Back to Journals » Cancer Management and Research » Volume 12
Cetuximab Plus Chemotherapy versus Chemotherapy Alone in Recurrent or Metastatic Head and Neck Squamous Cell Carcinoma: A Cost-Effectiveness Analysis
Received 20 July 2020
Accepted for publication 14 October 2020
Published 6 November 2020 Volume 2020:12 Pages 11383—11390
DOI https://doi.org/10.2147/CMAR.S272149
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Yitian Lang,1,2 Deshi Dong1,2
1Department of Pharmacy, The First Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China; 2College of Pharmacy, Dalian Medical University, Dalian, People’s Republic of China
Correspondence: Deshi Dong
Department of Pharmacy, The First Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China
Tel +86-411-83635963
Fax +86-411-83634643
Email [email protected]
Objective: The EXTREME clinical trial revealed that cetuximab plus chemotherapy improved the overall survival time of patients with recurrent or metastatic head and neck squamous cell carcinoma (R/M HNSCC) versus chemotherapy alone. The current study examined the cost-effectiveness of cetuximab plus chemotherapy compared with chemotherapy alone in HNSCC patients from the perspective of China.
Materials and Methods: A partitioned survival model was implemented for R/M HNSCC patients. Survival information was derived from the CHANGE-2 trial. The model was designed as a ten-year time horizon, a 3-week cycle, and a 3% discount rate for costs and utilities. An incremental cost-effectiveness ratio (ICER) value is less than $30,201/quality-adjusted life-year (QALY) was considered cost-effective in China. We analyzed the uncertainty by performing one-way and probabilistic sensitivity analyses.
Results: In the base-case analysis, we found that the ICER of cetuximab plus chemotherapy compared with chemotherapy alone is $172,702/QALY. The results of one-way sensitivity analysis and probabilistic analysis showed that the fluctuations of each variable in its ranges do not cause ICERs to reach acceptable thresholds.
Conclusion: The current observations suggested that treatment with cetuximab plus chemotherapy is not a cost-effective strategy for R/M HNSCC patients in China at a $30,201 willingness to pay threshold.
Keywords: recurrent or metastatic head and neck squamous cell carcinoma, HNSCC, cetuximab, CHANGE-2, cost-effectiveness
Introduction
Worldwide, over 830,000 individuals are diagnosed with head and neck cancer, which caused annually about 430,000 deaths. Although head and neck cancer could derived from different cell progenitors and anatomic sites, over 90% were head and neck squamous cell carcinoma (HNSCC).1 In the event of advanced HNSCC, multidisciplinary interventions are taken, such as surgical, radiotherapy and chemotherapy. Hoverer, the prognosis is still poor despite the improvement of these treatment interventions.2
Cetuximab is an IgG1 monoclonal antibody that specifically targets the epidermal growth factor receptor (EGFR). Cetuximab blockade of the EGFR results in inhibition of tumor growth, invasion and metastasis, DNA damage repair and angiogenesis.3,4 The EXTREME trial showed that adding the cetuximab to cisplatin/carboplatin and 5-FU (5-fluorouracil) dramatically improved overall survival (OS: 10.1 vs 7.4 months)5 for European patients with recurrent or metastatic HNSCC (R/M HNSCC) compared with chemotherapy. On account of ethnic factors that may affect the response or tolerability of therapy, the CHANGE-2 trial (NCT02383966) evaluated the efficacy and safety of EXTREME regimen in Chinese patients with R/M HNSCC. The results also undoubtedly demonstrated that cetuximab plus chemotherapy prolonged the progression-free survival time (PFS: 5.5 vs 4.2 months) and overall survival (OS: 10.2 vs 8.9 months) compared with chemotherapy.6 At present, clinical practice guidelines, including the Guideline of the Chinese Society of Clinical Oncology (CSCO) and National Comprehensive Cancer Network (NCCN), recommend the EXTREME regimen (cetuximab + cisplatin/carboplatin + 5-FU followed by cetuximab maintenance until progressive disease) as a standard-of-care first-line therapy for patients with R/M HNSCC.7 However, due to the relatively high price of cetuximab, its wide prescription was limited. The economic evidence would be helpful for decision-makers when the health-care system covers cetuximab. The purpose of this study is to analyze the cost-effectiveness of adding the cetuximab to chemotherapy for patients with R/M HNSCC from the perspective of the Chinese health sector.
Materials and Methods
Patients Population
The target population of this study was comparable with CHANGE-2 trial, who had been confirmed histologically and/or cytologically R/M HNSCC. The baseline characteristics of CHANGE-2 trial were displayed in Table S1.
Therapeutic Regimen
Two treatment strategies were assigned: (1) chemotherapy alone, which was composed of cisplatin (75mg/m2 on day 1) plus 5-FU (750mg/m2 on days 1–5) and maintenance therapy up to 6 cycles; (2) cetuximab (400mg/m2 for the initial dose, then weekly doses of 250mg/m2) plus chemotherapy. When the disease progressed, it is assumed that the initial treatment effect was poor, and both of the two groups would end the current treatment and receive subsequent treatment. Subsequent treatment regimens were adjusted based on the recommended treatment, which was composed of methotrexate (40mg/m2 on days 1, 8, 15), docetaxel (35mg/m2 on days 1, 8, 15) or paclitaxel (80mg/m2 on days 1, 8, 15).
Model Structure
We used a partitioned survival model that programmed in R (version 3.6.0, http://www.r-project.org) to simulate survival states of R/M HNSCC patients over time and evaluate the cost-effectiveness of treatment with cetuximab plus chemotherapy in comparison with chemotherapy alone based on CHANGE-2 trial. Figure 1 shows the diagram of the model. The structure of the model included 3 mutually exclusive health stages, which is respectively progression-free (PF) stage, progressive disease (PD) stage and death. The time within each stage above was derived from PFS and OS data that were observed in CHANGE-2 trial.6,8,9 The likelihoods of distributions of PF state, PD state and death state were varied because of different PFS and OS probabilities in two competing strategies. A three-week cycle was used in order to keep with a treatment interval of CHANGE-2. The time horizon of the model was ten years to ensure that the survivors are less than 1%. Each health state was assigned a specific cost and health utility value, which were used to project the cumulative cost, quality-adjusted life-year (QALY) by running the model. A 3% annual discount rate was applied for costs and utilities. Average cost-effectiveness ratios (CER) and incremental cost-effectiveness ratios (ICER) were measured. The CER could indicate that gaining a QALY requires cost, and ICER could show that additional cost of cetuximab plus chemotherapy regimen per additional QALY compared with chemotherapy alone. If the ICER value was within the willingness-to-pay (WTP) threshold, the treatment strategy was deemed as “cost-effective”. The WTP threshold was suggested to use three times of the Chinese per capita gross domestic product (GDP) ($30,201) in 2019.10,11
 |
Figure 1 The diagram of two therapeutic regimens and three health states transitions in the partitioned survival model. |
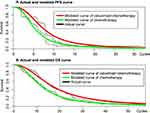
Clinical Data
The observational time of CHANGE-2 clinical trial was 40 months for OS and 28months for PFS. In order to obtain the results over a ten-year time horizon, we need to extrapolate the survival probability beyond the follow-up time. We digitized the OS and PFS Kaplan–Meier curves for cetuximab plus chemotherapy and chemotherapy alone regimen by using the R package “digitize” (version 0.0.4; https://github.com/tpoisot/digitize/). Then, using the method proposed by Guyot to generate pseudo individual patient data (IPD, based on time-to-event data),12 which were fitted by following parametric model: Weibull, exponential, log-logistic, log-normal and Gompertz parametric distributions. Based on the Akaike information criterion (AIC) value, the final parametric model that we used was log-logistic distribution, whose parameters are presented in Table 1. The validation by comparing the observational and predicted curves is shown in Figure 2.
 |
Table 1 Input Parameters of the Model |
Costs and Utility Estimates
The current analysis was conducted from the perspective of the Chinese health sector. The included costs were direct medical costs, such as medications, administration, follow-up, management of adverse events and palliative care. All costs were presented in 2019 US dollars ($). Medication costs of each treatment regimen were determined by dosages and unit price, where the body surface area (BSA) determined the dosages. For Chinese patients, the mean BSA was estimated to be 1.81m2.13 The prices of cetuximab, cisplatin, 5-FU and other chemotherapy drugs were collected from the local charge database.14 Other cost data were collected from published literature.15–18
The CHANGE-2 trial published treatment-related adverse events (AEs) incidences that occurred in the different treatment groups. AEs (grade 3 to 5) had obvious distinctions in incidence between two regimens of CHANGE-2. The costs related to AEs (grades 3 to 5) should be included in the cost-effectiveness model. The incidence of grade 3 to 5 AEs, including neutropenia, anemia, leukopenia, neutrophil count decreased and hyponatremia, should be considered in cost-effectiveness analysis. So, the cost of the AEs would be determined and calculated. The values of the incidence of the main grade 3 to 5 AEs for the different regimens are displayed in Table S2.
In this cost-effectiveness model, we use QALY to measure the main health outcome. To calculate the QALYs, we need to assign a utility value for each health stage. The utility estimates for the “progression-free” and “progressive disease” were 0.862 and 0.284, respectively.19 All costs and utilities value are shown in Table 1.
Analysis
To identify the variables that have considerable impacts on the model outcomes, we performed one-way sensitivity analyses by using the upper and lower limits of model inputs. Additionally, we conduct a probabilistic sensitivity analysis (PSA) through 1000 iterations to check whether the cetuximab plus chemotherapy regimen would be cost-effective under the willingness to pay threshold. The utilities were assumed to be sampled from Beta distribution, and costs were sampled from a gamma distribution. The standard deviation of cost and utility that have not been confirmed in the literature is set to 20% of the expected value.20 The PSA results are presented as a cost-effectiveness acceptability curve.
Result
Base-Case Analysis
The results showed that life-year (LY), QALY and cost were 1.021, 0.531 and $3349 in the chemotherapy alone. The LY, QALY and cost in cetuximab plus chemotherapy were 1.265, 0.669 and $27,182. Compared with chemotherapy alone, the cetuximab plus chemotherapy strategy increased the overall cost by $23,833 with the augments of 0.244 LYs and 0.138 QALYs. The average cost-effectiveness ratios of chemotherapy alone were $3280/LY and $6307/QALY, and cetuximab plus chemotherapy regimen was $21,488/LY and $40,631/QALY. The ICER of cetuximab plus chemotherapy compared with chemotherapy alone is $97,676/LY and $172,702/QALY. The ICER was well beyond the threshold ($30,201). The base-case analysis results are displayed in Table 2.
 |
Table 2 Results of the Base-Case Analysis |
One-Way Sensitivity Analysis
The one-way sensitivity analysis showed that the BSA, utility of progression-free and cost of cetuximab were sensitive variables ranked top three. Other variables had a medium and a paucity of impacts, such as the variables associated with adverse events. The results of the deterministic sensitivity analysis were summarized in the tornado diagrams (Figure 3). The one-way sensitivity analysis showed the results were robust because the adjustments of all variables could not push the ICERs to be lower than the threshold.
 |
Figure 3 Tornado diagram. The results of one-way sensitivity analysis in the US in the form of a tornado diagram. |
Probabilistic Sensitivity Analysis
Based on the probabilistic sensitivity analysis, the cost-effectiveness acceptable curve (Figure 4) showed the likelihood of the chemotherapy alone regimen being cost-effective was more than 99% at a WTP threshold of $30,201/QALY, and the likelihood of the cetuximab plus chemotherapy regimen was less than 1%.
 |
Figure 4 Cost-effectiveness acceptable curve. The y-axis indicates the probability that a strategy is cost-effective across the willingness to pay per QALY gained (x-axis). |
Discussion
The analysis showed that cetuximab plus chemotherapy for R/M HNSCC is not a cost-effective option than chemotherapy alone because its ICER exceeded the willingness to pay threshold in China’s context ($30,201). Although cetuximab plus chemotherapy treatment strategy has been recommended as the first-line standard treatment for R/M HNSCC, this regimen is not yet approved by the National Medical Products Administration of China. World Health Organization (WHO) has suggested that the most cost-effective treatment strategy should be taken into account in the context with limited medical resources.11 According to the above information, cetuximab plus chemotherapy strategy should not be covered by the Chinese health-care system at the current price of cetuximab. We also conducted one-way and probabilistic sensitivity analyses, whose results further also supported the above findings. Our findings were coherent with the report, which was published by Hannouf MB and colleagues.21 From the Canadian perspective, they found that the ICER of cetuximab plus chemotherapy versus chemotherapy alone is $386,000/QALY, which was far higher than Canada’s threshold.
Our one-way and probabilistic indicated that BSA is a considerable model input because cetuximab and chemotherapy regimens are administered according to BSA. The costs of the two schemes are mainly composed of unit prices and dosages. In this way, more significant differences in ICER would appear among those obese patients because they need a higher dosage of cetuximab due to the greater BSA level. An alternative payment program, such as the payment per patient, could improve the economic outcomes in these obese patients. In the report of Hannouf MB and colleagues, the cost related to cetuximab is too expensive to cover. Our analysis also suggested that the cost of cetuximab has a substantial impact on the outcome. However, the ICER value was still higher than the threshold of $30,201/QALY even when the price of cetuximab reduced by 50%, which indicated that the price of cetuximab should reduce more than 50% for meeting the Chinese threshold because Chinese health sectors face the rigorous health resource-limited setting as the biggest middle-income country.
The study reported by Hannouf MB and colleagues used the clinical data from EXTREME trial that enrolled the Western population. To compare the results by using the CHANGE-2 and EXTREME trials, we also conduct a base-case analysis by using the survival data from EXTREME trial.5 In this additional analysis, costs and utility estimates were kept unchangeable. The PFS and OS curves of EXTREME trial were re-modeled by using the described techniques in the section of the method. The final selected parametric model and analytical results are presented in Table S3. This additional analysis showed that chemotherapy alone strategy gained 0.494 QALYs with the cost of $3217, and cetuximab plus chemotherapy strategy gained 0.586 QALYs with a cost of $25,673. The ICER value is $244,087/QALY, which was poorer than the results based on the CHANGE-2 trial. The better survival outcome could explain the different results in the CHANGE-2 trial than the EXTREME trial. Because the patients in the EXTREME trial were Western population and the CHANGE-2 trial were Chinese patients, we believe this economic outcome based on the CHANGE-2 trials is more meaningful than the EXTREME trial in the Chinese context.
This study also has the following limitations: First, we cannot obtain the exact withdrawal time of the patients who interrupted the initial treatment, which may overestimate the total cost. Second, the quality of life data of HNSCC patients was not derived from the CHANGE-2 trial because the most reliable and accurate quality of life information is unavailable in the CHANGE-2 trial. Our study used the utility data reported by van der Linden,19 which would lead to deviations in the cumulative QALYs.19 Our one-way sensitivity analysis checked this shortcoming and found that utility value fluctuations do not cause ICERs to reach the acceptable threshold. Third, our study only included the costs related to managing grade 3 to 5 AEs whose incidence was >5% and ignored the disutilities of AEs. Fortunately, one-way sensitivity analysis indicated that the outcomes are not sensitive to the variables related to AEs. In addition to limitations, in order to make our study more scientific, we selected a partitioned survival model from the Markov model and partitioned model. The survival data were obtained from only PFS and OS Kaplan curves. If we selected the traditional Markov model, we could need to make some assumptions about the transition probabilities that from PF state to death and PD state to death.22
In summary, adding cetuximab to chemotherapy is not a cost-effective strategy compared with chemotherapy alone for Chinese patients with R/M HNSCC, although it provided considerable survival benefits. Reducing the cost of cetuximab could improve the economic outcome of this new regimen.
Acknowledgment
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hu M, Xie P, Lee NY, et al. Hypoxia with 18F-fluoroerythronitroimidazole integrated positron emission tomography and computed tomography (18F-FETNIM PET/CT) in locoregionally advanced head and neck cancer: hypoxia changes during chemoradiotherapy and impact on clinical outcome. Medicine. 2019;98(40):e17067. doi:10.1097/MD.0000000000017067
2. Schulz D, Stancev I, Sorrentino A, et al. Increased PD-L1 expression in radioresistant HNSCC cell lines after irradiation affects cell proliferation due to inactivation of GSK-3beta. Oncotarget. 2019;10(5):573–583. doi:10.18632/oncotarget.26542
3. Borel C, Regnier-Gavier O, Carinato H, et al. Interest to consider re-challenging by cetuximab and platinum containing regimen in recurrent head and neck cancer. Oncotarget. 2018;9(101):37581–37588. doi:10.18632/oncotarget.26506
4. Bernier J. Drug Insight: cetuximab in the treatment of recurrent and metastatic squamous cell carcinoma of the head and neck. Nat Clin Pract Oncol. 2008;5(12):705–713. doi:10.1038/ncponc1228
5. Vermorken JB, Mesia R, Rivera F, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359(11):1116–1127. doi:10.1056/NEJMoa0802656
6. Guo Y, Luo Y, Zhang Q, et al. LBA6 - First-line cetuximab plus cisplatin and fluorouracil vs cisplatin and fluorouracil in Chinese patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck: the randomized, Phase III CHANGE-2 trial. Ann Oncol. 2018;29:ix176. doi:10.1093/annonc/mdy483.005
7. National Comprehensive Cancer Network. (NCCN) clinical practice guidelines in oncology. Available from: https://www.nccn.org/professionals/physician_gls/default.aspx.
8. Guo Y. Cetuximab + chemotherapy as a first-line (1L) treatment for recurrent/metastatic squamous cell carcinoma of the head and neck (R/M SCCHN) in China: final overall survival analysis of the randomized, Phase 3 CHANGE-2 trial. CSCO. 2019;
9. Phase III trial to assess efficacy and safety of cetuximab for the treatment of Chinese participants with head and neck cancer (CHANGE-2). ClinicalTrials.gov. Available from: https://clinicaltrials.gov/ct2/show/results/NCT02383966?term=CHANGE-2&draw=2&rank=3.
10. Zhao Y, Feng HM, Qu J, Luo X, Ma WJ, Tian JH. A systematic review of pharmacoeconomic guidelines. J Med Econ. 2018;21(1):85–96. doi:10.1080/13696998.2017.1387118
11. Hutubessy R, Chisholm D, Edejer TT. Generalized cost-effectiveness analysis for national-level priority-setting in the health sector. Cost Eff Resour Alloc. 2003;1(1):8. doi:10.1186/1478-7547-1-8
12. Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9. doi:10.1186/1471-2288-12-9
13. Hu Y, Wu X, Hu Z, et al. Study of formula for calculating body surface areas of the Chinese adults. Acta Physiol Sin. 1999;51(01):
14. Chinese drug price of drug centralized bid procurement. Available from: https://db.yaozh.com/yaopinzhongbiao.
15. Wu B, Zhang Q, Sun J. Cost-effectiveness of nivolumab plus ipilimumab as first-line therapy in advanced renal-cell carcinoma. J Immunother Cancer. 2018;6(1):124. doi:10.1186/s40425-018-0440-9
16. Cao H, Wang J, Shi Y. Survey of the advanced cancer patients’ medical costs in registered hospice care agencies in five provinces and municipalities. Chin Gen Pract. 2010. doi:10.3969/j.issn.1007-9572.2010.31.023
17. Tang S, Chen W. Pharmacoeconomic study on 3 chemotherapy regimens for advanced pancreatic cancer in China based on Markov model. China Pharm. 2018;29(6). doi:10.6039/j.issn.1001-0408.2018.06.15
18. Wu B, Dong B, Xu Y, et al. Economic evaluation of first-line treatments for metastatic renal cell carcinoma: a cost-effectiveness analysis in a health resource-limited setting. PLoS One. 2012;7(3):e32530. doi:10.1371/journal.pone.0032530
19. van der Linden N, van Gils CW, Pescott CP, Buter J, Vergeer MR, Groot CA. Real-world cost-effectiveness of cetuximab in locally advanced squamous cell carcinoma of the head and neck. Eur Arch Otorhinolaryngol. 2015;272(8):2007–2016. doi:10.1007/s00405-014-3106-3
20. Acevedo JR, Fero KE, Wilson B, et al. Cost-effectiveness analysis of elective neck dissection in patients with clinically node-negative oral cavity cancer. J Clin Oncol. 2016;34(32):3886–3891. doi:10.1200/JCO.2016.68.4563
21. Hannouf MB, Sehgal C, Cao JQ, Mocanu JD, Winquist E, Zaric GS. Cost-effectiveness of adding cetuximab to platinum-based chemotherapy for first-line treatment of recurrent or metastatic head and neck cancer. PLoS One. 2012;7(6):e38557. doi:10.1371/journal.pone.0038557
22. Liu X, Tan C, Zeng X. Introduction of partitioned survival model in pharmacoeconomics evaluation and case analysis. Chin J Mod Appl Pharm. 2019;36(24). doi:10.13748/j.cnki.issn1007-7693.2019.24.018
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.