Back to Journals » ClinicoEconomics and Outcomes Research » Volume 10
Clinical and economic impact of the 21-gene recurrence score assay in adjuvant therapy decision making in patients with early-stage breast cancer: pooled analysis in 4 Basque Country university hospitals
Authors Martínez del Prado P , Alvarez-López I, Domínguez-Fernández S, Plazaola A, Ibarrondo O, Galve-Calvo E, Ancizar-Lizarraga N, Gutierrez-Toribio M, Lahuerta-Martínez A, Mar J
Received 12 July 2017
Accepted for publication 6 December 2017
Published 19 March 2018 Volume 2018:10 Pages 189—199
DOI https://doi.org/10.2147/CEOR.S146095
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Purificación Martínez del Prado,1 Isabel Alvarez-López,2,3 Severina Domínguez-Fernández,4 Arrate Plazaola,5 Oliver Ibarrondo,6 Elena Galve-Calvo,1 Nerea Ancizar-Lizarraga,2,3 María Gutierrez-Toribio,4 Ainhara Lahuerta-Martínez,5 Javier Mar6,7
1Medical Oncology Service, Basurto University Hospital, Bilbao, Spain; 2Medical Oncology Service, Donostia University Hospital, Donostia-San Sebastián, Spain; 3Biodonostia Health Research Institute, Donostia-San Sebastián, Spain; 4Medical Oncology Service, Araba University Hospital, Vitoria-Gasteiz, Spain; 5Medical Oncology Service, Onkologikoa, Donostia-San Sebastián, Spain; 6AP-OSI Research Unit, Alto Deba Integrated Health Care Organization, Mondragon, Spain; 7Health Services Research on Chronic Patients Network, Kronikgune Group, Bilbao, Spain
Purpose: The 21-gene recurrence score (RS) is a genomic test developed as a prognostic and predictive tool to improve the treatment decision making in cases of estrogen receptor-positive and human epidermal growth factor receptor 2-negative early-stage breast cancer. This study examined the clinical and economic impact of its use in 4 Basque Country university hospitals.
Methods: Taking into consideration the RS result, we recorded the recommended initial systemic adjuvant therapy (endocrine therapy with or without chemotherapy) according to standard clinicopathologic factors and the final decision about chemotherapy. Then, if the RS was high, chemotherapy was recommended; it was not recommended if the RS was low; for those with an intermediate RS, clinicopathologic factors were considered, and the initial recommendation based on those factors was maintained. In addition, the probability of switching treatment was calculated. Then, we developed an economic evaluation by measuring the treatment’s incremental short-term budget impact from both the societal perspective and that of the Basque Health System. Patients’ characteristics and chemotherapy use were analyzed using logistic regressions and receiver operating characteristic curves.
Results: Without an RS, chemotherapy would have been prescribed to 56% of 401 patients, but, with RS use, that percentage decreased to 25. The overall rate of decision change was 35.4%. Test inclusion led to a reduction in chemotherapy costs of €922 per patient in the total population. Although this reduction did not entirely offset the cost of the test, the productivity loss per patient was reduced by €1,977.
Conclusion: The 21-gene RS test significantly changed the indication for chemotherapy. As chemotherapy treatments with no benefit were avoided, patients’ quality of life was improved. The short-term economic impact was negative for the Basque Health Service, but savings resulted when sick-leave costs were included.
Keywords: early-stage breast cancer, adjuvant chemotherapy, 21-gene assay, economic evaluation, health care costs
Introduction
The mainstay of adjuvant treatment in patients with estrogen receptor-positive (ER+) and human epidermal growth factor receptor 2-negative (HER2−) early-stage breast cancer (BC) is endocrine therapy. Chemotherapy is not recommended for all patients, because some have a more favorable prognosis and benefit less from chemotherapy. However, predictive models based only on clinical and histochemical features have not been shown to accurately identify which patients benefit from adjuvant chemotherapy.1 Thus, in recent years, genomic tests with a strong prognostic and predictive power have been developed.2
The 21-gene recurrence score (RS) for early-stage BC (Oncotype DX; Genomic Health, Redwood City, CA, USA) is based on a reverse transcriptase polymerase chain reaction assay of 5 reference genes and 16 cancer-related genes associated with cell proliferation, invasion, and hormone response.3 It became commercially available in 2004 and uses a continuous scale (from 0 to 100) to predict 10-year cancer recurrence risk and benefit of adjuvant chemotherapy in patients with early-stage ER+, lymph node-negative disease. That score is subdivided into 3 risk categories: low, intermediate, and high.3,4 Its impact on the decision-making process for adjuvant therapy in patients with ER+ and HER2− BC was addressed in different studies,4,5 which determined its inclusion in clinical guidelines.6–8 However, other experts, like those in the Evaluation of Genomic Applications in Practice and Prevention group, believe that there is no definitive evidence demonstrating the test’s utility as a predictive tool of the benefit of adjuvant chemotherapy.9 The Basque Health Service (Osakidetza) included the 21-gene RS test in its portfolio in September 2012, and its real-life application meant a possible change in the final treatment decision for patients needing evaluation.
The main objective of the study was to carry out an economic evaluation by measuring the assay’s incremental short-term budget impact. The second objective was to measure the probability of a treatment change due to the use of the 21-gene RS when compared to treatment based on the use of clinical criteria alone.
Methods
This study was an observational, prospective, multicenter study to assess the impact of Oncotype DX-RS test use on adjuvant chemotherapy decision making and was carried out in 4 hospitals within the Basque Health Service (Basurto, Donostia, Onkologikoa, and Araba hospitals) between September 1, 2012, and September 30, 2015.
Inclusion criteria were the following: 1) operable early-stage BC and adequate surgery performed for primary tumor; 2) ER+/HER2−; and 3) pathological TNM (TNM): pT1b, if at least 2 of the following 3 factors were present: histologic grade (G) III, Ki-67 ≥14% and lymphovascular invasion; pT1c, all except those with both GI and Ki-67 <14%; pT2, all except those with GIII; pN0 or 1mi; and M0. The pT criteria, although arbitrary, were established by the group of experts from the Basque Country Health System by consensus to optimize the economic cost of the test and perform it when the decision to administer chemotherapy was less clear. Exclusion criteria were as follows: 1) patient’s refusal to undergo the assay; 2) patient’s refusal to receive chemotherapy; and 3) contraindication for chemotherapy (elderly patients and concomitant diseases).
The recommendation of adjuvant systemic therapy, only endocrine therapy or chemotherapy plus endocrine therapy, was recorded before (based on conventional clinicopathologic factors) and after the result of the test. The recommendation for chemotherapy based on clinicopathologic factors was pT2 (all) and pT1c if at least 1 of 2 factors was present (high Ki-67, GIII); no chemotherapy was recommended for pT1a-b. The recommendation after the test was as follows: 1) if RS was low (<18), no chemotherapy was recommended; 2) if RS was high (≥31), chemotherapy was recommended; and 3) if RS was intermediate (18–30), the recommendation took into account the clinicopathologic factors and remained unchanged. The final treatment the patient received was also recorded and was performed according to the final patient choice. The study protocol was approved by the Basque Country Central Ethics Committee.
All data for the variables in the study were collected by each participating medical oncologist in an anonymized manner in a specific database. First, the clinician completed a pretest questionnaire to establish the recommended initial treatment according to standard clinical criteria. The following clinical features were recorded: age, TNM classification, ERs, progesterone receptors (PRs), Ki-67,10 tumor size, tumor grade, surgery type, type of diagnostic (detected at screening program, interval cancer, or outside screening program), and intrinsic subtype according to Prat’s classification and menopause status.11 Variables related to the test such as the RS, the pretest and posttest treatment recommendations (endocrine therapy vs endocrine plus chemotherapy), and final treatment choice were also collected. Follow-up data included recurrence, recurrence data, type of recurrence, last contact, and last contact condition (alive without disease, alive with disease, dead from BC, and dead from other causes), but they were not included in this study, given its short-term approach. The RSs were classified into 3 levels of risk: low (RS <18), medium (RS ≥18<31), and high (RS ≥31). These cutoff points were chosen based on the results of the National Surgical Adjuvant Breast and Bowel Project Protocol B20.3 The economic assessment included the resource use in terms of chemotherapy, first and successive consultations, and adverse effects.
Statistical analysis
Treatment-pattern change was analyzed through cross tables that included the established treatment and the applied criteria (conventional clinical/histochemical criteria and 21-gene RS test). The Mann–Whitney test was used to compare variables with 2 categories, and the Kruskal–Wallis test was used to compare variables with more than 2 categories. The significance level was set at 95%. Differences in categorical variables were evaluated with the χ2 test.
The relationship between the probability of receiving chemotherapy according to applied decision-making criteria (clinical/histochemical or 21-gene RS testing) and patients’ characteristics was analyzed by logistic regressions. Zhang et al proposed a network-regularized logistic regression to improve the performance by incorporating the network regularizations.12 However, we used standard logistic regression as our aim was to explore the change in the predictive capacity of certain variables to identify which patients should receive chemotherapy. Furthermore, we used a complementary approach based on receiver operating characteristic (ROC) curves to measure the discriminative ability of Ki-67, tumor size, and PR to identify which patients would receive chemotherapy based on the 21-gene RS test.13,14 ROC curves determined whether a diagnostic test identified the condition of interest (chemotherapy treatment) and were obtained by plotting sensitivity for each break point on the y-axis and its corresponding 1 - specificity on the x-axis. If the test was sensitive, the ROC curve had sensitivity peaks with associated minimum values of 1 - specificity. Conversely, if the test was nonsensitive, the ROC curve was near the reference line (diagonal line dividing the axis quadrant into 2 equal parts), which indicated the minimum level of discrimination. To characterize the test as a discriminant, areas >70% were required.13,14 All statistical analyses were performed by using SPSS Version 23 (IBM Corporation, Armonk, NY, USA).
Cost analysis
The base case short-term budget impact analysis was carried out from the perspective of the public health system; therefore, only the health care costs were included, but a complementary societal approach was also used.15,16 Resource consumption was recorded prospectively from the beginning of the decision-making process until the end of treatment in terms of visits, chemotherapy, and hospitalizations caused by the chemotherapy toxicity. Treatment decisions about endocrine therapy and chemotherapy prescription were recorded before and after the clinicians received the results of the 21-gene RS testing. Total costs of chemotherapy (ie, chemotherapy drugs, concomitant medications such as granulocyte colony-stimulating factor [G-CSF], administration cost, and follow-up medical visits) were calculated by multiplying resource consumption by unit costs. This cost estimate included only short-term costs associated with chemotherapy treatment; it did not incorporate long-term costs such as long-term side effects. This cost estimate, therefore, constitutes a conservative estimate of the real cost of chemotherapy to the Basque Health Service.
All unit costs were adjusted to 2014 and are displayed in Tables S1 and S2. The hospital admission cost was calculated by the analytical accounting system of the Basque Health Service and the diagnosis-related group system. Unit costs for pharmacy, outpatient visits, emergency room visits, and outpatient clinic service were retrieved from the same accounting system. The costs of adverse effects were calculated by multiplying the frequency of the event by the unit cost. The actual price for the 21-gene RS test to the regional health care payer in Basque Country in 2014 (€2,620) was communicated by the Spanish distributor itself. Given the uncertainty about certain parameters, we carried out a sensitivity analysis by changing the unit costs for chemotherapy and test cost by ±20%. We also reviewed the economic impact of the range of decision-change percentages in single hospitals.
In addition to the health service perspective, the societal perspective was applied to address the consequences of chemotherapy on patient sick leave. The patient’s time lost due to health problems should be independently quantified when it is likely to have a significant economic impact.15,16 In this case, the lost time as paid work was addressed from the perspective of human capital, where the work time lost due to illness was the outcome measure.15,16 Thus, the societal perspective was applied by measuring the potential impact of productivity loss.17 The unit cost for productivity loss for each patient was estimated from the Spanish average monthly gross salary in 2014 (€1,881/month)18 and the length of the treatment for each chemotherapy regimen.
Informed consent
The study protocol was approved by the Euskadi Ethical Committee (PI2015185). Patients gave their signed informed consent when required and applicable according to the Ethic Committee Review Board. The research was conducted in accordance with the Declaration of Helsinki (1975).
Results
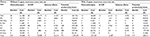
The 21-gene RS test was used to evaluate 401 cases of BC. Table 1 lists the patient and tumor characteristics: low (54.6%), intermediate (38.5%), and high (6.9%). One third of the patients were aged <50 years; the mean age was 57 years, and most patients were postmenopausal (64.5%). The group with largest tumor size corresponded to T1c (65.1%). Three patients presented with T1a tumors, which, therefore, were not within the general criteria for tumor size. However, the results were included in the total data set because these scores were applied in the actual clinical decision making. Using the BC subclassification by Prat et al, we divided the population into individuals with either the luminal A subtype (116 patients, 28.9%) or the luminal B subtype (285 patients, 71.1%).11 The comparison with RS classification resulted in 79 individuals with the luminal A subtype at a low risk of recurrence (68.1%), 36 at an intermediate risk (31%), and 1 at a high risk (0.9%). The RS classification of the luminal B subtype showed 143 persons to be at a low risk of recurrence (50.2%), 117 at an intermediate risk (41.1%), and 25 at a high risk (8.8%).
  | Table 1 Patients’ clinical characteristics Abbreviation: Ki, cellular proliferation marker. |
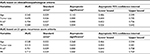
Consistent with our results, chemotherapy would have been prescribed to 56% of patients based on conventional clinicopathologic factors, and that percentage would have decreased to 25% with RS testing. Table 2 summarizes the treatment recommendations and treatment shift between pre- and post-RS. The initial chemoendocrine recommendation was changed to an endocrine recommendation for 124 individuals (31%).
  | Table 2 Treatment recommendation and treatment shift after 21-gene RS testing Abbreviations: CET, chemoendocrine treatment; HT, hormonal treatment; RS, recurrence score. |
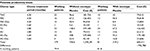
On the ROC curve (Figure 1), PRs and Ki-67 appeared to be accurate predictors of chemotherapy use when decision making was based on the 21-gene RS, because their area under the curve values were >0.70 (Table S3). The results of the logistic regressions (Table 3) reinforce the different roles of PR and tumor size in the effect of the ROC curve. Only Ki-67 showed significant odds ratios in both logistic regressions.
Table 4 displays the disaggregated short-term budget impact with and without 21-gene RS testing distributed by chemotherapy regimen. On the one hand, there was an increase in the total cost per patient due to the cost of the 21-gene RS assay. On the other hand, the decision shift in adjuvant treatment resulted in a reduction in the total number of cases requiring chemotherapy. Thus, the inclusion of the test led to a reduction in overall chemotherapy costs (€369,740). Given the estimated cost of €2,620 per test, there were no net savings, as the difference in chemotherapy treatment did not entirely offset the test cost. However, when a societal perspective was taken into account, the overall budget impact of the 21-gene RS test was cost-neutral, as the savings in chemotherapy costs, in addition to the savings in productivity loss, were greater than the incremental costs due to testing. The total net cost associated with sick leaves was estimated to be €792,780, and the reduction in productivity loss per patient was €1,977. Table S4 disaggregates productivity losses according to the type of chemotherapy. The sensitivity analysis (Table 5) showed no relevant change in the impact according to the perspective. The societal perspective revealed a higher cost only when the test price was increased.
  | Table 5 Impact of sensitivity analysis on the short-term budget according to perspective Abbreviation: BIA, budget impact analysis. |
Discussion
The use of the 21-gene RS test has significantly changed the indication for chemotherapy in our group of patients with BC ER+/HER2− and pT1b-2N01miM0 with predefined criteria. In our patient population, an absolute change in the final treatment decision occurred in 35% of cases. These results are similar to the results of other studies in the Spanish population where the change rate was 32%.17 In the same way, the results of other studies conducted in European19–21 and non-European countries22–25 aligned with ours. The most relevant shift was from initial chemoendocrine therapy to hormonal treatment alone. First, a chemotherapy recommendation was advised in 56% of cases, but after the 21-gene RS assay, that recommendation was reduced to 25%. These results are similar to those presented by the cited studies.
Long-term studies have featured the use of the 21-gene RS assay as cost-effective.26–28 Our results cannot be compared with those of cost-effectiveness studies because we used a short-term budget impact approach. In the Basque Health Service, the net cost per patient was €1,697 higher, in contrast to other studies that found the assay to be cost-saving.26,27 A budget impact analysis carried out in Ireland found net savings explained by a much higher chemotherapy cost and percentage of change (59%).29 This short-term impact relied on 2 drivers: percentage of treatment change and chemotherapy unit cost. The higher the percentage change in the treatment decision and the unit cost of chemotherapy, the more favorable the economic result of the test. Our results are consistent with the literature in which treatment was changed in approximately one third of cases after the use of the 21-gene RS test.19–21 The figures for chemotherapy unit cost, however, vary significantly. Thus, Smyth et al applied a total cost of €7,903 in 2014 for each patient in Ireland treated with chemotherapy, including pharmacy and administration costs (€2,161), G-CSF with pegfilgrastim (€4,985), and adverse effects (€756).29 The main difference between that study and ours is that currently the Basque Health Service uses drugs with a very low unit cost to stimulate the bone marrow. Our study followed the recommendation of experts for economic evaluations and applied 2 perspectives (societal and health system) that produced different results depending on the inclusion of specific stakeholders.16 The interpretation of the shift from one perspective to the other is that maximizing the welfare of society could not always be consistent with the cost containment obtained by the health care sector.16,30 Application of a broader perspective by including the costs associated with the productivity losses produced a different conclusion. Chemotherapy-related sick leaves are long, as they last the duration of treatment, and avoiding treatment results in a €1,977 net saving per patient that offsets the test cost. Besides the sick leave, the consequences for the patients’ quality of life must be considered. The reclassification avoided the chemotherapy-associated suffering, and thus, the patient’s well-being was improved. However, we did not take into account either the costs associated with long-term side effects and potential metastasis or the long-term outcomes associated with the improved quality of life and potentially avoided recurrence due to improved treatment decisions.
As a strength, the present prospective study shows a large patient cohort (401 individuals with BC stages pN0 and pN1mi) in a small population area (2.2 million). A previous Spanish study analyzed a smaller cohort of 107 patients.19 In addition, patients analyzed with the 21-gene RS assay corresponded to the entire BC incident population of the participating hospitals. However, the patient cohort presents a limitation. The testing criteria established by the experts excluded 2 large groups of individuals. The patients with a more favorable prognosis and lower recurrence probability (T1a, T1b without high-risk features, and T1cG1 + low Ki-67) received hormonal treatment without other test evaluation, and the patients with a higher risk for recurrence (T2 + G3) who received chemotherapy directly also were not evaluated with the 21-gene RS test. Therefore, the test was applied to a patient pool with a questionable risk for cancer recurrence according to clinicopathologic classic criteria. By selecting those patients, we could, in fact, define the key target population for which the RS test reduced the uncertainty about chemotherapy decision making and therefore ensured its efficient use.
The PR and Ki-67 levels are relevant variables in Prat’s BC subclassification as luminal A and B subtypes.11 The application of the 21-gene RS test modified significantly the relation between the clinical/histochemical characteristics and the probability of chemotherapy treatment. The results are consistent with the literature, indicating that a decreased level of progesterone and an increased Ki-67 level are associated with an increased long-term risk of cancer recurrence.31 While Ki-67 was maintained as a significant variable in both scenarios, the roles of PR and tumor size were reversed in logistic regressions and ROC curves. In contrast with the study of Jasem et al,25 we did not ascertain tumor size to be significant in predicting the prescription of chemotherapy when a 21-gene RS test was used. These findings reinforce the inclusion of patients with a large tumor size in the target population for 21-gene RS testing because a larger size does not mean a higher recurrence risk, if we adjust by a 21-gene RS.
Conclusion
We can underscore that the use of a 21-gene RS assay reduced the percentage of decisions to use chemotherapy from 56% to 25% of cases. Its short-term economic impact was negative for the Basque Health Service, but it became cost-saving when sick-leave costs were included.
Acknowledgments
The authors acknowledge Patricia Novas-Vidal, Cristina Churruca, Garbiñe Unanue, and Lide Larburu for their contribution in the collection and assembly of data and Arantzazu Arrospide in the data analysis. We would like to acknowledge the English editorial assistance provided by Sally Ebeling. Partial results were presented at the European Society for Medical Oncology Conference held in Copenhagen (Denmark), October 7–11, 2016, and the XXXVI Conference Spanish Health Economics Association held in Murcia (Spain), June 15–17, 2016. The authors’ project was supported by means of the resources of each medical service. Oliver Ibarrondo received an unrestricted grant from Palex Medical SA to carry out the statistical analysis. Isabel Álvarez-López has received honoraria as a member of an advisory board for Genomic Health.
Disclosure
The authors report no conflicts of interest in this work.
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Davies C, Godwin J, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–784. | ||
Harbeck N, Sotlar K, Wuerstlein R, Doisneau-Sixou S. Molecular and protein markers for clinical decision making in breast cancer: today and tomorrow. Cancer Treat Rev. 2014;40(3):434–444. | ||
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351(27):2817–2826. | ||
Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726–3734. | ||
Albain KS, Barlow WE, Shak S, et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010;11(1):55–65. | ||
Coates AS, Winer EP, Goldhirsch A, et al. Tailoring therapies—improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015;26(8):1533–1546. | ||
Senkus E, Kyriakides S, Ohno S, et al. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v8–v30. | ||
Harris LN, Ismaila N, McShane LM, et al. Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2016;34(10):1134–1150. | ||
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group. Recommendations from the EGAPP Working Group: does the use of Oncotype DX tumor gene expression profiling to guide treatment decisions improve outcomes in patients with breast cancer? Genet Med. 2016;18(8):770–779. | ||
Urruticoechea A, Smith IE, Dowsett M. Proliferation marker Ki-67 in early breast cancer. J Clin Oncol. 2005;23(28):7212–7220. | ||
Prat A, Cheang MC, Martín M, et al. Prognostic significance of progesterone receptor-positive tumour cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2013;31(2):203–209. | ||
Zhang W, Wan YW, Allen GI, Pang K, Anderson ML, Liu Z. Molecular pathway identification using biological network-regularized logistic models. BMC Genomics. 2013;14(Suppl 8):S7. | ||
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. | ||
Hanley JA, McNeil BJ. A method of comparing the area under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148(3):839–843. | ||
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3rd ed. Oxford: OUP; 2005. | ||
López-Bastida J, Oliva J, Antoñanzas F, et al. Spanish recommendations on economic evaluation of health technologies. Eur J Health Econ. 2010;11(5):513–520. | ||
Lensberg BR, Drummond MF, Danchenko N, Despiégel N, François C. Challenges in measuring and valuing productivity costs, and their relevance in mood disorders. Clinicoecon Outcomes Res. 2013;5:565–573. | ||
Instituto Nacional de Estadística [National Statistics Institute] (INE); 2015. Decil de salarios del empleo principal. Encuesta de Población Activa (EPA). Año 2014. [Decile of principal employment wages. Economically Active Population Survey (EAPS). Year 2014]. Available from http://www.ine.es/prensa/np939.pdf. Accessed February 16, 2018. Spanish. | ||
Albanell J, González A, Ruiz-Borrego M, et al. Prospective transGEICAM study of the impact of the 21-gene Recurrence Score assay and traditional clinicopathological factors on adjuvant clinical decision making in women with estrogen receptor-positive (ER+) node-negative breast cancer. Ann Oncol. 2012;23(3):625–631. | ||
Gligorov J, Pivot XB, Jacot W, et al. Prospective clinical utility study of the use of the 21-gene assay in adjuvant clinical decision making in women with estrogen receptor-positive early invasive breast cancer: results from the SWITCH study. Oncologist. 2015;20(8):873–879. | ||
Eiermann W, Rezai M, Kümmel S, et al. The 21-gene recurrence score assay impacts adjuvant therapy recommendations for ER-positive, node-negative and node-positive early breast cancer resulting in a risk-adapted change in chemotherapy use. Ann Oncol. 2013;24(3):618–624. | ||
Lo SS, Mumby PB, Norton J, et al. Prospective multicenter study of the impact of the 21-gene recurrence score assay on medical oncologist and patient adjuvant breast cancer treatment selection. J Clin Oncol. 2010;28(10):1671–1676. | ||
de Boer RH, Baker C, Speakman D, Chao CY, Yoshizawa C, Mann GB. The impact of a genomic assay (Oncotype DX) on adjuvant treatment recommendations in early breast cancer. Med J Aust. 2013;199(3):205–208. | ||
Oratz R, Kim B, Chao C, et al. Physician survey of the effect of the 21-gene recurrence score assay results on treatment recommendations for patients with lymph node-positive, estrogen receptor-positive breast cancer. J Oncol Pract. 2011;7(2):94–99. | ||
Jasem J, Amini A, Rabinovitch R, et al. 21-gene recurrence score assay as a predictor of adjuvant chemotherapy administration for early-stage breast cancer: an analysis of use, therapeutic implications, and disparity profile. J Clin Oncol. 2016;34(17):1995–2002. | ||
Hornberger J, Cosler LE, Lyman GH. Economic analysis of targeting chemotherapy using a 21-gene RT-PCR assay in lymph-node-negative, estrogen-receptor-positive, early-stage breast cancer. Am J Manag Care. 2005;11(5):313–324. | ||
Tsoi DT, Inoue M, Kelly CM, Verma S, Pritchard KI. Cost-effectiveness analysis of recurrence score-guided treatment using a 21-gene assay in early breast cancer. Oncologist. 2010;15(5):457–465. | ||
Rouzier R, Pronzato P, Chéreau E, Carlson J, Hunt B, Valentine WJ. Multigene assays and molecular markers in breast cancer: systematic review of health economic analyses. Breast Cancer Res Treat. 2013;139(3):621–637. | ||
Smyth L, Watson G, Walsh EM, et al. Economic impact of 21-gene recurrence score testing on early-stage breast cancer in Ireland. Breast Cancer Res Treat. 2015;153(3):573–582. | ||
Byford S, Raftery J. Perspectives in economic evaluation. BMJ. 1998;316(7143): 1529–1530. | ||
Chang J, Powles TJ, Allred DC, et al. Prediction of clinical outcome from primary tamoxifen by expression of biologic markers in breast cancer patients. Clin Cancer Res. 2000;6(2):616–621. |
Supplementary materials
  | Table S1 Unit costs of resources Abbreviation: G-CSF, granulocyte colony-stimulating factor. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.