Back to Journals » Clinical Epidemiology » Volume 16
Cancer Survival Trends in Southeastern China, 2011–2021: A Population-Based Study
Authors Zhou Y, Wen Y, Xiang Z , Ma J, Lin Y, Huang Y, Chen C
Received 26 September 2023
Accepted for publication 17 January 2024
Published 1 February 2024 Volume 2024:16 Pages 45—56
DOI https://doi.org/10.2147/CLEP.S442152
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Vera Ehrenstein
Yan Zhou,1,* Yeying Wen,1,* Zhisheng Xiang,1,* Jingyu Ma,1 Yongtian Lin,1 Yongying Huang,1 Chuanben Chen2
1Department of Epidemiology, Clinical Oncology School of Fujian Medical University and Fujian Cancer Hospital, Fuzhou, People’s Republic of China; 2Department of Radiation Oncology, Clinical Oncology School of Fujian Medical University and Fujian Cancer Hospital, Fuzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chuanben Chen, Department of Radiation Oncology, Clinical Oncology School of Fujian Medical University and Fujian Cancer Hospital, Fuzhou, People’s Republic of China, Tel +86-591-83660063, Email [email protected]
Purpose: The 5-year cancer survival rate among Chinese patients is lower than that among patients in developed countries and varies widely across geographic regions. The aim of this study was to analyse the 5-year relative cancer survival rate in southeastern China, between 2011 and 2021.
Patients and Methods: We utilised population-based statistics from 12 cancer registries in Fujian, China. Study population data were up to date as of Dec 31, 2019, and survival outcome status was updated as of Dec 31, 2021. We used the ICD-10 and the ICD-O-3 to categorize all cancer cases. We analysed the 5-year relative survival for cancers combined and different cancer types stratified by sex, urban and rural areas, and age. Survival estimates were stratified according to calendar period (2011– 13, 2014– 15, 2016– 18 and 2019– 21).
Results: Ultimately, a total of 160,294 cancer patients were enrolled in the study. In 2011– 13, 2014– 15, 2016– 18 and 2019– 21, the age-standardised 5-year relative survival for cancers combined were 29.1% (95% CI: 28.6– 29.7), 31.5% (95% CI: 31.0– 32.0), 36.8% (95% CI: 36.4– 37.3) and 39.1% (95% CI: 38.7– 39.6), respectively. The age-standardised 5-year relative survival for lung, prostate, larynx, colon-rectum, kidney and bone cancers increased 4.3%, 4.0%, 3.8%, 3.4%, 3.4% and 2.70%, respectively. Cancers with high 5-year relative survival rates (> 60%) in 2019– 21 included thyroid, testis, breast, bladder, cervix, prostate and uterus cancers. The 5-year survival rates in 2019– 2021 was higher for females than for males (47.8% vs 32.0%) and higher in urban areas than in rural areas (41.7% vs 37.1%). Relative survival rates decreased with increasing age.
Conclusion: The 5-year cancer survival in Fujian Province increased between 2011 and 2021 but remained at a low level. Building a strong primary public health system may be a key step in reducing the cancer burden in Fujian Province.
Keywords: relative survival, cancer, population-based study, cancer registry
Introduction
Cancer is a major disease that seriously endangers the health of the population and has become an important public health problem worldwide.1 GLOBOCAN 2020 estimates that China accounts for 23.7% of the 19.29 million newly diagnosed cancer cases globally.2 The incidence of cancer in China exceeds the global average; therefore, effective cancer control is a serious challenge to the health care system in a country with one-fifth of the global population.
Population-level cancer survival is a critical measure of the quality of cancer care delivery and is of great importance for making progress in cancer control for a specific region.3 Population-based Cancer survival statistics from 17 cancer registries released by the National Cancer Centre of China indicated that the age-standardised 5-year relative cancer survival rose significantly from 30.9% in 2003–2005 to 40.5% in 2012–2015 in China,4 but it was still at a low level compared to developed countries.5 Furthermore, survival rates varied widely across geographic regions.6
In this study, we focus on the survival trend of cancer patients in Fujian Province, China. Fujian is a province on the southeast coast of China, with a population of 41.5 million and a gross domestic product (GDP) per capita of ¥116,939 (approximately $16,749) in 2021.7 Cancer has become the main reason for mortality in the region and is one of the major diseases that poses a serious health risk to residents.8
Therefore, to understand the trend in survival of cancer patients in Fujian Province, this study collected and pooled cancer follow-up data from 12 registries in Fujian Province, calculated population-based 5-year cancer survival rates, analysed the reasons for the change in survival rates, and provided a scientific foundation for the formulation of cancer management and control programmes and the evaluation of their effectiveness.
Materials and Methods
Data Collection
Fujian Province created population-based cancer registries in 2009.9 The Fujian Cancer Prevention and Control Office is in charge of cancer surveillance in the region and regularly collects cancer data from the various cancer registries within its jurisdiction. Data for this research were obtained from 12 registries under the Fujian Cancer Prevention and Control Office, of which 4 registries (Changtai, Fuqing, Xinluo, and Yongan) had a study population of cancer patients diagnosed between 2014 and 2019, while the remaining 8 registries had a study population of cancer patients diagnosed between 2011 and 2019. The survival outcome status of all cases examined herein was up to date as of Dec 31, 2021.
We coded and classified all cancer cases using the tenth edition of the International Classification of Diseases (ICD-10) and the third edition of the International Classification of Diseases for Oncology (ICD-O-3). The registration covers all malignant tumours (C00-C97, D45-D47), benign tumours of the central nervous system (D32-D33) and dynamic undetermined tumours of the central nervous system (D42-D43). The final dataset included the diagnosis date, morphology, anatomical site, date of last contact, and behaviour code. Each registry utilised a combination of passive and active follow-up to access the survival status. Passive follow-up was conducted using population-wide cause-of-death surveillance information matched with cancer registry information to obtain the time of death and underlying cause of death. Active follow-up entailed telephone and regular visits to identify the survival of patients. Demographic information was obtained from the Public Security Household Registration Department. The number of all-cause mortality and the corresponding population (stratified by sex and age group) for each year between 2011 and 2021 were obtained from the cause of death surveillance departments in the registration areas and were used to create the Simple Life Table.
Quality Control and Exclusions
Guidelines for Chinese Cancer Registration and International Agency for Research on Cancer/International Association of Cancer Registries (IARC/IACR) were used to identify the combinations between cancer site and morphology.10,11 We also examined the concordance between the combination of date of birth and diagnosis with follow-up. Unusual cases were returned to local registries to verify the validity of the data. If a case was based on a death certificate only, if there was unknown vital status, or if the case had two or more primary malignant tumours, the case was excluded from our study.
Statistical Analysis
The “Fujian Cancer Registration Information System” was developed by the Fujian Cancer Prevention and Control Office and was used to collate and export the data. We used relative survival as the primary index, which was computed as the proportion of the observed survival rate to the expected survival rate of a similar cohort in the population at large. We evaluated expected survival according to the Ederer II method.12 The Elandt-Johnson method was used to smooth the Abridged life tables into the full life table and extend it to 99 years.13 The years of diagnosis were divided into four calendar periods: 2011–13, 2014–15, 2016–18 and 2019–21. The cohort method was used to compute relative survival for 2011–13 and 2014–15; the complete method was used to compute relative survival for 2016–18; and the hybrid method was used to predict relative survival for 2019–21.14
According to the International Cancer Survival Standards (ICSS), the patients were divided into five main age groups (0–44 years old, 45–54 years old, 55–64 years old, 65–74 years old and 75–99 years old). The age-standardised relative survival of most cancers was calculated according to the ICSS1 as follows: 0–44 years, 7%; 45–54 years, 12%; 55–64 years, 23%; 65–74 years, 29%; and 75–99 years, 29%. The age-standardised relative survival of nasopharyngeal, cervix, brain, thyroid, and bone cancer was calculated according to the ICSS2 as follows: 0–44 years, 28%; 45–54 years, 17%; 55–64 years, 21%; 65–74 years, 20%; and 75–99 years, 14%.15 To assess changes in survival differences between regions, we divided the registries into rural and urban areas and compared survival differences among regions based on the regional classification of the National Bureau of Statistics of China. To quantify the change in survival, we calculated the absolute average change across consecutive diagnosis periods. We used a weighted linear regression with the linear trend assumption to test the survival differences between successive periods for statistical significance. The weight for each survival estimate was its variance. The linear regression slope gives estimates of the mean change among consecutive diagnosis periods and the 95% CI from their standard errors. Descriptive analyses were performed using SAS (version 9.2), and survival analyses were performed using the program strs in Stata (version 14.0).16
Results
Basic Information
Data were collected from 8 registries for 2011–13 and 12 registries for 2014–21. The number of cancer cases that met the data review criteria in the 12 cancer registries between 2011 and 2019 was 167,768, and after excluding 1527 cases with death certificates only, 1493 cases with unknown vital status cases and 4446 cases with multiple primary tumors, a total of 160,294 cases were ultimately enrolled in the analysis (Table 1 and Figure S1). Of these, 93,232 (58.16%) were males and 67,062 (41.84%) were females, with 73,623 (45.93%) cases in urban areas and 86,671 (54.07%) in rural areas. The 12 registries were located in areas with a household registered population of 7,800,280 in 2019, representing 20.02% of the province’s household registered population. The proportion of all cancer patients diagnosed by morphology was 71.49%. The numbers of patients enrolled in the analyses by sex and cancer type are shown in Table 2 and Figure S2.
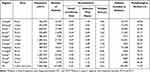 |
Table 1 Characteristics of the Study Population |
 |
Table 2 Number of Patients Included in the Analyses by Sex and Type of Cancer |
Overall 5-Year Relative Survival
In 2011–13, 2014–15, 2016–18 and 2019–21, the age-standardised 5-year relative survival for all cancers were 29.1% (95% CI: 28.6–29.7), 31.5% (95% CI: 31.1–32.0), 36.8% (95% CI: 36.4–37.3) and 39.1% (95% CI: 38.7–39.6), respectively. In all four time periods, the age-standardised 5-year relative survival was lower for males than for females and was higher in urban areas than in rural areas (Table 3).
 |
Table 3 Overall 5-Year Relative Survival Rates for All Cancers Combined |
Relative Survival of Each Cancer Type
Age-standardised 5-year relative survival differed substantially by type of cancer: the lowest 5-year relative survival was 6.5% (95% CI: 5.0–8.3) for pancreatic cancer, and the highest rate was 94.5% (95% CI: 90.9–96.7) for thyroid cancer in 2019–2021 (Table 4). Cancers with high 5-year relative survival (>60%) in 2019–2021 included thyroid, testis, breast, bladder, cervix, prostate and uterus cancers. The low 5-year relative survival rates (<30%) were for pancreatic, liver, gallbladder, oesophagus, leukaemia, lung and bone cancers during the same period. In 2011–2021, the survival rates for oral cavity and pharynx, oesophagus, stomach, colon-rectum, larynx, lung, bone, prostate, kidney, bladder and lymphoma cancers improved significantly over time, with an increase of 1.8%, 1.7%, 0.9%, 3.4%, 3.8%, 4.3%, 2.7%, 4.0%, 3.4%, 1.8% and 2.4%, respectively (Table 4).
 |
Table 4 Trends in Age-Standardised 5-Year Relative Survival Rates by Cancer Type(95% CI) |
Differences in Relative Survival by Sex
For all cancers combined, the survival rate among female patients was 10.9–15.8% higher than that among male patients in all time periods (Table 3). Survival rate was better in female patients than in male patients in almost all cancer types in 2019–2021, with the exception of thyroid, gallbladder, leukaemia, liver and stomach cancer. Overall survival improved for all cancers combined and for cancers of the colon-rectum, lung, and bladder in both males and females. For females, breast cancer survival rates also improved (Figure 1).
 |
Figure 1 Age-standardised 5-year relative survival rates by sex. (A) Male patients; (B) Female patients. |
Differences in Relative Survival Between Urban and Rural Areas
In 2011–2021, for the 4 calendar periods, the age-standardised 5-year relative survival for cancer patients in urban areas was higher than that in rural areas by 3.6%, 3.0%, 4.2% and 4.6%, respectively. For the ten most common cancers in Fujian Province, survival was higher in urban areas than in rural areas, except for lung cancer (2011–2015), liver cancer (2014–2015) and thyroid cancer (2011–2021). From 2011–2021, survival for all ten common cancers increased in lung cancer, colon-rectum cancer, thyroid cancer in urban areas and lung cancer, colon-rectum cancer, lymphoma in rural areas (Table 5).
 |
Table 5 Age-Standardised 5-Year Relative Survival Rates for All Cancers Combined and ten Major Cancers by Area |
Differences in Relative Survival by Age Group
The five-year relative survival rate of older patients was typically lower than that of younger patients over the four time periods. The 5-year relative survival rate for all cancers decreased with older age. In 2019–2021, the 5-year relative survival rate for patients under 45 years of age was 73.4%, while the rate for patients 75 years of age and over was 18.9%. There was an absolute variation of 54.5% among the two arms. The 5-year relative survival rate for all cancers combined, lung cancer, colon-rectum cancer, breast cancer and lymphoma increased in all age groups between 2011 and 2021 (Figure 2 and Table S1).
 |
Figure 2 5-year relative survival for all cancers combined and ten major cancers, by age. |
Discussion
Population-level cancer survival is widely considered to be a critical measure of the overall success of health systems in preventing and controlling cancer.17 This study is the first systematic analysis of population-level cancer follow-up data from 12 cancer registry areas in Fujian Province, China. The findings provide insight into the changes in survival and prognosis of cancer patients in southeast China over the last decade.
The findings of this research indicated that the age-standardised 5-year cancer survival for all cancers combined in Fujian Province improved markedly over time, from 29.1% in 2011–2013 to 39.1% in 2019–2021. We also noted remarkable improvement in the 5-year survival rates for eleven cancers: lung, oral cavity and pharynx, oesophagus, stomach, colon-rectum, larynx, bone, prostate, kidney, bladder and lymphoma cancers. Improvements in cancer survival rates are strongly associated with the funding of cancer health care services and the expansion of insurance coverage.18 Actual factors like improved primary health care, the availability of diagnostic equipment and increased levels of therapy contribute significantly to improved survival rates.19,20 In order to adapt to the fast growth of the national economy, the Chinese government has increased its investment in health resources in recent years.21 In 2005, the National Health Commission of China included cancer screening and early detection programs in the scope of central financial subsidies for local public health special funds support. These programs were initially conducted in rural regions with a significant prevalence of selected cancer category; by 2015, the programs were expanded to 31 provinces.22 Furthermore, by analysing the 5-year survival rates for different cancer types, we found that the survival rate for lung cancer increased substantially – from 13.3% in 2011–2013 to 25.4% in 2019–2021, a change of 62.77%. This could be related to the spread of health education about lung cancer, the increased rate of early detection, and the improvement of treatment methods.23,24 In particular, advances in technology and systemic therapy have led to dramatic improvements in the prognosis of lung cancer patients.25
The age-standardised 5-year survival rate in Fujian Province was 31.5% in 2014–2015, lower than the national survival rate of 40.5% during the same period (2012–2015).4 Regarding the major cancer types in the country, the 5-year survival rates of lung, liver, stomach, colorectal and oesophageal cancer in Fujian Province were 15.6%, 11.2%, 29.2%, 45.5%, and 17.6%, respectively, which were lower than the national rates (19.7%, 12.1%, 35.1%, 56.9%, and 30.3%, respectively) during the corresponding time period. The 5-year survival rates of thyroid and brain cancer were 86.9% and 42.9%, respectively, higher than the national rates (84.3% and 26.7%, respectively). This discrepancy may be due, on the one hand, to the fact that the nationally reported survival of 40.5% is on the basis of statistics from registries with financial status that is higher the national average, and thus, the true national survival level may be lower than 40.5%. On the other hand, the 5-year survival rates of lung, liver, stomach and colon-rectum cancers, which account for a high proportion of cancers in Fujian Province, were lower than the national rates. This suggests that the intervention, early diagnosis and treatment of common cancers such as lung, liver, stomach and colon-rectum cancer in Fujian Province still need to be further strengthened. In comparison with other Chinese provinces, we observed that the age-standardised 5-year survival rate in Fujian Province was similar to that in Shandong Province26 (39.1% in 2019–2021 vs 40.2% in 2018–20, respectively). This similarity reflects the smaller differences in cancer survival between regions with similar gross domestic product (GDP) per capita.
The data regarding survival differences between male and female patients for cancers combined indicate that females have better cancer survival rates than males (47.8% vs 32.0% in 2019–2021, respectively), which is strongly related to the different composition of each cancer type in males and females. The top four cancers among males in Fujian Province were lung, liver, stomach and colon-rectum cancer. The survival rates for stomach and colon-rectum cancer were 31.9% and 51.8%, respectively; the survival rates of the other two cancers were less than 20%. The most common cancers among females were breast, thyroid, lung and colon-rectum cancer. The survival rates for both lung and colon-rectum cancer were higher among females than among males, and the survival rates for breast cancer and thyroid cancer were as high as 75.9% and 93.8%, thus indicating improved survival among females. In terms of sex differences in survival among cancer types, such variation should be further investigated to obtain clinical evidence.
Cancers’ combined survival also improved over time in urban and rural areas to varying degrees, and the level of survival was higher overall in urban areas (41.7%) than in rural areas (37.1%). Additionally, survival rates for the majority of cancer types were greater in urban areas than in rural areas. Economic status, level of social support, health-seeking behaviours, and treatment technology all contribute to the outcomes of cancer. We can see the efforts of the government to constantly reduce the disparity between urban and rural areas. Government initiatives to distribute more medical resources proportionally to rural areas to enhance cancer health care have been beneficial in reducing survival disparities between regions.27 In addition, since 2003, China has begun to resolve the economic burden of large medical expenses on rural families through the New Rural Cooperative Medical System and has gradually increased the rate of reimbursement.28 This expansion of insurance coverage for cancer patients, especially in rural and isolated regions, has the possibility to improve overall survival even further.
Age-specific survival disparities are an essential public health concern and need additional focus. Survival for most cancers decreased with age, meaning that there was a very significant survival disadvantage for older adults (≥65 years). Most of the elderly patients with cancer were middle to late stage at diagnosis and have relatively less intention for treatment, and elderly patients have more comorbidities, such as combined cardiovascular and cerebrovascular diseases, resulting in less survival than young and middle-aged patients.29
This study provides an updated temporal and regional comparison of cancer survival utilising population-level data from cancer registries in Fujian Province, complementing the epidemiological data on cancer survival in southeastern China. All 12 cancer registries in the present research used a combination of passive and active follow-up to obtain survival outcomes for cancer patients. Active follow-up can decreases the effect of follow-up bias, provide accurate survival data, and avoid an excessive upwards bias in estimates of cancer survival caused by the sole use of passive follow-up.30 However, some limitations should be taken into account when explaining these cancer survival estimates. First, like many studies, our study inevitably suffers from the effects of statistical biases, for example, lead-time bias and overdiagnosis, leading to overestimation of survival. Second, the coverage areas are the registration areas in Fujian Province, which could not completely reflect the cancer survival rates of the province. The following will be a compilation and analysis of all the province’s cancer registration data to gain a further more complete and precise picture of cancer survival.
Conclusion
The 5-year cancer survival rate in Fujian Province increased between 2011 and 2021 but remained at a low level. Therefore, to reduce cancer burden and improve quality of life, it is necessary to strengthen primary and secondary prevention programs for the general public with flexible procedures and multiple measures and to deliver evidence-based treatments within a medically admissible time frame.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are contained within the Fujian Cancer Prevention and Control Office, but are not publicly available due to confidentiality, security and ownership matters. They may be available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Institutional Review Board of Fujian Cancer Hospital (No. 2017-047-01). The need of informed consent was waived by Research Ethics Review Committee of Fujian Cancer Hospital due to retrospective and anonymous study design. All methods were performed in accordance with the relevant guidelines and regulations.
Acknowledgments
The authors thank the staff of the Fujian Cancer Registries whose endless efforts to collect accurate and complete data have made this report possible.
Disclosure
The authors report no conflicts of interest in this work.
References
1. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222.
2. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
3. Arnold M, Rutherford MJ, Bardot A, et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 2019;20(11):1493–1505. doi:10.1016/S1470-2045(19)30456-5
4. Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Global Health. 2018;6(5):e555–e567. doi:10.1016/S2214-109X(18)30127-X
5. Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (Concord-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075.
6. Li Y, Yu L, Na J, et al. Survival of cancer patients in Northeast China: analysis of sampled cancers from population-based cancer registries. Cancer Res Treat. 2017;49(4):1106–1113. doi:10.4143/crt.2016.613
7. National bureau of statistics of the People’s Republic of China. Zhonghua renmin gongheguo guojia tongjiju; 2023. Available from: http://www.stats.gov.cn/.
8. Ye Y, Zhong W, Huang S, Li X. Fujian sheng 1990-2010 nian jumin chusheng qiwang shouming [A comparison study on the life expectancy among residents in Fujian province, 1990–2010]. Chin J Epidemiol. 2014;35(3):280–284. Chinese.
9. Wei W, Zeng H, Zheng R, et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol. 2020;21(7):e342–e349. doi:10.1016/S1470-2045(20)30073-5
10. Wei K-R, Chen W-Q, Zhang S-W, et al. Cancer registration in the Peoples Republic of China. Asian Pac J Cancer Prev. 2012;13(8):4209–4214.
11. Curado M-P, Edwards B, Shin HR, et al. Cancer Incidence in Five Continents, Volume IX. IARC Press, International Agency for Research on Cancer; 2007.
12. Ederer F, Heise H. Instructions to IBM 650 Programmers in Processing Survival Computations. Bethesda, MD: National Cancer Institute; 1959.
13. Eldandt-Johnson R, Johnson N. Survival Models and Data Analysis (Wiley Series in Probability and Mathematical Statistics). Indianapolis: Wiley; 1980.
14. Brenner H, Rachet B. Hybrid analysis for up-to-date long-term survival rates in cancer registries with delayed recording of incident cases. Eur J Cancer. 2004;40(16):2494–2501. doi:10.1016/j.ejca.2004.07.022
15. Corazziari I, Quinn M, Capocaccia R. Standard cancer patient population for age standardising survival ratios. Eur J Cancer. 2004;40(15):2307–2316. doi:10.1016/j.ejca.2004.07.002
16. Brenner H, Gefeller O, Hakulinen T. A computer program for period analysis of cancer patient survival. Eur J Cancer. 2002;38(5):690–695. doi:10.1016/S0959-8049(02)00003-5
17. Coleman MP. Cancer survival: global surveillance will stimulate health policy and improve equity. Lancet. 2014;383(9916):564–573. doi:10.1016/S0140-6736(13)62225-4
18. Brown S, Castelli M, Hunter DJ, et al. How might healthcare systems influence speed of cancer diagnosis: a narrative review. Soc Sci Med. 2014;116:56–63. doi:10.1016/j.socscimed.2014.06.030
19. Nielsen M. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993;328(17):1237–1243. doi:10.1056/NEJM199304293281706
20. Li X, Lu J, Hu S, et al. The primary health-care system in China. Lancet. 2017;390(10112):2584–2594. doi:10.1016/S0140-6736(17)33109-4
21. Cai Y, Xue M, Chen W, et al. Expenditure of hospital care on cancer in China, from 2011 to 2015. Chin J Cancer Res. 2017;29(3):253–262. doi:10.21147/j.issn.1000-9604.2017.03.11
22. Xiao-Nong Z, Xiao-Nong Z. Epidemic trend, screening, and early detection and treatment of cancer in Chinese population. Cancer Biol Med. 2017;14(1):50–59. doi:10.20892/j.issn.2095-3941.2016.0047
23. Luo YH, Chiu CH, Kuo C, et al. Lung cancer in Republic of China. J Thorac Oncol. 2021;16(4):519–527. doi:10.1016/j.jtho.2020.10.155
24. Chen P, Liu Y, Wen Y, Zhou C. Non-small cell lung cancer in China. Cancer Commun. 2022;42(10):937–970.
25. Howlader N, Forjaz G, Mooradian MJ, et al. The effect of advances in lung-cancer treatment on population mortality. N Engl J Med. 2020;383(7):640–649. doi:10.1056/NEJMoa1916623
26. Jiang F, Fu ZT, Lu ZL, et al. 2012-2018 nian shandong sheng zhongliu dengji diqu aizheng xinfa bingli de shengcun fenxi [Cancer survival during 2012–2018 in cancer registries of Shandong Province]. Chin J Prev Med. 2022;56(6):806–814. Chinese.
27. Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–814. doi:10.1016/S0140-6736(12)60278-5
28. Li D, Zhang J, Yang J, et al. Socio-economic inequalities in health service utilization among Chinese rural migrant workers with new cooperative medical scheme: a multilevel regression approach. BMC Public Health. 2022;22(1):1–14. doi:10.1186/s12889-021-12274-7
29. Zeng C, Wen W, Morgans AK, et al. Disparities by race, age, and sex in the improvement of survival for major cancers: results from the national cancer institute Surveillance, Epidemiology, and End Results (SEER) program in the United States, 1990 to 2010. JAMA Oncol. 2015;1(1):88–96. doi:10.1001/jamaoncol.2014.161
30. Swaminathan R, Rama R, Shanta V. Lack of active follow-up of cancer patients in Chennai, India: implications for population-based survival estimates. Bull World Health Organ. 2008;86(7):509–515. doi:10.2471/BLT.07.046979
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
