Back to Journals » Journal of Pain Research » Volume 13
Big Five Personality Traits and Disabling Chronic Low Back Pain: Association with Fear-Avoidance, Anxious and Depressive Moods
Authors Ibrahim ME , Weber K, Courvoisier DS, Genevay S
Received 6 November 2019
Accepted for publication 24 March 2020
Published 14 April 2020 Volume 2020:13 Pages 745—754
DOI https://doi.org/10.2147/JPR.S237522
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Maha Emad Ibrahim,1,2 Kerstin Weber,3 Delphine S Courvoisier,1,4,5 Stéphane Genevay1
1Division of Rheumatology, University Hospitals of Geneva, Geneva, Switzerland; 2Department of Physical Medicine, Rheumatology and Rehabilitation, Suez Canal University, Ismailia, Egypt; 3Medical Direction, University Hospitals of Geneva, Geneva, Switzerland; 4Quality of Care Service, Geneva University Hospitals, Geneva, Switzerland; 5Department of Readaptation and Geriatrics, University of Geneva, Geneva, Switzerland
Correspondence: Maha Emad Ibrahim
Department of Physical Medicine, Rheumatology and Rehabilitation, Suez Canal University, Ring Road, Ismailia 41511, Egypt
Tel +20 1005607210
Email [email protected]
Purpose: Physical dysfunction in chronic low back pain patients is influenced by psychological variables rather than by pain severity. Assessing personality traits may help clinicians address the complexity of patients’ experiences and design treatments that target these vulnerabilities. This study aimed to identify the distinguishing personality traits of a cohort of patients with disabling chronic low back pain and to determine associations between those traits and fear-avoidance beliefs, depressive, and anxious moods.
Patients and Methods: This cross-sectional study included 102 chronic low back pain patients (57% male), who failed standard management and were referred to a multidisciplinary rehabilitation program. All patients completed the five domains of the NEO Personality Inventory (NEO PI)–Revised (Neuroticism, Extraversion, Openness to experience, Agreeableness and Conscientiousness), the Tampa Scale for Kinesiophobia (TSK), and the Hospital Anxiety and Depression Scale (HADS). One-sample t-test was used to compare sample personality means with average population norms. Association between the five personality domains with TSK and HADS was assessed using Pearson’s correlation, adjusted for patient demographics and pain-related variables. Linear regression was used to estimate associations adjusted for covariates.
Results: Both men and women had significantly lower scores in the Openness to experience domain and significantly higher scores in the Conscientiousness domain than the general population norms. After adjusting for covariates, Neuroticism was associated with higher fear-avoidance, depression and anxiety scores. Conversely, Extraversion and Openness to experience negatively correlated with depression scores. Extraversion also inversely correlated with fear-avoidance. Conscientiousness negatively correlated with depression and anxiety after adjustment.
Conclusion: Patients with disabling chronic low back pain show personality characteristics that deviate significantly from the normal population norms but do not reach maladaptive forms of personality disorders. Clinicians would benefit from assessing patients’ personality traits to address protective and risk factors for psychological distress, particularly in difficult-to-treat, highly disabled low back pain patients.
Keywords: NEO PI, anxiety, depression, kinesiophobia, chronic low back pain, personality
Plain Language Summary
Chronic low back pain is one of the most common and costly healthcare problems. Research has shown that chronic low back pain is not just a physical disruption of the spine, rather it results from the combined effect of physical, psychological and social factors. One of the most important psychological factors is the personality type of the patient. Personality type refers to the psychological classification of people into different categories according to their preferences, tendencies, and consistent behaviors. It has been shown in research that personality type can affect one’s perception of pain, the duration of pain, as well as how one copes with painful experiences. The current study aimed to find out if chronic low back pain patients have a distinct personality type, and whether the patients’ personality type relates to being depressed, anxious or afraid to move because of the pain.
Our study found that both men and women with chronic low back pain had lower scores in the Openness to experience domain and higher scores in the Conscientiousness domain. This means that disabled low back pain patients may be less curious, and they may also be less open to their emotions. They also have a tendency to plan their moves cautiously. Patients with a higher personal tendency to experience negative emotions were more likely to be depressed and anxious.
We therefore conclude that patients with disabling chronic low back pain show characteristic personality features that make them more prone to be anxious, depressed and afraid to move because of their pain. Physicians would benefit from assessing patients’ personalities to address protective and risk factors for psychological distress in those patients.
Introduction
Low back pain is a major health problem, and a leading cause of disability worldwide.1,2 The majority of patients have mild episodes with favorable functional outcomes.3 Nevertheless, a proportion of those patients progress into chronic low back pain, when the pain persists for more than 3 months and is usually associated with significant disability.1 These patients drive most of the direct and indirect costs associated with low back pain.4,5 Failure of recovery and transition to chronicity are more influenced by psychological determinants, than by physical or social ones.6–8 Such determinants including depression, anxiety, and fear-avoidance beliefs, affect patient adherence to treatment,9 and are strong predictors of long-term disability and poor quality of life.10,11
Patients’ well-being is more closely dependent on psychological resources and subjective evaluations than on objective parameters. Pain-related beliefs and pain-coping strategies are known to be predictive of adjustment to chronic pain.12–16 According to the fear-avoidance model, individuals maintain chronic pain as a result of negative appraisal of pain, which evokes catastrophic thinking, leading to pain-related fear, and ultimately to avoidant behavior.17,18 Previous studies have suggested that acceptance and catastrophizing about chronic pain are associated with patients’ personality traits.19,20 The diathesis stress model suggests that personality traits existing before the onset of chronic pain are activated and aggravated when confronted with stressful life events, such as chronic pain. Those same traits may trigger psychopathology and pain catastrophizing, leading to avoidant and disabling attitudes.21 For instance, patients with personality traits such as high Neuroticism and negative affect present more catastrophic thoughts about pain, which lead to kinesiophobia, and eventually to poor pain adjustment, higher pain intensity and depression.17,22 Further, depending on their personality traits, some patients with chronic low back pain are more prone to the development of central sensitization symptoms, causing a dysregulation of the central nervous system with neuronal hyperexcitability to both noxious and non-noxious pain stimuli.23
Existing evidence on the personality and pain coping relationship comes from heterogeneous samples including a wide variety of chronic pain conditions such as fibromyalgia, headache and migraine, trigeminal neuropathy, as well as musculoskeletal disorders.19,24,25 Studies specifically focusing on the personality–pain-coping relationship in patients with chronic low back pain remain scarce.14,23,26,27 It is thus important to identify the patients whose personality traits put them most at risk of maladjustment to pain and negative mood, subjecting them to the risk of pain recurrence and chronicity, as well as long-term disability, and hence design interventions that seek to modify their behaviors to avoid further pain.13,14
In addition, previous studies have mainly focused on maladaptive personality traits or personality traits corresponding with psychiatric diagnosis in pain patients.19,28 Conversely, trait models of personality, such as the Five-Factor Model,15 view personality along a continuum rather than a categorical approach and avoid distinguishing between clinically significant personality maladaptation diagnosed as personality disorders and healthy conditions of personality. Trait models define personality traits as enduring patterns of thoughts, feelings and behaviours, which are formed through childhood and increase in consistency throughout life. The Five-Factor Model determines each person’s individuality according to five broad dimensions: Neuroticism contrasts emotional stability with negative emotionality associated notably with pain, Extraversion implies an energetic approach towards social life and activity, Openness to experience describes the depth and complexity of patients’ mental and experiential life, Agreeableness describes how patients relate to others in terms of trust and altruism and Conscientiousness defines task- and goal-oriented behaviour including pain management.15 Among these five broad personality dimensions, most pain studies limited their focus on the role of Neuroticism, which is known to increase vulnerability to develop depression,16,29 anxiety,30,31 kinesiophobia22 and pain catastrophizing.17,25 Most studies predominantly considered personality traits to be risk factors, neglecting their protective role. Yet, patients with a high level of Agreeableness rely on their social support network to relieve their emotional distress. In addition, high levels of Conscientiousness have been positively related to acceptance of life with the disease,13 while low levels of Conscientiousness may lead to difficulties in defining meaningful goals, low motivation, and problems with adaptive coping.25
Therefore, the present cross-sectional study adopted a trait model perspective and specifically assessed all five personality dimensions in a homogeneous carefully selected sample of 102 patients presenting with disabling chronic low back pain, without current psychiatric disorders, and analyzed how personality traits are associated with anxious and depressive mood as well as with fear-avoidance beliefs.
Patients and Methods
Program and Participants
This is a cross-sectional study of chronic highly disabled low back pain patients joining the multidisciplinary biopsychosocial rehabilitation program run at the University Hospitals of Geneva, Switzerland. The program is designed for patients who are still highly disabled despite standard care from their general practitioner, including pain medication and individual exercised based physiotherapy.
This program for chronic low back pain patients was designed in 2005 to restore the individual’s musculoskeletal function. A multidisciplinary team (rheumatologist, rehabilitation physician, pain specialist, psychiatrist, physical therapists, occupational therapists and a psychologist) run the setup, essentially following small groups of four to six patients in a high-intensity, outpatient four-week program of a total of 100 hours, as previously described in detail in an earlier publication.32,33 Basically, this program aimed to integrate cognitive behavioral components, and work-related goals and outcomes, into sessions of land- and pool-based physical therapy, and spine ergonomic counselling and psychological support.
To enroll in this program, patients had to be 18 to 65 years old and suffering from disabling non-specific chronic low back pain (with or without radiating leg pain) for more than 3 months, despite standard medical and exercise-based physical therapy prescribed by their general practitioner. Exclusion criteria were specific low back pain due to infection, a tumor, spondyloarthropathy, radicular leg pain due to disc herniation, and neurogenic claudication related to spinal stenosis. The diagnosis of chronic non-specific low back pain was confirmed by a senior Rehabilitation physician or a Rheumatologist. Patients suffering from medical comorbidities that could interfere with or prohibit their participation (e.g., cardiac or pulmonary failure, severe mood disorder, disabling knee osteoarthritis), or from neck pain or diffuse chronic pain syndrome (including fibromyalgia, chronic fatigue syndrome and somatoform disorders), were also excluded, as well as patients with current active psychiatric diagnosis, such as major depressive episode or alcohol abuse according to ICD-10 diagnostic criteria.
The study was conducted in accordance with the Declaration of Helsinki 2000. The study was performed on the anonymized data of patients enrolled in the program. At inclusion, all patients signed an informed written consent form allowing for the anonymized use of their clinical data for research purposes. One hundred and two participants joining the multidisciplinary functional rehabilitation program were included in the present study. The program starts with a one-day individual evaluation that involved physical and psychological testing by senior health professionals, and the completion of a series of questionnaires. All the collected data were shared in a multidisciplinary meeting in order to set adapted, individualized goals for each patient.
Measures
Pain
Self-rated pain was assessed on a visual analogue scale of 0–10 cm, where “0” represented no pain and “10” represented the worst pain experienced. Duration of the current episode was defined according to patients’ medical record.
Disability
Disability was assessed using the Oswestry Disability Index (ODI).34,35 It is the most commonly condition-specific disability measure used in chronic low back pain. Its 10 self-rated items measure how back or leg pain affects the patient’s ability to manage everyday life. The total score ranges from 0 to 100: 0–20% indicate minimal disability, 20–40% moderate disability, 40–60% severe disability, 60–80% crippled state and 80–100% indicate patients who are bed-bound.
Personality Traits
The Revised Neuroticism-Extraversion-Openness Personality Inventory (NEO-PI R) is a 240-item questionnaire that has been extensively validated.36 It was developed to measure the five-factor model using rational and factor analytic methods on large samples of normal adult volunteers and is a comprehensive self-report instrument that operationalizes the five-factor model of personality.36,37 The questionnaire was previously validated in pain populations.25,38 Internationally recognized as a gold standard, the 240 items are rated on a 5-point agreement scale and grouped into five main personality dimensions (score range 0–192). Each domain is subdivided into six lower-order facets (score range 0–32).
Neuroticism contrasts emotional stability with negative emotionality, such as feeling anxious, nervous, or tense. Extraversion implies an energetic approach towards the social and material world and includes traits such as sociability, assertiveness, and positive emotionality. Openness to experience describes the breadth, depth, and originality of an individual’s mental and experiential life. Agreeableness includes traits such as altruism, tender-mindedness, and modesty. Finally, Conscientiousness refers to socially prescribed impulse control that facilitates task-directed behavior, such as thinking before acting, delaying gratification, and prioritizing tasks.
Fear-Avoidance
The Tampa Scale for Kinesiophobia (TSK) developed by Miller et al39 is a self-rated measure of fear of movement. Kinesiophobia is defined as an excessive, irrational and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or re-injury. The scale was validated and found to be responsive in chronic low back pain patients.40,41 Seventeen items are rated on a 4-point Likert scale ranging from “strongly disagree” to “strongly agree”. A total score is calculated with a range from 17 to 68, where higher scores indicate higher degrees of kinesiophobia.
Depressive and Anxious Moods
The Hospital Anxiety and Depression scale (HADS)42 is a self-rated scale and a reliable instrument for detecting states of depression and anxiety in the setting of a general hospital practice. The scale was validated in chronic low back pain patients.43 It is composed of 14 items each rated on a 4-point (0–3) response category with a total score of 0 to 21 for anxiety and 0 to 21 for depression. A score of 8 to 10 is suggestive of the presence of the respective mood, and a score of 11 or higher indicating probable presence of the mood disorder.
Sample Size Calculation
When comparing the CLBP population to the normal population, 44 patients are required to have a 90% chance of detecting, at 5% significance level, a difference in a personality type of 0.5 standard deviation. Since average personality scores differ between men and women, the total sample size required is 44 men and 44 women.
Statistics
One-sample t-test was used to compare sample means in the five personality domains and the French average population norms.44 Associations between the five personality domains and fear-avoidance (TSK), and anxiety and depression (HADS) were assessed using Pearson’s correlation, after checking for bivariate normality. Associations adjusted for gender, age, duration of current episode of low back pain and current pain intensity were estimated using linear regression. R squared were used as a measure of effect size. A specific focus was included on the six facets of the Neuroticism domain and their association with fear-avoidance, anxiety and depression. All calculations were implemented in R software. P values <0.05 were considered significant, without correction for multiple testing, since the focus of this study is more on the strength of the associations.
Results
The study sample (n =102) of chronic low back pain patients included slightly more men than women (57.8% male), with a mean age of 40.8±10.1. The average pain intensity was 5.7±2.9, and the average score on the ODI was 43.0±13.8 indicating severe disability. Socio-demographic characteristics and baseline scores are presented in Table 1. Scores of HADS indicated that the sample was in the borderline range for both anxiety and depression, with slightly higher scores on anxiety. The average score for kinesiophobia as assessed by the TSK was 43.1±7.6, which lies above the cut-off score of >37 for clinically significant fear of movement.
 |
Table 1 Characteristics of the Sample (n=102) |
Regarding personality traits, both men and women were found to have significantly lower average scores on the Openness to experience domain than the general population according to reference norms of the French NEO PI-R44 (105.0 vs 115.5 for men, and 108.7 vs 117.5 for women, p-values <0.01 for both men and women, as shown in Table 2). Both genders also had higher average Conscientiousness scores (124 vs 115.5 for men and 124.5 vs 116.5 for women, p-value <0.01 for both men and women), while only women in our sample had significantly higher Agreeableness scores than the general population (129.5 vs 124, p-value = 0.02).
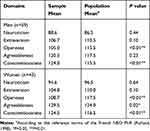 |
Table 2 Comparison of Population and Sample Mean Scores in Personality Domains |
As shown in Table 3, results of the correlation show that Neuroticism was positively associated with higher fear-avoidance, depression and anxiety, with anxiety showing the strongest association (correlation coefficient equals 0.21, 0.35 and 0.44, respectively). Interestingly, these results did not change after adjusting for age, gender, duration of current low back pain episode and pain level (0.25, 0.38 and 0.49, respectively). Extraversion and Openness domains showed weak negative correlation with depression scores (−0.25, −0.27), with Extraversion also inversely correlated with fear-avoidance, but only after adjustment with covariates (adjusted correlation coefficient equals −0.23). Conscientiousness showed weak negative correlation with depression and with anxiety after adjustment (−0.21, −0.21).
 |
Table 3 Association of Personality Domains with Fear-Avoidance, Anxiety and Depression (n=102) |
Analysis of the six facets of the Neuroticism domains revealed that all facets, except for Impulsiveness, showed moderate-to-strong positive correlations with depressive (correlation coefficient after adjustment: Anxiety 0.25, Anger hostility 0.27, Depression 0.42, Self-consciousness 0.32, and Vulnerability to stress 0.30) and anxious moods (Anxiety 0.56, Anger hostility 0.36, Depression 0.51, Self-consciousness 0.21 and Vulnerability to stress 0.31). Fear-avoidance weakly correlated with Anxiety, Anger Hostility and Depression facets (0.26, 0.23 and 0.28, respectively) (Table 4).
 |
Table 4 Association of Neuroticism Facets with Fear-Avoidance, Anxiety and Depression (n=102) |
Discussion
In the current study, disabled chronic low back pain patients showed characteristic personality features that deviated from the general population norms when assessed by the dimensional Five-Factor Model of personality. However, they did not reach maladaptive or clinically significant forms of personality disorders, confirming that chronic pain patients present with a underlying personality structure that is similar to non-pain-suffering individuals of the general population.38 This result confirms the need to assess personality, not only as a comorbid psychiatric disorder but rather as an individual vulnerability and resilience factor in multidisciplinary biopsychosocial rehabilitation programs for non-specific chronic low back pain patients.45 Proper assessment enables the individualization of treatment to build upon each patient’s psychological frame of mind to maximize the potential for effective functioning.
Previous evidence suggest that two typical distinguishing personality traits in chronic pain sufferers from the general population include high levels of harm avoidance and low levels of self-directedness.25 Low self-directedness often manifests as difficulty with defining and setting meaningful goals, low motivation, and problems with adaptive coping. In the present study, the personality profiles of chronic low back pain patients were indeed characterized by high levels of Conscientiousness and milder levels of Openness to experiences in both male and female patients. According to the Five-Factor Model of Costa and McCrae,15 low levels of Openness to experience indicate a lack of intellectual curiosity, imagination and preference for a variety of activities. These individuals prefer strict routines and experience difficulties adapting to the changes requested in their lives. In the context of chronic low back pain, such changes include working incapacity, inability to carry food purchase, impact on sexual life and marital dynamics. High levels of Conscientiousness reveal a tendency to be organized, disciplined and to prefer planned rather than spontaneous behavior.15 Our results confirm that chronic low back pain patients present with little capacity to regulate and adapt behavior to demands of a situation in order to achieve their goals and fail to adaptively cope with emerging difficulties.
Within the general chronic pain population, a high level of harm avoidance is also reported. This personality feature refers to a tendency to be fearful, pessimistic, sensitive to criticism, and requiring high levels of re-assurance.25 The Neuroticism dimension of the Five-Factor Model assesses the individuals’ tendency to experience negative emotions and interpret ordinary situations as threatening and minor frustrations as hopelessly difficult.15 Individuals with high Neuroticism are emotionally overwhelmed and at higher risk to develop common mood disorders such as depressive or anxious disorders. Contrary to previous evidence, the patients of the present study have not shown high levels of Neuroticism. This result might be explained by the fact that patients with clinically diagnosed major depression have been excluded from the present study sample. Indeed, Naylor and colleagues25 have previously highlighted that controlling for comorbid anxiety and depression in study samples may lead to different results, because of the overlap between depressive-anxious mood states and Neuroticism personality traits.
Besides the distinguished patterns of low Openness and high Conscientiousness, higher levels of Agreeableness emerged as a distinctive personality feature in the women subgroup. According to the Five-Factor Model, individuals with high Agreeableness levels are perceived as kind, cooperative, warm and considerate.15 In the general population, Agreeableness is higher in women.46 Results of our study suggest that this gender bias is even stronger in a clinical chronic low back pain population. Interestingly, this dimension showed no association neither with fear-avoidance nor depressive or anxious mood in pain patients, and seems indeed related to a gender bias rather than to psychological pain repercussions.
Regarding the association between personality traits and adjustment to chronic pain, we assessed the relationship between the five personality dimensions and patients’ level of fear-avoidance, depressive and anxious mood. Results show that Neuroticism is positively related to anxious and depressive mood, as well as fear-avoidance, even in our sample free of psychiatric diagnoses. Kadimpati and colleagues26 had previously indicated that Neuroticism is independently associated with greater pain catastrophizing above-and-beyond the contributions of sociodemographic characteristics, pain severity, and clinical depression. In the present sample, anxious and depressive moods were positively associated with five out of the six Neuroticism facets after adjusting for covariates. Patients seem capable to resist temptation and tolerate frustration, however what seems to be related to their emotional distress is the social intimidation and embarrassment as well as difficulties to remain calm under pressure. Neuroticism increases these processes, by leading to more catastrophic thoughts about pain and the production of more negative emotions.17 In our study, analysis of the six sub-facets of Neuroticism showed that fear-avoidance is significantly related to anxiety, anger and depression facets. Thus, high Neuroticism is indeed not per se a characteristic feature of chronic pain patients, but it is associated with the patients’ use of coping strategies to control and adjust to pain. On the other hand, Extraversion showed a reverse association with fear-avoidance and depressive moods. This association remained significant after adjusting for covariates. This finding coincides with the rare existing evidence relating Extraversion to positive pain-related beliefs.22 In the general population, Extraversion has been found to have a strong and direct effect on psychological well-being.47 In pain patients, positive personality traits, such as optimism and hope have a protective role towards pain and they show an inverse relationship with pain catastrophizing.48
With respect to Openness to experience, the present study confirmed that this dimension presents a reverse relationship with depressive mood, without relating to fear-avoidance. For the past 30 years, cognitive-behavioral models of pain have guided the development of psychologically based treatment approaches, and they stress the fact that patients with increased psychological flexibility, who are open and engaged, reach more positive outcomes because of their decentering and committed behavior.49 While the Neuroticism dimension seems to interact with patients’ cognitive processes, in contrast Openness to experience seems to relate to their emotional state. The dimension of Openness to experience surely deserves further attention and research in chronic pain patients. Interestingly, we also found no significant association between Conscientiousness and fear-avoidance, instead, this personality dimension was negatively related to anxious and depressive moods. In the current sample of patients, with high levels of Conscientiousness and low levels of Openness, they seem to accept a life with chronic pain without tendency of avoidant behavior; however, they express higher levels of anxious and depressive mood in their current condition. High Conscientiousness seems to intervene in emotional regulation rather than behavioral avoidance in pain patients.
Results of the current study show how personal determinants such as personality traits associate with pain avoidance, depressive and anxious mood in chronic low back pain patients. These results, therefore, have an important implication on the design of treatment programs for those patients. They underline the importance of incorporating a pre-treatment screening to identify those patients at risk of poor pain adjustment and subsequent disability and loss of quality of life, especially in intensive treatment programs for highly disabled population. This element appears to be neglected by many multidisciplinary treatment programs.50 Identifying these traits could help anticipating and better addressing psychopathological comorbidities that could interfere with the program success.51,52 It would provide important clues for therapists on how to individualize their approach even within a group program, for example in setting adapted realistic rehabilitation goals for each participant or when identifying personality features to encourage and endorse as facilitators to the success of the treatment. Finally, since Extraversion had an inverse association with fear-avoidance and depression, it would be plausible that programs be designed in a way that allows patients to interact within psychologically diverse groups, and thus benefit from treatment-based activities to expand their social networks and develop their social support.
The strengths of the current study include the utilization of a comprehensive assessment of all five dimensions of personality, rather than limiting the analysis to Neuroticism as in previous studies.22,26 Most importantly, the use of a dimensional and self-assessed approach of personality, fear-avoidance and mood, allowed for focusing on underlying psychological processes, rather than on comorbid psychiatric disorders according to diagnostic categories. An additional strength of the study is the carefully selected homogenous sample of a group of disabling chronic low back pain patients without psychiatric disorders. Those patients incur larger share of the social burden, and drive most of the costs related to low back pain management. Nevertheless, the study has some limitations. We did not include a control group from the general Swiss population to compare our sample’s personality to a non-clinical Swiss sample. We relied on the general population norms of the French NEO PI-R. However, mean differences in personality traits across countries and cultures are known to be about 8.5 times smaller than differences between any two individuals randomly selected from these samples.53 In addition, the cross-sectional design did not allow for exploring temporal relations, or effects of personality on treatment response.
Conclusions
The present study stresses the importance of considering chronic pain patients’ personality traits, in order to assess their individual differences regarding pain-related cognitive and affective distress. Chronic low back pain patients present lower Openness to experience and higher Conscientiousness in comparison to the general population norms. Four out of the five personality dimensions, except for Agreeableness, were significantly associated with patients’ depressive mood. We confirmed in the chronic low back pain population, the positive association between Neuroticism and depressive mood reported in other chronic pain populations. Extraversion, Openness to experience and Conscientiousness showed a reverse relationship with depressive mood.
These results also suggest that highly demanding treatments like intensive multidisciplinary treatment programs would gain from exploring personality traits as they could be important facilitators or barriers to the success of the program. Further research in the domain is warranted, particularly using a longitudinal design, to confirm these results and refine recommendations for clinicians.
Finally, Openness to experience and Conscientiousness are potential protective factors in chronic low back pain patients, again deserving assessment in future longitudinal studies. They could be promising determinants of patients’ psychological flexibility and degree of acceptance with respect to their chronic pain.
Ethics and Consent Statement
Tacit approval was given by the Cantonal Commission for Research Ethics (CCER) to this study as it was built from clinically collected data in the intent to improve quality of care and did not involve any therapeutic modification. All patients signed an informed consent form agreeing to the use their anonymized clinical data for research purposes.
Acknowledgments
A special thanks to Mrs Marlène Sartori for her help in data collection. We would also like to thank the patients for taking the time to fill the questionnaires.
Author Contributions
S.G. supervised the fieldwork and data acquisition and contributed to the conception and design of the study and data interpretation. K.W. contributed to the design of the study, and data analysis and interpretation. D.S.C contributed to the data analysis and interpretation M.E.I contributed to the design of the study, data analysis and interpretation. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was supported by a grant from Rheuma Search Foundation. Maha E. Ibrahim was supported by a postdoc Swiss Government Excellence Scholarship supplied by the Swiss Confederation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. doi:10.1016/S0140-6736(18)30480-X
2. Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. doi:10.1016/j.berh.2010.10.002
3. Costa L, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012;184(11):E613–E624.
4. Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2004;29(1):79–86. doi:10.1097/01.BRS.0000105527.13866.0F
5. Becker A, Held H, Redaelli M, et al. Low back pain in primary care: costs of care and prediction of future health care utilization. Spine. 2010;35(18):1714–1720. doi:10.1097/BRS.0b013e3181cd656f
6. Hasenbring M, Hallner D, Klasen B. Psychological mechanisms in the transition from acute to chronic pain: over-or underrated? Schmerz. 2001;15(6):442–447. doi:10.1007/s004820100030
7. Nordstoga AL, Nilsen TIL, Vasseljen O, Unsgaard-Tøndel M, Mork PJ. The influence of multisite pain and psychological comorbidity on prognosis of chronic low back pain: longitudinal data from the Norwegian HUNT Study. BMJ Open. 2017;7(5):e015312. doi:10.1136/bmjopen-2016-015312
8. Viniol A, Jegan N, Brugger M, et al. Even worse — risk factors and protective factors for transition from chronic localized low back pain to chronic widespread pain in general practice. Spine. 2015;40(15):E890–E899. doi:10.1097/BRS.0000000000000980
9. Thompson EL, Broadbent J, Bertino MD, Staiger PK. Do pain-related beliefs influence adherence to multidisciplinary rehabilitation?: A systematic review. Clin J Pain. 2016;32(2):164–178. doi:10.1097/AJP.0000000000000235
10. Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. 2019;53(9):554–559. doi:10.1136/bjsports-2017-098673
11. Westman A, Linton SJ, Öhrvik J, Wahlén P, Leppert J. Do psychosocial factors predict disability and health at a 3-year follow-up for patients with non-acute musculoskeletal pain? A validation of the Örebro Musculoskeletal pain screening questionnaire. Eur J Pain. 2008;12(5):641–649. doi:10.1016/j.ejpain.2007.10.007
12. Wettstein M, Eich W, Bieber C, Tesarz J. Profiles of subjective well-being in patients with chronic back pain: contrasting subjective and objective correlates. Pain Med. 2019;20(4):668–680.
13. Janowski K, Steuden S, Kuryłowicz J. Factors accounting for psychosocial functioning in patients with low back pain. Eur spine j. 2010;19(4):613–623. doi:10.1007/s00586-009-1151-1
14. Franklin ZC, Holmes PS, Smith NC, Fowler NE, Keil A. Personality type influences attentional bias in individuals with chronic back pain. PLoS One. 2016;11(1):e0147035. doi:10.1371/journal.pone.0147035
15. Costa PT
16. Hirschfeld RM, Klerman GL, Lavori P, Keller MB, Griffith P, Coryell W. Premorbid personality assessments of first onset of major depression. Arch Gen Psychiatry. 1989;46(4):345–350. doi:10.1001/archpsyc.1989.01810040051008
17. Wong WS, Lam HMJ, Chen P, et al. The fear-avoidance model of chronic pain: assessing the role of neuroticism and negative affect in pain catastrophizing using structural equation modeling. Int J Behav Med. 2015;22(1):118–131. doi:10.1007/s12529-014-9413-7
18. Vlaeyen JW, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. 2016;157(8):1588–1589. doi:10.1097/j.pain.0000000000000574
19. Poppe C, Crombez G, Devulder J, Hanoulle I, Vogelaers D, Petrovic M. Personality traits in chronic pain patients are associated with low acceptance and catastrophizing about pain. Acta Clin Belg. 2011;66(3):209–215. doi:10.2143/ACB.66.3.2062549
20. Semeru GM, Halim MS. Acceptance versus catastrophizing in predicting quality of life in patients with chronic low back pain. Korean J Pain. 2019;32(1):22. doi:10.3344/kjp.2019.32.1.22
21. Dersh J, Polatin PB, Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med. 2002;64(5):773–786. doi:10.1097/01.psy.0000024232.11538.54
22. Goubert L, Crombez G, Van Damme S. The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: a structural equations approach. Pain. 2004;107(3):234–241. doi:10.1016/j.pain.2003.11.005
23. Clark JR, Nijs J, Yeowell G, Holmes P, Goodwin PC. Trait sensitivity, anxiety and personality are predictive of central sensitisation symptoms in patients with chronic low back pain. Pain Pract. 2019;19(8):800–810. doi:10.1111/papr.12809
24. Asghari A, Nicholas MK. Personality and pain-related beliefs/coping strategies: a prospective study. Clin J Pain. 2006;22(1):10–18. doi:10.1097/01.ajp.0000146218.31780.0b
25. Naylor B, Boag S, Gustin SM. New evidence for a pain personality? A critical review of the last 120 years of pain and personality. Scand J Pain. 2017;17(1):58–67. doi:10.1016/j.sjpain.2017.07.011
26. Kadimpati S, Zale EL, Hooten MW, Ditre JW, Warner DO, Eldabe S. Associations between neuroticism and depression in relation to catastrophizing and pain-related anxiety in chronic pain patients. PLoS One. 2015;10(4):e0126351. doi:10.1371/journal.pone.0126351
27. BenDebba M, Torgerson WS, Long DM. Personality traits, pain duration and severity, functional impairment, and psychological distress in patients with persistent low back pain. Pain. 1997;72(1–2):115–125. doi:10.1016/S0304-3959(97)00020-1
28. Conrad R, Wegener I, Geiser F, Kleiman A. Temperament, character, and personality disorders in chronic pain. Curr Pain Headache Rep. 2013;17(3):318. doi:10.1007/s11916-012-0318-3
29. Krueger RF, Caspi A, Moffitt TE, Silva PA, McGee R. Personality traits are differentially linked to mental disorders: a multitrait-multidiagnosis study of an adolescent birth cohort. J Abnorm Psychol. 1996;105(3):299. doi:10.1037/0021-843X.105.3.299
30. Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 2010;136(5):768. doi:10.1037/a0020327
31. Paulus DJ, Vanwoerden S, Norton PJ, Sharp C. From neuroticism to anxiety: examining unique contributions of three transdiagnostic vulnerability factors. Pers Individ Dif. 2016;94:38–43. doi:10.1016/j.paid.2016.01.012
32. Steiner A-S, Sartori M, Leal S, et al. Added value of an intensive multidisciplinary functional rehabilitation programme for chronic low back pain patients. Swiss Med Wkly. 2013;143:453.
33. Kupper DGJ, Rentsch D, Barthassat V, Cedraschi C, Genevay S. Programmes multidisciplinaires et lombalgies chroniques: concepts et aspects pratiques: première partie: concepts et développement. [Multidisciplinary programs and chronic low back pain: concepts and practical aspects.1: concepts and Development]. Kinésithérapie la revue. 2010;10(102):35–39. doi:10.1016/S1779-0123(10)74858-0
34. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273.
35. Vogler D, Paillex R, Norberg M, Cabri J Cross-cultural validation of the Oswestry disability index in French.
36. Costa PT
37. Xu J, Potenza MN. White matter integrity and five-factor personality measures in healthy adults. Neuroimage. 2012;59(1):800–807. doi:10.1016/j.neuroimage.2011.07.040
38. Wade JB, Dougherty LM, Hart RP, Cook DB. Patterns of normal personality structure among chronic pain patients. Pain. 1992;48(1):37–43. doi:10.1016/0304-3959(92)90129-Y
39. Miller RPKS, Todd DD. Tampa scale. Unpublished report. 1991.
40. Goubert L, Crombez G, Van Damme S, Vlaeyen JW, Bijttebier P, Roelofs J. Confirmatory factor analysis of the tampa scale for Kinesiophobia: invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain. 2004;20(2):103–110. doi:10.1097/00002508-200403000-00007
41. Roelofs J, Goubert L, Peters ML, Vlaeyen JW, Crombez G. The tampa scale for kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain. 2004;8(5):495–502. doi:10.1016/j.ejpain.2003.11.016
42. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
43. Herrmann C. International experiences with the hospital anxiety and depression scale-a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi:10.1016/S0022-3999(96)00216-4
44. Rolland J. Manuel De L’inventaire NEO-PI-R (Adaptation Française)[Manual of the NEO-PI-R, French Adaptation]. Paris: ECPA; 1998.
45. Kamper SJ, Apeldoorn A, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ. 2015;350(feb18 5):h444. doi:10.1136/bmj.h444
46. Costa PT
47. Lu L, Shih J. Personality and happiness: is mental health a mediator? Pers Individ Dif. 1997;22(2):249–256. doi:10.1016/S0191-8869(96)00187-0
48. Pulvers K, Hood A. The role of positive traits and pain catastrophizing in pain perception. Curr Pain Headache Rep. 2013;17(5):330. doi:10.1007/s11916-013-0330-2
49. McCracken LM, Morley S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J Pain. 2014;15(3):221–234. doi:10.1016/j.jpain.2013.10.014
50. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147–152. doi:10.1007/s11916-012-0252-4
51. Gatchel RJ, Haggard R, Thomas C, Howard KJ. Biopsychosocial approaches to understanding chronic pain and disability. In: Moore RJ, Editor. Handbook of Pain and Palliative Care. Cham: Springer; 2018:3–22.
52. George SZ, Beneciuk JM. Psychological predictors of recovery from low back pain: a prospective study. BMC Musculoskelet Disord. 2015;16(1):49. doi:10.1186/s12891-015-0509-2
53. Allik J, Church AT, Ortiz FA, et al. Mean profiles of the NEO personality inventory. J Cross Cult Psychol. 2017;48(3):402–420. doi:10.1177/0022022117692100
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
