Back to Journals » Journal of Inflammation Research » Volume 16
Changes in Laboratory Indexes for Multiple Myeloma Patients Before and After Autologous Stem Cell Transplant
Authors Zhao R, Zhao J, Song Y, Fu W, Wang Q, Zhang R
Received 31 August 2023
Accepted for publication 7 November 2023
Published 5 December 2023 Volume 2023:16 Pages 5779—5789
DOI https://doi.org/10.2147/JIR.S433424
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Tara Strutt
Rui Zhao, Jing Zhao, Yichuan Song, Wenxuan Fu, Qingtao Wang, Rui Zhang
Department of Clinical Laboratory, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Qingtao Wang; Rui Zhang, Department of Clinical Laboratory, Beijing Chao-yang Hospital, Capital Medical University, No. 8, Gongtinan Road, Chao-Yang District, Beijing, 100020, People’s Republic of China, Tel +86 1085231660, Email [email protected]; [email protected]
Purpose: Outcomes after autologous stem cell transplantation (ASCT) are quite variable and difficult to predict. Second-generation flow, second-generation sequencing, and other tests are invasive and expensive for patients. In this study, we aimed to analyze laboratory data before and after transplantation to look for laboratory indicators that could predict disease progression in patients with newly diagnosed multiple myeloma (NDMM) patients underwent ASCT.
Patients and Methods: Standard complete blood count (CBC) parameters, clinical biochemical, and immunological indicators on day -5 and day 90 after ASCT were obtained. Receiver-operating characteristic (ROC) curve was used to determine the cutoff values, we evaluated the predictive abilities of laboratory parameters for progression-free survival (PFS). Univariate and multivariate analyses were performed to evaluate the prognostic significance of variables associated with the PFS of 166 NDMM who underwent ASCT.
Results: At day-5, a low absolute monocyte count (AMC, p=0.001), systemic inflammation response index< 1.56 (SIRI, P=0.03), serum calcium (p=0.02), and albumin (p=0.006) can predict for superior PFS. At Day +90, a high absolute neutrophil count (ANC, p = 0.008) and lymphocyte-to-monocyte ratio (LMR, p = 0.02), a low neutrophil-to-lymphocyte ratio (NLR, p =0.02) and SIRI< 0.41 (p=0.02) predicted for superior PFS.
Conclusion: There are inflammation-related indicators derived from peripheral blood cell count (WBCC) – ANC, NLR, SIRI, and LMR - which can serve as potential biomarkers for predicting PFS of NDMM patients underwent ASCT.
Keywords: multiple myeloma, autologous stem cell transplantation, SIRI, lymphocyte-to-monocyte ratio
Introduction
The incurable malignancy of multiple myeloma (MM) is characterized by the abnormal proliferation of clonal plasma cells. It ranks as the second most prevalent malignant neoplasm in the hematopoietic system in numerous nations.1,2 Findings from prospective controlled trials comparing induction therapy with thalidomide and lenalidomide, followed by sequential ASCT and continuous novel drugs, have demonstrated that MM patients who undergo ASCT experience improved PFS, underscoring the significance of ASCT in the management of newly diagnosed MM.3,4 Nevertheless, the outcomes following ASCT exhibit considerable variability among patients. The progression of disease in multiple myeloma is characterized by variability and heterogeneity, as some patients may experience prolonged periods of remission while others may undergo rapid disease progression.5 A study suggested that the cumulative incidence rates of relapse at 1, 3, and 5 years in the short-term survival group were 9%, 63%, and 82%, respectively, compared to 2%, 20%, and 40%, in the long-term survivor group.6 The timing for assessing treatment response following transplantation lacks standardization and varies across different clinical trials. Following ASCT, patients with multiple myeloma have their tumor burden reevaluated approximately 100 days before initiating maintenance therapy.7 One of the reasons for recurrence was that multiple myeloma cell lines became resistant to proteasome inhibitors. There are several common mechanisms of resistance, such as mutations and aberrant expression of proteasome subunits, endoplasmic reticulum stress, autophagy inhibition, activation of efflux drug pumps, bone marrow microenvironment, excessive nuclear export of proteins, and metabolic adaptation.8
The immunological microenvironment is correlated with clinical outcomes in multiple myeloma patients. In addition, recent studies have demonstrated that the LMR can provide useful insight into the immune status of the organism and can be a critical factor in predicting the prognosis of a variety of blood tumors and solid tumors. Meta-analysis of 13 studies on MM reported that the indexes NLR and LMR/MLR derived from WBC were useful biomarkers to predict prognosis.9 The LMR is calculated as lymphocyte count/monocyte count, and the NLR is calculated as neutrophil count/lymphocyte count. Multiple myeloma is characterized by anemia, leukopenia, and leukopenia thrombocytopenia, which is less common. Among the prognostic markers used in the Durie-Salmon staging system 2, anemia is associated with a worse prognosis.10 Several previous studies have demonstrated clinical significance for MM patients’ prognosis according to red cell distribution (RDW), hemoglobin (Hgb), and platelet counts (PLT).11–13
In a single-center retrospective study, we analyzed laboratory data for patients before and after autologous stem cell transplantation to identify indicators of disease progression. Our study examined the value and significance of these indicators in clinical treatment.
Materials and Methods
Patients
MM patients who underwent ASCT for the first time between January 2017 and March 2022 were included in our retrospective study. We received approval for the protocol of this study from Beijing Chao-Yang Hospital Ethics Committee (2022-ke-48) and institutional review board. Informed consent was waived by the Research Ethics Board of Beijing Chaoyang Hospital due to the retrospective nature of the study. Patient data was anonymized before analysis. All methods were carried out in accordance with the Declaration of Helsinki. A symptomatic diagnosis of MM as defined by the International Myeloma Working Group was required for eligibility. Patients who were younger than 18 years of age, who had undergone tandem ASCT, or who had undergone an allogeneic or ASCT before the trial were excluded.
Laboratory Measures
Baseline demographic data, disease and treatment characteristics, and Standard CBC parameters were collected at day 5 and day 90 post-ASCT,14 including Hgb, PLT, and MCV, as well as immune status markers called LMR and NLR. The blood routine analysis was performed using an automatic hematology analyzer (XN-20, Sysmex). Clinical biochemical and immunological indicators such as albumin, lactate dehydrogenase (LDH), creatinine, blood calcium, and Beta 2-microglobulin (β2-mg) were also assessed. Biochemical Index Biochemical examination was carried out by an automatic biochemical analyzer (ADVIA2400, Siemens). SIRI is the neutrophil count multiplied by the monocyte count divided by the lymphocyte count. To evaluate the predictive powers and optimal cutoff values of other laboratory indicators of PFS, ROC curves and area under the ROC curves (AUCs) were used.
Statistical Analysis
Before running each statistical test, we checked whether its assumptions were met. We analyzed data using SPSS 22.0 (IBM Corp., Armonk, NY, USA) and R (version 3.5.3). Overall survival (OS) was defined as the time from ASCT to death, progression, or last follow-up date, while PFS was defined as the time from ASCT to death, progression, or last follow-up date. To compare OS and PFS, Kaplan-Meier (KM) curve estimates were applied, along with Log rank tests (Univariate analysis). An evaluation of the effect of these parameters on PFS was then conducted using multivariate Cox’s proportional hazards model. The relationship between these parameters and PFS was then evaluated using Cox’s proportional hazards model. P values < 0.05 were considered significant. The accuracy of our model was further verified by bootstrap validation using computer resampling for 1000 repetitions of simple random sampling with replacement. The calibration curve was employed to detect the concentricity between the model probability curve and the ideal curve (see Supplementary Figures 1–3).
Results
Patient Characteristics
In the final analysis, 166 patients underwent their first ASCT between 2017 and 2022. The baseline characteristics are presented in Table 1. The flow chart of inclusion and exclusion criteria is summarized in Figure 1. The median diagnosis age was 54.8 (50–60). IgA (n=36, 22%) and IgG (n=67, 40.9%) subtypes were found in most patients, as well as stage 3 myeloma (n = 56, 35.7%). FISH abnormalities most commonly found were 1q21 amplification (n=62, 37.1%) and t (11;14) (n=28, 16.8%). Lenalidomide, bortezomib, and dexamethasone (VRD, n=74, 47.2%) was the most commonly used induction regimen. Cyclophosphamide is the most commonly used mobilization scheme. There was one patient who died during the study, and the median follow-up time was 25 months (range: 3–67 months). Median PFS and OS were not reached. In the 3 years, 71% of respondents reported PFS. An analysis of the correlation between laboratory data in MM patients before and after ASCT was conducted in the entire series. There was a positive correlation between SIRI and AMC and a negative correlation between SIRI and LMR in Figure 2. ALB and serum were positively correlated (r=0.59, p < 0.001)
 |
Table 1 Baseline Characteristics of All Patients |
 |
Figure 1 Flowchart depicting the composition of patients with MM who underwent ASCT in the study group. |
 |
Figure 2 The association between laboratory data in MM patients before (A) and after ASCT (B). |
Differences in Pre-and Post-ASCT of Laboratory Tests
The lower, median, and upper quartiles for Neutrophil, lymphocytes, NLR, monocytes, HGB, PLT, MCV, LMR, ALB, LDH, Creatinine, Blood calcium, and β2-MG on Day −5 and Day +90 are shown in Table 2. We first analyzed differences in pre-and post-ASCT median values and found that the ANC levels (2.6 versus 2.5 × 103/μL, p = 0.84) and Creatinine (58.9 versus 57.2 μmol/L, p = 0.16) were similar. We also found that ALC levels (0.9 versus 1.8 × 103/μL, p < 0.0001), AMC (0.34 versus 0.35 × 103/μL, p < 0.05), LMR (2.5 versus 4.9 × 103/μL, p < 0.0001), HGB levels (121 versus 123 g/L, p<0.002), MCV (92.2 versus 93 fL, p < 0.003), ALB (40.4 versus 44.5 g/L, p< 0.0001), β2-MG (2.2 versus 2.4 mg/L, p< 0.0001), LDH (176 versus 195 U/L, p< 0.0001), and serum calcium (2.2 versus 2.3 mmol/L, p< 0.0001) were increased. In comparison, NLR (3.0 versus 1.6 × 103/μL, p < 0.0001), PLT levels (199 versus 152 × 103/μL, p < 0.0001), and SIRI (1.04 versus 0.53, p< 0.0001) were decreased after transplant. The results are shown in Figure 3.
 |
Table 2 Median, Upper (75%), and Lower (25%) Quartiles for Neutrophil, Lymphocytes, NLR, Monocytes, HGB, PLT, MCV, LMR, ALB, LDH, Creatinine, Blood Calcium, and β2-MG on Day −5 and Day +90 |
Predictive Impact of Pre-and Post-ASCT Laboratory Tests
We then analyzed the impact of both pre-and post-ASCT ANC, ALC, AMC, NLR, ALB, LDH, and Blood calcium on PFS. First, we found that neither pre- nor post-ASCT ALC, ALB, LDH, or serum calcium predicted PFS. In addition, the day −5 ANC (p = 0.9), ALC (p = 0.9), NLR (p = 0.9), and LDH (p=0.2), did not predict PFS. But a low AMC (p=0.0014; Figure 4A), albumin (p=0.0055; Figure 4B), serum calcium (p=0.02; Figure 4C), and SIRI<1.56 (P=0.03; Figure 4D) can be predicted for superior PFS. At Day 90 post-ASCT, a high ANC (p = 0.0078; Figure 4E) and LMR (p =0.02; Figure 4F), a low NLR (p =0.016; Figure 4G) and SIRI<0.41 (P=0.02; Figure 4H) can be predicted for superior PFS, while the AMC and ALC had no impact on PFS. Accordingly, FISH results were used to categorize patients by high-risk and low-risk and examined their relationship with PFS (Figure 5).
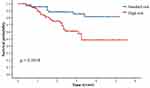 |
Figure 5 Comparison of PFS in patients with ASCT among standard risk and high risk. |
Univariable and Multivariable Analysis for PFS Before or After ASCT
In our univariate and multivariate analyses, Cox’s proportional hazards model was used to investigate the influence of other prognostic factors on PFS (Tables 3 and 4). A comprehensive analysis of the entire cohort indicated that patient PFS was significantly related to their ISS stage, NLR, and LMR after ASCT (p = 0.001, p < 0.0001, p = 0.004). These and other potential confounding factors were included in a multivariate analysis, which yielded the following findings: the ISS stage and NLR were independently associated with superior PFS (hazard ratio (HR) 2.52, 95% CI 1.32–4.78, p = 0.005; HR 3.93, 95% CI 2.18–7.09, p <0.0001). We have also developed a nomogram and further performed internal validation and calibration curves, as detailed in the Supplementary Materials.
 |
Table 3 Univariable and Multivariable Analysis for PFS Before ASCT |
 |
Table 4 Univariable and Multivariable Analysis for PFS After ASCT |
Discussion
It is currently the second most common hematological malignant tumor after leukemia. Multiple myeloma (MM) is a malignancy of plasma cells. MM patients newly diagnosed with the disease can benefit from the combination of proteasome inhibitors and/or immunomodulatory drugs combined with ASCT.15 MM prognosis remains difficult to predict, especially in post-ASCT settings because of considerable variability in survival rates. While existing diagnostic tools, such as the revised International Staging System (R-ISS), incorporate tumor cytogenetics and tumor load as factors, they cannot provide specific prognostic predictions post-ASCT. Further, alternative methods to predict disease progression after ASCT, such as minimal residual disease assessment (MRD) and positron emission tomography (PET), are both expensive and time-consuming.16–18 Here, we analyzed laboratory data from patients before and after transplantation. Our study was to find laboratory indicators that predict progression after ASCT for NDMM patients.
Even though ASCT is the standard treatment for NDMM patients, ASCT is not curative, and progressions and relapses are common even if CR is attained after transplant.19
There were complex reasons for their relapse. Studies by the International Myeloma Working Group have shown that disease stage, poor response to chemotherapy, and lack of maintenance therapy after transplantation are associated with relapse. Of course, one possible factor is related to resistance to bortezomib, a commonly used proteasome inhibitor in the treatment of MM.20 The mechanism of bortezomib is inhibition of the intracellular protein degradation pathway alters the levels of several intracellular regulatory and signaling proteins, effectively altering downstream cellular processes in a manner that leads to apoptosis or growth arrest.21 Bortezomib also has been reported to have some potential side effects that involve several systems, including the gastrointestinal, hematological, nervous, and musculoskeletal systems.22 Due to proteasome inhibitors are currently used to treat MM, most MM patients demonstrate drug-resistant relapse following long-term treatment. Consequently, the development of new therapeutic strategies, such as combination therapies, that overcome bortezomib resistance is urgently needed. A study suggested that treatment with bortezomib and hydroxychloroquine prevents the pro-angiogenic effect of bortezomib, the proliferation of a small residual tumor PC clone, and thus the relapse.8
A myeloma microenvironment can enhance myeloma cell growth and survival and contribute to drug resistance.23 A study of the tumor microenvironment revealed that inflammation plays a critical role in tumor occurrence, growth, and development.24 Previous studies have suggested that SIRIs like NLR and MLR contribute to tumorigenesis, development, and prognosis.25 Inflammatory markers have been shown to predict the outcome of different cancers, including non-small cell lung cancer, cervical cancer, and NDMM.26,27 The inflammatory microenvironment is closely linked to inflammatory cells.28 There has been an increase in attention to systemic inflammatory markers in MM in recent years (NLR, PLR, and LMR/MLR). The LMR is indicative of the equilibrium between host immunity and the tumor environment. Various studies have demonstrated the significance of LMR in predicting patient outcomes at different stages, including diagnosis, and early treatment.29,30 In previous studies, NLR was an independent prognosticator for gastric cancer and other diseases.31 There is a meta-analysis showing that elevated NLR and decreased LMR predict poor OS/PFS in patients with NDMM. Immune responses are mediated by lymphocytes, a cellular component of the body. Patients with low lymphocyte counts have a suppressed immune system, which can negatively impact their prognosis for various types of cancer.25 According to recent studies, LMR plays a critical role in MM survival. A significant difference in PFS and OS was observed between NDMM patients treated with bortezomib between the low and high LMR groups.32,33 In our study, we also found that these inflammatory markers can predict the prognosis of multiple myeloma after ASCT.
This study has potential limitations. The study included a limited number of patients. Although good internal verification results were obtained, the present study could not be externally verified due to the small number of cases. Second, this was a retrospective study that was conducted at a single center, so its representativeness may be limited. In our study, the longest follow-up period was 63 months, and obtaining long-term stable prediction results may require a longer follow-up period. In the future, we should conduct a multicenter investigation with a larger number of patients to validate our findings and explore the relationship between relapse mechanisms and drugs.
Conclusion
In conclusion, our results suggest that ANC, NLR, SIRI, and LMR are a series of inflammation-related indicators, that are readily available and inexpensive and can be considered as potential biomarkers for predicting PFS of MM underwent ASCT.
Funding
This study was supported by the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZYLX202137) and Beijing Chaoyang Hospital Science and Technology Innovation Fund (grant numbers 22kcjjzd-7).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang S, Xu L, Feng J, et al. Prevalence and incidence of multiple myeloma in urban area in china: a national population-based analysis. Front Oncol. 2020;9:1513. doi:10.3389/fonc.2019.01513
2. Liu W, Liu J, Song Y, et al. Mortality of lymphoma and myeloma in China, 2004–2017: an observational study. J Hematol Oncol. 2019;12(1):22. doi:10.1186/s13045-019-0706-9
3. Palumbo A, Cavallo F, Gay F, et al. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med. 2014;371(10):895–905. doi:10.1056/NEJMoa1402888
4. van de Donk NW, van der Holt B, Minnema MC, et al. Thalidomide before and after autologous stem cell transplantation in recently diagnosed multiple myeloma (HOVON-50): long-term results from the Phase 3, randomized controlled trial. Lancet Haematol. 2018;5(10):e479–e492. doi:10.1016/S2352-3026(18)30149-2
5. Martinez-Lopez J, Blade J, Mateos MV, et al. Long-term prognostic significance of response in multiple myeloma after stem cell transplantation. Blood. 2011;118(3):529–534. doi:10.1182/blood-2011-01-332320
6. Samer A, Bashir Q, Denái R, et al. Long-term survival for myeloma after autologous stem cell transplantation. Blood. 2020;136(Supplement 1):23–24.
7. Minakata D, Fujiwara SI, Murahashi R, et al. Relationship of tumor load parameters before and after autologous stem cell transplantation with clinical prognosis in transplant-eligible patients with multiple myeloma: a retrospective analysis. Leuk Res. 2022;112:106750. doi:10.1016/j.leukres.2021.106750
8. Di Lernia G, Leone P, Solimando AG, et al. Bortezomib treatment modulates autophagy in multiple myeloma. J Clin Med. 2020;9(2):552. doi:10.3390/jcm9020552
9. Zhang X, Duan J, Wen Z, et al. Are the derived indexes of peripheral whole blood cell counts (NLR, PLR, LMR/MLR) clinically significant prognostic biomarkers in multiple myeloma? A systematic review and meta-analysis. Front Oncol. 2021;11:766672. doi:10.3389/fonc.2021.766672
10. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21–33. doi:10.4065/78.1.21
11. Sun C, Ye JN, Wang H, et al. Prognostic value of red blood cell distribution width in senile patients with non-transplanted multiple myeloma. Zhong guo Shi Yan Xue Ye Xue Za Zhi. 2019;27:115–122.
12. Kelkitli E, Atay H, Cilingir F, et al. Predicting survival for multiple myeloma patients using baseline neutrophil/lymphocyte ratio. Ann Hematol. 2014;93(5):841–846. doi:10.1007/s00277-013-1978-8
13. Sweiss K, Calip GS, Johnson JJ, Rondelli D, Patel PR. Pretransplant hemoglobin and creatinine clearance correlate with treatment-free survival after autologous stem cell transplantation for multiple myeloma. Bone Marrow Transplant. 2019;54(12):2081–2087. doi:10.1038/s41409-019-0628-8
14. Plasma Cell Disease Group. Chinese Society of Hematology, Chinese Medical Association, Chinese Myeloma Committee-Chinese Hematology Association. Chinese guidelines of autologous stem cell transplantation for multiple myeloma (2021). Chin J Hematol. 2021;42:353–357. doi:10.3760/cma.j.issn.0253-2727.2021.05.001
15. Shah JJ, Stadtmauer EA, Abonour R, et al. Carfilzomib, pomalidomide, and dexamethasone for relapsed or refractory myeloma. Blood. 2015;126(20):2284–2290. doi:10.1182/blood-2015-05-643320
16. Munshi NC, Avet-Loiseau H, Rawstron AC, et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 2017;3(1):28–35. doi:10.1001/jamaoncol.2016.3160
17. Moreau P, Attal M, Caillot D, et al. Prospective evaluation of magnetic resonance imaging and [18F] fluorodeoxyglucose positron emission tomography-computed tomography at diagnosis and before maintenance therapy in symptomatic patients with multiple myeloma included in the IFM/DFCI 2009 trial: results of the IMAJEM study. J Clin Oncol. 2017;35(25):2911–2918. doi:10.1200/JCO.2017.72.2975
18. Podar K, Chauhan D, Anderson KC. Bone marrow microenvironment and the identification of new targets for myeloma therapy. Leukemia. 2009;23(1):10–24. doi:10.1038/leu.2008.259
19. Al Hamed R, Bazarbachi AH, Malard F, et al. Current status of autologous stem cell transplantation for multiple myeloma. Blood Cancer J. 2019;9(4):44. doi:10.1038/s41408-019-0205-9
20. Kumar SK, Dispenzieri A, Fraser R, et al. Early relapse after autologous hematopoietic cell transplantation remains a poor prognostic factor in multiple myeloma but outcomes have improved over time. Leukemia. 2018;32(4):986–995. doi:10.1038/leu.2017.331
21. Ludwig H, Khayat D, Giaccone G, et al. Proteasome inhibition and its clinical prospects in the treatment of hematologic and solid malignancies. Cancer. 2005;104(9):1794–1807. doi:10.1002/cncr.21414
22. Kane RC, Bross PF, Farrell AT, et al. Velcade: u.S. FDA approval for the treatment of multiple myeloma progressing on prior therapy. Oncologist. 2003;8(6):508–513. doi:10.1634/theoncologist.8-6-508
23. Dolan RD, Laird BJA, Horgan PG, et al. The prognostic value of the systemic inflammatory response in randomised clinical trials in cancer: a systematic review. Crit Rev Oncol Hematol. 2018;132:130–137. doi:10.1634/theoncologist.8-6-508
24. Tokunaga R, Sakamoto Y, Nakagawa S, et al. Comparison of systemic inflammatory and nutritional scores in colorectal cancer patients who underwent potentially curative resection. Int J Clin Oncol. 2017;22(4):740–748. doi:10.1007/s10147-017-1102-5
25. Zhao QT, Yuan Z, Zhang H, et al. Prognostic role of platelet to lymphocyte ratio in non-small cell lung cancers: a meta-analysis including 3720 patients. Int J Cancer. 2016;139(1):164–170. doi:10.1002/ijc.30060
26. Chao B, Ju X, Zhang L, Xu X, Zhao Y. A novel prognostic marker Systemic Inflammation Response Index (SIRI) for operable cervical cancer patients. Front Oncol. 2020;10:766. doi:10.3389/fonc.2020.00766
27. Ren L, Xu J, Li J, et al. A prognostic model incorporating inflammatory cells and cytokines for newly diagnosed multiple myeloma patients [published online ahead of print, 2023 Jan 13]. Clin Exp Med. 2023. doi:10.1007/s10238-023-00992-8.
28. Chauhan D, Singh AV, Brahmandam M, et al. Functional interaction of plasmacytoid dendritic cells with multiple myeloma cells: a therapeutic target. Cancer Cell. 2009;16(4):309–323. doi:10.1016/j.ccr.2009.08.019
29. Suzuki K, Nishiwaki K, Nagao R, et al. Clinical significance of the lymphocyte-to-monocyte ratio in multiple myeloma patients with negative minimal residual disease: a single-center retrospective analysis. Int J Hematol. 2021;114(5):599–607. doi:10.1007/s12185-021-03201-y
30. Sweiss K, Lee J, Mahmud N, et al. Combined immune score of lymphocyte to monocyte ratio and immunoglobulin levels predicts treatment-free survival of multiple myeloma patients after autologous stem cell transplant. Bone Marrow Transplant. 2020;55(1):199–206. doi:10.1038/s41409-019-0681-3
31. Sun J, Chen X, Gao P, et al. Can the neutrophil to lymphocyte ratio be used to determine gastric cancer treatment outcomes? A systematic review and meta-analysis. Dis Markers. 2016;2016:7862469. doi:10.1155/2016/7862469
32. Romano A, Laura Parrinello N, Cerchione C, et al. The NLR and LMR ratio in newly diagnosed MM patients treated upfront with novel agents. Blood Cancer J. 2017;7(12):649. doi:10.1038/s41408-017-0019-6
33. Dosani T, Covut F, Beck R, Driscoll JJ, de Lima M, Malek E. Significance of the absolute lymphocyte/monocyte ratio as a prognostic immune biomarker in newly diagnosed multiple myeloma. Blood Cancer J. 2017;7(6):e579. doi:10.1038/bcj.2017.60
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


