Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Association of HbA1c Variability with Vibrating Perception Threshold in Middle-Aged and Elderly Patients with Type 2 Diabetes Mellitus: A Retrospective Cohort Study
Authors Ding J, Shi Q, Dong L, Su H, Du Y, Pan T, Zhong X
Received 23 October 2023
Accepted for publication 7 January 2024
Published 10 January 2024 Volume 2024:17 Pages 193—202
DOI https://doi.org/10.2147/DMSO.S443917
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Jingcheng Ding,1,* Qian Shi,1,* Ling Dong,2 Hong Su,3 Yijun Du,1 Tianrong Pan,1 Xing Zhong1
1Department of Endocrinology, The Second Affiliated Hospital of Anhui Medical University, Hefei City, Anhui Province, 230601, People’s Republic of China; 2Department of Anesthesiology and Perioperative Medicine, The Second Affiliated Hospital of Anhui Medical University, Hefei City, Anhui Province, 230601, People’s Republic of China; 3Department of Epidemiology and Health Statistics, Anhui Medical University, Hefei City, Anhui Province, 230601, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xing Zhong, Department of Endocrinology, The Second Affiliated Hospital of Anhui Medical University, No. 678 Furong Road, Hefei City, Anhui province, People’s Republic of China, Tel +86 18905692292, Email [email protected]
Purpose: To investigate the relationship between HbA1c variability and vibrating perception threshold (VPT) in middle-aged and elderly patients with type 2 diabetes mellitus (T2DM).
Patients and Methods: A total of 367 middle-aged and elderly patients with T2DM were enrolled. All patients were categorized into the control and vibration sensation deficiency group (VSD) based on VPT. Clinical data were collected. The coefficient of variation of glycated hemoglobin A1c (HbA1c-CV) and the mean glycated hemoglobin A1c(HbA1c-Mean) are considered as indexes of HbA1c variability. Multivariate logistic regression analysis, the generalized linear model and ROC curve correlation analysis were used to analyze the correlation of various factors and VPT.
Results: The multivariate logistic regression analysis revealed that age, systolic blood pressure (SBP), and HbA1c-CV were identified as risk factors for vibration sensation deficiency in middle-aged and elderly patients with T2DM, while estimated glomerular filtration rate (eGFR), triiodothyronine (T3), and alanine aminotransferase (ALT) were considered as protective factors. In the unadjusted generalized linear model, a significant association was observed between HbA1c-CV and VPT values. After adjusting for age, diabetic duration, SBP, homeostatic model assessment for beta-cell function (HOMA-β), ALT, eGFR, T3, 24-hour urinary protein excretion levels, and HbA1c-Mean, HbA1c-CV remained significantly correlated with VPT values on both sides. (left side, B=2.560, 95% CI 1.298~3.823; P< 0.001; right side, B=2.608, 95% CI 1.498~3.718, P< 0.001). The area under the curve (AUC) for HbA1c-CV and VSD prevalence was 0.723, with a sensitivity of 79.85%, specificity of 56.22%.
Conclusion: The risk of developing VSD increases proportionally with higher HbA1c-CV levels in middle-aged and elderly patients with T2DM. Reaching and maintaining blood glucose stability is essential to the mitigation of diabetes peripheral neuropathy occurrence.
Keywords: type 2 diabetes mellitus, HbA1c variability, vibrating perception threshold, diabetic peripheral neuropathy
Introduction
The prevalence rate of type 2 diabetes mellitus (T2DM) among adults in China is as high as 12.8%,1 establishing it as the country with the highest diabetic population globally. The prevalence of diabetic peripheral neuropathy (DPN)2 is remarkably high among individuals with diabetes mellitus, making it one of the most prevalent complications associated with this metabolic disorder. Due to the insidious onset and slow progression of DPN, clinical symptoms often manifest when irreversible pathological changes have already occurred in most peripheral nerves, thereby predisposing individuals to foot ulcers and an elevated risk of amputation. According to the Standards of Medical Care in Diabetes published by the American Diabetes Association (ADA), the prevalence of DPN is reported to be 13.1%.3 DPN significantly impacting the overall quality of life for individuals with diabetes mellitus.
Currently, the screening methods commonly employed for DPN encompass vibration sensory threshold detection, temperature threshold detection, pressure threshold detection, and ankle reflex detection and so on. The Vibrating Perception Threshold (VPT) detection4 is primarily employed for assessing lesions in vibrating perception, and reflecting the functionality of large fiber. Due to its non-invasive nature, high accuracy, and convenient usability, VPT has emerged as a primary modality for clinical diagnosis and evaluation of diabetic peripheral neuropathy both domestically and internationally. Ponirakis et al5 conducted a comprehensive assessment of the neurological function in 144 subjects, revealing that VPT exhibited the strongest correlation with sensory nerve conduction velocity and diagnostic accuracy.
In addition to glycemic control, it is imperative not to overlook the impact of blood glucose variability on the incidence and progression of chronic complications associated with diabetes mellitus. Blood glucose variability,6 also referred to as glycemic fluctuations, encompasses both short-term and long-term variations in blood glucose levels. Short-term fluctuations in blood sugar levels reflect daily and/or intraday variations, whereas long-term fluctuations are typically determined by multiple measurements of glycated hemoglobin A1c(HbA1c) or fasting plasma glucose(FPG) over an extended period, indicating changes in blood sugar levels over months to years. The findings of a prospective study7 revealed that, even among patients with type 2 diabetes mellitus who maintained well-controlled HbA1c levels (HbA1c<7%), the mean amplitude of glycemic excursions (MAGE) continued to be an independent risk factor for DPN. However, the existing literature predominantly focuses on the association between continuous dynamic glucose monitoring systems and diabetic peripheral neuropathy, with limited investigations into long-term HbA1c variability.
The latest epidemiological survey1 reveals that the prevalence of diabetes mellitus among the elderly population in China is 30%, significantly exceeding the average incidence rate observed in the general population, thereby establishing this demographic as a prominent group affected by diabetes mellitus. Middle-aged and elderly patients with type 2 diabetes mellitus (T2DM) typically exhibit characteristics such as a prolonged disease duration, progressive renal function decline, impaired islet function, etc., which collectively contribute to the challenge of achieving optimal blood glucose control and significantly elevate the risk of complications compared to younger individuals. This retrospective study aims to investigate the association between HbA1c variability and vibration perception threshold values in middle-aged and elderly patients with type 2 diabetes mellitus, providing crucial clinical evidence for the prevention and treatment of diabetic peripheral neuropathy.
Participants and Methods
Participants
This retrospective study enrolled 367 middle-aged and elderly patients with type 2 diabetes mellitus (T2DM) who received regular visits at the Second Affiliated Hospital of Anhui Medical University from January 2021 to August 2023. Inclusion criteria: (1) Type 2 diabetes mellitus diagnosed based on the statement of the American Diabetes Association (ADA) in 2011;8 (2) Age exceeding 45 years; (3) A minimum of three HbA1c tests were conducted prior to the investigation. Exclusion criteria: (1) Peripheral neuropathy caused by factors other than T2DM (eg trauma, medication-induced, vitamin B deficiency); (2) Acute and chronic severe complications of diabetes mellitus (eg DKA, HHS, diabetic foot); (3) Concurrent presence of significant systemic diseases (eg, heart failure, liver dysfunction, renal insufficiency).
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Anhui Medical University (Ethics number: YX2022-043). Human research was registered at the Chinese Clinical Trial Registry (registered 23 December 2022), chictr.org.cn (ChiCTR2200067020). All participants voluntarily consented to take part in the study and provided written informed consent. This study adhered to the standards of the International Committee on Harmonization of Good Clinical Practice and the revised version of the Declaration of Helsinki.
Data Collection
Demographic variables such as age, gender, exercise habits, smoking and alcohol history were collected. The height, weight, systolic blood pressure (SBP), and diastolic blood pressure (DBP) of the study participants were measured, and their body mass index (BMI) was calculated. Blood tests were carried out after an overnight fasting for glucose, glycosylated hemoglobin A1c (HbA1c), alanine aminotransferase (ALT), aspartate aminotransferase (AST), total cholesterol (TC), triglycerides (TG), creatinine, 24-hour urinary protein excretion, urine albumin-to-creatinine ratio (UACR), triiodothyronine (T3), thyroxine (T4), thyroid-stimulating hormone (TSH) and other relevant parameters. All data were collected during the last HbA1c test.
HbA1c Variability
In this study, the HbA1c-CV and HbA1c-Mean are considered as indexes of HbA1c variability. HbA1c values were also obtained from the hospital system during previous follow-up visits. The coefficient of variation of glycated hemoglobin A1c (HbA1c-CV) and the mean glycated hemoglobin A1c (HbA1c-Mean) were computed based on the recorded HbA1c values provided by the patients, where the coefficient of variation was determined as the ratio between the mean and standard deviation.
Vibration Perception Threshold (VPT) Assessment
During the last HbA1c test, the VPT using a vibratory sensory analysis device (Sensiometer A200, Beijing Blue news times technology Co. LTD) was measured: the first toe and dorsal of both left and right feet were detected respectively. The vibration intensity and amplitude were gradually increased until they reached a level that could be perceived by the individuals, and the corresponding vibration values were recorded (ranging from 0 to 50 V with an accuracy of 0.1). Each position was measured three times consecutively, and the average of these measurements was considered as the final result.
The findings of previous studies9 have demonstrated a significant correlation between VPT levels exceeding 25V and an increased cumulative risk of neuropathic foot ulcers. Therefore, for the purpose of this study, diabetes mellitus combined with vibration sensation deficiency was defined as the presence of VPT levels higher than 25V on at least one side of the foot.
Other Clinical Indicators Assessment
The Homeostasis Model Assessment of Beta-cell function index (HOMA-β) and the Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) were evaluated using the homeostasis model assessment, which is based on paired measurements of fasting plasma glucose and fasting C-peptide (HOMA2 v2.2.3; Homacalculator/https://www.dtu.ox.ac.uk/). Calculation of body surface area (BSA) in patients was performed using the DuBois formula:10 0.007184×weight (kg)0.425×height(cm)0.725. The estimation of creatinine clearance rate (Ccr) was determined using the Cockcroft-Gauh (CG) formula:11 eCcr for  ; eCcr for
; eCcr for  . According to gender differences, glomerular filtration rate (GFR) calculated by the Cockcroft-Gauh formula was normalized by BSA:
. According to gender differences, glomerular filtration rate (GFR) calculated by the Cockcroft-Gauh formula was normalized by BSA:  . It is important to note that blood creatinine values in this equation are expressed in mg/dl, and 1μmol/l=0.0113mg/dl.
. It is important to note that blood creatinine values in this equation are expressed in mg/dl, and 1μmol/l=0.0113mg/dl.
Statistical Analysis
All statistical analyzes using SPSS Ver. 26.0 software. Comparisons between groups were made using t-test for normally distributed variables, the Mann–Whitney U-test for asymmetrically distributed variables, and Chi-Square test for categorical variables. Variables with statistical differences were entered into a multivariate logistic regression analysis model to determine their net effects on vibration sensation deficiency. The generalized linear regression model was employed to further ascertain the independent association of HbA1c-CV with vibration value. The subjects’ working characteristic curves (ROCs) were mapped using R software (V4.3.1) and the area under the ROC curve was calculated (AUC) using MedCalc Software version 20.100 (https://www.medcalc.org/). A two-sided P-value < 0.05 was considered to indicate statistical significance.
Results
Clinical Characteristics of the Study Population
The participants’ clinical characteristics are summarized in Table 1. A total of 367 middle-aged and elderly patients diagnosed with type 2 diabetes mellitus were included in this study, and they were categorized based on the presence or absence of vibration sensation deficiency. The control group consisted of 149 male and 84 female participants, while the vibration sensation deficiency group (VSD) comprised 90 males and 44 females. The median follow-up duration for both groups was 15 months. Compared to the control group, the VSD group exhibited significant increases in age, duration of diabetes, SBP, HbA1c-Mean, HbA1c-CV, 24h urinary protein levels, and VPT values (P<0.05). Moreover, there were significant decreases in HOMA-β, ALT, eGFR and T3 levels (P<0.05).
 |
Table 1 Characteristics of the Study Cohort |
Multivariate Logistic Regression Analysis of T2DM Combined with VSD
The multivariate logistic regression analysis revealed that age, SBP, and HbA1c-CV were identified as risk factors for vibration sensation deficiency in middle-aged and elderly patients with type 2 diabetes mellitus. Conversely, eGFR, ALT, and T3 were found to be protective factors (Table 2).
 |
Table 2 Multivariate Logistic Regression Analysis of T2DM Patients with VSD-Related Influencing Factors |
Correlation Between HbA1c-CV and VPT Values
In order to further elucidate the relationship between HbA1c-CV and VPT values on both sides, the generalized linear regression analysis was conducted with VPT values as dependent variables. In the unadjusted analyses, a significant association was observed between HbA1c-CV and both left and right VPT values. After adjusting for age, duration of diabetes, SBP, HOMA-β, ALT, eGFR, T3, 24-hour urinary protein excretion levels, and HbA1c-Mean, HbA1c-CV remained significantly correlated with VPT values on both the left and right sides. (left side, B=2.560, 95% CI 1.298~3.823; P<0.001; right side, B=2.608, 95% CI 1.498~3.718, P<0.001)(Table 3).
 |
Table 3 Generalized Linear Regression Analysis of HbA1c-CV and the Left and Right VPT Values in Middle-Aged and Elderly Patients with Type 2 Diabetes Mellitus |
ROC Curve Analysis for HbA1c-CV and VSD Prevalence
The area under the curve (AUC) for HbA1c-CV and VSD prevalence was 0.723(95% CI [0.674~0.768], P<0.001), the sensitivity was 79.85%, the specificity was 56.22%, and the best diagnostic value was 0.08 (Figure 1).
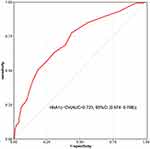 |
Figure 1 ROC curve analysis for HbA1c-CV and VSD prevalence. Abbreviation: VSD, vibration sensation deficiency. |
Discussion
This study aimed to investigate the association between HbA1c variability and other influencing factors with vibration sensation deficiency in middle-aged and elderly patients diagnosed with type 2 diabetes mellitus. The assessment of HbA1c variability was conducted using HbA1c-CV and HbA1c-Mean. The findings revealed a positive correlation between increased HbA1c-CV variability and elevated VPT levels, thereby indicating a significantly heightened risk of peripheral neuropathy. However, no statistically significant correlation was observed between HbA1c-Mean and peripheral neuropathy. Furthermore, age and SBP are recognized as risk factors for vibration sensation deficiency in middle-aged and elderly individuals with type 2 diabetes mellitus, while ALT, eGFR, and T3 may exert a protective effect.
Diabetic peripheral neuropathy (DPN), being the most prevalent complication of diabetes mellitus, stands as the primary cause of neuropathy on a global scale.12 It can be divided into large fiber neuropathy, small fiber neuropathy or mixed neuropathy. The predominant manifestation of diabetic peripheral neuropathy is characterized by progressive paresthesia, which gradually extends from the peripheral extremities to the central regions, exhibiting a gloves or socks distribution pattern. In severe cases, patients may experience intense pain, muscle weakness and atrophy, along with diminished tendon reflexes. The vibration sensory threshold detection (VPT), as a standardized and quantified method for assessing nerve function, reflecting the functionality of large fiber. Dominguez-Munoz et al13 conducted repeated assessments of the vibration sensory threshold in individuals with type 2 diabetes mellitus, considering variations in gender and BMI. Their findings demonstrate robust reliability and stability in the VPT. The studies14–16 have shown that using VPT to diagnose DPN has high sensitivity and specificity. McIllhatton et al17 demonstrated that VPT can be recommended as a valuable assessment tool for diabetic peripheral neuropathy.
Healthy individuals exhibit normal islet secretion function and maintain a stable blood glucose fluctuation curve throughout the day. Conversely, in patients with type 2 diabetes mellitus resulting from either islet failure or insulin resistance, alterations in the internal glycemic environment not only lead to a significant increase in average blood glucose levels but also amplify the amplitude of blood glucose fluctuations. Notably, even among diabetics with similar HbA1c levels, there can be substantial variations in the magnitude of blood sugar fluctuations. Continuous glucose monitoring (CGM), as an emerging method for blood glucose monitoring, offers uninterrupted, comprehensive, and reliable information on daily glycemic levels. Consequently, it has gained widespread adoption in the clinical diagnosis and treatment of individuals with diabetes mellitus. Hu et al18 discovered that glycaemic variability assessed by MAGE is a independent risk factor for diabetic peripheral neuropathy, with an optimal cut-off value of 4.60 mmol/l, exhibiting a sensitivity of 64.47% and specificity of 75.54%. The study19 showed that Time in range (TIR) was significantly correlated with the prevalence of painful diabetic neuropathy. However, continuous glucose monitoring systems solely capture hyperglycemia or hypoglycemia episodes over a span of several days, whereas HbA1c variability serves as an indicator of glycemic trends and may offer a more comprehensive assessment of diabetes-related risk. Therefore, in the process of diagnosis and treatment, it is imperative to consider both short-term and glycemic fluctuations management. In this study, HbA1c-CV and HbA1c-Mean were employed as measures to assess the HbA1c variability in middle-aged and elderly patients with type 2 diabetes mellitus, thereby providing a more accurate reflection of blood glucose fluctuations. It was found that the HbA1c-CV and HbA1c-Mean of patients in VSD group were significantly higher than those in the control group, and multivariate logistic regression analysis showed that HbA1c-CV was a risk factor for the development of vibration sensation deficiency. The results of further generalized linear regression analysis revealed a significant association between HbA1c-CV and both left and right VPT values, even without adjusting for confounding factors. Moreover, this correlation remained statistically significant after controlling for relevant risk factors. (left side, B=2.560, 95% CI 1.298~3.823; P<0.001; right side, B=2.608, 95% CI 1.498~3.718, P<0.001). There was no statistically significant difference observed in the HbA1c-Mean values as determined by multivariate logistic regression analysis. Therefore, HbA1c-CV may serve as a significant risk factor for diabetes mellitus in conjunction with vibration sensation deficiency, whereas HbA1c-Mean does not exhibit the same association. The underlying mechanism through which blood glucose fluctuations contribute to the development of peripheral neuropathy in diabetes patients remains elusive. Animal studies20 have shown that blood glucose fluctuation can exacerbate oxidative stress and inflammatory response by up-regulating the expression of inflammatory regulatory factors and intercellular adhesion molecule-1 gene, which are considered to be important pathways of neurological dysfunction and apoptosis.21 Quagliaro et al22 found that exposure of endothelial cells to fluctuating hyperglycemia results in an upregulation of apoptosis through the activation of PKC-dependent NAD(P)H oxidase.
Through multivariate regression analysis, we identified age as a potential risk factor for diabetes individuals with vibration sensation deficiency. (OR=1.066, 95% CI 1.024~1.108, P=0.002). The prevalence of peripheral neuropathy in patients with type 1 diabetes mellitus has been observed to increase with age according to epidemiological studies,23 ranging from 18% among individuals aged 18–29 years to 58% among those aged 30 and above. In the ACCORD trial,24 the incidence of peripheral neuropathy in adults with type 2 diabetes mellitus was reported to be 42%. The incidence of peripheral neuropathy may gradually increase as diabetes individuals age. Moreover, the prevalence of diabetic peripheral neuropathy varies across different countries and regions. Pop-Busui et al2 reported a 28% incidence of diabetic peripheral neuropathy in the United States, while the corresponding San Luis Valley cohort study25 documented a slightly lower incidence rate of 25.8% for peripheral neuropathy. A cross-sectional study conducted in Beijing, China26 revealed that peripheral neuropathy was present in 23.5% of individuals diagnosed with type 2 diabetes mellitus. The prevalence of type 2 diabetic peripheral neuropathy in the middle-aged and elderly population was found to be 35.6% in this study, which is significantly higher compared to previous research findings. This discrepancy may be attributed to variations in the age range or assessment methodologies employed within the studied population.
The patients enrolled in this study exhibited glomerular filtration rates at stage 3 or higher (eGFR>30 mL/min/1.73m2). The multivariate logistic regression analysis revealed that maintaining a high estimated glomerular filtration rate (eGFR) could potentially serve as a protective factor for vibration sensation in middle-aged and elderly patients with type 2 diabetes mellitus. (OR=0.983, 95% CI 0.969~0.998, P=0.022). Similar to previous findings,27 it was also shown that the prevalence and severity of peripheral neuropathy would increase with the deterioration of renal function. Peripheral neuropathy is more likely to occur in patients with severe renal insufficiency or uremia due to metabolic disorders, acid-base imbalance, toxin accumulation, and other factors.28 The prospective studies29 demonstrated that elderly patients with chronic kidney disease had a 2.3-fold higher risk of motor nerve conduction velocity impairment compared to non-CKD subjects. In recent years, Moorthi et al30 have discovered a significant association between renal function and peripheral neuropathy in middle-aged and elderly diabetic patients, even during the early stages of renal decline. Hence, it is suggested that there exists a substantial correlation between renal function status and diabetic peripheral neuropathy.
In middle-aged and elderly patients with type 2 diabetes mellitus, the majority exhibit concomitant blood lipid deposition and arterial wall sclerosis, leading to an elevation in systolic blood pressure and pulse pressure difference. The results of animal experiments31 have demonstrated that hypertension can expedite the pathogenesis of peripheral neuropathy in ZDF rats, primarily characterized by a reduction in nerve myelin thickness. In order to ascertain the specific blood pressure index that contributes to neuropathy, Jarmuzewska et al32 conducted a cross-sectional survey on a limited sample size, revealing significant correlations between systolic blood pressure (SBP), pulse pressure difference (PP), and nerve function. Similar to the above results, after adjusting for potential confounders such as age and medical history, a positive correlation was observed between systolic blood pressure (SBP) and the occurrence of VSD (OR=1.018, 95% CI 1.000–1.037, P=0.048). These results suggest that SBP may serve as one of the risk factors for peripheral neuropathy in middle-aged and elderly patients with type 2 diabetes mellitus.
The thyroid hormone, synthesized and secreted by the thyroid follicular epithelial cells, exerts regulatory effects on human body metabolism. Several studies33,34 have demonstrated that thyroid hormone secretion disorder is associated with an increased likelihood of developing metabolic syndrome and significantly elevates the risk of complications related to diabetes mellitus. Lin et al35 demonstrated a negative correlation between FT3 levels and the prevalence of diabetic peripheral neuropathy, as well as an increased risk of DPN in patients with elevated FT4 levels. He et al36 found that the presence of low T3 syndrome in diabetic patients can lead to severe glucose toxicity and nerve fiber damage, thereby significantly elevating the risk of diabetic peripheral neuropathy (DPN). The findings of this study suggest that T3 may serve as a protective factor for vibration perception in middle-aged and elderly patients with T2DM (OR=0.285, 95% CI 0.111~0.738, P=0.010). Consequently, there exists an association between T3 levels and diabetic neuropathy.
This study suggests that the presence of alanine aminotransferase (ALT) may confer a protective effect on vibration perception (OR=0.968, 95% CI 0.943~0.995, P=0.020). Reiterating the findings of Mohsen et al,37 their study indicated a negative correlation between markers of liver injury (such as elevated ALT, fatty liver or fatty liver combined with elevated ALT) and diabetic peripheral neuropathy. However, inconsistent research findings have also been reported. For instance, Huang et al38 observed a significant increase in the prevalence of diabetic peripheral neuropathy among individuals with type 2 diabetes mellitus (T2DM) and non-alcoholic liver disease (NAFLD). Mantovani et al39 also reported a significantly higher incidence of distal symmetric polyneuropathy in patients with non-alcoholic liver disease (NAFLD) compared to those without NAFLD. The disparities observed in the aforementioned study findings may be attributed to variations in the racial composition, age distribution, and duration of diabetes among the enrolled patients.
Limitations
However, it is important to acknowledge the limitations of this study. Firstly, it employed a retrospective design with a small sample size at a single center, thereby restricting the statistical power of the analysis. Moreover, the age range of participants was limited to individuals aged over 45 years, leaving the relationship between glycemic variability and vibration sensory threshold (VPT) in other age groups uncertain. We intend to gradually address these inquiries in future investigations.
Conclusions
This study shows an association between HbA1c variability and vibration sensation in middle-aged and elderly patients with type 2 diabetes mellitus. Specifically, a higher risk of vibration sensation deficiency is observed in individuals with greater HbA1c-CV values within this patient population. Furthermore, age and SBP are identified as risk factors for vibration sensation deficiency in T2DM patients, while ALT, eGFR, and T3 serve as protective factors. Therefore, effective management of blood glucose levels in middle-aged and elderly patients with T2DM should aim to minimize fluctuations, which can contribute to the mitigation of diabetes peripheral neuropathy occurrence.
Acknowledgments
We would like to express our heartfelt gratitude to all the staff of the Department of Endocrinology, the Second Affiliated Hospital of Anhui Medical University, Department of Anesthesiology and Perioperative Medicine, the Second Affiliated Hospital of Anhui Medical University and Department of Epidemiology and Health Statistics, Anhui Medical University for their selfless help and valuable assistance.
Funding
This work was supported by the Clinical Research Incubation Program of the Second Affiliated Hospital of Anhui Medical University (2021LCZD14), Anhui Medical University Scientific Research Fund Project (2020xkj200), Natural Science Research Project of Universities in Anhui Province (2023AH053182), Endocrinology-Epidemiology and Biostatistic Co-Construction Project of Anhui Medical University (2021lcxk024).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020:m997. doi:10.1136/bmj.m997
2. Pop-Busui R, Boulton AJ, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–154. doi:10.2337/dc16-2042
3. American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S13–S27. doi:10.2337/dc18-S002
4. Jung J, Kim MG, Kang YJ, et al. Vibration perception threshold and related factors for balance assessment in patients with type 2 diabetes mellitus. Int J Environ Res Public Health. 2021;18(11):6046. doi:10.3390/ijerph18116046
5. Ponirakis G, Odriozola MN, Odriozola S, et al. NerveCheck for the detection of sensory loss and neuropathic pain in diabetes. Diabetes Technol Ther. 2016;18(12):800–805. doi:10.1089/dia.2016.0279
6. Skrha J, Soupal J, Skrha JJ, et al. Glucose variability, HbA1c and microvascular complications. Rev Endocr Metab Disord. 2016;17(1):103–110. doi:10.1007/s11154-016-9347-2
7. Xu F, Zhao LH, Su JB, et al. The relationship between glycemic variability and diabetic peripheral neuropathy in type 2 diabetes with well-controlled HbA1c. Diabetol Metab Syndr. 2014;6(1):139. doi:10.1186/1758-5996-6-139
8. American Diabetes Association. Diagnosis and classifcation of diabetes mellitus. Diabetes Care. 2011;34(Suppl 1):S62–S69. doi:10.2337/dc11-S062
9. Young MJ, Breddy JL, Veves A, et al. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds: a prospective study. Diabetes Care. 1994;17(6):557–560. doi:10.2337/diacare.17.6.557
10. Si H, Lei Z, Han C, et al. Evaluation of body surface area formulae for scaling GFR of adult renal patients: more between-subject variability explained by the DuBois & DuBois formula. Q J Nucl Med Mol Imaging. 2018;62(2):185–189. doi:10.23736/S1824-4785.16.02714-X
11. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. doi:10.1159/000180580
12. Iqbal Z, Azmi S, Yadav R, et al. Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018;40(6):828–849. doi:10.1016/j.clinthera.2018.04.001
13. Dominguez-Munoz FJ, Adsuar JC, Villafaina S, et al. Test-retest reliability of vibration perception threshold test in people with type 2 diabetes mellitus. Int J Environ Res Public Health. 2020;17(5):1. doi:10.3390/ijerph17051773
14. Brown JJ, Pribesh SL, Baskette KG, et al. A comparison of screening tools for the early detection of peripheral neuropathy in adults with and without type 2 diabetes. J Diabetes Res. 2017;2017:1467213. doi:10.1155/2017/1467213
15. Santos T, Melo JV, Leite NC, et al. Usefulness of the vibration perception thresholds measurement as a diagnostic method for diabetic peripheral neuropathy: results from the Rio de Janeiro type 2 diabetes cohort study. J Diabetes Complications. 2018;32(8):770–776. doi:10.1016/j.jdiacomp.2018.05.010
16. Willits I, Cole H, Jones R, et al. ViibraTip for testing vibration perception to detect diabetic peripheral neuropathy: a NICE medical technology guidance. Appl Health Econ Health Policy. 2015;13(4):315–324. doi:10.1007/s40258-015-0181-6
17. McIllhatton A, Lanting S, Lambkin D, et al. Reliability of recommended non-invasive chairside screening tests for diabetes-related peripheral neuropathy: a systematic review with meta-analyses. BMJ Open Diabetes Res Care. 2021;9(2):e002528. doi:10.1136/bmjdrc-2021-002528
18. Hu YM, Zhao LH, Zhang XL, et al. Association of glycaemic variability evaluated by continuous glucose monitoring with diabetic peripheral neuropathy in type 2 diabetic patients. Endocrine. 2018;60(2):292–300. doi:10.1007/s12020-018-1546-z
19. Yang J, Yang X, Zhao D, et al. Association of time in range, as assessed by continuous glucose monitoring, with painful diabetic polyneuropathy. J Diabetes Investig. 2021;12(5):828–836. doi:10.1111/jdi.13394
20. Abdelzaher LA, Imaizumi T, Suzuki T, et al. Astaxanthin alleviates oxidative stress insults-related derangements in human vascular endothelial cells exposed to glucose fluctuations. Life Sci. 2016;150:24–31. doi:10.1016/j.lfs.2016.02.087
21. Feldman EL, Nave KA, Jensen TS, et al. New horizons in diabetic neuropathy: mechanisms, bioenergetics, and pain. Neuron. 2017;93(6):1296–1313. doi:10.1016/j.neuron.2017.02.005
22. Quagliaro L, Piconi L, Assaloni R, et al. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes. 2003;52(11):2795–2804. doi:10.2337/diabetes.52.11.2795
23. Maser RE, Steenkiste AR, Dorman JS, et al. Epidemiological correlates of diabetic neuropathy. Report from Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes. 1989;38(11):1456–1461. doi:10.2337/diab.38.11.1456
24. Ismail-Beigi F, Craven T, Banerji MA, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376(9739):419–430. doi:10.1016/S0140-6736(10)60576-4
25. Stino AM, Smith AG. Peripheral neuropathy in prediabetes and the metabolic syndrome. J Diabetes Investig. 2017;8(5):646–655. doi:10.1111/jdi.12650
26. Liu J, Yuan X, Liu J, et al. Risk factors for diabetic peripheral neuropathy, peripheral artery disease, and foot deformity among the population with diabetes in Beijing, China: a Multicenter, Cross-Sectional Study. Front Endocrinol. 2022;13:824215. doi:10.3389/fendo.2022.824215
27. Jasti DB, Mallipeddi S, Apparao A, et al. A clinical and electrophysiological study of peripheral neuropathies in predialysis chronic kidney disease patients and relation of severity of peripheral neuropathy with degree of renal failure. J Neurosci Rural Pract. 2017;8(4):516–524. doi:10.4103/jnrp.jnrp_186_17
28. Aggarwal HK, Sood S, Jain D, et al. Evaluation of spectrum of peripheral neuropathy in predialysis patients with chronic kidney disease. Ren Fail. 2013;35(10):1323–1329. doi:10.3109/0886022X.2013.828261
29. Doshi S, Moorthi RN, Fried LF, et al. Chronic kidney disease as a risk factor for peripheral nerve impairment in older adults: a longitudinal analysis of Health, Aging and Body Composition (Health ABC) study. PLoS One. 2020;15(12):e242406. doi:10.1371/journal.pone.0242406
30. Moorthi RN, Doshi S, Fried LF, et al. Chronic kidney disease and peripheral nerve function in the Health, Aging and Body Composition Study. Nephrol Dial Transplant. 2019;34(4):625–632. doi:10.1093/ndt/gfy102
31. De Visser A, Hemming A, Yang C, et al. The adjuvant effect of hypertension upon diabetic peripheral neuropathy in experimental type 2 diabetes. Neurobiol Dis. 2014;62:18–30. doi:10.1016/j.nbd.2013.07.019
32. Jarmuzewska EA, Mangoni AA. Pulse pressure is independently associated with sensorimotor peripheral neuropathy in patients with type 2 diabetes. J Intern Med. 2005;258(1):38–44. doi:10.1111/j.1365-2796.2005.01500.x
33. Moura NA, Zantut-Wittmann DE. Abnormalities of thyroid hormone metabolism during systemic illness: the low T3 syndrome in different clinical settings. Int J Endocrinol. 2016;2016:2157583. doi:10.1155/2016/2157583
34. Kong X, Wang J, Gao G, et al. Association between free thyroxine levels and diabetic retinopathy in euthyroid patients with type 2 diabetes mellitus. Endocr Res. 2020;45(2):111–118. doi:10.1080/07435800.2019.1690504
35. Lin J, Xiang X, Qin Y, et al. Correlation of thyroid-related hormones with vascular complications in type 2 diabetes patients with euthyroid. Front Endocrinol. 2022;13:1037969. doi:10.3389/fendo.2022.1037969
36. He W, Pang C, Chen L, et al. Low T3 syndrome is associated with peripheral neuropathy in patients with type 2 diabetes mellitus. Muscle Nerve. 2022;66(6):723–729. doi:10.1002/mus.27719
37. Afarideh M, Aryan Z, Ghajar A, et al. Association of non-alcoholic fatty liver disease with microvascular complications of type 2 diabetes. Prim Care Diabetes. 2019;13(6):505–514. doi:10.1016/j.pcd.2019.03.009
38. Huang J, Li R, Liu N, et al. Liver fibrosis is independently associated with diabetic peripheral neuropathy in type 2 diabetes mellitus. J Diabetes Invest. 2021;12(11):2019–2027. doi:10.1111/jdi.13562
39. Mantovani A, Rigolon R, Mingolla L, et al. Nonalcoholic fatty liver disease is associated with an increased prevalence of distal symmetric polyneuropathy in adult patients with type 1 diabetes. J Diabetes Complications. 2017;31(6):1021–1026. doi:10.1016/j.jdiacomp.2017.01.024
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
