Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Changes in Oral Corticosteroid Utilization in Patients with COPD Following Initiation of FF/UMEC/VI
Authors Bogart M, Abbott CB, Bangalore M, McMorrow D, Packnett ER, DiRocco K
Received 22 May 2023
Accepted for publication 3 October 2023
Published 1 November 2023 Volume 2023:18 Pages 2367—2379
DOI https://doi.org/10.2147/COPD.S419272
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Michael Bogart,1 Carl B Abbott,2 Mohan Bangalore,3 Donna McMorrow,4 Elizabeth R Packnett,4 Kristi DiRocco3
1US Value Evidence and Outcomes, GSK, Durham, NC, USA; 2US Medical Affairs, GSK, Durham, NC, USA; 3US Medical Affairs, GSK, Collegeville, PA, USA; 4Merative, Ann Arbor, MI, USA
Correspondence: Kristi DiRocco, US Medical Affairs, GSK, 1250 S. Collegeville Road, Collegeville, PA 19426, USA, Tel +1 610-412-7175, Email [email protected]
Purpose: Oral corticosteroids (OCS) play a role in the treatment of acute chronic obstructive pulmonary disease (COPD) exacerbations; however, chronic use is not recommended due to the high rate of systemic complications, development of comorbidities, and increased mortality. Data assessing the real-world impact of fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) on OCS utilization rates are limited. This study assessed the impact of FF/UMEC/VI on OCS use among patients with COPD previously treated with OCS.
Patients and Methods: A retrospective database study of patients with COPD aged ≥ 40 years who initiated FF/UMEC/VI from 1 November 2017 to 31 December 2018, identified through the MarketScan® Commercial and Medicare Supplemental databases. Patients were required to have ≥ 1 dispensing of an OCS prior to initiation of FF/UMEC/VI (index) and were followed up for 12 months post-index. OCS utilization patterns, potential OCS-related adverse events, healthcare resource utilization (HCRU), and costs were compared between the 12-month pre- and post-index periods.
Results: A total of 2013 patients were identified (mean age 63.5 years, 55.7% female). The proportion of patients with ≥ 1 OCS claim decreased by 32.2% between the pre- and post-index period (67.8% vs 100%; p < 0.001). Comparing the post-index period to the pre-index period, mean number of OCS pharmacy claims per patient decreased from 3.3 to 2.5 (p < 0.001) and mean daily dose was reduced from 3.1 to 2.6 mg/day (p = 0.004); 30.0% of patients reduced their daily dose by 90– 100%. Reductions were also seen in COPD-related HCRU. The proportion of patients with an inpatient admission for COPD decreased from 11.4% to 7.1% (p < 0.001), emergency room visits decreased from 23.1% to 17.4% (p < 0.001), and office visits from 97.5% to 90.1% (p < 0.001). Similar results were seen for all-cause HCRU.
Conclusion: Among patients with COPD with prior OCS use, FF/UMEC/VI initiation resulted in significant reductions in OCS utilization, COPD-related HCRU (including hospitalization), and all-cause HCRU.
Plain Language Summary: Oral corticosteroids (OCS) are drugs that are often used in the short term to treat chronic obstructive pulmonary disease (COPD) exacerbations. Long-term use of OCS is not recommended as this can increase the risk of pneumonia and death. Fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) is a maintenance treatment for COPD, which combines three drugs into one inhaler. In this study, we investigated OCS use before and after starting FF/UMEC/VI. We found that there were 32.2% less patients with an OCS claim in the year after starting FF/UMEC/VI compared with the year before. In addition, 30.0% of patients reduced their daily OCS dose by 90– 100%. We also looked at how often patients were using healthcare services because of their COPD after starting FF/UMEC/VI, and how much this cost. We found that there were fewer inpatient stays, emergency room visits, and doctor’s office visits due to COPD in the year after starting FF/UMEC/VI treatment compared with the year before. Overall, these results show that patients who use OCS every day may be able to reduce their dose after starting FF/UMEC/VI treatment, which may avoid some of the potential side effects of OCS.
Keywords: COPD, FF/UMEC/VI, oral corticosteroids
Introduction
Oral corticosteroids (OCS) are used to treat acute chronic obstructive pulmonary disease (COPD) exacerbations, although use should be limited to 5 days.1 Chronic OCS use is not recommended due to the high rate of systemic complications associated with their use, including respiratory muscle deterioration, immunosuppression, increased blood glucose, increased blood pressure, and adrenal suppression.2–5 Prolonged use of high dose OCS has been shown to contribute to the development of comorbidities such as diabetes, osteoporosis, and hypertension.3,6 Studies have also reported that long term use of high-dose OCS may increase mortality in patients with stable severe and very severe COPD.4,7,8
A large population-based study of non-elderly (<64 years) adults in the US with a wide range of conditions demonstrated that even short-term use of OCS is associated with an increased risk of pneumonia, sepsis, and death.9 These results are supported by Global Initiative for Chronic Obstructive Lung Disease recommendations, which state that due to these associations, use should be confined to patients with significant exacerbations.1
Despite their association with cumulative issues, the prevalence of OCS use remains high and widespread. A retrospective database analysis of healthcare claims data from 2007 to 2008 found that 17,457 (31.5%) patients with COPD had used OCS in 2008.10 Another study using Medicare claims data from 2013 to 2019 found that 36% of patients newly diagnosed with COPD received OCS in the 48 months following diagnosis, lasting longer than 5–7 days for 38% of episodes.11
Once-daily single-inhaler triple therapy (SITT) with fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) was approved by the US Food and Drug Administration in September 2017.12 Compared to dual therapy, FF/UMEC/VI has been shown to reduce the risk of COPD exacerbations and improve lung function and health-related quality of life.13 SITT with FF/UMEC/VI delivered via the Ellipta inhaler has also been shown to improve lung function and result in significantly more patients achieving health status improvement compared to non-Ellipta multiple-inhaler triple therapy.14 However, data assessing the real-world impact of FF/UMEC/VI on rates of OCS utilization are limited.
This study was therefore designed to assess the relationship between initiation of FF/UMEC/VI and OCS utilization, and describe all-cause and COPD-related healthcare resource utilization (HCRU), potential OCS-related adverse events (AEs), and costs among patients with COPD previously treated with OCS.
Materials and Methods
Study Design
This was a retrospective study conducted using medical and pharmacy claims data from the MarketScan® Commercial and Medicare Supplemental databases. Patients aged ≥40 years who were diagnosed with COPD during the patient selection period (1 November 2017 to 31 December 2018) were identified (Supplementary Figure 1).
The index date was the date of the first FF/UMEC/VI pharmacy claim following the first COPD diagnosis during the patient selection period. The index date was considered part of the pre-index period. OCS use, potential OCS-related AEs, and all-cause and COPD-related HCRU and costs were compared between the 12-month pre- and post-index periods.
Data Collection
The MarketScan® Research databases used for this study provided access to healthcare data for patients insured commercially. Both the Commercial and Medicare Supplemental databases provide detailed cost, use, and outcomes data for healthcare services performed in both inpatient and outpatient settings. Medical claims are linked to outpatient prescription drug claims and person-level enrollment data via unique enrollee identifiers.
Study Population
Eligible patients met the following inclusion criteria: ≥1 inpatient claim with a diagnosis of COPD in the primary position, or ≥2 non-diagnostic outpatient claims with a diagnosis of COPD with different service dates from 1 November 2017 to 31 December 2018 in the MarketScan® Commercial or Medicare Supplemental databases; ≥40 years of age at COPD diagnosis; ≥12 months of continuous enrollment prior to and following COPD diagnosis; ≥1 pharmacy claim for FF/UMEC/VI following COPD diagnosis; ≥12 months of continuous enrollment prior to and following index; and ≥1 OCS pharmacy claim in the 12 months prior to index. No exclusion criteria were applied.
Outcomes
Primary Objective: OCS Use
Two primary OCS outcome measures were assessed in the post-index period relative to the pre-index period. Any OCS use was assessed as a binary indicator to determine the percentage of patients who had any pharmacy claims for OCS. Mean number of OCS pharmacy claims per patient was described as a continuous variable for the pre- and post-index periods.
OCS bursts were also assessed and defined by an average daily dose ≥20 mg prednisone equivalents (Supplementary Table 1) for 3–28 days, and an outpatient/emergency room (ER) claim with a diagnosis of COPD in any position within –7/6+ days of the pharmacy claim.
Chronic OCS use was defined as an OCS mean daily dose ≥5 mg prednisone equivalents over the pre- or post-index period.
Proportion of days covered (PDC) was calculated as the sum of days’ supply divided by 365. PDC was calculated among all patients and separately among patients with ≥1 OCS claim during the pre- and post-index periods.
Mean daily dose in prednisone equivalents per 12 months was calculated among all patients over the pre- and post-index periods. Reduction in mean daily dose was calculated as the difference in mean daily dose between the pre- and post-index periods in mg/day. The magnitude of reduction in mean daily dose in the post-index period compared to the pre-index period was summarized as follows: 90–100%, 75 to <90%, 50 to <75%, 0 to <50%, no reduction, and no use. Magnitude of reduction in mg/day was also categorized after examining the distribution of the difference in mean mg/day as <1 mg/day, 1–4 mg/day, 5–9 mg/day, and ≥10 mg/day.
Secondary Objectives: Potential OCS-Related AEs, HCRU, and Costs
Patients with each potential OCS-related AE were identified using the presence of a diagnosis code or a non-diagnostic medical claim during the post-index period. As we compared overall AE incidence before and after initiation of FF/UMEC/VI, potential OCS-related AEs reported during the post-index period were not necessarily new.
The number and proportion of patients with each of the following potential OCS-related AEs during the post-index period was described: bone and muscle-related (acute [bursitis], chronic [fractures, avascular necrosis, osteoporosis]); cardiovascular (acute [myocardial infarction], chronic [atrial fibrillation/flutter, congestive heart failure, stroke]); central nervous system-related (chronic [steroid psychosis]); dermatologic (chronic [hirsutism, erythema]); gastrointestinal (acute [gastrointestinal ulcers or bleeds, acute pancreatitis]); immune system-related (acute [urinary tract infection, sepsis]); metabolic and endocrinologic (chronic [metabolic syndrome, Cushing syndrome, drug-induced adrenocortical insufficiency]); ophthalmologic (chronic [cataracts, glaucoma]).
A post-hoc sensitivity analysis was conducted for potential OCS-related AEs among: (1) patients with no OCS during follow-up; (2) patients with a reduction in OCS dose during follow-up; and (3) patients with no reduction in OCS dose during follow-up.
All-cause and COPD-related healthcare costs were reported during the post-index period. COPD-related utilization and costs were calculated using inpatient claims with a COPD diagnosis in the primary position or outpatient claims with a COPD diagnosis in any position, or medical or pharmacy claims for COPD treatments. Costs were based on paid amounts of adjudicated claims, including insurer and health plan payments, as well as patient cost-sharing in the form of co-payment, deductible, and coinsurance. All costs were adjusted using the Consumer Price Index and standardized to 2019 US dollars. Total costs, inpatient resource use and costs, outpatient resource use and costs, and outpatient pharmacy resource use and costs were reported. Outpatient resource use and costs were itemized by ER resource use and costs, outpatient office visit resource use and costs, and other outpatient HCRU and costs (including any outpatient services not specifically reported separately, such as laboratory and radiology services).
Data Analysis
Means, standard deviations (SDs), and medians were reported for continuous variables, and counts and percentages were reported for dichotomous or categorical variables. McNemar’s chi-squared test was used to evaluate the statistical significance of differences for dichotomous or categorical variables; paired t-tests were used for comparison of continuous variables. A p-value of 0.05 was the maximum p-value for which differences between treatment groups were considered statistically significant.
Results
Study Population
A total of 2013 patients were included in the analyses (Supplementary Table 2). Patients had a mean (SD) age of 63.5 (10.2) years and 55.7% were female. Mean (SD) Deyo-Charlson Comorbidity Index score was 2.4 (1.9), and the most common pre-index comorbidities were infections (78.3%), hypertension (68.0%), hyperlipidemia (55.3%), asthma (33.4%), and depression (33.2%). In the pre-index period, 44.6% had ≥1 claim for inhaled corticosteroid/long-acting beta agonist, and 39.4% had ≥1 claim for long-acting muscarinic antagonist. Patient demographic and clinical characteristics are reported in Table 1.
 |
Table 1 Patient Baseline Demographic and Clinical Characteristics |
OCS Use
The proportion of patients with ≥1 OCS claim was reduced by 32.2% in the post-index period (100.0% in the pre-index period vs 67.8% in the post-index period; p < 0.001) (Figure 1A). The mean number of OCS pharmacy claims per patient also decreased significantly in the post-index period (3.3 [SD 3.0] vs 2.5 [SD 3.4]; p < 0.001) (Figure 1B).
 |
Figure 1 Proportion of patients with ≥1 OCS claim (A) and mean number of OCS claims per patient (B). Abbreviation: OCS, oral corticosteroids. |
There was a significant reduction in the proportion of patients with an OCS burst (60.4% in the pre-index period vs 38.6% in the post-index period; p < 0.001). Statistically significant reductions were also observed for the mean number of OCS bursts per patient (1.2 [SD 1.5] in the pre-index period vs 0.8 [SD 1.5] in the post-index period; p < 0.001) (Figure 2).
 |
Figure 2 Mean number of OCS bursts per patient. Abbreviation: OCS, oral corticosteroids. |
Compared to during the pre-index period, there was a slight non-significant decrease in chronic OCS use in the post-index period (n = 276, 13.7% vs n = 266, 13.2%; p = 0.515). Across the entire population, mean daily OCS dose dropped significantly during the post-index period compared with the pre-index period (2.6 mg/day vs 3.1 mg/day; p = 0.004). Among all patients, 64.7% (n = 1302) patients had a reduction in OCS use (Figure 3A). Of the total sample (N = 2013), 48.1% patients had a reduction ≥50%, and 30% had a reduction of 90–100%. Most patients (69.4%) had a decrease of <1 mg/day averaged over the post-index period (Figure 3B). However, around 5% of patients were able to reduce their mean daily OCS dose by ≥5 mg/day.
Potential OCS-Related AEs
Among the entire cohort, the three most common potential OCS-related AEs during the post-index period were congestive heart failure (16.5%), atrial fibrillation/flutter (14.5%), and urinary tract infection (8.7%) (Figure 4). The proportion of patients experiencing these AEs was significantly increased in the post-index period compared with the pre-index period (congestive heart failure: p < 0.01; atrial fibrillation/flutter: p < 0.001; urinary tract infection: p < 0.05).
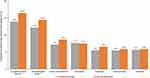 |
Figure 4 Incidence of potential OCS-related AEs. Abbreviations: AE, adverse event; OCS, oral corticosteroids. Notes: *p < 0.05; **p < 0.01; ***p < 0.001, comparing pre- and post-index periods. |
In the post-hoc sensitivity analyses, results for the cohort with no reduction in OCS dose during follow-up were similar to the overall cohort (Supplementary Figure 2).
HCRU and Costs
Utilization of all-cause inpatient admissions, ER visits, and outpatient office visits was lower during the post-index period compared with the pre-index period (Table 2). Likewise, fewer patients had COPD-related inpatient admissions or any type of outpatient service during the post-index period compared with the pre-index period (Table 3). In addition, with the exception of other outpatient services, there were fewer COPD-related admissions, outpatient visits, or services during the post-index-period.
 |
Table 2 All-Cause HCRU |
 |
Table 3 COPD-Related HCRU |
All-cause costs were higher in the post-index period in all categories compared with the pre-index period (Figure 5). COPD-related total outpatient and outpatient drug costs were higher in the post-index period, although COPD-related inpatient costs were lower than pre-index period costs (Figure 6).
 |
Figure 5 All-cause costs. Abbreviations: ER, emergency room; Rx, prescription; USD, US dollars. Notes: *p < 0.01; **p < 0.001, comparing pre- and post-index periods. |
 |
Figure 6 COPD-related costs. Abbreviations: COPD, chronic obstructive pulmonary disease; ER, emergency room; USD, US dollars. Notes: *p < 0.05; **p < 0.001, comparing pre- and post-index periods. |
Discussion
This retrospective database analysis found that use of OCS decreased in patients with COPD following initiation of FF/UMEC/VI. Mean number of OCS claims, annual frequency of OCS bursts, and mean OCS dose were significantly lower during the post-index period compared with the pre-index period. However, decreases in the proportion of patients with chronic OCS use were small and not statistically significant; and further, approximately two thirds of patients were still exposed to OCS in the post-index period, despite a reduction in the magnitude of exposure.
Despite the observed decrease in OCS use (with the exception of chronic OCS use), the incidence of potential OCS-related AEs in the exploratory analysis was higher during the post-index period. As all patients were on OCS in the pre-index period, it may have taken time for potential OCS-related AEs to occur, and for the impact of a medication change on AEs to be observed. In addition, many of the AEs investigated are time-confounded and may be unrelated to OCS use, with aging increasing the risk of their development (eg, hip fracture). Further, a recent literature review reported short-term use of OCS was associated with risk from serious AEs, including osteoporosis, hyperglycemia, and muscle weakness.15 As the results of the sensitivity analysis for patients with no reduction in OCS dose were similar to the overall cohort, it is likely that the pre- versus post-index changes in potential OCS-related AEs were attributable to continued use of OCS, rather than another factor.
Fewer patients had an all-cause or COPD-related inpatient admission, ER visit, or outpatient office visit during the post-index period than the pre-index period. However, mean all-cause and COPD-related post-index costs were similar or higher in the post-index than pre-index period, with the exception of COPD-related inpatient costs. This may reflect the high comorbidity profile of these patients, alongside increased pharmacy costs associated with initiating FF/UMEC/VI. In addition, this is a cohort of older patients (mean age: 63.5 years) who will be older in the post-index period and may therefore naturally incur more costs due to this increase in age.
After a COPD exacerbation, a large proportion of patients continue to use the same medication. In a retrospective database analysis, Bogart et al found that 64.3% of the 307,727 included patients remained on the same medication after an exacerbation, rather than escalating their treatment.16 These results suggest a benefit of switching to FF/UMEC/VI to reduce OCS bursts and COPD exacerbations, reiterating the importance of correct treatment escalation.
There are several limitations which should be considered. This study was unable to capture medications administered during an inpatient admission and may therefore underestimate the total number of patients receiving COPD treatments. Patients who died during the 12 months following their COPD diagnosis were not included in the study population, and many patients with COPD included in the study were employed. This may lead to selection of a “healthier” patient population. Potential OCS-related AEs may take longer to develop than the 12-month post-index period and may therefore not be recorded in this study. The source population only included individuals with 24 months of continuous private insurance enrollment. Results may therefore not be generalizable to patients with COPD who do not have health insurance, or who have different types of insurance. Comorbid conditions were measured during the pre-index period and so time-varying covariates which may be important risk factors for OCS use, potential OCS-related AEs, or HCRU and costs were not accounted for during the post-index period. It should also be noted that approximately one third of patients included in this study had concomitant asthma, which may have impacted our results. Finally, patients were assumed to be compliant with their medication.
Conclusion
Among patients with COPD who have prior OCS use, the initiation of FF/UMEC/VI resulted in significant reductions in OCS utilization, COPD-related HCRU (including hospitalization), and all-cause HCRU. As long-term OCS use is associated with systemic complications, physicians should consider changing maintenance COPD therapy in patients with a history of OCS use to reduce incidence of potential OCS-related AEs. This study suggests that OCS use can be reduced in patients on daily OCS who initiate (or switch to) FF/UMEC/VI from their previous maintenance regimen. Further research is needed to assess the impact of OCS reduction on potential OCS-related AEs.
Abbreviations
COPD, chronic obstructive pulmonary disease; ER, emergency room; FF/UMEC/VI, fluticasone furoate/umeclidinium/vilanterol; HCRU, healthcare resource utilization; OCS, oral corticosteroids; PDC, proportion of days covered; SD, standard deviation; SITT, single-inhaler triple therapy.
Data Sharing Statement
The data that support the findings of this study are available from Merative (https://www.merative.com/). Restrictions apply to the availability of these data, which were used under license for this study.
Ethics Approval and Informed Consent
All database records are statistically de-identified and certified to be fully compliant with US patient confidentiality requirements set forth in the Health Insurance Portability and Accountability Act of 1996. Because this study used only de-identified patient records and did not involve the collection, use, or transmittal of individually identifiable data, this study did not require institutional review board approval.
Acknowledgments
Editorial support (in the form of writing assistance, including preparation of the draft manuscript under the direction and guidance of the authors, collating and incorporating authors’ comments for each draft, assembling tables and figures, grammatical editing, and referencing) was provided by Kathryn Wardle of Apollo, OPEN Health Communications, and was funded by GSK.
These data have been previously presented in abstract/presentation form at the American College of Chest Physicians – CHEST Annual Meeting, virtual event, 17–20 October, 2021: Bogart M, Bangalore M, McMorrow D, Packnett E. Changes in oral corticosteroids utilization in patients with COPD following initiation of FF/UMEC/VI. CHEST. 2021;160(4):A1826. doi: 10.1016/j.chest.2021.07.1641
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the manuscript; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by GSK (study number 214319). The sponsor was involved in study conception and design, data interpretation, and the decision to submit the article for publication. The sponsor was also given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Disclosure
MBo, CBA, and MBa were employees of, and/or shareholders in, GSK at the time of study. DM and ERP are employees of Merative (IBM Watson Health at the time of study), which received research funds from GSK to conduct this study, but not for manuscript development. KD is an employee of, and/or shareholder in, GSK. The authors report no other conflicts of interest in this work.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2023 report; 2023. Available from: https://goldcopd.org/2023-gold-report-2/.
2. Decramer M, Lacquet LM, Fagard R, Rogiers P. Corticosteroids contribute to muscle weakness in chronic airflow obstruction. Am J Respir Crit Care Med. 1994;150(1):11–16. doi:10.1164/ajrccm.150.1.8025735
3. Walters JA, Walters EH, Wood-Baker R. Oral corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;(3):CD005374. doi:10.1002/14651858.CD005374
4. Horita N, Miyazawa N, Morita S, et al. Evidence suggesting that oral corticosteroids increase mortality in stable chronic obstructive pulmonary disease. Respir Res. 2014;15(1):37. Available from: https://respiratory-research.biomedcentral.com/articles/10.1186/1465-9921-15-37
5. Mortimer KJ, Tata LJ, Smith CJ, et al. Oral and inhaled corticosteroids and adrenal insufficiency: a case-control study. Thorax. 2006;61(5):405–408. doi:10.1136/thx.2005.052456
6. McEvoy CE, Niewoehner DE. Adverse effects of corticosteroid therapy for COPD. A critical review. Chest. 1997;111(3):732–743. doi:10.1378/chest.111.3.732
7. Chang YP, Lai CH, Lin CY, et al. Mortality and vertebral fracture risk associated with long-term oral steroid use in patients with chronic obstructive pulmonary disease: a systemic review and meta-analysis. Chron Respir Dis. 2019;16:1479973119838280. doi:10.1177/1479973119838280
8. Schols AM, Wesseling G, Kester AD, et al. Dose dependent increased mortality risk in COPD patients treated with oral glucocorticoids. Eur Respir J. 2001;17(3):337–342. doi:10.1183/09031936.01.17303370
9. Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. 2017;357:j1415. doi:10.1136/bmj.j1415
10. Diette GB, Dalal AA, D’Souza AO, Lunacsek OE, Nagar SP. Treatment patterns of chronic obstructive pulmonary disease in employed adults in the United States. Int J Chron Obstruct Pulmon Dis. 2015;10:415–422. doi:10.2147/COPD.S75034
11. Bazell C, Pollack M, Comellas AP, et al. A 4-year retrospective claims analysis of oral corticosteroid use and health conditions in newly diagnosed Medicare FFS patients with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:2635–2652. doi:10.2147/copd.S373590
12. GlaxoSmithKline. Trelegy Ellipta. North Carolina: GlaxoSmithKline; 2020. https://us.gsk.com/media/5265/trelegy-ellipta-pi-mg-ifu.pdf.
13. Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680. doi:10.1056/NEJMoa1713901
14. Halpin DMG, Worsley S, Ismaila AS, et al. INTREPID: single- versus multiple-inhaler triple therapy for COPD in usual clinical practice. ERJ Open Res. 2021;7(2):00950–2020. doi:10.1183/23120541.00950-2020
15. Heaney LG, Schleich F, Korn S, et al. Recognising the long-term burden of short course oral corticosteroids. Eur Respir J. 2021;58:PA3548. doi:10.1183/13993003.congress-2021.PA3548
16. Bogart M, Germain G, Laliberté F, Lejeune D, Duh MS. Real-world treatment patterns and switching following chronic obstructive pulmonary disease exacerbation in patients with commercial or Medicare insurance in the United States. Int J Chron Obstruct Pulmon Dis. 2023;31:1575–1586. doi:10.2147/COPD.S398816
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

