN SARS-CoV-2 RNA control (Vircell, Granada, Spain) from 300 to 9.4 copies/reaction were used (n = 20). The LOD was defined as a 95% probability of 20 replicates testing positive.
Evaluation of Specificity
The specificity of the LabTurboTM AIO COVID-19 RNA testing kit was evaluated using three common upper respiratory tract viruses, as described in our previous report.18 Samples positive for influenza A, influenza B, and respiratory syncytial virus were obtained from viral cultures at the Taiwan CDC Viral Infection Contract Laboratory.
Comparison of Clinical Performance
A total of 414 viral RNA extracts from residual, natural, nasopharyngeal swabs obtained from universal transport medium specimens, of which 102 were confirmed as SARS-CoV-2-positive and 312 as SARS-CoV-2-negative, was evaluated to determine the clinical performance of the LabTurboTM AIO COVID-19 RNA testing kit on the Rotor-Gene-Q real-time PCR instrument and Roche LightCycler® 96 instrument. A total of 102 SARS-CoV-2-positive samples spanned the full range of previously observed Ct values (11–36 cycles). Statistical analysis of correlation was performed using Microsoft Office 365 Excel. R2 values of > 0.9 were considered to be highly correlated.
Results
Analytical Sensitivity of the LabTurboTM AIO COVID-19 RNA Testing Kit
Analytical sensitivity (LOD) was preliminarily assessed at concentrations around the detection endpoint using serial dilutions. To accurately determine the analytical sensitivity, 20 replicate reactions were performed, yielding 9.4 copies per reaction for both N1 and E using the LabTurboTM AIO COVID-19 RNA testing kit (Table 2).
 |
Table 2 Limit of Detection of LabTurboTM AIO COVID-19 RNA Testing Kit for N1 and E Using the Rotor-Gene-Q Real-Time PCR Instrument |
Clinical samples obtained from respiratory viruses, including those positive for influenza A, influenza B, respiratory syncytial virus, rhinovirus, parainfluenza virus, and adenovirus, as well as cell culture supernatants, were used to assess the kit’s analytical specificity. The E and N1 primer/probe sets from the LabTurboTM AIO COVID-19 RNA testing kit were found to be highly specific for SARS-CoV-2. Furthermore, they did not show cross-reactivity with the tested viruses or the cell culture supernatants (Table 3).
 |
Table 3 Cross-Reaction of the LabTurboTM AIO COVID-19 RNA Testing Assay with Known Respiratory Viruses in Clinical Samples or Cell Supernatants |
Comparison of Clinical Performance
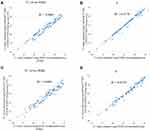
The RNase P target gene was not included in this comparison as it was used as quality control for RNA extraction. There were 102 SARS-CoV-2-positive samples and 312 SARS-CoV-2-negative samples among the 414 clinical samples analyzed using the LabTurboTM AIO COVID-19 RNA testing kit, demonstrating 100% correlation with the results obtained using the WHO-recommended RT-PCR assay. The Ct values for these two assays were highly correlated when the Rotor-Gene-Q real-time PCR instrument (LabTurboTM-N1 versus WHO-RdRp target, R2 = 0.9407; LabTurboTM-E versus WHO-E target, R2 = 0.9778) (Figure 1A and B; Table S1), and the Roche LightCycler®96 instrument (LabTurboTM-N1 versus WHO-RdRp target, R2 = 0.9401; LabTurboTM-E versus WHO-E target, R2 = 0.9725) (Figure 1C and D; Table S2) were used.
SARS-CoV-2 VOC Screening Test Using VirSNiP Probe-Based Melting Curve Assay
We further analyzed the 102 SARS-CoV-2-positive samples in our study. Ninety-four of the 102 positive samples were identified as SARS-CoV-2 B.1.1.7 variants with the spike mutations N501Y and del H69/V70, while the remaining samples were three SARS-CoV-2 B.1.351 (Beta variant) variants with spike mutations N501Y, E484K, and K417N, and five B.1.617 (Delta variant) variants with spike mutations P681R and L452R (Supplementary Tables S1 and S2).
Discussion
As of October 24, 2021, over 243 million cases of COVID-19 have been confirmed worldwide, with a death toll surpassing 4 million people.19 Various detection assays for SARS-CoV-2 have been developed since the pandemic began. RT-qPCR is currently being used as a reliable method for detecting symptomatic and asymptomatic patients infected with SARS-CoV-2.
Given the rapid spread of SARS-CoV-2 VOC worldwide, reliable, early, and accurate diagnosis is crucial to detect these variants. Although whole-genome sequencing is a standard method to detect the variants, it has limited accessibility and requires sophisticated infrastructure and trained personnel.20 Currently, the rapid spread of SARS-CoV-2 variants poses a significant public health challenge. A rapid molecular method to screen for SARS-CoV-2 VOC is necessary. A SARS-CoV-2 RT-PCR with additional VirSNiP probe-based melting curve assay for SARS-CoV-2 variants is a feasible, rapid, and efficient screening strategy that can be implemented in laboratories to perform VOC testing on SARS-CoV-2-positive samples. We observed an increase in the proportion of UK B.1.1.7 variant over time, which became the dominant variant, as well as the concurrent emergence of the ZA B.1.351 and Indian B.1.617 variants.
Some studies have reported that regular single-plex RT-PCR cannot reliably detect SARS-CoV-2 variants, resulting in decreased sensitivity and the specificity of SARS-CoV-2 detection. Moreover, instances of N dropout or Ct value shift have been reported in association with the assay, especially with the B.1.1.7 lineage.14 Multiplex PCR can increase the sensitivity and the specificity of SARS-CoV-2 variant detection and its dual or triple target approach can mitigate the risk of loss of sensitivity.
During the earlier stages of the COVID-19 outbreak, the sets of RT-qPCR primers and probes were publicly available and were used by several laboratories worldwide (Table 1). Assays performed using these sets used identical fluorescent reporters as probes. They also required each target gene to be assayed separately, leading to high reagent consumption and low production capacity when analyzing samples using 96-well plates. The LabTurboTM AIO COVID-19 RNA testing kit used in this study employs a single-reaction triplex assay for SARS-CoV-2 detection. The advantages of using a multiplex qRT-PCR assay are its high capacity in a single test run, effective and efficient detection, decreased reagent consumption, and short test duration. The LOD of the LabTurboTM AIO COVID-19 RNA testing kit for N1 and E was 9.4 copies per reaction, which is consistent with previously reported studies showing an LOD of < 10 copies per reaction.21 In the present study, the clinical performance of the LabTurboTM AIO COVID-19 RNA testing kit was comparable with that of the WHO-recommended RT-PCR assay for SARS-CoV-2 performed previously on the same samples and further confirmed by the Taiwan CDC Central Laboratory with 100% agreement for both positive and negative results. High correlation values (LabTurboTM versus WHO gene target) were obtained for both N1/RdRp (R2 = 0.9407) and E (R2 = 0.9778) using a Rotor-Gene-Q real-time PCR instrument and similar values were obtained for both N1/RdRp (R2 = 0.9401) and E (R2 = 0.9725) using a Roche LightCycler® 96, showing high levels of specificity associated with the LabTurboTM AIO COVID-19 RNA testing kit. Moreover, in the present study, N1 detection was more sensitive with the LabTurboTM AIO COVID-19 RNA testing kit than with the CDC test.13 Several commercial assays have been released, including the Cepheid Xpert Xpress SARS-CoV-2 (Cepheid, Sunnyvale, CA), DiaSorin Simplexa (Saluggia, Italy), and Cobas 6800 (Roche Diagnostics, Indianapolis, IN), with high sensitivity and short testing times. However, all of these assays require unique instruments.
Conclusions
Multiplex qRT-PCR is a critical tool for detecting unknown pathogens and allows multiple target gene detection. The LabTurboTM AIO COVID-19 RNA testing kit provides an effective and efficient method for SARS-CoV-2 detection and is highly compatible with SARS-CoV-2 variants.
Abbreviations
COVID-19, coronavirus disease 2019; LOD, the limit of detection; RT-PCR, reverse transcriptase-polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; VOC, variant of concern; WHO, World Health Organization; CDC, Centers for Disease Control.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of Tri-Service General Hospital (TSGHIRB No.: C202005041), registered in March 2021.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. This study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Tri-Service General Hospital, Taipei, Taiwan, ROC, (grant number TSGH-D-111086). The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Disclosure
The authors declare no conflict of interest.
References
1. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi:10.1056/NEJMoa2001316
2. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi:10.1056/NEJMoa2001017
3. World Health Organisation. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committe Regarding the Outbreak of Novel Coronavirus (2019-nCoV); 2020. Available from:https://www.who.int/news/item/01-08-2020-statement-on-the-fourth-meeting-of-the-interNational-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-coronavirus-disease-(covid-19).
4. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi:10.1056/NEJMoa2002032
5. Pourrajab F, Zare-Khormizi MR, Sheikhha MH. Molecular basis for pathogenicity of human coronaviruses. Infect Drug Resist. 2020;13:2385–2405. doi:10.2147/IDR.S255156
6. Sabino EC, Buss LF, Carvalho MPS, et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet. 2021;397:452–455. doi:10.1016/S0140-6736(21)00183-5
7. Munoz M, Patino LH, Ballesteros N, Paniz-Mondolfi A, Ramirez JD. Characterizing SARS-CoV-2 genome diversity circulating in South American countries: signatures of potentially emergent lineages? Int J Infect Dis. 2021;105:329–332. doi:10.1016/j.ijid.2021.02.073
8. Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. 2021;372. doi:10.1126/science.abg3055
9. Kruttgen A, Cornelissen CG, Dreher M, Hornef MW, Imohl M, Kleines M. Comparison of the SARS-CoV-2 rapid antigen test to the real star Sars-CoV-2 RT PCR kit. J Virol Methods. 2020;288:114024. doi:10.1016/j.jviromet.2020.114024
10. Nalla AK, Casto AM, Huang MW, et al. Comparative performance of SARS-CoV-2 detection assays using seven different primer-probe sets and one assay kit. J Clin Microbiol. 2020;58. doi:10.1128/JCM.00557-20
11. Green DA, Zucker J, Westblade LF, et al. Clinical performance of SARS-CoV-2 molecular tests. J Clin Microbiol. 2020;58. doi:10.1128/JCM.00995-20
12. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25. doi:10.2807/1560-7917.ES.2020.25.3.2000045
13. Centers for disease control and prevention. 2019-novel coronavirus (2019-nCoV) real-time rRT-PCR panel primers and probes; 2020. Available from:https://www.cdc.gov/coronavirus/2019-ncov/downloads/rt-pcr-panel-primer-probes.pdf.
14. Wollschlager P, Todt D, Gerlitz N, et al. SARS-CoV-2 N gene dropout and N gene Ct value shift as indicator for the presence of B.1.1.7 lineage in a commercial multiplex PCR assay. Clin Microbiol Infect. 2021;27:
15. Penarrubia L, Ruiz M, Porco R, et al. Multiple assays in a real-time RT-PCR SARS-CoV-2 panel can mitigate the risk of loss of sensitivity by new genomic variants during the COVID-19 outbreak. Int J Infect Dis. 2020;97:225–229. doi:10.1016/j.ijid.2020.06.027
16. Lippi G, Simundic AM, Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19). Clin Chem Lab Med. 2020;58:1070–1076. doi:10.1515/cclm-2020-0285
17. Jian MJ, Chung HY, Chang CK, et al. Clinical comparison of three sample-to-answer systems for detecting SARS-CoV-2 in B.1.1.7 lineage emergence. Infect Drug Resist. 2021;14:3255–3261. doi:10.2147/IDR.S328327
18. Jian MJ, Chung HY, Chang CK, et al. Novel automated sample-to-result SARS-CoV-2 laboratory-developed RT-PCR assay for high-throughput testing using LabTurbo AIO 48 system. Clin Chim Acta. 2020;514:54–58. doi:10.1016/j.cca.2020.12.003
19. World Health Organization. Coronavirus disease (COVID-19) epidemiological update; 2021. Available from: https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19—25-october-2021.
20. Neopane P, Nypaver J, Shrestha R, Beqaj SS. SARS-CoV-2 variants detection using TaqMan SARS-CoV-2 mutation panel molecular genotyping assays. Infect Drug Resist. 2021;14:4471–4479. doi:10.2147/IDR.S335583
21. Chu DKW, Pan Y, Cheng SMS, et al. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin Chem. 2020;66:549–555. doi:10.1093/clinchem/hvaa029
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.