Back to Journals » Veterinary Medicine: Research and Reports » Volume 7
Canine parvoviral enteritis: an update on the clinical diagnosis, treatment, and prevention
Authors Mylonakis M, Kalli I, Rallis T
Received 12 March 2016
Accepted for publication 7 May 2016
Published 11 July 2016 Volume 2016:7 Pages 91—100
DOI https://doi.org/10.2147/VMRR.S80971
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Young Lyoo
Mathios E Mylonakis, Iris Kalli, Timoleon S Rallis
Companion Animal Clinic, School of Veterinary Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
Abstract: Canine parvovirus type 2 is the cause of a highly contagious acute enteritis associated with high morbidity and mortality, with very low survival rates in untreated dogs. Although severe clinical disease typically occurs in dogs younger than 6 months of age, adults with insufficient immunity may potentially be affected. In this article, the current state of knowledge is reviewed regarding the diagnostic aspects of parvoviral enteritis, with special emphasis placed on the clinical relevance of the detection of viral antigens in the feces, detection of viral antibodies in the serum, or the polymerase chain reaction-based amplification of the viral DNA in the feces. In addition, the components of the supportive and symptomatic treatment aiming to optimize the outcome of the disease in the clinical setting are thoroughly reviewed. Immunization guidelines for the prevention of the disease are also updated.
Keywords: dog, parvovirus type 2, acute enteritis, treatment, vaccination
Introduction
Canine parvovirus enteritis (PVE), caused by three variants of canine parvovirus type 2 (CPV-2; family Parvoviridae, Genus Parvovirus), is a leading cause of morbidity and mortality in dogs globally.1,2 CPV-2 emerged as a cause of acute canine enteritis in mid-to-late 1970s, possibly from another carnivore parvovirus (cats or other hosts), spreading rapidly and triggering outbreaks worldwide.3–8 In early-to-mid 1980s, CPV-2 evolved into two variants (CPV-2a and CPV-2b),9,10 while in 2000, a third variant (CPV-2c) was documented in Italy and has since been found in all continents except Australia.11–16 All three variants are thought to have similar pathogenicity leading to indistinguishable clinical disease.8,17 Importantly, CPV-2a, CPV-2b, and CPV-2c strains have a broader host range compared to the original CPV-2 strain and may cause naturally occurring disease identical to feline panleukopenia in cats.3
Although severe clinical disease typically occurs in dogs younger than 6 months of age, adults with insufficient immunity may potentially be affected.17,18 Breed predisposition and seasonal prevalence of the disease are subject to considerable geographic variation.18,19 CPV-2 is ubiquitous and can survive in the environment for more than a year, enabling exposure of susceptible dogs to infected feces, vomitus, or fomites.2 The incubation period following natural or experimental exposure ranges from 4 to 14 days, and virus shedding starts a few days prior to the occurrence of clinical signs, progressively declining 3–4 weeks postexposure.20–23
The principal pathogenetic fact in CPV-2 infection is the virus-induced destruction of rapidly dividing cells, including crypt intestinal epithelial cells, thymus, lymph nodes, and bone marrow precursor cells.21–23 As a result, intestinal mucosal barrier disruption, villous atrophy, and malabsorption occur, along with profound leukopenia (mainly neutropenia and/or lymphopenia), leading to profuse diarrhea and vomiting, severe dehydration/hypovolemia, metabolic acidosis (or alkalosis), bacterial translocation with subsequent coliform septicemia and endotoxemia, systemic inflammatory response syndrome (SIRS), hypercoagulability, multiorgan dysfunction, and death.1,2,18,24–29 Comorbid conditions (eg, parasitic, viral, or bacterial intestinal pathogens) or stressors (eg, weaning, overcrowded and unsanitary conditions) may precipitate or exacerbate the disease.1,17,19,22 Because of the widespread vaccinations and/or the natural exposure of the adult animals, clinically relevant CPV-2-induced myocarditis is now an extremely rare manifestation in the clinical setting, unless infection occurs in utero or in puppies born to unvaccinated bitches.1,2,30
Clinical diagnosis of canine PVE
Canine PVE has clinical similarities with other causes of acute gastrointestinal disturbances, including, though not limited to, canine distemper infection and other viral enteritides, hemorrhagic gastroenteritis, enteric bacterial infections such as salmonellosis, acute pancreatitis, hypoadrenocorticism, inflammatory bowel disease, intestinal intussusception, gastrointestinal foreign bodies, and various intoxications.2 Therefore, clinical diagnosis of PVE necessitates the combination of compatible clinical and clinicopathologic abnormalities along with the detection of the viral antigen or the polymerase chain reaction (PCR)-based amplification of the viral DNA in the feces.
Clinical signs
The clinical manifestations of CPV-2 infection are nonspecific or referable to enteritis (Table 1), commonly including anorexia or lethargy, weakness, depression, foul-smelling diarrhea, which may range from mucoid to purely hemorrhagic, vomiting, dehydration, and fever.18,19,23,31–33 Due to intestinal dysmotility, intussusception may occur, an uncommon but potentially fatal complication of PVE.29,34 Several dogs demonstrate evidence of SIRS on admission, which may herald a poor prognosis.18 Rarely, dogs may be presented with congestive heart failure, neurological signs, or erythema multiforme.2,35–38 Subclinical infections are thought to occur commonly in adult unvaccinated dogs; however, severe fatal disease may also occur.18,32 Vomiting and depression or lethargy on admission were found to prolong the duration of hospitalization in one study.18
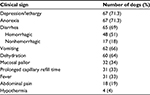  | Table 1 Physical examination findings on admission in 94 puppies with spontaneous parvoviral enteritis Note: Adapted from Res Vet Sci. 89(2), Kalli I, Leontides LS, Mylonakis ME, Adamama-Moraitou K, RallisT, Koutinas AF. Factors affecting the occurrence, duration of hospitalizationand final outcome in canine parvovirus infection. Pages 174–178. Copyright 2010, with permission from Elsevier.18 |
Clinicopathologic abnormalities
Leukopenia due to neutropenia and/or lymphopenia is the prominent hematological abnormality in canine PVE due to the destruction of bone marrow precursors, the depletion of lymphoid tissues, and the increased demands of the massively inflamed intestinal tract (Table 2). Anemia, thrombocytopenia or thrombocytosis, pancytopenia, neutrophilic leukocytosis, and monocytosis may also occur.2,18,39,40 The prognostic significance of total or differential leukocyte counts on admission or over time in PVE has been assessed previously. Lack of significant leukopenia (≥4,500/μL) or lymphopenia (≥1,000/μL) at 24 hours postadmission had a 100% positive predictive value for survival.40 Glickman et al41 did not find any association between leukopenia upon admission and outcome, as opposed to leukopenia and/or lymphopenia32 and neutropenia,23,42 that decreased the chances for survival. Lymphopenia (<1,000/μL) on admission was found to be significantly associated with prolonged hospitalization time in another study.18
Although nonspecific (Table 2), serum biochemistry abnormalities consistently include hypoproteinemia, hypoalbuminemia, hypoglycemia (or mild-to-moderate hyperglycemia) reflecting an interplay among severe malnutrition, septicemia, and/or the stress-induced activation of catecholamines, hypocalcemia, and electrolyte abnormalities such as hypokalemia, hyponatremia, hypochloremia, and hypomagnesemia.18,33,43–45 Prerenal azotemia may also occur, while less frequently, liver damage induced by hypoperfusion and/or SIRS may be denoted by increased liver enzyme activities or hyperbilirubinemia. In a study recently completed in our hospital, it was shown that ∼50% of dogs with PVE demonstrated mild acute pancreatitis (indicated by increased serum canine pancreatic lipase immunoreactivity concentration), which did not adversely affect the duration of hospitalization or the final outcome (Kalli et al, unpublished data, 2009). Hypoalbuminemia on admission was found to be significantly associated with prolonged hospitalization time previously.18 Furthermore, another study has suggested that hypocholesterolemia may indicate increased disease severity and a guarded-to-poor prognosis in affected dogs.28
  | Table 2 Hematological and serum biochemical abnormalities in 76 dogs with spontaneous parvoviral enteritis Note: Adapted from Res Vet Sci. 89(2), Kalli I, Leontides LS, Mylonakis ME, Adamama-Moraitou K, Rallis T, Koutinas AF. Factors affecting the occurrence, duration of hospitalization and final outcome in canine parvovirus infection. Pages 174–178. Copyright 2010, with permission from Elsevier.18 Abbrevation: ALT, alanine aminotransferase. |
The performance of noninvasive markers such as acute phase proteins in determining disease severity and prognosis of PVE has recently been addressed. Although C-reactive protein (CRP), haptoglobin, and ceruloplasmin were found to substantially increase and albumin concentration to decrease on admission in dogs with PVE, only CRP was associated with disease severity and outcome (survival or death).46,47
In another study, it was shown that higher serum CRP concentrations at 12 and 24 hours after admission were associated with shorter survival time and longer duration of hospitalization; however, the discriminative ability of CRP concentration alone in predicting outcome was only moderately accurate.48 High serum cortisol and low serum thyroxine concentrations 24 and 48 hours postadmission may also herald a poor prognosis in dogs with PVE.49
Diagnostic imaging
Abdominal radiography or ultrasonography detects largely nonspecific changes, including fluid- and gas-filled intestinal loops, hypomotile intestines, and possibly thinning of mucosal layers.50 However, radiography is valuable in assessing the presence of intestinal foreign bodies, while ultrasonography is an invaluable tool for the early recognition of an intussusception or the presence of peritoneal effusion.2
Serology in PVE
Antibodies to CPV-2 in the blood serum can be quantified in a laboratory setting using hemagglutination inhibition or semiquantitatively measured with an in-clinic enzyme linked immunosorbent assay (ELISA). However, since a significant proportion of dogs can be seropositive due to previous, often subclinical infection, maternally- or vaccination-derived antibodies, positive serology is not by itself diagnostic of active CPV-2 infection.2 In contrast, the quantitative assays may be useful in titrating the maternally derived antibodies, possibly allowing for the calculation of the time that vaccination can be performed without the interference of maternal immunity.38 In addition, the serological assays, especially the simple in-practice tests, are thought to be useful in assessing the presence of protective immunity against CPV following the completion of the initial puppy vaccination series, for determining the duration of immunity afforded by CPV vaccines and for improving management of shelter CPV infection outbreaks.51–53 As a rule, lack of seropositivity to CPV 4 weeks after the completion of the initial puppy series at 16 weeks of age indicates the absence of protective immunity justifying revaccination (likely with another vaccine product). Failure again to achieve seropositivity 4 weeks after the new vaccination is a strong evidence that the puppy may be a nonresponder incapable of mounting protective immunity.53 Similarly, veterinarians might wish to be able to offer their clients an alternative strategy to routine core vaccination at 3-yearly intervals. In the latter setting, a seronegative or a seropositive result justifies vaccination or extension of the booster core vaccination interval to >3 years, respectively.53
Detection of the viral antigen or DNA in the feces
The most cost-effective assays for the virus detection are the rapid point-of-care tests, including ELISA, immunomigration assay, and immunochromatography assay applied in fecal or rectal swab material.54 Although their specificity typically exceeds 90%,54,55 data on their sensitivity vary substantially. Depending on the method utilized as gold standard (eg, PCR or immune-electron microscopy), it has been estimated to range from 16% to 80%.17,38,54–58 False negatives may be due to decreased or intermittent viral shedding in earlier or later stages of the infection, the binding of serum-neutralizing antibodies with antigen in the intestinal lumen, or the dilutional effect of the diarrhea.29,58 Anecdotal reports indicate that CPV-2c-induced disease may occur in the context of negative ELISA results.29 However, recent studies have shown that the sensitivity of the ELISA tests is not affected by the virus variant.17,56,57 False-positive results may be associated very rarely with recent vaccination with modified live vaccines, although in a recent study, neither a CPV-2 nor a CPV-2b vaccine strain was detected at any time in the feces of vaccinated dogs.29,59 In the light of this evidence, in a dog with compatible clinical and clinicopathologic abnormalities, a negative fecal antigen test does not rule out PVE, while a positive fecal antigen test should be interpreted as reflecting a natural infection, until proven otherwise.
Several veterinary diagnostic laboratories offer a range of PCR assays (eg, real-time or conventional nested PCR) for the detection of CPV-2 variants.60 The major clinical indication for PCR is the suspicion of PVE, in the context of negative fecal antigen testing. Unfortunately, as demonstrated by Schmitz et al,54 positive PCR results for CPV may be seen in dogs without signs of gastroenteritis or even in dogs with chronic diarrhea, a finding of uncertain clinical significance. In addition, attenuated live vaccine virus can uncommonly be detected in the feces or in the blood with PCR assays for an undefined period after vaccination,59,61,62 although assays using minor groove binder probes have been developed that can differentiate between vaccine and wild-type virus, even in the same animal.38,61–64 In the future, quantification of virus loads in feces or in the blood using real-time PCR may be helpful in differentiating between the recently vaccinated and the naturally infected dogs.29
Treatment of canine PVE
Survival rate may be as low as 9% if no treatment is undertaken but may exceed 80% in tertiary care facilities.25,41,65 In the majority of cases, inpatient treatment is warranted; surprisingly, in a recent study, the proportion of dogs that recovered after treatment in the hospital (78.3%) did not differ from that of dogs recovered after at-home treatment (63.2%).17 Although these findings may be biased in that dogs with less severe disease are more likely to receive treatment at home, they still may indicate that mildly affected puppies may be treated on an outpatient basis.1
Treatment for PVE is largely supportive and symptomatic. The principal components of treatment include 1) fluid therapy, 2) antibiotic treatment, 3) antiemetic treatment, and 4) nutritional support. An array of other treatment measures including, though not limited to, antiviral treatments and pain management have been assessed in the past or are currently under investigation regarding their potential utility in PVE.
Fluid therapy
Maintenance of hydration and oncotic support as well as correction of acid–base and electrolyte disturbances are of utmost importance in PVE. Since subcutaneous fluid absorption is impaired in dehydrated animals, venous access is the cornerstone of fluid treatment. In case of a peripheral vein catheterization, catheter should be replaced in 72 hours to minimize the chances of bacterial colonization.66 Provided that the dog can tolerate the procedure, aseptic jugular vein catheterization by a multilumen catheter may be a better venous access option compared to a peripheral vein access in PVE because 1) optimization of fluid therapy can be assisted by central venous pressure measurement, 2) multiple drug and fluid types can be administered, 3) serial blood sampling is facilitated, 4) the catheter may remain in place for the entire period of hospitalization, and 5) contamination of the catheter site from vomiting or diarrhea can be easier to avoid compared to a peripheral vein catheter.67 Based on the evidence that PVE may be associated with a hypercoagulable state, jugular catheterization may raise the possibility of thrombosis.68 We have never seen clinically relevant thrombosis associated with jugular catheterization in PVE. If placement of an intravenous catheter is difficult, an intraosseous catheter is a very satisfactory alternative, until access to a vein is established.29,69
Puppies admitted with severe hypovolemia need reestablishment of their circulating volume in 1–2 hours. As a rule, a balanced isotonic crystalloid solution (eg, Lactated Ringers) is the fluid of choice for initial restoration of intravascular volume and rehydration, with a rate titrated to improve perfusion parameters, including capillary refill time, mucosal color, pulse character, and mean arterial pressure or lactate concentrations.70 Typically, the canine shock dose (80–90 mL/kg) is split in consecutive boluses of 15–20 mL/kg given over 15 minutes until improvement of the perfusion status is achieved.70 In general, if the administration of 50% of the calculated shock volume of isotonic crystalloids has failed to achieve sufficient improvement, adding a colloid should be considered.71 In dogs admitted without evidence of hypovolemic shock, hydration may be restored over 12–24 hours. The daily fluid allowances should incorporate the maintenance requirements (40–60 mL/kg), the current fluid deficits (body weight [kg] × % dehydration = volume [L] to correct), and the ongoing losses (might be subjectively estimated to 250 mL).70,71
Parvoviral enteritis may be associated with huge protein losses.31 Therefore, colloidal support should be provided when peripheral edema (subcutaneous, conjunctival, pleural, or abdominal effusions), hypoalbuminemia (<2 g/dL), or hypoproteinemia (<4 g/dL) occurs.27,71 Synthetic colloids (eg, 6% hetastarch) appear to be more cost-effective options in the clinical setting, as they provide better oncotic support (allowing for a 40%–60% reduction of the daily crystalloids volume) and are more affordable compared to natural colloids.27 Although synthetic colloids may reportedly adversely affect von Willebrand’s factor, factor VIII, platelet function, and fibrin polymerization, clinically relevant bleeding tendency has not been documented in animals receiving daily maintenance rate not exceeding 20 mL/kg.72 Fresh plasma has been suggested in the past because of its purported additional benefits, including coagulation factors and antiviral antibodies.33 However, plasma has limited availability, may be prohibitively expensive, and has relatively low oncotic pressure, and large volumes (22.5 mL/kg) are required to achieve a mild increase (0.5 g/dL) in the serum albumin concentrations.27,73 Human or canine albumin solutions may be used as alternatives to fresh plasma for oncotic support; however, their efficacy in PVE has yet to be evaluated. Whole blood (20 mL/kg, within 4 hours) or packed red blood cells is the preferred choice if severe anemia develops in the course of PVE.
Hypokalemia is a frequent issue in PVE,18 which may result in weakness, ileus, and cardiac compromise. Typically, maintenance fluids are supplemented with ≥20 mEq/L of potassium chloride for sustaining normokalemia or restoring hypokalemia. The rate of potassium administration should not exceed 0.5 mEq/kg/h, and daily measurement of serum level is warranted for better monitoring.74 Hypoglycemia may be a severe complication of PVE, especially in toy breeds.18 Therefore, glucose measurement should be performed at least once or twice daily, and supplementation of the maintenance fluids with 2.5%–5% dextrose may be warranted if a declining serum glucose concentration is documented.
Antibiotic treatment
Parenteral administration of wide-spectrum bactericidal antibiotics is warranted in dogs with severe PVE due to the high risk of septicemia associated with the disruption of the mucosal barrier and the concurrent profound neutropenia.24,25,27,75 Ampicillin and cefoxitin as single-agent treatments or in combination with enrofloxacin (Table 3) are rational empirical choices offering protection against Gram-positive, Gram-negative, and anaerobic organisms.27,76 Enrofloxacin may cause cartilage damage in young growing dogs; however, this is a rare occurrence if standard doses are used and the duration of treatment does not exceed 5 days.76 Aminoglycosides may also be considered in well-hydrated animals.
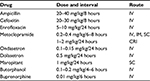  | Table 3 Doses of most commonly used drugs in canine parvoviral enteritis Abbrevations: IV, intravenously; IM, intramuscularly; SC, subcutaneously; CRI, constant-rate infusion. |
Antiemetic treatment
Metoclopramide, a dopaminergic antagonist that blocks the chemoreceptor trigger zone and exerts a prokinetic effect in the upper intestinal tract, may be given as a bolus or as a constant-rate infusion in dogs with severe vomiting (Table 3). The serotonin receptor antagonists ondasetron or dolasetron may be used successfully in cases of intractable vomiting.27 The recent advent of maropitant, an antagonist of neurokinin1 receptors, has improved substantially the efficacy of antiemetic treatment in dogs. Although the efficacy of maropitant in canine PVE has yet to be thoroughly evaluated, in a recent study, it was shown that maropitant was effective in preventing vomiting caused by stimulation of either central or peripheral emetic pathways, whereas metoclopramide or ondansetron prevented vomiting caused by either central or peripheral stimulation, respectively, but not both.77 In another study, a single daily dose of maropitant was more effective than metoclopramide administered two or three times daily in the treatment of emesis caused by various etiologies in dogs.78 In the latter study, only four of 183 (2%) examined dogs had evidence of acute viral enteritis/parvoenteritis, thus impairing the establishment of valid conclusions regarding the efficacy of the drug in dogs with PVE. In another study, maropitant was evaluated for safety and efficacy in the treatment and prevention of acute vomiting due to various etiologies in 275 dogs (26% of which had been diagnosed with PVE) in a randomized clinical trial. Although in that study mitigation of emesis was not assessed separately for the subgroup of dogs with PVE, overall, emesis was significantly reduced in maropitant-treated dogs compared to placebo-treated ones.79 Based on our experience, the administration of maropitant once daily, singly or in combination with metoclopramide, is very effective in reducing or abolishing emesis in PVE. Overall, the drug appears to be safe; dogs treated with maropitant may exhibit transient pain on injection site, which may be substantially reduced if the drug solution is kept refrigerated instead of stored at room temperature prior to being injected.78–80 Although antiemetic treatment is definitely warranted in PVE, many affected dogs have protracted vomiting despite antiemetic administration, and in a previous study, prolonged duration of hospitalization was found in dogs that received antiemetic treatment compared to those that did not.81
Nutritional support
The nil per os feeding strategy in PVE has recently been challenged. Enteral feeding is associated with improved mucosal integrity, faster repair, and as a result, reduced possibilities for bacterial translocation.27,29 This was accentuated in a relatively recent study, in which early enteral nutrition via nasoesophageal catheter starting 12 hours postadmission was associated with earlier clinical improvement, significant weight gain, and possibly improved gut barrier function compared to dogs subject to the traditional food withholding until cessation of vomiting for 12 hours.82 Parenteral nutrition is rarely needed in PVE because of the acute course of the disease.
Antiviral treatments
Use of convalescent serum from dogs that have recovered from CPV infection as a means of providing passive immunization has been reported anecdotally.27 In a recent study, the administration of a single 12 mL dose of CPV-immune plasma as adjunctive treatment for canine PVE after the appearance of clinical signs did not improve any assessed parameter, including time to hematologic recovery, viral load, severity of clinical findings, and duration of hospitalization.83 However, a beneficial effect may still be possible to achieve if a larger volume of plasma is given prior to the occurrence of the clinical signs.53
Recombinant feline interferon-ω (rFeIFN-ω) has been promising in previous studies. In a study of 94 dogs with naturally occurring PVE, severity of clinical signs and mortality reduced significantly in those treated with rFeIFN-ω (2.5 mU/kg, intravenously, daily for 3 days) as opposed to placebo-treated dogs.84 In another experimental study, rFeIFN-ω (2.5 mU/kg, intravenously, daily for 3 days) was also similarly effective.85 Currently, the limited commercial availability and the particularly high cost prevent rFeIFN-ω from being regularly included in the clinical setting.
Oseltamivir, a neuraminidase inhibitor, has attracted attention for the treatment of PVE. In a previous study, the use of oseltamivir (2 mg/kg, per os, for 5 days) improved body weight and hematological parameters in dogs with PVE compared to placebo-treated dogs; however, no tangible benefit was documented in terms of survival or duration of hospitalization.86 In addition, in a recent study in our hospital, oseltamivir at the same dose scheme was ineffective in decreasing morbidity and mortality in dogs with PVE.87 The lack of any clinically relevant benefit, along with the concern that widespread use of the drug in dogs may favor the development of oseltamivir resistance in humans with influenza infections, does not justify the routine inclusion of this drug in the treatment of PVE.
Pain management
Abdominal pain occurs frequently in PVE as a result of severe enteritis, and less commonly due to concurrent intussusception, and may adversely affect appetite.18 Therefore, analgesic treatment may be warranted. In this respect, butorphanol or buprenorphine (Table 3) may be useful. Interestingly, maropitant is a blocker of substance P, a mediator of visceral pain; ongoing research is focusing on the potential usefulness of maropitant to reduce visceral pain, which might be of value in PVE.88
Miscellaneous treatments
The efficacy of recombinant human granulocyte colony-stimulating factor (G-CSF) has been evaluated in PVE. No beneficial effect could be documented in terms of the time to hematological recovery, the duration of hospitalization, or the survival rate.89,90 In a recent study, the efficacy of recombinant canine G-CSF (rcG-CSF) was assessed in a clinical trial. Hematological recovery was hastened, and duration of hospitalization was reduced in rcG-CSF-treated dogs compared to nontreated ones; however, no survival benefit was demonstrated, and in fact, the rcG-CSF-treated dogs had shorter survival time.30 On the other hand, it has been documented that in neutropenic dogs with experimental PVE, endogenous G-CSF increases promoting neutrophil count recovery.91 Therefore, the benefit of exogenous G-CSF in PVE, if any, has yet to be substantiated.
Equine endotoxin antiserum has been utilized in the past with inconclusive results,45,92 while the use of recombinant bactericidal/permeability-increasing protein (rBPI21) failed to decrease endotoxin concentration and duration of hospitalization or to increase survival.65
In PVE, administration of anthelminthic treatment may also be of value in removing a comorbid condition that may exacerbate the clinical severity of the disease. An array of other empiric medications, including gastrointestinal protectants and H2 blockers, may be given for PVE at the discretion of the clinician; however, evidence-based justification for their use is currently lacking.1
Prevention of canine PVE
Effective immunization is essential for the protection of the individual pet and the decrease of the population of susceptible animals in a region, thus promoting the “herd immunity”.53 Modified live vaccines (MLVs) are currently used worldwide affording prolonged (7 years or longer) immunity that would confer protection against both disease and infection.93–96 The initial puppy vaccination series starts normally at 6–8 weeks of age, and then every 2–4 weeks until 16 weeks of age or older.53 If the dog is admitted for the initial vaccinations after the age of 16 weeks, two doses 2–4 weeks apart are generally recommended, but even one dose of MLV is very likely protective.96 According to the recently revised guidelines for the vaccinations of dogs and cats endorsed by the World Small Animal Veterinary Association, the first booster vaccine after the end of the initial series is now recommended to be delivered at any time between 6 and 12 months of age; however, 6 months of age is a convenient timing for the puppies that have completed their initial series at the age of 4 months. Thereafter, vaccinations for CPV (similar to other canine core vaccines) are given no more often than every 3 years.53
In the shelter environment, a more stringent vaccination schedule may be implemented. Vaccinations for CPV (along with other core vaccines) may start immediately on admission, as early as 4 weeks of age and be repeated at 2- to 3-week intervals until 20 weeks of age if the animal is still in the facility. For dogs older than 16–20 weeks on admission, one dose prior to or immediately on admission and a repeat in 2 weeks is proposed.53
Challenge studies have shown that currently available CPV vaccines containing CPV-2 or CPV-2b variants confer protection against all natural variants including CPV-2c.97–100 However, there is an increasing number of reports documenting severe outbreaks of PVE in young and adult dogs, despite being properly vaccinated.101–104
Health care beyond vaccination is also an integral part of every prevention strategy. Good hygienic practices in the kennels including disinfection of all exposed surfaces and personnel are important, given the extremely hardy nature of the virus in the environment. Sodium hypochloride (common household bleach) is an effective viricidal (one in 30 dilution), provided that contact time is at least 10 minutes.38 Importantly, socialization classes attended by vaccinated puppies aged <16 weeks were not found to be associated with a greater risk of CPV infection than vaccinated puppies that did not attend those classes.105
Conclusion
Canine parvoviral enteritis is a leading cause of morbidity and mortality in dogs younger than 6 months of age, despite the availability of safe and highly efficacious MLVs. Although the diagnosis of the disease is usually straightforward (compatible clinical and hematological abnormalities in a suboptimally vaccinated puppy, with or without a positive fecal viral antigen test), treatment and prevention strategies are ever evolving in an attempt to decrease the incidence of this life-threatening disease. Future studies should try to optimize the clinical management of the affected dogs by 1) improving the monitoring tools during hospitalization (eg, establishment of more robust noninvasive markers of the disease severity and prognosis), 2) establishing the best fluid therapy strategy (eg, to substantiate the beneficial role of and refine the most effective colloid solutions), and 3) suggesting more cost-effective antiemetic and antiviral treatments. On the other hand, further research may be warranted in elucidating to which extend the apparent vaccination failures in the clinical setting are vaccine-associated (eg, vaccines with reduced immunogenicity against the new field variants) or vaccination policy-associated (eg, level of herd immunity in an area, schedule of primary vaccination series, booster timing).
Disclosure
The authors report no conflicts of interest in this study.
References
Goddard A, Leisewitz AL. Canine parvovirus. Vet Clin North Am Small Anim Pract. 2010;40(6):1041–1053. | ||
Sykes JE. Canine parvovirus infections and other viral enteritides. In: Sykes JE, editor. Canine and Feline Infectious Diseases. 1st ed. St Louis, MO: Elsevier; 2014:141–151. | ||
Greene CE. Feline enteric viral infections. In: Greene CE, editor. Infectious Diseases of the Dog and Cat. 4th ed. St Louis, MO: Elsevier Saunders; 2012:80–91. | ||
Battilani M, Bassani M, Forti D, Moranti L. Analysis of the evolution of feline parvovirus (FPV). Vet Res Commun. 2006;30(3):223–226. | ||
Truyen U. Evolution of canine parvovirus-a need for new vaccines? Vet Microbiol. 2006;117(1):9–13. | ||
Decaro N, Desario C, Miccolupo A, et al. Genetic analysis of feline panleukopenia viruses from cats with gastroenteritis. J Gen Virol. 2008;89(9):2290–2298. | ||
Hoelzer K, Parrish CR. The emergence of parvoviruses of carnivores. Vet Res. 2010;41(6):39. | ||
Decaro N, Buonavoglia C. Canine parvovirus-a review of epidemiological and diagnostic aspects, with emphasis on type 2c. Vet Microbiol. 2012;155(1):1–12. | ||
Carmichael LE. An annotated historical account of canine parvovirus. J Vet Med Ser B. 2005;52(7–8):303–311. | ||
Martella V, Decaro N, Buonavoglia C. Evolution of CPV-2 and implication for antigenic/genetic characterization. Virus Genes. 2006;33(1):11–13. | ||
Buonavoglia C, Martella V, Pratelli A, et al. Evidence for evolution of canine parvovirus type 2 in Italy. J Gen Virol. 2001;82(12):3021–3025. | ||
Decaro N, Martella V, Desario C, et al. First detection of canine parvovirus type 2c in pups with haemorrhagic enteritis in Spain. J Vet Med B. 2006;53(10):468–472. | ||
Hong C, Decaro N, Desario C, et al. Occurrence of canine parvovirus type 2c in the United States. J Vet Diagn Invest. 2007;19(5):535–539. | ||
Pérez R, Francia L, Romero V, Maya L, Lopez I, Martin H. First detection of canine parvovirus type 2c in South America. Vet Microbiol. 2007;124(1–2):147–152. | ||
Kapil S, Cooper E, Lamm C, et al. Canine parvovirus types 2c and 2b circulating in North American dogs in 2006 and 2007. J Clin Microbiol. 2007;45(12):4044–4047. | ||
Ntafis V, Xylouri E, Kalli I, et al. Characterization of canine parvovirus type 2 (CPV-2) variants circulating in Greece. J Vet Diagn Invest. 2010;22(5):737–740. | ||
Marcovich JE, Stucker KM, Carr AH, Harbison CE, Scarlett JM, Parrish CR. Effects of canine parvovirus strain variations on diagnostic test results and clinical management of enteritis in dogs. J Am Vet Med Assoc. 2012;241(1):66–72. | ||
Kalli I, Leontides LS, Mylonakis ME, Adamama-Moraitou K, Rallis T, Koutinas AF. Factors affecting the occurrence, duration of hospitalization and final outcome in canine parvovirus infection. Res Vet Sci. 2010;89(2):174–178. | ||
Houston DM, Ribble CS, Head LL. Risk factors associated with parvovirus enteritis in dogs: 283 cases (1982-1991). J Am Vet Med Assoc. 1996;208(4):542–546. | ||
Decaro N, Desario C, Campolo M, et al. Clinical and virological findings in pups naturally infected by canine parvovirus type 2 Glu-426 mutant. J Vet Diagn Invest. 2005;17(2):133–138. | ||
Decaro N, Campolo M, Desario C, et al. Maternally-derived antibodies in pups and protection from canine parvovirus infection. Biologicals. 2005;33(4):261–267. | ||
Smith-Carr S, Macintire DK, Swango LJ. Canine parvovirus. Part I. Pathogenesis and vaccination. Compend Contin Educ Pract Vet. 1997;19(2):125–133. | ||
McCaw DL, Hoskins JD. Canine viral enteritis. In: Green CE, editor. Infectious Diseases of the Dog and Cat. 4th ed. St Louis, MO: Saunders; 2006:63–73. | ||
Turk J, Miller M, Brown T, et al. Coliform septicemia and pulmonary disease associated with canine parvoviral enteritis: 88 cases (1987–1988). J Am Vet Med Assoc. 1990;196(5):771–773. | ||
Otto CM, Drobatz KJ, Soter C. Endotoxemia and tumor necrosis factor activity in dogs with naturally occurring parvoviral enteritis. J Vet Intern Med. 1997;11(2):65–70. | ||
Macintire DK. Bacterial translocation: clinical implications and prevention. In: Bonagure JD, editor. Kirk’s Current Veterinary Therapy XIII Small Animal Practice. 13th ed. Philadelphia, PA: Saunders; 2000:201–203. | ||
Prittie J. Canine parvoviral enteritis: a review of diagnosis, management, and prevention. J Vet Emerg Crit Care. 2004;14(3):167–176. | ||
Yilmaz Z, Senturk S. Characterization of lipid profiles in dogs with parvoviral enteritis. J Small Anim Pract. 2007;48(11):643–650. | ||
Veir JK. Canine parvoviral enteritis. In: Bonagura JD, Twedt DC, editors. Kirk’s Current Veterinary Therapy XV. 15th ed. St Louis, MO: Elsevier; 2014:533–536. | ||
Duffy A, Dow S, Ogilvie G, Rao S, Hackett T. Hematologic improvement in dogs with parvovirus infection treated with recombinant canine granulocyte-colony stimulating factor. J Vet Pharmacol Ther. 2010;33(4):352–356. | ||
Macartney L, McCandlish IAP, Thompson H, Cornwell HJC. Canine parvovirus enteritis 1: clinical, haematological and pathological features of experimental infection. Vet Rec. 1984;115(9):201–210. | ||
Mason MJ, Gillett NA, Muggenburg BA. Clinical, pathological, and epidemiological aspects of canine parvoviral enteritis in an unvaccinated closed Beagle colony: 1978-1985. J Am Anim Hosp Assoc. 1987;23(2):183–192. | ||
Macintire DK, Smith-Carr S. Canine parvovirus. Part II. Clinical signs, diagnosis, and treatment. Compend Contin Educ Pract Vet. 1997;19(3):291–302. | ||
Rallis TS, Papazoglou LG, Adamama-Moraitou KK, Prassinos NN. Acute enteritis or gastroenteritis in young dogs as a predisposing factor for intestinal intussusception: a retrospective study. J Vet Med A Physiol Pathol Clin Med. 2000;47(8):507–511. | ||
Agungpriyono DR, Uchida K, Tabaru H, Yamaguchi R, Tateyama S. Subscute massive necrotizing myocarditis by canine parvovirus type-2 infection with diffuse leukoencephalomalacia in a puppy. Vet Pathol. 1999;36(1):77–80. | ||
Schaudien D, Polizopoulou Z, Koutinas A, et al. Leukoencephalopathy associated with parvovirus infection in Cretan hound puppies. J Clin Microbiol. 2010;48(9):3169–3175. | ||
Woldemeskel M, Liggett A, Ilha M, Saliki JT, Johnson LP. Canine parvovirus-2b-associated erythema multiforme in a litter of English Setter dogs. J Vet Diagn Invest. 2011;23(3):576–580. | ||
Greene CE, Decaro N. Canine viral enteritis. In: Greene CE, editor. Infectious Diseases of the Dog and Cat. 4th ed. St Louis, MO: Elsevier Saunders; 2012:67–80. | ||
Boosinger TR, Rebar AH, DeNicola DB, Boon GD. Bone marrow alterations associated with canine parvoviral enteritis. Vet Pathol. 1982;19(5):558–561. | ||
Goddard A, Leisewitz AL, Christopher MM, Duncan NM, Becker PL. Prognostic usefulness of blood leukocyte changes in canine parvoviral enteritis. J Vet Intern Med. 2008;22(2):309–316. | ||
Glickman LT, Domanski LM, Patronek GJ, Visintainer F. Breed-related risk factors for canine parvovirus enteritis. J Am Vet Med Assoc. 1985;187(6):589–594. | ||
Brunner CJ, Swango LJ. Canine parvovirus infection: effects on the immune system and factors that predispose to severe disease. Compend Contin Educ Pract Vet. 1985;85:979–988. | ||
Li R, Humm KR. Canine parvovirus infection. In: Silverstein DC, Hoper K, editors. Small Animal Critical Care Medicine. 2nd ed. St Louis, MO: Elsevier; 2015:509–513. | ||
Heald RD, Jones BD, Schmidt DA. Blood gas and electrolyte concentrations in canine parvoviral enteritis. J Am Anim Hosp Assoc. 1986;22(9):745–748. | ||
Mann FA, Boon GD, Wagner-Mann CC, Ruben DS, Harrington DP. Ionized and total magnesium concentrations in blood from dogs with naturally acquired parvoviral enteritis. J Am Vet Med Assoc. 1998;212(9):1398–1401. | ||
Kocaturk M, Martinez S, Eralp O, Tvarijonaviciute A, Ceron J, Yilmaz Z. Prognostic value of serum acute phase proteins in dogs with parvoviral enteritis. J Small Anim Pract. 2010;51(9):478–483. | ||
Kocaturk M, Tvarijonaviciute A, Martinez-Subiela S, et al. Inflammatory and oxidative biomarkers of disease severity in dogs with parvoviral enteritis. J Small Anim Pract. 2015;56(2):119–124. | ||
McClure V, van Schoor M, Thompson PN, Kjelgaard-Hansen M, Goddard A. Evaluation of the use of serum C-reactive protein concentration to predict outcome in puppies infected with canine parvovirus. J Am Vet Med Assoc. 2013;243(3):361–366. | ||
Schoeman JP, Goddard A, Herrtage ME. Serum cortisol and thyroxine concentrations as predictors of death in critically ill puppies with parvoviral diarrhea. J Am Vet Med Assoc. 2007;231(10):1534–1539. | ||
Stander N, Wagner WM, Goddard A, Kirberger RM. Ultrasonographic appearance of canine parvoviral enteritis in puppies. Vet Radiol Ultrasound. 2010;51(1):69–74. | ||
Gray LK, Crawford PC, Levy JK, Dubovi EJ. Comparison of two assays for detection of antibodies against canine parvovirus and canine distemper virus in dogs admitted to a Florida animal shelter. J Am Vet Med Assoc. 2012;240(9):1084–1087. | ||
Litster AL, Pressler B, Volpe A, Dubovi E. Accuracy of a point-of-care ELISA test kit for predicting the presence of protective canine parvovirus and canine distemper virus antibody concentrations in dogs. Vet J. 2012;193(2):363–366. | ||
Day MJ, Horzinek MC, Schultz RD, Squires RA. WSAVA guidelines for the vaccination of the dogs and cats. J Small Anim Pract. 2016;57(1):E1–E45. | ||
Schmitz S, Coenen C, König M, Thiel HJ, Neiger R. Comparison of three rapid commercial canine parvovirus antigen detection tests with electron microscopy and polymerase chain reaction. J Vet Diagn Invest. 2009;21(3):344–345. | ||
Desario C, Decaro N, Campolo M, et al. Canine parvovirus infection: which diagnostic test for virus? J Virol Methods. 2005;126(1–2):179–185. | ||
Decaro N, Desario C, Beall MJ, et al. Detection of canine parvovirus type 2c by a commercially available in-house rapid test. Vet J. 2010;184(3):373–375. | ||
Decaro N, Desario C, Billi M, et al. Evaluation of an in-clinic assay for the diagnosis of canine parvovirus. Vet J. 2013;198(2):504–507. | ||
Proksch AL, Unterer S, Speck S, Truyen U, Hartmann K. Influence of clinical and laboratory variables on faecal antigen ELISA results in dogs with canine parvovirus infection. Vet J. 2015;204(3):304–308. | ||
Burton JH, Veir JK, Morris AK, Hawley JR, Lappin MR. Detection of canine parvovirus DNA from blood and feces collected from healthy puppies after administration of modified live vaccines. J Vet Intern Med. 2008;22(3):703. | ||
Decaro N, Elia G, Martella V, et al. A real-time PCR assay for rapid detection and quantitation of canine parvovirus type 2 in the feces of dogs. Vet Microbiol. 2005;105(1):19–28. | ||
Decaro N, Desario C, Elia G, et al. Occurrence of severe gastroenteritis in pups after canine parvovirus vaccine administration: a clinical and laboratory diagnostic dilemma. Vaccine. 2007;25(7):1161–1166. | ||
Decaro N, Crescenzo G, Desario C, et al. Long-term viremia and fecal shedding in pups after modified-live canine parvovirus vaccination. Vaccine. 2014;32(30):3850–3853. | ||
Decaro N, Elia G, Desario C, et al. A minor groove binder probe real-time PCR assay for discrimination between type 2-based vaccines and field strains of canine parvovirus. J Virol Methods. 2006;136(1–2):65–70. | ||
Decaro N, Martella V, Elia G, et al. Diagnostic tools based on minor groove binder probe technology for rapid identification of vaccinal and field strains of canine parvovirus type 2b. J Virol Methods. 2006;138(1–2):10–16. | ||
Otto CM, Jackson CB, Rogell EJ, Prior RB, Ammons WS. Recombinant bactericidal/permeability-increasing protein (rBPI21) for treatment of parvovirus enteritis: a randomized, double-blinded, placebo-controlled trial. J Vet Intern Med. 2001;15(4):355–360. | ||
Lobetti RG, Joubert KE, Picard J, Carstens J, Pretorius E. Bacterial colonization of intravenous catheters in young dogs suspected to have parvoviral enteritis. J Am Vet Med Assoc. 2002;220(9):1321–1324. | ||
Davis H. Central venous catheterization. In: Silverstein C, Hopper K, editors. Small Animal Critical Care Medicine. 3nd ed. St Louis, MO: Elsevier; 2009:267–270. | ||
Otto CM, Rieser TM, Brooks MB, Russell MW. Evidence of hypercoagulability in dogs with parvoviral enteritis. J Am Vet Med Assoc. 2000;217(10):1500–1504. | ||
Giunti M, Otto C. Intraosseous catheterization. In: Silverstein C, Hopper K, editors. Small Animal Critical Care Medicine. 2nd ed. St Louis, MO: Elsevier; 2009:263–267. | ||
Anastasio JD, Fletcher DJ, Rozanski EA. Crystalloid fluid therapy. In: Bonagura JD, Twedt DC, editors. Kirk’s Current Veterinary Therapy XV. 15th ed. St Louis, MO: Elsevier; 2014:2–7. | ||
Davis H, Jensen T, Johnson A, et al. 2013 AAHA/AAFP fluid therapy guidelines for dogs and cats. J Am Anim Hosp Assoc. 2013;49(3):149–159. | ||
Rudloff E, Kirby R. Colloid fluid therapy. In: Bonagura JD, Twedt DC, editors. Kirk’s Current Veterinary Therapy XV. 15th ed. St Louis, MO: Elsevier; 2014:8–14. | ||
Mazzaferro EM, Rudloff E, Kirby R. The role of albumin replacement in the critically ill veterinary patient. J Vet Emerg Crit Care. 2002;12(2):113–124. | ||
DiBartola SP, Autran de Morais H. Disorders of potassium: hypokalemia and hyperkalemia. In: Dibartola SP, editor. Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice. 3rd ed. St Louis, MO: Elsevier; 2006:91–121. | ||
Turk J, Fales W, Miller M, et al. Enteric Clostridium perfringens infection associated with parvoviral enteritis in dogs: 74 cases (1987-1990). J Am Vet Med Assoc. 1992;200(7):991–994. | ||
Abrams-Ogg A. Neutropenia. In: Day MJ, Kohn B, editors. BSAVA Manual of Canine and Feline Haematology and Transfusion Medicine. 2nd ed. Gloucester: BSAVA; 2012:117–125. | ||
Sedlacek HS, Ramsey DS, Boucher JF, Eagleson JS, Conder GA, Clemence RG. Comparative efficacy of maropitant and selected drugs in preventing emesis induced by centrally or peripherally acting emetogens in dog. J Vet Pharmacol Ther. 2008;31(6):533–537. | ||
De La Puente VA, Siedek EM, Benchaoui HA, Tilt N, Rowan TG, Clemence RG. The anti-emetic efficacy of maropitant (Cerenia™) in the treatment of ongoing emesis caused by a wide range of underlying clinical aetiologies in canine patients in Europe. J Small Anim Pract. 2007;48(2):93–98. | ||
Ramsey DS, Kincaid K, Watkins JA, et al. Safety and efficacy of injectable and oral maropitant, a selective neurokinin1 receptor antagonist, in a randomized clinical trial for treatment of vomiting in dogs. J Vet Pharmacol Ther. 2008;31(6):538–543. | ||
Narishetty ST, Galvan B, Coscarelli E, et al. Effect of refrigeration of the antiemetic Cerenia (Maropitant) on pain on injection. Vet Ther. 2009;10(3):93–102. | ||
Mantione NL, Otto CM. Characterization of the use of antiemetic agents in dogs with parvoviral enteritis treated at a veterinary teaching hospital: 77 cases (1997-2000). J Am Vet Med Assoc. 2005;227(11):1787–1793. | ||
Mohr AJ, Leisewitz AL, Jacobson LS, Steiner JM, Ruaux CG, Williams DA. Effect of early enteral nutrition on intestinal permeability, intestinal protein loss, and outcome in dogs with severe parvoviral enteritis. J Vet Intern Med. 2003;17(6):791–798. | ||
Bragg RF, Duffy AL, DeCecco FA, et al. Clinical evaluation of a single dose of immune plasma for treatment of canine parvovirus infection. J Am Vet Med Assoc. 2012;240(6):700–704. | ||
De Mari K, Maynard L, Eun HM, Lebreux B. Treatment of canine parvoviral enteritis with interferon-omega in a placebo-controlled field trial. Vet Rec. 2003;152(4):105–108. | ||
Martin V, Najbar W, Gueguen S, et al. Treatment of canine parvoviral enteritis with interferon-omega in a placebo-controlled challenge trial. Vet Microbiol. 2002;89(2–3):115–127. | ||
Savigny MR, Macintire DK. Use of oseltamivir in the treatment of canine parvoviral enteritis. J Vet Emerg Crit Care. 2010;20(1):132–142. | ||
Papaioannou E, Soubasis N, Theodorou K, et al. The potential role of Oseltamivir in the management of canine parvoviral enteritis in 50 natural cases. Orally presented at: BSAVA Congress; April 4–7, 2013; Birmingham, UK. | ||
Boscan P, Monnet E, Mama K, Twedt DC, Congdon J, Steffey EP. Effect of maropitant, a neurokinin 1 receptor antagonist, on anesthetic requirements during noxious visceral stimulation of the ovary in dogs. Am J Vet Res. 2011;72(12):1576–1579. | ||
Rewerts JM, McCaw DL, Cohn LA, Wagner-Mann C, Harrington D. Recombinant human granulocyte colony-stimulating factor for treatment of puppies with neutropenia secondary to canine parvovirus infection. J Am Vet Med Assoc. 1998;213(7):991–992. | ||
Mischke R, Barth T, Wohlsein P, Rohn K, Nolte I. Effect of recombinant human granulocyte colony-stimulating factor (rhG-CSF) on leukocyte count and survival rate of dogs with parvoviral enteritis. Res Vet Sci. 2001;70(3):221–225. | ||
Cohn LA, Rewerts JM, McCaw D, Daniel Boon G, Wagner-Mann C, Lothrop CD Jr. Plasma granulocyte colony-stimulating factor concentrations in neutropenic, parvoviral enteritis-infected puppies. J Vet Intern Med. 1999;13(6):581–586. | ||
Dimmit R. Clinical experience with cross-protective antiendotoxin antiserum in dogs with parvoviral enteritis. Canine Pract. 1991;16(3):23–26. | ||
Twark L, Dodds WJ. Clinical use of serum parvovirus and distemper virus antibody titers for determining revaccination strategies in healthy dogs. J Am Vet Med Assoc. 2000;217(7):1021–1024. | ||
Abdelmagid OY, Larson L, Payne L, Tubbs A, Wasmoen T, Schultz RD. Evaluation of the efficacy and duration of a canine combination vaccine against virulent parvovirus, infectious canine hepatitis virus, and distemper virus experimental challenges. Vet Ther. 2004;5(3):173–186. | ||
Mouzin DE, Lorenzen MJ, Haworth JD, King VL. Duration of serologic responses to five viral antigens in dogs. J Am Vet Med Assoc. 2004;224(1):55–60. | ||
Schultz RD, Thiel B, Mukhtar E, Sharp P, Larson LJ. Age and long-term protective immunity in dogs and cats. J Comp Pathol. 2010;142(Suppl 1):S102–S108. | ||
Spibey N, Greenwood NM, Sutton D, Chalmers WS, Tarpey I. Canine parvovirus type 2 vaccine protects against virulent challenge with type 2c virus. Vet Microbiol. 2008;128(1–2):48–55. | ||
Larson LJ, Schultz RD. Do two current canine parvovirus type 2 and 2b vaccines provide protection against the new type 2c variant? Vet Ther. 2008;9(2):94–101. | ||
Siedek EM, Schmidt H, Sture GH, Raue R. Vaccination with canine parvovirus type 2 (CPV-2) protects against challenge with virulent CPV-2b and CPV-2c. Berl Munch Tierarztl Wochenschr. 2011;124(1–2):58–64. | ||
Wilson S, Stirling C, Borowski S, Thomas A, King V, Salt J. Vaccination of dogs with Duramune DAPPi+LC protects against pathogenic canine parvovirus type 2c challenge. Vet Rec. 2013;172(25):662. | ||
Decaro N, Desario C, Elia G, et al. Evidence for immunization failure in vaccinated adult dogs infected with canine parvovirus type 2c. New Microbiol. 2008;31(1):125–130. | ||
Decaro N, Cirone F, Desario C, et al. Severe parvovirus in a 12-year-old dog that had been repeatedly vaccinated. Vet Rec. 2009;164(19):593–595. | ||
Ling M, Norris JM, Kelman M, Ward MP. Risk factors for death from canine parvoviral-related disease in Australia. Vet Microbiol. 2012;158(3–4):280–290. | ||
Mittal M, Chakravarti S, Mohapatra JK, et al. Molecular typing of canine parvovirus strains circulating from 2008 to 2012 in an organized kennel in India reveals the possibility of vaccination failure. Infect Genet Evol. 2014;23:1–6. | ||
Stepita ME, Bain MJ, Kass PH. Frequency of CPV infection in vaccinated puppies that attended puppy socialization classes. J Am Anim Hosp Assoc. 2013;49(2):95–100. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
