Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Changes in Clinical Management of Patients with Schizophrenia Treated with Long-Acting Injectable Antipsychotics (LAIs), Including Telepsychiatry Use, During the COVID-19 Pandemic
Authors Haider B, O'Sullivan AK, Bessonova L, Keane E, Achtyes E , Harvey PD, Kane JM , Saklad SR , Trotter JP, Claxton A, Polak T, McGrory J, Noori W, Sikora Kessler A, Yarlas A, Velligan D
Received 29 October 2022
Accepted for publication 17 February 2023
Published 17 March 2023 Volume 2023:19 Pages 623—634
DOI https://doi.org/10.2147/NDT.S394220
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Batool Haider,1 Amy K O’Sullivan,1 Leona Bessonova,1 Elizabeth Keane,1 Eric Achtyes,2 Philip D Harvey,3 John M Kane,4 Stephen R Saklad,5 Jeffrey P Trotter,6 Amy Claxton,1 Tiffany Polak,1 James McGrory,1 Wahidullah Noori,1 Asia Sikora Kessler,7 Aaron Yarlas,7 Dawn Velligan8
1Alkermes, Inc, Waltham, MA, USA; 2Cherry Health and the Michigan State University College of Human Medicine, Grand Rapids, MI, USA; 3University of Miami Miller School of Medicine, Miami, FL, USA; 4The Zucker Hillside Hospital, Glen Oaks, NY, USA; 5College of Pharmacy, University of Texas at Austin, Pharmacotherapy Division, San Antonio, TX, USA; 6Worldwide Clinical Trials, Research Triangle, NC, USA; 7QualityMetric Incorporated, LLC, Johnston, RI, USA; 8University of Texas Health Science Center at San Antonio, San Antonio, TX, USA
Correspondence: Batool Haider, Alkermes, Inc, 852 Winter Street, Waltham, MA, 02451-1420, USA, Tel +1 781 609 6035, Email [email protected]
Purpose: The COVID-19 pandemic substantially impacted care of patients with schizophrenia treated with long-acting injectable antipsychotics (LAIs). This study (OASIS-MAPS) examined how clinical sites adapted operations and used telepsychiatry to maintain standard of care for these patients during the pandemic.
Methods: Two online surveys (initial: October–November 2020, N = 35; follow-up: July–September 2021, N = 21) were completed by a principal investigator (PI) or PI-appointed designee at sites participating in the OASIS study (NCT03919994). Survey responses were analyzed descriptively.
Results: At the time of the initial survey, all 35 participating sites were using variants of telepsychiatry, with 20 sites adopting it after the pandemic started. Most sites reported no negative impacts of the pandemic on medication adherence, although approximately 20% of sites reported decreased adherence for LAIs. Twelve sites (34%) reported switching patients with schizophrenia from LAIs to oral antipsychotic medications, while 11 sites (31%) reported switching patients from shorter to longer injection interval LAIs during the pandemic. Most sites did not experience difficulties in implementing or expanding telepsychiatry services, although lower reimbursement rate for telepsychiatry and patients’ lack of access to and training on relevant technologies were the most frequently reported barriers.
Conclusion: Changes made by sites after the pandemic onset were viewed by almost all participants as satisfactory for maintaining standard of care. Almost all participants thought that the use of telepsychiatry services would continue after the pandemic in a hybrid manner combining telepsychiatry and office visits. Ensuring that patients have equitable access to telepsychiatry will be important in the post-pandemic future.
Keywords: telehealth, coronavirus, care management, medication adherence
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the SARS-CoV-2 virus, significantly impacted non-COVID health care for patients with physical and mental health conditions. One effect on health care providers (HCPs) was the need to reduce the number of on-site clinic visits to accommodate public health policies including social distancing. On-site visits to HCPs decreased by almost 60% in the United States (US) during the early period of the pandemic (ie, mid-March to late-May 2020).1,2 To maintain patients’ care, HCPs increasingly adopted telemedicine, which uses a technology-based platform to deliver care virtually,3 for communicating with patients remotely.1
Patients with serious mental illnesses (SMIs) have been disproportionately affected by the pandemic due to disparities in access to health care, social inequalities, and unhealthy behaviors (eg, smoking).4 Incidence of COVID-19 is higher in patients with schizophrenia or other SMIs compared to those without psychiatric diagnoses.5–7 Patients with schizophrenia who are infected with COVID-19 are at a higher risk of hospitalization and death than the general population.7–10 Survey studies have found that patients with SMIs report higher anxiety, stress, and depression, and worse behavioral responses (eg, weight gain, sleep disruption) as a result of the pandemic.11–13 Continuity of pharmacologic and psychosocial care for these patients is critical to reduce the likelihood of relapse, hospitalization, or other negative outcomes such as suicide.14–17
Pre-pandemic research identified telemedicine as a viable strategy for communication between HCPs and patients with schizophrenia.18–20 Non-adherence to antipsychotic medications, a well-documented problem for this patient population,15,21 was improved in those who received telemedicine services.22,23
Long-acting injectable antipsychotics (LAIs) are an effective treatment for schizophrenia, as they are associated with improvements in medication adherence,24,25 compared to oral antipsychotics (OAPs). However, because LAIs require administration by an HCP at regular intervals, typically during on-site visits, the pandemic introduced unique challenges for LAI administration.26,27 For example, patients treated with LAIs were at risk of missing doses due to office closures, or when they had to quarantine after contracting or being exposed to COVID-19.26 Although no best practice guidance exists for use of LAIs during the pandemic, a variety of strategies such as utilizing LAIs with longer injection intervals, at-home LAI administration by a visiting HCP, or switching patients to OAPs are methods that have been employed to help ensure continuity of care.28,29
Given the numerous obstacles to maintaining continuity of care during the pandemic, it is essential to understand how clinical facilities have adapted their services to continue supporting patients with schizophrenia. The objective of this study was to capture HCPs’ perspectives on the impact of the COVID-19 pandemic on management of patients with schizophrenia, particularly those treated with LAIs, and the role of telepsychiatry in managing care for these patients.
Materials and Methods
Study Design and Procedures
The Observational Study of LAIs in Schizophrenia: Impact of COVID-19 Pandemic on Outpatient LAI Management and Use of Telepsychiatry for Patients with Schizophrenia (OASIS-MAPS) was an observational, online survey sub-study of the OASIS cohort study (NCT03919994). The objectives of the ongoing parent OASIS study are to describe demographic, clinical, and socioeconomic characteristics, as well as treatment patterns, clinical, economic, and patient-reported outcomes among patients who were newly prescribed a second-generation LAI at behavioral health clinics in the US over a 12-month period.
For the OASIS-MAPS sub-study, HCPs at participating OASIS sites received two surveys (an initial survey administered October 7 – November 2, 2020, and a follow-up survey administered July 28 – September 9, 2021; Supplemental Surveys 1 and 2, respectively) asking about the pandemic’s impact on the provision of health care at their sites. Pre-survey screening established that individuals met study eligibility criteria: a principal investigator (PI), or PI-appointed designee, who was also a prescribing clinician; was employed at the site for at least one year; and was sufficiently knowledgeable about the pandemic’s impact on site operations. Only one individual per site was eligible to participate in each survey.
Initial survey participants were recruited from each of the 50 sites active in OASIS at the time of data collection. Follow-up survey participants were recruited from among the 35 sites that completed the initial survey. If the initial survey participant was unable to complete the follow-up survey, another eligible individual at that site could participate. Upon completion of the initial survey, the site received a $50 honorarium. No honorarium was provided for completion of the shorter follow-up survey. Selected site characteristics (eg, geographic location, site type) were linked to participants via a Site ID.
All participants in both the initial and the follow-up surveys provided electronic consent, which included acknowledgement that de-identified responses may be published or presented.
Study materials were submitted for review to the Sterling Institutional Review Board (IRB; www.sterlingirb.com), which indicated that the study was exempt under Category 2(ii).30 Because the initial survey met study exemption, the follow-up survey was not submitted for IRB review.
Survey Content
All initial and follow-up survey items were uniquely developed by health outcomes measurement researchers with input from expert clinicians to capture the concepts set out in the study objectives. The initial survey focused on gathering insight into the pandemic’s impact on site operations and patient care, including changes in prescribing patterns, and perceived impact on patients’ medication adherence. This survey also collected information about telepsychiatry services, including changes in frequency of use and acquisition of new technologies during the pandemic, as well as impressions of the service’s capability and predictions for its use post-pandemic. The follow-up survey elicited more detailed information as to how prescribing patterns for patients with schizophrenia changed during the pandemic, including factors considered when switching treatment regimens, and types of treatment changes HCPs were willing to make based solely on communication with patients via telepsychiatry. Lastly, participants were asked about differential reimbursement rates for telepsychiatry and on-site visits, and if this affected willingness to utilize telepsychiatry. Only two participants indicated awareness of differential reimbursement rates, so results from these latter items are not reported here.
Most survey items were closed-ended (eg, choosing from among multiple listed response options; indicating degree of agreement with a statement on a Likert-type scale). Three open-ended items in the initial survey asked participants to provide free-text responses.
Data Analysis
Descriptive univariate analyses were conducted for responses to all closed-ended items. Categorical variables were summarized and reported as frequencies and percentages (only frequencies are reported wherever data for a subgroup of sites are presented), while continuous variables were summarized and reported as means and standard deviations (SDs). Responses to open-ended items were not formally analyzed; rather, selected quotations that inform findings are reported here.
No hypotheses were tested, and no inferential statistics, including those representing associations among variables, were calculated.
Results
Site and Participant Characteristics
Site characteristics for the initial and the follow-up surveys appear in Table 1. Participants at 35 of the 50 active OASIS sites completed the initial survey. Fifteen of these 35 sites (43%) were in the Southern region of the US, and 21 (60%) were in an urban setting. Nearly all sites identified as either independent/private practices (n = 16, 46%) or community mental health clinics (CMHCs; n = 17, 49%). Twenty-one of the 35 sites completed the follow-up survey (60%). Site characteristics for the subset of sites that completed the follow-up survey were similar to those of the full sample (Table 1).
 |
Table 1 Characteristics of Participating Sites for Initial and Follow-Up Surveys |
Participant characteristics for both the initial and the follow-up surveys appear in Table 2. Ten participants completed both surveys; different individuals completed the initial and follow-up surveys at 11 of 21 sites. Participant characteristics were similar across the two surveys.
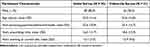 |
Table 2 Characteristics of Initial and Follow-Up Survey Participants |
Findings from the Initial Survey
Impact of the COVID-19 Pandemic on Site Operations
Table 3 reports the most frequently cited impacts of the pandemic by the participants. The most frequently reported impacts were increased safety precautions (eg, providing masks, hand sanitizer, and/or other personal protective equipment [PPE]) and procedural changes for office visits to adhere to governmental guidelines (n = 30, 86% each).
 |
Table 3 Impact of the COVID-19 Pandemic on Participants’ Sites (N = 35) |
Strategies for Maintaining Continuity of Care for Patients During the COVID-19 Pandemic
All but one site reported implementing or expanding telepsychiatry services (n = 34, 97%) to maintain continuity of care for patients with schizophrenia treated with LAIs during the COVID-19 pandemic. Some sites did adopt other strategies including patient referral to off-site locations (eg, pharmacies, “minute clinics”; n = 2), and establishing a drive-thru clinic (n = 1) or in-home visits (n = 1).
Impact of the COVID-19 Pandemic on Prescribing Patterns and Medication Adherence
Approximately one-third of sites reported switching patients with schizophrenia from LAIs to OAPs (n = 12, 34%). A similar number of sites reported switching patients from shorter to longer injection interval LAIs (n = 11, 31%).
More sites perceived that medication adherence was unchanged for patients treated with LAIs (n = 21, 60%) than for those treated with OAPs (n = 15, 43%). Decreased medication adherence was reported by eight sites (23%) for patients treated with LAIs and 11 sites (31%) for those treated with OAPs. Among the eight sites reporting decreased medication adherence for LAIs, the most frequently reported reasons were decreased injection visits due to patients not wanting to leave their homes (n = 6) or reduced clinic hours (n = 4). Some of these sites reported adopting the following measures to improve medication adherence: educating patients on reducing exposure to COVID-19 when leaving their homes (n = 5), providing alternate sites for LAI administration (n = 3), assisting patients with transportation (n = 3), providing patients with PPE (n = 3), and switching patients from LAIs to OAPs (n = 4).
The following quotes provide more insight into how participants viewed the pandemic’s impact on medication adherence at their sites:
- “All patients are seen via telemedicine on a monthly basis to ensure stability and medication adherence.”
- “Transportation is always a major barrier for our SMI clients, but clients missing LAIs has become more common.”
- “We have had good adherence by calling the patients to remind them even though they receive a reminder by email or text automatically.”
Implementation and Use of Telepsychiatry Services Before and After the Start of the COVID-19 Pandemic
All 35 sites reported using telepsychiatry during the pandemic. Among the 15 sites (43%) using telepsychiatry pre-pandemic, 13 expanded telepsychiatry services after the pandemic started. The remaining 20 sites (57%) adopted telepsychiatry only after pandemic onset.
Prior to the pandemic, an average of 12–15% of outpatient visits among all patients at participating sites occurred via telepsychiatry (Figure 1). During the pandemic, however, the proportion of telepsychiatry visits increased, ranging from 45%–69% across outpatient visit types. Routine visits experienced the largest increase, for which the use of telepsychiatry increased from 15% pre-pandemic to 69% after pandemic onset.
 |
Figure 1 Percentage of outpatient visits using telepsychiatry before and during the COVID-19 pandemic across sites (N = 35). |
Among the sites treating patients with schizophrenia, 28 (80%) utilized telepsychiatry for patients treated with LAIs, while 34 (97%) used telepsychiatry for those treated with OAPs. Sixteen sites (46%) increased use of telepsychiatry for patients treated with LAIs after pandemic onset, while 26 (74%) did so for patients treated with OAPs.
A differential impact of the pandemic on the frequency of “no shows” and/or cancellations among patients with schizophrenia treated with LAIs was observed for in-person and telepsychiatry visits. Twenty percent of sites (n = 7) observed an increase in the frequency of “no shows” and/or cancellations for in-person crisis visits, and 37% of sites (n = 13) observed the same increase for in-person new patient visits. Regarding telepsychiatry visits, 29% of sites (n = 10) reported a decrease in “no shows” and/or cancellations for treatment initiation visits, and 34% of sites (n = 12) reported the same for routine visits.
The most common modalities sites used for telepsychiatry visits with patients with schizophrenia treated with LAIs were audio only (eg, telephone; n = 33, 94%) and combined audio with video (eg, online teleconferencing; n = 31, 89%). Most sites (n = 24, 69%) purchased new technology and/or equipment after pandemic onset to facilitate telepsychiatry visits. A larger number of CMHCs (n = 11) reported such changes than independent/private practices (n = 8).
Most participants agreed that telepsychiatry visits were suitable for managing many aspects of care for patients with schizophrenia treated with LAIs (Figure 2), including side effect management, prescription of new antipsychotics, and patient care management.
 |
Figure 2 Percentages of sites reporting ability of telepsychiatry to provide a service (N = 35). Abbreviations: AP, antipsychotic; LAI, long-acting injectable. |
Barriers for Implementation and Use of Telepsychiatry Services
Participants reported experiencing some barriers to implementing or utilizing telepsychiatry services (Figure 3). The most frequently reported barriers (moderately or extremely limiting) were financial (ie, reimbursement rates, costs of implementation), and were reported by approximately 31% and 29% of sites, respectively.
 |
Figure 3 Site/system-related barriers for implementation and use of telepsychiatry services (N=35). Abbreviations: EMR, electronic medical record; IT, information technology. |
Participants also reported patient-related barriers to implementing or utilizing telepsychiatry services among patients with schizophrenia treated with LAIs (Figure 4). The most reported patient-related barriers were lack of internet/technology access (74%) and lack of technology training (60%).
 |
Figure 4 Patient-related barriers for implementation and use of telepsychiatry services (N=35). |
When asked how to overcome patient-related barriers to telepsychiatry, the approaches participants most frequently endorsed were to improve patients’ comfort with telepsychiatry (n = 22, 63%), to assist patients in acquiring access to needed technology (n = 19, 54%), and to train patients to use this technology (n = 18, 51%).
Predictions for Use of Telepsychiatry in Post-Pandemic Health Care
Almost all survey participants (n = 33, 94%) predicted their sites would employ a hybrid approach that combines in-person and telepsychiatry visits after the pandemic has ended.
The following quotes provide more insight into participants’ predictions regarding how telepsychiatry would be used at their sites post-pandemic:
- “We already have had a full-time telepsychiatry provider off site, and onsite providers have gone to [a] hybrid onsite and telework model. I am not sure if onsite providers will remain hybrid after the pandemic, but this has seemingly been a successful model so far.”
- “I will still do my own LAI injections in person. My preference will be for all appointments to be in office, but I would be willing to make exceptions now, as long as insurance will reimburse for the visit.”
Participants’ Satisfaction with Continued Care of Patients During the COVID-19 Pandemic
The vast majority of participants (n = 33, 94%) indicated satisfaction with using telepsychiatry to support patients with schizophrenia treated with LAIs.
The following quotes provide more insight into how participants viewed their sites’ abilities to support patients with schizophrenia treated with LAIs during the COVID-19 pandemic:
- “COVID-19 has hastened our adoption/expansion of telehealth services, especially in populations we may have considered the best candidates. We are happy with the success we have encountered.”
- “The COVID-19 pandemic has been without a doubt a big challenge for our practice and our patients. However, we have been able to maintain constant communication with our patients over the phone or virtual calls in order to guarantee their safety and their well-being.”
Follow-Up Survey
Impact of the COVID-19 Pandemic on Prescribing Patterns
Sixteen of the 21 sites that participated in the follow-up survey reported switching patients from an LAI to an OAP. Nine sites reported switching patients from a shorter to a longer injection interval LAI. However, at sites where these changes were made, they were typically made for a small proportion of patients: the median estimated percentage of patients who had been switched from LAIs to OAPs was 10%. The median estimated percentage of patients switched from a shorter to a longer injection interval LAI was also 10%.
Factors related to insurance coverage had the largest influences on decisions to switch patients from LAIs to OAPs at the 16 sites where such switches occurred. Six sites each reported being influenced by increased affordability of OAPs relative to LAIs due to changes in insurance coverage and by changes in insurance approval processes that made prescribing LAIs more difficult. Additionally, five sites reported switching to reduce the need for patients to leave their homes to attend on-site injection visits.
Six of the nine sites reported switching patients to longer injection interval LAIs for the purpose of limiting patients’ need to attend in-person injection visits. No other listed reasons for switching were endorsed by more than one site.
Use of Telepsychiatry Services After the Start of the COVID-19 Pandemic
Sixteen of the 21 follow-up survey participants were willing to make treatment decisions about antipsychotic medications (eg, starting a new treatment, switching a patient from LAI to OAP medication or vice-versa) for patients with schizophrenia based solely on telepsychiatry visits for established patients, while 14 participants were willing to make these types of decisions for new patients.
Between seven and 15 of the 21 participants indicated a willingness to make several treatment decisions based solely on telepsychiatry. These decisions included switching patients from an LAI to an OAP, or vice versa, that uses the same medication; switching from an LAI to an OAP, or vice versa, that uses a different medication; switching from an OAP to a different OAP or from an LAI to a different LAI; prescribing an OAP or LAI to a new patient; and adding/removing an antipsychotic medication to/from a patient’s current regimen (Supplemental Table 1).
Factors for making treatment decisions based solely on telepsychiatry visits considered by more than half of sites included efficacy and side effects experienced by the patient (n = 15 and n = 16, respectively), the duration of the treatment regimen (n = 15), and the patient’s symptom severity (n = 15), while issues related to insurance coverage were cited by one-third or fewer sites (Supplemental Table 2).
Discussion
This study provides a firsthand account from experienced, practicing behavioral health professionals of the COVID-19 pandemic’s impact on continued care of patients with schizophrenia being treated with LAIs in the US. Clinicians at all 35 sites that participated in this survey study reported using telepsychiatry services to care for patients with schizophrenia during the COVID-19 pandemic. The majority began using telepsychiatry services as a direct result of the pandemic, while sites that used telepsychiatry pre-pandemic expanded its use. Most sites reported no negative impact of the pandemic on medication adherence for patients treated with antipsychotic medications, with decreased adherence reported by only 23% of sites for LAIs and 31% of sites for OAPs. Most sites did not experience difficulties implementing or expanding telepsychiatry services. Insurance coverage and patient access to and training on relevant technologies were the most frequently reported barriers. Survey participants found telepsychiatry helpful for almost all aspects of care, and almost all predicted that use would continue in a hybrid manner with on-site visits after the pandemic ends.
The majority of participants in the current study reported that medication adherence in patients treated with LAIs was not negatively impacted by the pandemic. This finding is consistent with evidence from a clinical site in Pennsylvania where the number of LAI administrations remained consistent before and after the State of Emergency declared on March 13, 2020.31 Thus, while there were some cases of changing treatment regimens in that study, like in the current study, in most cases prescribing physicians continued to use LAIs, leaving medication adherence largely unaffected.
Remote care of patients treated with LAIs may be challenging, as LAIs typically require administration by an HCP on a fixed schedule. Patients’ decreased willingness or ability to attend on-site visits for injections to reduce risk of COVID-19 exposure and a lack of alternative options for in-person injections (eg, drive-through clinics) were cited as reasons for clinicians switching patients from LAIs to OAPs or to longer injection interval LAIs, both of which require fewer on-site visits. Results from the initial survey (approximately seven to eight months following the start of the pandemic) indicated that one-third of sites switched patients with schizophrenia from LAIs to OAPs. Similar estimates were reported for sites switching patients from shorter to longer injection interval LAIs. Although these practices were likely due to the unique circumstances of the COVID-19 pandemic and appearance of new variants over the course of the pandemic, increased availability of alternate locations (such as pharmacies) for injection administration in general may help ensure continuity of care and increase medication accessibility for patients treated with LAIs.
Participants described some of the significant site/system-related barriers to telepsychiatry implementation, namely related to lower reimbursement rates for telepsychiatry visits, and costs to implement and support telepsychiatry services. Furthermore, reimbursement issues were partially mitigated with national healthcare policy changes, such as the Centers for Medicare and Medicaid Services’ mandated parity in reimbursement between telemedicine and in-person visits on April 1, 2020.32 Reimbursement policies for telepsychiatry have evolved since the beginning of the pandemic and vary by payer type (public vs private); for Medicaid, these policies also vary by state.33 Despite reported site/system-related barriers in the current study, HCPs were largely satisfied with the use of telepsychiatry in managing various aspects of patient care. This is consistent with findings from another recent survey of mental health care providers across the US who reported good experience with the use of telepsychiatry.34
Participants also reported on patient-related barriers to utilization of telepsychiatry such as lack of access to technology and need for technological training. Sites implemented strategies to overcome these barriers by working with patients to improve their comfort with the modality and to provide training on best telepsychiatry practices. Very few participants thought that patients’ distrust or unwillingness to use technology was a barrier to using telepsychiatry. This is consistent with findings from a previous survey in which the majority of patients with schizophrenia reported interest in online meetings with their HCPs,35 as well as findings from a recent review reporting high acceptance of videoconferencing from participants with schizophrenia-spectrum disorders.34 Another recent review of 26 studies comparing costs of telepsychiatry services with in-person office visits or usual care for patients with SMIs found that the majority of studies reported telepsychiatry visits to be the less expensive option for patients, primarily due to savings in travel time and expenses and a reduction in lost work time.36 Clinicians’ high satisfaction with telepsychiatry and its perceived acceptability among patients may contribute to the expectation held by nearly all participants that telepsychiatry would continue to be used in patient care, in combination with on-site visits in a hybrid manner, after the pandemic ends.
Since the start of the pandemic, patients, HCPs, researchers, and population health decision-makers have called for an increase in telepsychiatry utilization to ensure continuity of care for patients with SMIs.35,37–40 The current survey findings continue to underscore the need for a hybrid model for patient care, education of patients regarding available treatment options including LAIs for treatment of schizophrenia, and the need for best practice guidelines for telepsychiatry.
This study had several limitations. The relatively small number of participating sites may not be representative of all clinical sites treating patients with schizophrenia and prescribing LAIs, limiting generalizability of findings. The participating sites were also experienced in prescribing LAIs; therefore, less experienced clinical sites and HCPs may have encountered greater barriers in providing patient care and utilizing telepsychiatry during the pandemic. Further, the number of sites within key subgroups was often too small to provide interpretable patterns of data. For example, very few sites were from rural areas or were hospital networks, which limited the ability to interpret data or generalize to other sites with differing characteristics.
Another limitation of this study was that data were self-reported. Despite participants being practitioners with many years of experience at their respective sites, no objective data were collected that might have provided more accurate information to help verify self-reported changes (eg, records of telepsychiatry expenditures or of reimbursement rates by visit type). It was also the case that, for approximately half of the sites that participated in the follow-up survey, the participant was not the same individual who completed the initial survey. While the surveys’ focus was on site operations that would optimally be independent of characteristics specific to the reporting individual, different initial and follow-up survey participants limit the consistency of responses across the two surveys and prevent attempts to link responses and examine changes in these responses over time. Lastly, 60% of the initial survey participants responded to the follow-up survey. Data were not collected on COVID-19-, operational-, or staffing-related differences amongst responding and non-responding sites.
Conclusion
The COVID-19 pandemic has greatly impacted the practice of health care for patients with schizophrenia, including those treated with LAIs. Results of these two surveys found that telepsychiatry was widely used to overcome obstacles introduced by the pandemic, which limited in-person communications between patients and their HCPs. Participants found telepsychiatry to be effective for most aspects of patient care. Almost all participating clinicians thought that the use of telepsychiatry services will continue, even after the pandemic has ended, in a hybrid manner that combines telepsychiatry and in-person office visits. Participating clinicians thus support the use of telepsychiatry in this manner for continuing care of patients with schizophrenia treated with LAIs, both during and after the COVID-19 pandemic. For this to occur, it is essential that patients are provided with equitable access to and support for relevant technologies and equipment to ensure that they can access and benefit from telepsychiatry post-pandemic. Establishing an infrastructure for LAI treatment and administration will be critical to support patient care. Future research on establishing standard practices and guidelines on the use of telepsychiatry is warranted.
Abbreviations
CMHC, Community mental health clinics; COVID-19, Coronavirus disease 2019; HCP, Health care provider; IRB, Institutional Review Board; LAI, Long-acting injectable; OAP, Oral antipsychotic; OASIS-MAPS, Observational Study of LAIs in Schizophrenia: Impact of COVID-19 Pandemic on Outpatient LAI Management and Use of Telepsychiatry for Patients with Schizophrenia; PI, Principal investigator; PPE, Personal protective equipment; SD, Standard deviation; SMI, Serious mental illness; US, United States.
Data Sharing Statement
Data will not be made available because the informed consent forms stated that participants’ individual data would not be shared.
Acknowledgments
The authors would like to thank April Foster, Cory Saucier, Andrew Lovley, and Elizabeth Costa of QualityMetric for their assistance in the development of this manuscript.
Data from this manuscript were presented as an abstract/poster at the American Society of Clinical Psychopharmacology (ASCP) Annual Meeting (held virtually) in May 2021, at the American Psychiatric Association (APA) Annual Meeting in May 2022 (New Orleans, LA), at the Neuroscience Education Institute (NEI) Congress in November 2021 (Colorado Springs, CO), and at Psych Congress in October–November 2021 (San Antonio, TX).
This abstract was published in CNS Spectrums (a publication of NEI 2021) in April 2022. Hyperlink: https://www.cambridge.org/core/journals/cns-spectrums/article/clinical-management-of-patients-with-schizophrenia-treated-with-longacting-injectable-antipsychotics-and-telepsychiatry-use-during-covid19-pandemic/A0ED270A2F14B391FEF8ABB2C7970275. doi:10.1017/S1092852922000256.
Funding
This research was funded by Alkermes, Inc.
Disclosure
Batool Haider, James McGrory, and Elizabeth Keane are employees of Alkermes, Inc., a pharmaceutical company which manufactures products including antipsychotic medications for people with schizophrenia and bipolar I disorder. These authors may be shareholders. Amy K. O’Sullivan, Leona Bessonova, Amy Claxton, Tiffany Polak, and Wahidullah Noori were employees of Alkermes, Inc. at the time this study was conducted. Asia Sikora Kessler and Aaron Yarlas were employees of QualityMetric Incorporated, LLC, a consulting company specializing in health measurement solutions, which was paid by Alkermes, Inc. for assistance in study design, analyses, and manuscript development, at the time this study was conducted. Eric Achtyes has consulted or served on advisory boards for Alkermes Inc., and has received research grants and/personal fees from Alkermes, Inc, Biogen, Boehringer Ingelheim, Janssen, Neurocrine Biosciences, Takeda, Atheneum, Karuna, Lundbeck, Otsuka, Sunovion, Teva; briefly owned stock from AstraZeneca, Johnson and Johnson, Moderna, and Pfizer, outside the submitted work. Philip D. Harvey, John M. Kane, Stephen R. Saklad, and Dawn Velligan have served as paid consultants for Alkermes, Inc. Philip D. Harvey reports personal fees from Bioexcel, Boehringer Ingelheim, Karuna Pharma, Merck Pharma, Minerva Pharma, Roche Pharma, Sunovion Pharma, principal investigator for iFunction, royalties from WCG Verasci, payment for grant reviews from Alkermes, outside the submitted work. John M. Kane reports personal fees from Alkermes, Allergan, Boehringer Ingelheim, Indivior, Intracellular Therapies, Johnson & Johnson, Merck, Minerva, Neurocrine, HLS, HealthRhythms; personal fees from and shareholder of LB Pharmaceuticals, Vanguard Research Group, North Shore Therapeutics; grants and personal fees from Janssen Pharmaceutical, Sunovion; personal fees from and advisory board of Newron, Novartis, Otsuka, Teva, Click Therapeutics, Cerevel, Dainippon Sumitomo, H. Lundbeck; royalties from UpToDate, outside the submitted work. Dawn Velligan reports grants and/or personal fees from Alkermes, Indivior, Otsuka, Karuna, and Janssen, during the conduct of the study. Jeffrey Trotter is an employee of Worldwide Clinical Trials, a clinical research vendor paid by Alkermes, Inc. The authors report no other conflicts of interest in this work.
References
1. Kopec K, Janney CA, Johnson B, Spykerman K, Ryskamp B, Achtyes ED. Rapid Transition to Telehealth in a Community Mental Health Service Provider During the COVID-19 Pandemic. Primary Care Companion CNS Dis. 2020;22(5):20br02787. doi:10.4088/PCC.20br02787
2. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D, Schneider EC. The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases. The Commonwealth Fund; 2021.
3. Mechanic OJ, Persaud Y, Kimball AB. StatPearls: Telehealth Systems. StatPearls: Treasure Island (FL); 2021.
4. Druss BG. Addressing the COVID-19 Pandemic in Populations With Serious Mental Illness. JAMA Psychiatry. 2020;77(9):891–892. doi:10.1001/jamapsychiatry.2020.0894
5. Ji W, Huh K, Kang M, et al. Effect of Underlying Comorbidities on the Infection and Severity of COVID-19 in Korea: a Nationwide Case-Control Study. J Korean Med Sci. 2020;35(25):e237. doi:10.3346/jkms.2020.35.e237
6. Wang X, Vouk N, Heaukulani C, et al. HOPES: an Integrative Digital Phenotyping Platform for Data Collection, Monitoring, and Machine Learning. J Med Internet Res. 2021;23(3):e23984. doi:10.2196/23984
7. Karaoulanis SE, Christodoulou NG. Do patients with schizophrenia have higher infection and mortality rates due to COVID-19? A systematic review. Psychiatriki. 2021;32(3):219–223.
8. Vai B, Mazza MG, Delli Colli C, et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8(9):797–812. doi:10.1016/S2215-0366(21)00232-7
9. Nemani K, Li C, Olfson M, et al. Association of Psychiatric Disorders With Mortality Among Patients With COVID-19. JAMA Psychiatry. 2021;78(4):380–386. doi:10.1001/jamapsychiatry.2020.4442
10. Barlati S, Nibbio G, Vita A. Schizophrenia during the COVID-19 pandemic. Curr Opin Psychiatry. 2021;34(3):203–210. doi:10.1097/YCO.0000000000000702
11. González-Blanco L, Dal Santo F, García-álvarez L, et al. COVID-19 lockdown in people with severe mental disorders in Spain: do they have a specific psychological reaction compared with other mental disorders and healthy controls? Schizophr Res. 2020;223:192–198. doi:10.1016/j.schres.2020.07.018
12. Solé B, Verdolini N, Amoretti S, et al. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY. J Affect Disord. 2021;281:13–23. doi:10.1016/j.jad.2020.11.099
13. Robillard R, Daros AR, Phillips JL, et al. Emerging New Psychiatric Symptoms and the Worsening of Pre-existing Mental Disorders during the COVID-19 Pandemic: a Canadian Multisite Study. Canadian J Psychiatry. 2021;66(9):815–826. doi:10.1177/0706743720986786
14. Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. 2013;13:50. doi:10.1186/1471-244X-13-50
15. Kane JM, Kishimoto T, Correll CU. Non‐adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013;12(3):216–226. doi:10.1002/wps.20060
16. Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2–3):109–113. doi:10.1016/j.psychres.2009.05.004
17. Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatric Services. 2004;55(8):886–891. doi:10.1176/appi.ps.55.8.886
18. Backhaus A, Agha Z, Maglione ML, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv. 2012;9(2):111–131. doi:10.1037/a0027924
19. Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G. Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses. 2014;8(1):21–27A. doi:10.3371/CSRP.KAFE.021513
20. Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile Phone Ownership and Endorsement of “mHealth” Among People With Psychosis: a Meta-analysis of Cross-sectional Studies. Schizophr Bull. 2016;42(2):448–455. doi:10.1093/schbul/sbv132
21. Dobber J, Latour C. Medication adherence in patients with schizophrenia: a qualitative study of the patient process in motivational interviewing. BMC Psychiatry. 2018;18(1):135. doi:10.1186/s12888-018-1724-9
22. Schulze LN, Stentzel U, Leipert J, et al. Improving Medication Adherence With Telemedicine for Adults With Severe Mental Illness. Psychiatric Services. 2019;70(3):225–228. doi:10.1176/appi.ps.201800286
23. Basit SA, Mathews N, Kunik ME. Telemedicine interventions for medication adherence in mental illness: a systematic review. Gen Hosp Psychiatry. 2020;62:28–36. doi:10.1016/j.genhosppsych.2019.11.004
24. Greene M, Yan T, Chang E, Hartry A, Touya M, Broder MS. Medication adherence and discontinuation of long-acting injectable versus oral antipsychotics in patients with schizophrenia or bipolar disorder. J Med Econ. 2018;21(2):127–134. doi:10.1080/13696998.2017.1379412
25. Ceylan MF, Erdogan B, Tural Hesapcioglu S, Cop E. Effectiveness, Adverse Effects and Drug Compliance of Long-Acting Injectable Risperidone in Children and Adolescents. Clin Drug Investig. 2017;37(10):947–956. doi:10.1007/s40261-017-0555-7
26. Schnitzer K, MacLaurin S, Freudenreich O. Long-acting injectable antipsychotics during COVID-19. CP. 2021;20(2):8–13. doi:10.12788/cp.0087
27. Alevizopoulos G, Nystazaki M. Long Acting Injectable Antipsychotics: ongoing use during the COVID-19 pandemic and successful use of internet-based support in Greece. Eur J Psychiatry. 2021;35(3):204–205. doi:10.1016/j.ejpsy.2021.03.001
28. MacLaurin SA, Mulligan C, van Alphen MU, Freudenreich O. Optimal Long-Acting Injectable Antipsychotic Management During COVID-19. J Clin Psychiatry. 2021;82(1). doi:10.4088/JCP.20l13730
29. Ifteni P, Dima L, Teodorescu A. Long-acting injectable antipsychotics treatment during COVID-19 pandemic - A new challenge. Schizophr Res. 2020;220:265–266. doi:10.1016/j.schres.2020.04.030
30. Hicks L Final Rule Material: changes to Exempt Determination Process: biomedical Research Alliance of New York, LLC; 2017. Available from: www.citiprogram.org.
31. Gannon JM, Conlogue J, Sherwood R, et al. Long acting injectable antipsychotic medications: ensuring care continuity during the COVID-19 pandemic restrictions. Schizophr Res. 2020;222:532–533. doi:10.1016/j.schres.2020.05.001
32. Centers for Medicare & Medicaid Services. Additional Background: sweeping Regulatory Changes to Help U.S. Healthcare System Address COVID-19 Patient Surge: centers for Medicare & Medicaid Services; 2020. Available from: https://www.cms.gov/newsroom/fact-sheets/additional-backgroundsweeping-regulatory-changes-help-us-healthcare-system-address-covid-19-patient.
33. Substance Abuse and Mental Health Services Administration (SAMHSA). Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders. Rockville, MD: SAMHSA Publication No. PEP21-06-02-001; 2021.
34. Santesteban-Echarri O, Piskulic D, Nyman RK, Addington J. Telehealth interventions for schizophrenia-spectrum disorders and clinical high-risk for psychosis individuals: a scoping review. J Telemed Telecare. 2020;26(1–2):14–20. doi:10.1177/1357633X18794100
35. Civan Kahve A, Kaya H, Darben Y, Gul Cakil A, Goka E. From predictions to evidence: treatment compliance, disease progression and social compliance of patients with schizophrenia in the COVID-19 pandemic. Perspect Psychiatr Care. 2021;57(4):1991–1998. doi:10.1111/ppc.12824
36. Naslund JA, Mitchell LM, Joshi U, Nagda D, Lu C. Economic evaluation and costs of telepsychiatry programmes: a systematic review. J Telemed Telecare. 2020;28(5):311–330. doi:10.1177/1357633X20938919
37. Roach M, Lin D, Graf M, et al. Schizophrenia population health management: perspectives of and lessons learned from population health decision makers. J Managed Care Specialty Pharmacy. 2021;27(10–a Suppl):S2–S13. doi:10.18553/jmcp.2021.27.10-aa.s2
38. Saeed SA, Masters RM. Disparities in Health Care and the Digital Divide. Curr Psychiatry Rep. 2021;23(9):61. doi:10.1007/s11920-021-01274-4
39. Gude J, Subhedar RV, Zhang MH, et al. Emerging Needs and Viability of Telepsychiatry During and Post COVID-19 Era: a Literature Review. Cureus. 2021;13(8):e16974. doi:10.7759/cureus.16974
40. Seo JH, Kim SJ, Lee M. Impact of the COVID-19 pandemic on mental health service use among psychiatric outpatients in a tertiary hospital. J Affect Disord. 2021;290:279–283. doi:10.1016/j.jad.2021.04.070
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
