Back to Journals » Vascular Health and Risk Management » Volume 19
Clinical Characteristics, Patterns of Use, and incidence of Adverse Events in Patients With Nonvalvular Atrial Fibrillation Treated With Oral Anticoagulants in Colombia
Authors Machado-Duque ME , Gaviria-Mendoza A , Reyes JM, Mesa A, Castaño-Gamboa N, Valladales-Restrepo LF , Machado-Alba JE
Received 8 October 2022
Accepted for publication 27 February 2023
Published 27 March 2023 Volume 2023:19 Pages 157—167
DOI https://doi.org/10.2147/VHRM.S391549
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Daniel Duprez
Manuel E Machado-Duque,1,2 Andrés Gaviria-Mendoza,1,2 Juan Manuel Reyes,3 Alejandro Mesa,3 Natalia Castaño-Gamboa,3 Luis Fernando Valladales-Restrepo,1,2 Jorge Enrique Machado-Alba1
1Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira-Audifarma S.A, Pereira, Colombia; 2Grupo de Investigación en Biomedicina, Fundación Universitaria Autónoma de las Américas, Pereira, Colombia; 3Pfizer Colombia, Bogotá, Colombia
Correspondence: Jorge Enrique Machado-Alba, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira-Audifarma S.A, Calle 105 No. 14-140, Pereira, Risaralda, 660003, Colombia, Tel +57 3108326970, Fax +57 63137822, Email [email protected]
Purpose: The aim was to analyze the characteristics, treatment patterns, and clinical outcomes of Colombian patients with non-valvular atrial fibrillation (NVAF) under treatment with oral anticoagulants (OAs).
Patients and Methods: Retrospective cohort in patients with NVAF identified from a drug dispensing database, aged ≥ 18 years, with first prescription of an OA (index) between January/2013 and June/2018, and a follow-up until June/2019. Data from the clinical history, pharmacological variables, and outcomes were searched. International Classification of Diseases-10 codes were used to identify the patient sample and outcomes. Patients were followed until a general composite outcome of effectiveness (thrombotic events), bleeding/safety or persistence (switch/discontinuation of anticoagulant) events. Descriptive and multivariate analyzes (Cox regressions comparing warfarin and direct oral anticoagulants-DOACs) were carried out.
Results: A total of 2076 patients with NVAF were included. The 57.0% of patients were women and the mean age was 73.3± 10.4 years. Patients were followed for a mean of 2.3± 1.6 years. 8.7% received warfarin before the index date. The most frequent OA was rivaroxaban (n=950; 45.8%), followed by warfarin (n=459; 22.1%) and apixaban (n=405; 19.5%). Hypertension was present in 87.5% and diabetes mellitus in 22.6%. The mean CHA2DS2-VASc Score was 3.6± 1.5. The 71.0% (n=326/459) of the warfarin patients presented the general composite outcome, and 24.6% of those with DOACs (n=397/1617). The main effectiveness and safety outcomes were stroke (3.1%) and gastrointestinal bleeding (2.0%) respectively. There were no significant differences between patients with warfarin and DOACs regarding thrombotic events (HR: 1.28; 95% CI: 0.68– 2.42), but warfarin was associated with higher bleeding/safety events (HR: 4.29; 95% CI: 2.82– 6.52) and persistence events (HR: 4.51; 95% CI: 3.81 − 5.33).
Conclusion: The patients with NVAF in this study were mainly older adults with multiple comorbidities. Compared to warfarin, DOACs were found to be equally effective, but safer and had a lower probability of discontinuation or switch.
Keywords: anticoagulation, direct oral anticoagulant, non-valvular atrial fibrillation, warfarin, real-world study, pharmacoepidemiology
Introduction
Non-valvular atrial fibrillation (NVAF) is an acute or chronic heart disorder associated with an increase in the mortality rate, strokes and other thromboembolic events.1 This is further increased by individual conditions of patients, such as hypertension, abnormal renal or hepatic function, stroke, history of or predisposition to bleeding, people over 65, among others.2
One of the standard treatments for prevention of stroke or systemic embolism in these patients is usually vitamin K antagonists (VKA, eg warfarin); in the analysis of net clinical benefits of this therapy it is suggested that the effect of VKA is even more favorable in patients with a high score on the HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile International Normalized Ratio, elderly, drugs/alcohol concomitantly) scale, compared to acetylsalicylic acid.3 Another therapeutic alternative is the direct oral anticoagulants (DOAC) ─ dabigatran, rivaroxaban and apixaban ─, which according to evidence have advantages in efficacy and safety compared to warfarin4 and even when the risk of bleeding and stroke are high, the net clinical benefit appears to be more significant when compared to warfarin.5 Likewise, there is a lower prevalence of intracranial hemorrhage and its different subtypes in patients being treated with new oral anticoagulants when compared to warfarin.6,7
While several studies seek to understand the characteristics of patients who were diagnosed with NVAF under different treatment options, and even subpopulation analyses, the evidence at the national level is limited in Colombia, both in demographic and clinical characteristics and in treatment patterns of this population. In a retrospective descriptive study of an emergency department in a third level care center in Bogota, it was observed that the main comorbidities of patients with atrial fibrillation (AF) were arterial hypertension and heart failure, where most patients do not receive anticoagulation.8 In turn, for the overall population it is estimated that the prevalence of AF in Colombia (4.8%) seems to be higher than that reported in developed countries (0.03% to 1.25%),9 according to a study conducted in a university hospital in Colombia.10
The Colombian health system offers universal coverage for the entire population through two regimes, one contributory, or paid by the worker and his employer, and another subsidized by the state for those without the ability to pay, which has a benefit plan that includes warfarin and the different DOACs. Considering the limited knowledge about the use of oral anticoagulants in patients diagnosed with NVAF in Colombia and the differences in response to these therapies in different subpopulations, the study aimed to determine the demographic and clinical characteristics treatment patterns, and incidence of events (discontinuation, persistence, primary clinical outcomes such as major and minor bleeding) in a group of patients with NVAF who started oral anticoagulants in a population from Colombia.
Materials and Methods
An observational study of a retrospective cohort of adult patients diagnosed with NVAF was carried out in a health insurer in Colombia who was identified from the drug dispensing database of Audifarma SA (drug logistics operator).
This database, which started in 2006, contains patient information for 9.5 million people affiliated to the Colombian healthcare system (including both contributory and subsidized regimes). It includes ambulatory or hospital variables regarding sociodemographic characteristics of the patients, as well as drug information (drug claim date, name, dose, quantity, etc) and the related International Classification of Diseases, version 10.0 (ICD-10) codes. We included only information regarding one healthcare insurer, which comprises 3.4 million patients, because the additional clinical records of these patients are also available for research and contained the rest of the variables necessary to conduct the study. This database has been validated in other studies on medication use in the Colombian population.8,11
Included were patients older than 18 years of either sex with the first prescription of a DOAC (apixaban, dabigatran, or rivaroxaban) or warfarin between January 1, 2013 and June 30, 2018, who underwent a minimum follow-up of 1 year. Data collection stopped on December 31, 2019. The patients had to have a diagnosis of NVAF according to the ICD-10 code (ICD-10: I48) previously or on the index date, defined as the date of the first dispensation of the treatment. The patient also had to be active in the Colombian health system for the six months before this date (reference period). Patients with a diagnosis of heart valve disease or valve replacement were excluded (ICD-10: I05, I06, I07, I08, I09, I21, I22, I34, I35, I700, I702-I709; Q22, Q23, Q25, T82), as were those who were pregnant during the study period (ICD-10: O00-O9) and those who had a diagnosis of venous thromboembolism (VTE) (ICD-10: I80-I82).
In this way, cohorts were constructed for the follow-up of patients separately with each DOAC or warfarin. A group of physicians trained by the researchers in the development of the research protocol reviewed the clinical records of each patient included and recorded the patient’s data. The variables identified in each patient were the following:
Variables at Index Date
- Sociodemographic: age, sex, ethnicity, weight (kilograms), body mass index, place of residence.
- Clinical: date of diagnosis of NVAF, diabetes mellitus, liver disease, hypertension, rheumatological disease, kidney disease, congestive heart failure, acute myocardial infarction, chronic obstructive pulmonary disease, peripheral vascular disease, dementia, hemiplegia, leukemia, malignant lymphoma, peptic ulcer disease, history of stroke, anemia, tobacco use, gastrointestinal bleeding, intracranial bleeding, other bleeding. The HAS-BLED score, CHA2DS2-VASc score, and the Charlson comorbidity index were also calculated.
- Concomitant therapies: previous use of acetylsalicylic acid, P2Y12 inhibitors, or nonsteroidal anti-inflammatory drugs (NSAIDs); use of concomitant treatments for the treatment of comorbidities.
Treatment Variables
Treatment variables were assessed both at index and during follow-up. Oral anticoagulant started, initial dose, frequency of use, date of initiation, previous use of warfarin. Reduced doses were classified as apixaban 5 mg/day, rivaroxaban 15 mg/day, and dabigatran 220 mg/day. The relationship between the mean dose and the defined daily dose (ratio of DDD) was established. Polypharmacy was defined by the concomitant use of five or more medications.
Outcomes
Several outcomes were identified during follow-up: i) Effectiveness composite outcome of thrombotic events (ischemic stroke, systemic embolism), ii) Bleeding/safety composite outcome (gastrointestinal bleeding, hemorrhagic cerebrovascular event, another major bleeding, death associated with adverse event), iii) Persistence composite outcome of anticoagulant use (switch or discontinuation of anticoagulant). The follow-up was stopped at the time of first appearance of any of these outcomes.
Death associated with adverse event was considered in those patients who died as consequence of safety outcomes and was evaluated directly in the clinical records, not in the database. Persistence was defined as time under oral anticoagulant therapy. Discontinuation occurred when there was no evidence of a new anticoagulant prescription for 60 days since the last dispensation. Both outcomes were identified by date.
The general composite outcome that included any of the previous three outcomes (effectiveness, bleeding/safety or persistence) was also calculated. A clinical outcome was defined as a composite of effectiveness or bleeding/safety outcomes. Supplementary Table 1 presents the ICD-10 codes for the outcomes.
Statistical Analysis
This study was designed and conducted with a descriptive perspective. All the comparisons and analytical results should be considered in an exploratory manner. For the data analysis, the Statistical Package for the Social Sciences (SPSS), version 28.0 (IBM, USA) for Windows, was used. Continuous variables are presented as the means with standard deviations or other measures of central tendency or position, while categorical variables are presented as frequencies and percentages. The incidence rate for the general composite outcome was calculated in person-years. The cumulative incidence of the outcomes was calculated and presented as frequencies. Survival curves for the clinical outcome were derived using the Kaplan‒Meier method. Cox regression analysis were performed for clinical, persistence, effectiveness and bleeding/safety outcomes, comparing warfarin and DOACs. Variables with biological plausibility to affect the outcome were included as covariates in the multivariate analyses, such as age and sex, as well as those variables that were significantly associated with the outcome in the bivariate analyses (Chi-squared tests). A sub-analysis through an adjusted Cox proportional-hazards regression looked for differences in effectiveness outcomes and bleeding/safety issues between patients receiving reduced versus recommended doses of DOACs.
Bioethical Considerations
The study was approved by the Bioethics Committee of the Universidad Tecnológica de Pereira in the category of research without risk (Approval code: 02122019). The ethical principles established by the Declaration of Helsinki were respected. Risk-free investigations that collect data from clinical records do not require informed consent according to Resolution 8430 of 1993 of the Colombian Ministry of Health. The principles of confidentiality of the information were respected.
Results
A total of 2076 patients were identified with NVAF who met the inclusion criteria (Supplementary Figure 1). A total of 57.0% were women. The mean age was 73.3 years (range: 26.0–101.0 years), and 79.9% (n = 1659) were 65 years or older. The most prevalent ethnic group was the mestizos (n = 1752; 84.4%). The main city of residence was Bogotá (n = 445; 21.4%). The most common comorbidities were arterial hypertension, chronic kidney disease, diabetes mellitus, and a history of acute myocardial infarction. Table 1 shows the sociodemographic variables, the mean CHA2DS2-VASc and HAS-BLED scores, the other comorbidities, and the related antecedents of the whole patient population and of each treatment group of treatments. A total of 288 subjects (13.8%) had a diagnosis of NVAF before January 2013. The mean follow-up of all patients was 2.3 ± 1.6 years (27.6 ± 19.2 months).
 |
Table 1 Baseline Demographic and Clinical Characteristics of Non-Valvular Atrial Fibrillation Group of Patients from Colombia |
At the index time, in order of frequency of use, the oral anticoagulants were rivaroxaban (45.8%), warfarin (22.1%), apixaban (19.5%), and dabigatran (12.6%) (Table 1). A total of 181 (11.2%) patients received warfarin before the index date on which they began to receive dabigatran (n = 42; 16.0%), rivaroxaban (n = 125; 13.2%), and apixaban (n. = 14; 3.5%). The most common dosage of rivaroxaban was 20 mg (n = 563; 59.3%), for warfarin 5 mg (n = 381; 83.0%), apixaban 5 mg (n = 240; 59.3%), and dabigatran 110 mg (n = 165; 63.0%). The mean weekly dose of warfarin was 29.3 ± 10.1 mg. Table 2 shows the patterns of use of these treatments with the dose, ratio of DDD, clinical characteristics of the patients, use of concomitant treatments, and cases of polypharmacy. Supplementary Table 2 shows the frequencies of use of each DOAC at different dosages and Supplementary Table 3 the HAS-BLED Score by dosage strengths.
 |
Table 2 Treatment Patterns of Non-Valvular Atrial Fibrillation Group of Patients from Colombia |
It was identified that 39.6% of rivaroxaban patients used the drug at reduced doses, as did 41.7% of apixaban and 60.3% of dabigatran (Table 2). Among patients with reduced doses, it was evidenced that 193 (51.6%) of those with rivaroxaban, 135 (79.8%) apixaban, and 97 (61.4%) dabigatran showed concordance between the dose they were taking and the clinical indication for its use.
On average, patients took 6.1 drugs at the beginning of treatment, including anticoagulants. The most frequent concomitant treatments were β-blockers, statins, angiotensin-2 receptor antagonists, furosemide, angiotensin-converting enzyme inhibitors (ACEi), and proton pump inhibitors. Table 2 shows the concomitant treatments in patients of each group of treatments under study.
Outcomes and Follow-Up
Patients were followed up until the appearance of any variable of the general composite outcome, such as an ischemic cerebrovascular event, bleeding/safety event, or switch or discontinuation of the anticoagulant. A total of 71.0% (n = 326/459) of the warfarin patients presented the general composite outcome during follow-up, and 24.6% of those with DOACs (n = 397/1617). Overall, participants were followed for 4787.1 person-years. The incidence rate of the general composite outcome was 15.10 per 100 person-years (95% CI: 14.02–16.25); 40.19 per 100 person-years (95% CI: 35.94–44.79) in the group of warfarin and 9.99 per 100 person-years (95% CI: 9.03–11.02) in the group of DOACs.
The most frequent switches and treatment discontinuation were in patients with warfarin. The main effectiveness and safety outcomes were stroke (3.1%) and gastrointestinal bleeding (2.0%) respectively. Table 3 shows the data of the outcomes and the variables that composed it. Regarding chronic kidney disease, it was present in 57.1% (n=52) of those with the bleeding/safety composite outcome and in 44.3% (n=879) of those without this outcome.
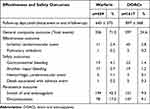 |
Table 3 Effectiveness and Safety Outcomes of Non-Valvular Atrial Fibrillation Group of Patients from Colombia |
When making the comparison by a Cox proportional-hazards regression adjusted for sex, age, use of ACEi, angiotensin receptor 2 antagonists, β-blockers, antiarrhythmics, statins, and Charlson comorbidity index, it became evident that there was a greater probability of presenting a clinical outcome (effectiveness or bleeding/safety outcomes) in warfarin patients than DOACs patients (adjusted hazard ratio (HRa): 2.79; 95% CI: 1.99–3.91; p<0.001). In a similar comparison a greater probability of switch or discontinuation (persistence outcome) was found in warfarin patients compared with DOAC patients (HRa: 4.51; 95% CI: 3.81 −5.33; p<0.001). Figure 1 shows the Kaplan‒Meier analysis of time to clinical outcome.
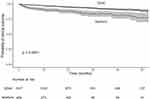 |
Figure 1 Kaplan Meier of non-valvular atrial fibrillation group of patients from Colombia by treatment type. |
An analysis was performed for the specific effectiveness outcome of thrombosis through adjusted Cox proportional-hazards regression, which found that there were no significant differences between patients with warfarin and DOACs (HRa: 1.28; 95% CI: 0.68–2.42; p = 0.447). Comparing the components of the bleeding/safety outcome, it was found that warfarin patients had a higher risk of presenting them (HRa: 4.29; 95% CI: 2.82–6.52; p<0.001) (Supplementary Figure 2).
The sub-analysis that compared patients who used DOACs at recommended doses versus those prescribed at reduced doses, through an adjusted Cox proportional-hazards regression, found that there were no significant differences in the specific outcome of thrombotic events (HRa: 1.31; 95% CI: 0.69–2.49; p = 0.417). The same type of analysis adjusted for sex, age, use of ACEi, angiotensin receptor 2 antagonists, β-blockers, antiarrhythmics, statins, HAS-BLED score, and Charlson comorbidity index identified a greater probability of bleeding in reduced-dose patients than normal-dose patients of DOACs (HRa: 2.29; 95% CI: 1.17–4.48; p = 0.001).
Discussion
The present study describes the clinical characteristics, treatment patterns, and effectiveness and safety outcomes of a large cohort of patients with NVAF under management with oral anticoagulants. This real-world evidence may be useful for treating physicians and others responsible for these patients’ care in that it could facilitate the choice of treatment and to identify expected and undesired effects during follow up, given the significant risk of bleeding to which they are exposed.
The clinical characteristics of the patients included were consistent with the data previously described in Colombia for patients with AF using oral anticoagulants, with a similar proportion of women (52%) and an average age close to 70 years,8,12 and were also consistent with studies carried out in the United States, Italy, Japan, Pakistan, and Turkey.13–17 The average CHA2DS2-VASc score of 3.6 points for this population was similar to that reported by Medina-Morales et al in Colombia,12 Brown et al in the United States,14 and Gedikly in Turkey,16 but higher than that reported in Pakistan (1.6 points),17 which can be explained by the inclusion criteria used in the different studies, the heterogeneity of the populations, or even the use of pharmacological therapies at different times of the evolution of the disease.
The high Charlson comorbidity index (4.95) identified in this analysis, added to the diagnosis of NVAF and its treatment with oral anticoagulants, is evidence of the increased risk of suffering an adverse bleeding-type outcome that these patients had.18,19 This is mainly because some of the most common comorbidities were arterial hypertension, chronic kidney disease, diabetes mellitus, ischemic heart disease, and chronic obstructive pulmonary disease, which confer additional risks and are conditions consistent with other published studies.6,12,20 The management of anticoagulant therapy in patients with chronic kidney disease is of particular interest since in this report, the prevalence exceeded 40% of cases, which together with age put them at high risk of adverse outcomes, since these drugs are recommended only in subjects with glomerular filtration rates greater than 30 mL/min and creatinine less than 2.5 mg/dL.21 Although the evidence shows that, due to certain anti-inflammatory properties, vascular protection, and the greater efficacy and safety of DOACs compared to warfarin, they would be better recommended in this particular group of patients.22–24
The average prescription of 6.1 treatments per patient, including the oral anticoagulant, means that almost 70% of them had polypharmacy,25 a situation that puts them at significant risk of a higher incidence of general adverse reactions, drug‒drug interactions, and therapeutic duplications,26 added to the use of treatments that increase the risk of falls or delirium in older adults (such as benzodiazepines, antihistamines, and opioids).27,28 More than 20% of patients were prescribed with acetylsalicylic acid or a P2Y12 inhibitor along with the oral anticoagulant, a combination that increases their risk of suffering major bleeding.17 This situation was previously described in observational studies with real-life data, where patients with NVAF treated with DOACs with polypharmacy had a lower risk of stroke and embolism than those with warfarin.5
More than 30% of the subjects included in this study were 80 or older, a determining factor of the prescriber’s approach to treating the patient with NVAF. In adults older than this age who have AF, there is an increased risk of death, stroke/embolism, and major bleeding; however, studies such as that of Lip et al describe a significant reduction in these events in patients treated with oral anticoagulants, even at advanced age.29 The high frequency (> 40%) of the use of oral anticoagulants in reduced doses, without defined indications in the clinical records for this dosage regimen, highlights the possible fear of physicians of prescribing this therapeutic group.30,31 The increased risk of bleeding in patients who received reduced doses of DOACs without altering the effectiveness to prevent thrombotic events is contrary to that reported in Japan and the meta-analysis published by Zhang et al,32,33 which can be explained by the selection process of DOAC patients in Colombia, the frequency of comorbidities, their severity, the number of other drugs they are receiving, and some possible unidentified or measured factors that may be determinants of risk of bleeding and the reason why the treating physician decided to use reduced doses of the drug.
The higher frequency of DOACs, in particular rivaroxaban, in this report is consistent with other studies of patients in Colombia that have shown that they have moved past warfarin in the management of NVAF;8 in addition, they have shown persistence of continuous use of more than one year, similar to records from Spain,20 the Netherlands,34 and the United Kingdom.35 Warfarin patients switched to another anticoagulant in more than 40% of cases, compared to only 9% of those with DOACs. The former also discontinued treatment much more frequently. These data highlight the preferences of prescribers and patients in the search for effective but safer treatments.14,36,37
The most relevant finding of this research is related to the identification with real-world evidence of an increased risk of bleeding in the gastrointestinal tract, the central nervous system, and other major bleeding in warfarin patients compared to DOACs, despite having the same probability of suffering thrombotic events, such as ischemic strokes or pulmonary thromboembolism and death associated with adverse drug reactions, a situation consistent with other publications of observational studies and controlled clinical trials.16,38,39 This is in addition to the reports that show the advantages of this relatively new group of drugs in terms of their safety profile, with a predictable bioavailability, fewer drug‒drug interactions, and ease of dosing and adjustments, due to a lower variability in metabolism and the advantage of not requiring periodic laboratory controls such as measuring the international normalized ratio.40
This study has some limitations, which include its observational nature; the censoring of the follow-up of patients between 21 and 30 months, which prevented the identification of longer-term outcomes of interest; the inability to identify the causes and reasons for the discontinuation or changes of therapy; and the reason for initial selection of each of the prescribed anticoagulants, despite the rigorous search for information in each of the clinical records. It has certain strengths, such as the large sample, the adequate selection of research subjects based on the inclusion and exclusion criteria, and the magnitude of data collected on clinical and follow-up outcomes.
Conclusions
Patients under treatment for NVAF in Colombia are mainly women, older than 79 years, with significant comorbidities, especially arterial hypertension and chronic kidney disease, polypharmacy, and increasingly managed with DOACs instead of warfarin. DOACs have been found to be equally effective, but safer in terms of the risk of major bleeding and also have a lower probability of discontinuation and switch over the first 30 months. These results provide useful real-world evidence for clinicians and decision-makers in charge of patients requiring anticoagulant therapy, particularly those with NVAF.
Data Sharing Statement
protocols.io. Access availability from DOI: dx.doi.org/10.17504/protocols.io.rm7vzb852vx1/v1.
Acknowledgments
This manuscript was submitted for participation in ISPOR Europe and accepted. Only the abstract was published in Value in Health. 2022.25(7):S590.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study (B1801420) received funding from Pfizer Colombia.
Disclosure
Reyes JM, Castaño-Gamboa N, and Mesa A are employees of Pfizer. Pfizer did not participate in the management or data analysis of the study information. Gaviria-Mendoza A, Machado-Duque ME, Valladales-Restrepo L, and Machado-Alba JE have developed studies funded by GSK, Pfizer, Biotoscana, Sanofi, Sanofi-Pasteur, Abbot, Tecnoquímicas, Bayer, and Novartis. Machado-Duque ME and Machado-Alba JE also report grants from Pfizer, during the conduct of the study. Gaviria-Mendoza A also reports grants from Audifarma, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Molteni M, Polo Friz H, Primitz L, et al. The definition of valvular and non-valvular atrial fibrillation: results of a physicians’ survey. Europace. 2014;16(12):1720–1725.
2. Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi:10.1378/chest.09-1584
3. Olesen JB, Lip GY, Lindhardsen J, et al. Risks of thromboembolism and bleeding with thromboprophylaxis in patients with atrial fibrillation: a net clinical benefit analysis using a ‘real world’ nationwide cohort study. Thromb Haemost. 2011;106(4):739–749. doi:10.1160/TH11-05-0364
4. Banerjee A, Lane DA, Torp-Pedersen C, et al. Net clinical benefit of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus no treatment in a ‘real world’ atrial fibrillation population: a modelling analysis based on a nationwide cohort study. Thromb Haemost. 2012;107(3):584–589. doi:10.1160/TH11-11-0784
5. Lip GYH, Keshishian A, Kang A, et al. Effectiveness and safety of oral anticoagulants among non-valvular atrial fibrillation patients with polypharmacy. Eur Heart J Cardiovasc Pharmacother. 2021;7(5):405–414. doi:10.1093/ehjcvp/pvaa117
6. Pinto DA, Sánchez-Vallejo CA, Pedraza AL, et al. Description of patients with non-valvular atrial fibrillation admitted to the emergency room. Rev Colomb Cardiol. 2016;23(4):270–276.
7. Archontakis-Barakakis P, Li W, Kalaitzoglou D, et al. Effectiveness and safety of intracranial events associated with the use of direct oral anticoagulants for atrial fibrillation: a systematic review and meta-analysis of 92 studies. Br J Clin Pharmacol. 2022;88(11):4663–4675. doi:10.1111/bcp.15464
8. Machado-Alba JE, Gaviria-Mendoza A, Machado-Duque ME, et al. Use of non-vitamin K antagonist oral anticoagulants in Colombia: a descriptive study using a national administrative healthcare database. Pharmacoepidemiol Drug Saf. 2021;30(4):426–434. doi:10.1002/pds.5124
9. Nguyen TN, Hilmer SN, Cumming RG. Review of epidemiology and management of atrial fibrillation in developing countries. Int J Cardiol. 2013;167(6):2412–2420. doi:10.1016/j.ijcard.2013.01.184
10. Rosselli D, Rodríguez AJ, García ÁA, et al. Atrial fibrillation prevalence in a Colombian university hospital. Rev Colom Cardiol. 2013;20(6):383–385.
11. Franco JS, Vizcaya D. Availability of secondary healthcare data for conducting pharmacoepidemiology studies in Colombia: a systematic review. Pharmacol Res Perspect. 2020;8(5):e00661. doi:10.1002/prp2.661
12. Medina-Morales DA, Machado-Duque ME, Gaviria-Mendoza A, et al. Clinical characteristics and stratification of the cerebrovascular accident risk among patients with atrial fibrillation in Colombia, 2011–2016. Expert Rev Cardiovasc Ther. 2021;19(2):181–187. doi:10.1080/14779072.2021.1873766
13. Sakuma I, Uchiyama S, Atarashi H, et al. Clinical risk factors of stroke and major bleeding in patients with non-valvular atrial fibrillation under rivaroxaban: the EXPAND Study sub-analysis. Heart Vessels. 2019;34(11):1839–1851. doi:10.1007/s00380-019-01425-x
14. Brown JD, Shewale AR, Dherange P, et al. A comparison of oral anticoagulant use for atrial fibrillation in the pre- and post-DOAC Eras. Drugs Aging. 2016;33(6):427–436. doi:10.1007/s40266-016-0369-y
15. Bodega F, Russi A, Melillo F, et al. INSigHT (Italian DOACs San Raffaele Hospital) registry investigators. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and extreme body weight. Eur J Clin Invest. 2022;52(1):e13658. doi:10.1111/eci.13658
16. Gedikli Ö, Altay S, Ünlü S, et al. Real-life data of major and minor bleeding events with direct oral anticoagulants in the one-year follow-up period: the NOAC-Turk study. Anatol J Cardiol. 2021;25(3):196–204. doi:10.5152/AnatolJCardiol.2021.57635
17. Almas T, Musheer A, Ejaz A, et al. Efficacy and safety of direct oral anticoagulants with and without Aspirin: a systematic review and Meta-analysis. Int J Cardiol Heart Vasc. 2022;40:101016. doi:10.1016/j.ijcha.2022.101016
18. van den Ham HA, Souverein PC, Klungel OH, et al. Major bleeding in users of direct oral anticoagulants in atrial fibrillation: a pooled analysis of results from multiple population-based cohort studies. Pharmacoepidemiol Drug Saf. 2021;30(10):1339–1352. doi:10.1002/pds.5317
19. Lobraico-Fernandez J, Baksh S, Nemec E. Elderly bleeding risk of direct oral anticoagulants in nonvalvular atrial fibrillation: a systematic review and meta-analysis of cohort studies. Drugs R D. 2019;19(3):235–245. doi:10.1007/s40268-019-0275-y
20. Giner-Soriano M, Cortes J, Gomez-Lumbreras A, et al. The use and adherence of oral anticoagulants in primary health care in catalunya, Spain: a real-world data cohort study. Aten Primaria. 2020;52(8):529–538. doi:10.1016/j.aprim.2020.05.016
21. Hindricks G, Potpara T, Dagres N, et al.; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
22. Rogula S, Gąsecka A, Mazurek T, et al. Safety and efficacy of DOACs in patients with advanced and end-stage renal disease. Int J Environ Res Public Health. 2022;19(3):1436. doi:10.3390/ijerph19031436
23. Ellinghaus P, Perzborn E, Hauenschild P, et al. Expression of pro-inflammatory genes in human endothelial cells: comparison of rivaroxaban and dabigatran. Thromb Res. 2016;142:44–51. doi:10.1016/j.thromres.2016.04.008
24. Ishibashi Y, Matsui T, Yamagishi S. Apixaban exerts anti-inflammatory effects in mesangial cells by blocking thrombin/protease-activated receptor-1 system. Thromb Res. 2014;134(6):1365–1367. doi:10.1016/j.thromres.2014.09.028
25. Machado-Alba JE, Machado-Duque ME, Gaviria-Mendoza A. Extreme polypharmacy: the need to mint a new term. Pharmacoepidemiol Drug Saf. 2020;29(2):224–225. doi:10.1002/pds.4942
26. Castro-Rodríguez A, Machado-Duque ME, Gaviria-Mendoza A, et al. Factors related to excessive polypharmacy (≥15 medications) in an outpatient population from Colombia. Int J Clin Pract;2018. e13278. doi:10.1111/ijcp.13278
27. Machado-Duque ME, Castaño-Montoya JP, Medina-Morales DA, et al. Drugs with anticholinergic potential and risk of falls with hip fracture in the elderly patients: a case-control study. J Geriatr Psychiatry Neurol. 2018;31(2):63–69. doi:10.1177/0891988718757370
28. Machado-Duque ME, Castaño-Montoya JP, Medina-Morales DA, et al. Association between the use of benzodiazepines and opioids with the risk of falls and Hip fractures in older adults. Int Psychogeriatr. 2018;30(7):941–946. doi:10.1017/S1041610217002745
29. Lip GY, Clementy N, Pericart L, et al. Stroke and major bleeding risk in elderly patients aged ≥75 years with atrial fibrillation: the Loire Valley atrial fibrillation project. Stroke. 2015;46(1):143–150. doi:10.1161/STROKEAHA.114.007199
30. Steinberg BA, Kim S, Thomas L, et al. Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) Investigators and Patients. Lack of concordance between empirical scores and physician assessments of stroke and bleeding risk in atrial fibrillation: results from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF) registry. Circulation. 2014;129(20):2005–2012. doi:10.1161/CIRCULATIONAHA.114.008643
31. Sanghai SR, Liu W, Wang W, et al. Prevalence of frailty and associations with oral anticoagulant prescribing in atrial fibrillation. J Gen Intern Med. 2022;37(4):730–736. doi:10.1007/s11606-021-06834-1
32. Sasaki S, Sotomi Y, Hirata A, et al. Comparison of low-dose direct oral anticoagulants for patients <80 Versus ≥80 years of age with atrial fibrillation. Am J Cardiol. 2022;162:86–91. doi:10.1016/j.amjcard.2021.09.019
33. Zhang XL, Zhang XW, Wang TY, et al. Off-label under- and overdosing of direct oral anticoagulants in patients with atrial fibrillation: a meta-analysis. Circ Cardiovasc Qual Outcomes. 2021;14(12):e007971. doi:10.1161/CIRCOUTCOMES.121.007971
34. Toorop MMA, Chen Q, Tichelaar VYIG, et al. Predictors, time course, and outcomes of persistence patterns in oral anticoagulation for non-valvular atrial fibrillation: a Dutch nationwide cohort study. Eur Heart J. 2021;42(40):4126–4137. doi:10.1093/eurheartj/ehab421
35. Banerjee A, Benedetto V, Gichuru P, et al. Adherence and persistence to direct oral anticoagulants in atrial fibrillation: a population-based study. Heart. 2020;106(2):119–126. doi:10.1136/heartjnl-2019-315307
36. Hadžibegović I, Jurin I, Letilović T, et al. Changes of recommended anticoagulation therapy in patients with atrial fibrillation and high thrombotic risk: long-term follow-up data from two hospital centers. Expert Rev Cardiovasc Ther. 2021;19(9):857–863. doi:10.1080/14779072.2021.1962293
37. Kirchmayer U, Narduzzi S, Mayer F, et al. Safety and effectiveness of direct oral anticoagulants versus vitamin K antagonists: results from 3 Italian regions. Recenti Prog Med. 2019;110(4):195–202. doi:10.1701/3154.31345
38. ROCKET AF Study Investigators. Rivaroxaban-once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation: rationale and design of the ROCKET AF study. Am Heart J. 2010;159(3):340–347.e1. doi:10.1016/j.ahj.2009.11.025
39. Bahit MC, Lopes RD, Wojdyla DM, et al. Apixaban in patients with atrial fibrillation and prior coronary artery disease: insights from the ARISTOTLE trial. Int J Cardiol. 2013;170(2):215–220. doi:10.1016/j.ijcard.2013.10.062
40. Carnicelli AP, Hong H, Connolly SJ, et al. COMBINE AF (A collaboration between multiple institutions to better investigate non-vitamin K antagonist oral anticoagulant use in atrial fibrillation) investigators. Direct oral anticoagulants versus warfarin in patients with atrial fibrillation: patient-level network meta-analyses of randomized clinical trials with interaction testing by age and sex. Circulation. 2022;145(4):242–255. doi:10.1161/CIRCULATIONAHA.121.056355
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Anticoagulation Management in Patients Receiving Warfarin at Private Cardiac Centers in Addis Ababa, Ethiopia
Getachew R, Tadesse TA, Shashu BA, Degu A, Alemkere G
Journal of Blood Medicine 2023, 14:107-117
Published Date: 10 February 2023
Effects of Anticoagulant Therapy and Frailty in the Elderly Patients with Atrial Fibrillation
Ding J, Sun Y, Zhang K, Huang W, Tang M, Zhang D, Xing Y
Clinical Interventions in Aging 2024, 19:247-254
Published Date: 14 February 2024
