Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Association of Circulating Carbohydrate Antigen 19-9 Level with Type 2 Diabetic Kidney Disease in Chinese Adults: A Cross-Sectional Study
Authors Yan P , Li J, Zhang Y, Dan X, Wu X, Zhang X, Yang Y, Chen X, Li S, Chen P, Wan Q , Xu Y
Received 18 September 2023
Accepted for publication 16 January 2024
Published 31 January 2024 Volume 2024:17 Pages 467—477
DOI https://doi.org/10.2147/DMSO.S434972
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Muthuswamy Balasubramanyam
Pijun Yan,1– 5 Jia Li,1– 5 Yi Zhang,1– 5 Xiaofang Dan,1– 5 Xian Wu,1– 5 Xing Zhang,1– 5 Yuxia Yang,1– 5 Xiping Chen,6 Shengxi Li,6 Pan Chen,1– 5 Qin Wan,1– 5 Yong Xu1– 5
1Department of Endocrinology and Metabolism, the Affiliated Hospital of Southwest Medical University, Luzhou, People’s Republic of China; 2Metabolic Vascular Disease Key Laboratory of Sichuan Province, Luzhou, People’s Republic of China; 3Sichuan Clinical Research Center for Diabetes and Metabolism, Luzhou, People’s Republic of China; 4Sichuan Clinical Research Center for Nephropathy, Luzhou, People’s Republic of China; 5Cardiovascular and Metabolic Diseases Key Laboratory of Luzhou, Luzhou, People’s Republic of China; 6Clinical medical College, Southwest Medical University, Luzhou, People’s Republic of China
Correspondence: Pijun Yan, Department of Endocrinology and Metabolism, The Affiliated Hospital of Southwest Medical University, Luzhou, Sichuan, 646000, People’s Republic of China, Tel/Fax +86-830-3165361, Email [email protected]
Objective: Very few and conflicting data are available regarding the correlation between circulating carbohydrate antigen 19-9 (CA19-9) levels and diabetic kidney disease (DKD) and its components including albuminuria and a low estimated glomerular filtration rate (eGFR). This study aimed to examine the association of circulating CA19-9 and DKD in Chinese patients with type 2 diabetes mellitus (T2DM).
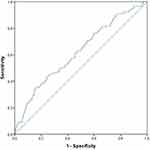
Methods: A total of 402 hospitalized T2DM patients between September 2017 and December 2021 were included in this cross-sectional study. There were 224 and 178 subjects in non-DKD and DKD groups, respectively. Serum CA19-9 was measured by chemiluminescence method, and its potential relationship with DKD was evaluated by multivariate logistic regression and correlation analyses, and receiver operating characteristic (ROC) curve analysis.
Results: T2DM patients with DKD had significantly higher serum CA19-9 levels than those without, and serum CA19-9 levels were positively related to urinary albumin-to-creatinine ratio and negatively to eGFR (P< 0.01). Multivariate regression analysis revealed that serum CA 19-9 was an independent factor of DKD [odds ratio (OR), 1.018; 95% confidence interval (CI), 1.002– 1.035; P< 0.05]. Moreover, an increased progressively risk of DKD with an increase in serum CA19-9 quartiles was observed (P for trend < 0.001), and T2DM patients in the highest serum CA19-9 quartile were associated with an increased likelihood of DKD when compared to those in the lowest quartile (OR: 2.936, 95% CI 1.129– 7.633, P< 0.05). Last, the analysis of ROC curves suggested that serum CA 19-9 at a cut of 25.09 U/mL resulted in the highest Youden index with sensitivity 43.8% and 75.4% specificity to predict the presence of DKD.
Conclusion: These results showed that high circulating CA19-9 was related to DKD and may serve as a useful biomarker of DKD in hospitalized Chinese T2DM patients.
Keywords: carbohydrate antigen 19-9, urinary albumin-to-creatinine ratio, diabetic kidney disease, estimated glomerular filtration rate, Chinese population
Introduction
Diabetic kidney disease (DKD) is one of the most common and intractable microvascular complications that occurs in approximately 25–40% of diabetic patients worldwide.1,2 It is well established that DKD is not only the main cause of end-stage renal disease worldwide,1 but also the leading cause of cardiovascular disease and all-cause mortality in diabetic patients,3,4 which imposes a considerable burden on healthcare systems and patients. Currently, albuminuria has been still considered to be a primary indicator of the onset or progression of DKD, yet albuminuria lacks the necessary sensitivity and specificity to accurately predict the development and progression of DKD in patients with type 2 diabetes mellitus (T2DM)5,6 because albuminuria is susceptible to many factors, such as infection, fever, exercise, diet, menstruation,7 and progressive nephropathy and renal impairment can occur in certain diabetic individuals who exhibit normal urinary albumin levels.6 Therefore, identification of new, non-invasive biomarkers for early diagnosis of DKD is imminent so as to better detect high-risk patients for early intervention.
Carbohydrate antigen 19-9 (CA19-9) is a tumor-associated antigen originally isolated from a human colorectal cancer cell line as a mucin-like product by Koprowski et al in 1976.8,9 CA19-9 was expressed in some tissues, including pancreatic cells, in the normal human body in very small amounts, and its levels were elevated in pancreatic cancer.8,10 Elevated serum CA19-9 levels were observed not only in many malignant tumors other than pancreatic cancer but also in benign diseases such as pancreatitis, biliary tract obstruction, inflammatory bowel disease, and thyroid disease.8,11 Recently, new evidence suggests that higher serum CA19-9 levels may be involved in abnormal glucose and lipid metabolism and were related to an increased risk of metabolic syndrome (MetS), insulin resistance (IR), dyslipidemia, T2DM, cerebrovascular microangiopathy, arterial stiffness, and coronary artery calcification (CAC).8,10,12–15 Since the above-mentioned cardio-metabolic abnormalities have been reported to be associated with microvascular complications in patients with T2DM,4,16,17 thus changes of serum CA19-9 levels may be related to diabetic microvascular complications. Indeed, some previous small sample size studies have shown that elevated circulating CA19-9 levels were associated with diabetic microvascular complications, such as diabetic retinopathy and neuropathy.18–22 However, very few and conflicting data are available regarding the association between circulating CA19-9 and DKD and its components, including albuminuria and renal function impairment, in patients with T2DM.18–24
Accordingly, we planned this study to explore the association of serum CA19-9 with DKD in Chinese patients with T2DM. Further, we explored the possible mechanisms by analyzing the association of serum CA19-9 with metabolic parameters, and inflammation and atherosclerotic vascular disease markers.
Materials and Methods
Study Population
A total of 2804 T2DM patients from September 2017 to December 2021, who were hospitalized for screening of diabetic chronic complications and optimizing their anti-diabetic regimen, were initially recruited. Subjects were diagnosed with T2DM according to the 1999 World Health Organization criteria.25 Inclusion criterion of the participants was adult patients with T2DM aged between 18 and 86 years, who signed an informed consent form. The exclusion criteria were as follows: 1) T1DM, recent acute complications of diabetes, severe diabetic foot ulcers, previous amputation, endocrine diseases other than T2DM; 2) pancreatic cancer, acute and chronic pancreatitis, cancers of the gastrointestinal tract, hepatocellular cancer, cholangitis, cholestasis, obstructive jaundice, liver abscess, liver cirrhosis, and other hepatobiliary, pancreatic and gastrointestinal diseases, and so on; 3) non-diabetic kidney disease, hepatic dysfunction, severe renal failure; 4) acute stroke and coronary syndromes, heart failure, pulmonary disease, hematological diseases, thromboembolic disease; 5) ovarian cancer, endometriosis; 6) connective tissue disorders, autoimmune diseases, inflammatory diseases, infectious disease, presence of stressful conditions (recent surgery, trauma); 7) current pregnancy and lactation; 8) history of abundant alcohol intake; 9) administration of immunosuppressive drug, hormonal replacement therapy, systemic corticosteroids; 10) missing data for serum CA 19-9 and other demographic or clinical characteristic indicators; 13) serum CA 19-9 >37 U/mL. Finally, 402 participants with T2DM were included in the analysis.
Clinical and Biochemical Measurements
A standard questionnaire was used for every participant to gather systematic information regarding demography (age, gender, number of cohabitants, educational attainment, family income, etc.), sleep quality, smoking, alcohol consumption, family history, medical history, and medication status. The classification of education level is as follows: less than high school (<9 years) and high school or further (≥9 years). Family income was classified as follows: low [0–100,000 Ren Min Bi (RMB)/year], medium (101,000–300,000 RMB/year), and high (>300,000 RMB/year). Sleep quality was classified as being either poor or good.
Weight and height were measured using a digital scale, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared.
Neck circumference (NC) was obtained with the use of standard methods, as described previously.26 Seated systolic and diastolic blood pressures (SBP and DBP) were measured three times by a well-trained nurse following a standard protocol using a mercury sphygmomanometer after the patients had rested quietly for 5–10 minutes, and the average of the three measurements was used for analysis.25
Venous blood samples were collected after 8–12 h overnight fasting in all subjects. Fasting blood glucose (FBG), 2h blood glucose (PBG), triglyceride (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C), creatinine (Cr) were measured using a 7060 fully-automatic biochemical analyzer (Hitachi) at the registered central laboratory located at the Affiliated Hospital of Southwestern Medical University. Glycated hemoglobin A1C (HbA1c) was measured by the anion exchange high performance liquid chromatography (Arkray Eluent 80A). White blood cell (WBC) count was determined using an automated blood cell counter (Mindray BC-6800). Serum CA 19-9 and fasting C-peptide (FCP) levels were measured by chemiluminescence method.
Atherogenic indices (atherogenic coefficient [AC], atherogenic index of plasma [AIP]) were calculated using lipid parameters.25 The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation was used to calculate the estimated glomerular filtration rate (eGFR).25,27 The urine samples were collected the following morning to measure the urinary microalbumin using immunoturbidimetric tests and creatinine enzymatically, and albumin-to-createinine ratio (UACR; mg/g creatinine) was calculated.26,28 DKD was diagnosed through low eGFR (eGFR <60 mL/min/1.73 m2), albuminuria (UACR ≥30 mg/g), or both.25,27,28
Statistical Analysis
The Statistical Package for Social Sciences (SPSS, version 20.0; IBM, Chicago, IL) was used to analyze the data. Continuous data are presented as mean ± standard deviation (SD) and categorical variables as number (percentage). The clinical and biochemical parameters were compared between the two groups or among the three groups by Student’s t-test and one-way analysis of variance (ANOVA) (normally distributed data) or the Mann–Whitney U- and Kruskal–Wallis tests (nonnormally distributed data) or χ2 tests (categorical data). The Spearman’s and partial correlation analysis were performed to analyze the correlations between CA19-9 and other parameters. Univariate and multivariate binary logistic regression analyses were performed to investigate the associations between circulating CA19-9 and DKD in all T2DM patients. In addition, all T2DM subjects were split into four groups according to the quartiles of circulating CA19-9: Q1 (0.57–11.49 U/mL), Q2 (11.50–18.94 U/mL), Q3 (18.95–30.60 U/mL), and Q4 (30.61–33.48 U/mL), and the association between circulating CA19-9 quartiles and DKD was investigated by analysis. The results were expressed as Odds ratios (OR) and 95% confidence intervals (CI). Further, we used receiver operating characteristic (ROC) curves and area under the curve (AUC) to assess the diagnostic and predictive values of circulating CA19-9 for DKD in all subjects. P-values <0.05 were considered statistically significant.
Results
Characteristics of Study Participants
Table 1 displays the baseline characteristics of participants between DKD and Non-DKD groups. Out of the study participants, 178 (44.28%) patients had DKD. Compared with T2DM patients without DKD, those with DKD demonstrated significantly longer diabetic duration, higher age, BMI, blood pressure (SBP, DBP), TC, TG, atherogenic indices (AIP, AC), WBC, serum Cr, UACR, CA19-9, and lower HDL-C and eGFR (P<0.0001 or P<0.01 or P<0.05). Supplementary Table 1 reports characteristics of participants among different quartiles of circulating CA 19-9. T2DM patients with higher circulating CA19-9 were less likely to be male (P<0.0001). Moving from the lowest to the highest circulating CA19-9 quartile, we observed increased levels of SBP, PBG, HbA1c, TC, TG, atherogenic indices, UACR, as well as increased percentages of participants with poor sleep quality, DKD, and albuminuria, and decreased levels of HDL-C, and eGFR (P<0.0001 or P<0.01 or P<0.05).
 |
Table 1 Characteristics of Study Participants |
Association of Circulating CA19-9 with DKD-Related Parameters
Spearman correlation analysis showed that circulating CA19-9 was positively related to blood pressure, blood glucose (FBG, PBG, HbA1c), TC, TG, atherogenic indices, UACR, and negatively to HDL-C and eGFR (P<0.0001 or P<0.01 or P<0.05; Table 2). Partial correlation analysis demonstrated that the associations among circulating CA19-9 and blood pressure, blood glucose, TG, HDL-C, atherogenic indices, WBC, serum Cr, eGFR, and UACR weakened, but still remained statistically significant (P<0.0001 or P<0.01 or P<0.05; Table 2).
 |
Table 2 Association of Circulating CA19-9 with DKD-Related Parameters |
Univariate and Multivariate Analysis of Determinants of DKD
Table 3 shows univariable and multivariable analyses of factors associated with DKD. On univariable analysis, age, diabetic duration, BMI, blood pressure, FBG, TC, TG, HDL, atherogenic indices, WBC, and circulating CA19-9 were significantly related to DKD (P<0.0001 or P<0.01 or P<0.05). Circulating CA19-9 remained independently significantly related to an increased risk of DKD on multivariable analysis (OR = 1.021, 95% CI: 1.005–1.037; P<0.01).
 |
Table 3 Univariate and Multivariate Logistic Analysis of Factors Associated with DKD |
Adjusted ORs and 95% CIs for DKD According to Quartiles of Circulating CA19-9
As presented in Table 4, the risk of DKD increased progressively with the increase in serum CA19-9 quartiles (P for trend <0.0001 or P for trend <0.01 or P for trend <0.05). T2DM patients in the highest serum CA19-9 quartile were associated with an increased likelihood of DKD when compared to those in the lowest quartile after adjusting for all confounding factors (OR: 2.864, 95% CI 1.101–7.450, P<0.05).
 |
Table 4 Adjusted ORs and 95% CIs for DKD According to Quartiles of Circulating CA19-9 |
The Diagnostic Value of Circulating CA19-9 for DKD in Patients with T2DM
As shown in Figure 1, serum CA 19-9 at a cut of 25.09 U/mL resulted in the highest Youden index with sensitivity 43.8% and 75.4% specificity to predict the presence of DKD.
Discussion
In the present study, we showed that T2DM patients with DKD had significantly increased levels of circulating CA19-9, and circulating CA19-9 was independently significantly associated with the presence of DKD. Moreover, the risk of DKD increased progressively with the increase in circulating CA19-9 quartiles. Last, circulating CA19-9 could predict the presence of DKD. These results indicate that increased CA19-9 was closely associated with DKD, and CA19-9 may be useful as a biomarker of DKD in T2DM patients.
CA19-9, a member of the Lewis antigen family, has become a commonly used biomarker for clinical diagnosis and monitoring of responses to pancreatic cancer therapy.29 Nowadays, there is evidence to suggest that altered circulating CA19-9 levels were related to IR, impaired glucose regulation, diabetes mellitus, dyslipidemia, MetS, cerebrovascular microangiopathy, arterial stiffness, CAC,8,10,12–15 thus it is plausible that elevated level of circulating CA19-9 may be an early signal for being at risk for DKD in T2DM patients. Here, we found that circulating CA19-9 levels were significantly elevated in T2DM subjects with DKD, and T2DM patients in the highest CA19-9 quartile demonstrated significantly higher prevalence of DKD and its components including albuminuria and low eGFR when compared with those in the lowest quartile. Further, circulating CA19-9 levels were positively related to UACR and negatively related to eGFR. Together, these results demonstrated that circulating CA19-9 level might be associated with DKD, and may be a useful marker of DKD in T2DM patients. Moreover, circulating CA19-9 was independently associated with DKD, and the risk of DKD increased progressively with the increase in circulating CA19-9 quartiles. Additionally, circulating CA19-9 could predict the presence of DKD. Consistent with our results, several previous studies demonstrated that T2DM patients with DKD or albuminuria or persistent proteinuria had higher circulating CA19-9 than controls,18,19,22–24 further suggesting that circulating CA19-9 level has a potential relationship with DKD. However, several small- sample studies found that circulating CA 19-9 level was not related to DKD and microalbuminuria (MIC) in Asian patients with T2DM.20,21 The difference between these results could be explained by differences in study population and their characteristics, ethnic background, range of circulating CA19-9 included, diagnostic criteria of DKD and MIC, statistical methods, sample size, and confounding factors adjusted in these studies. More studies are needed before conclusions can be drawn. Obesity, hyperglycemia, hypertension, and dyslipidemia have been recognized as risk factors for DKD.16,30,31 Consistent with that, we found that T2DM patients with DKD had significantly higher BMI, blood pressure, TC, TG, and lower HDL-C. Moreover, SBP, PBG, HbA1c, TC, and TG increased and HDL-C decreased progressively with the increase in serum CA19-9 quartiles, and circulating CA19-9 was positively related to blood pressure, TC, TG, blood glucose (FBG, PBG, HbA1c), and negatively to HDL-C, which were largely in accordance with results from previous studies.8,13,32–36 A cross-sectional study from India, consisted of 193 patients with T2DM who received different treatment modalities, showed that serum CA 19-9 level was positively correlated with BMI, 2-hour plasma glucose level, HbA1c, very low density lipoprotein cholesterol, TG, TC, LDL-C and negatively correlated with HDL-C.37 Another study performed by Tu et al demonstrated that participants with obesity and T2DM had significantly higher levels of serum CA19-9 than the control group, and changes in CA19-9 were independently and significantly related to changes of FBG, HbA1c, and homeostasis model assessment of IR (HOMA-IR) in subjects with obesity and T2DM after Roux-en-Y gastric bypass.8 Similar findings were reported in another two Chinese studies of T2DM patients.32,33 Moreover, healthy subjects or middle-aged and elderly community-dwelling residents with elevated CA 19-9 levels had higher blood glucose, TC, TG, LDL-C, incidence of hypertension, and prevalence of hyperglycemia, hypertension, and dyslipidemia (decreased HDL-C and increased TG) significantly increased across serum CA 19-9 tertiles.13,34–36 Combined, these results demonstrated that circulating CA19-9 levels may be closely related to IR, obesity, hyperglycemia, hypertension, and dyslipidemia, and the above-mentioned metabolic imbalance may, at least in part, mediate the association between circulating CA19-9 and DKD in type 2 diabetes. Studies found that persistent hyperglycemia, excessive cholesterol accumulation, and hypertension might contribute to glucolipotoxicity and inflammation and oxidative stress in the islet β cells, subsequently leading to pancreatic β cell dysfunction and impaired insulin secretion, eventually triggering the release of CA19-9, which was a marker of pancreatic exocrine tissue damage, through the pancreatic ducts.8,13,32,34–36,38,39 These data together suggest that circulating CA19-9 level might be associated with DKD in T2DM patients due to pancreatic β cell dysfunction and impaired insulin secretion induced by poor metabolic control. Future research is required to confirm our findings and to better understand the mechanisms associated with a possible pathogenic effect of circulating CA19-9 on DKD.
Compelling and increasing evidence has demonstrated that atherosclerosis due to endothelial dysfunction plays a paramount role in the pathogenesis of DKD.40–42 Here, we discovered that two atherogenic indices (AIP and AC) were significantly elevated in patients with DKD, and were both significantly associated with DKD, offering further evidence for the role of atherosclerosis in the pathogenesis of DKD. Moreover, the two atherogenic indices increased progressively with the increase in serum CA19-9 quartiles, and circulating CA19-9 was positively related to the two atherogenic indices. Further, circulating CA19-9 levels were positively related to UACR, which was an early hallmark of DKD43 and also an indicator of widespread inflammation, endothelial dysfunction, and vascular disease burden.44 These data together suggest that elevated circulating CA19-9 may be associated with atherosclerosis and endothelial dysfunction in patients with DKD, which was in line with those from most previous studies.15,45,46 A cross-sectional study discovered that serum CA 19-9 level was positively and independently related to coronary calcium score and brachial-ankle pulse wave velocity in 1732 Korean adults aged ≥45 years.15 Another two studies revealed that an increase in CA 19-9 was related to congestive heart disease and heart failure.45,46 Combined, these results demonstrated that atherosclerosis due to endothelial dysfunction might, in part, also mediate the role of circulating CA19-9 in and DKD in patients with T2DM. More prospective longitudinal studies should be performed to confirm our findings and further dissect the specific mechanism of action.
Limitations of our study must be appreciated for an accurate interpretation of the data. First, we cannot infer causal associations between circulating CA19-9 and DKD due to the cross-sectional design of this study. Further prospective, longitudinal studies with the progression – ie, diabetes to MIC to macroalbuminuria and end-stage kidney disease are needed to clarify the associations of circulating CA19-9 and DKD and to elucidate the precise mechanism underlying the association. Second, circulating CA 19-9 levels in healthy individuals were not available, which does not affect our experimental results, because previous studies have reported that serum CA19-9 levels were higher in T2DM patients than healthy individuals. Third, the lack of classical inflammatory markers, such as interleukin-6 and tumor necrosis factor-α, which could possibly impact the results. Fourth, not all patients received carotid ultrasonography examinations, which is a substitute marker of atherosclerosis, thus carotid intima-media thickness was not analyzed in the current study, which makes it difficult to further explore the association mechanism of CA19-9 and atherosclerosis. Despite these limitations, the advantages of the current study included a relatively large sample size, use of a standardized method at a single center, strict inclusion/exclusion criteria, thorough adjustment of possible confounding variables, and well-characterized nature of the patient cohort.
Conclusions
In summary, our data delineate that T2DM patients with DKD had significantly higher circulating CA19-9 level, and circulating CA19-9 was independently significantly related to DKD, thereby demonstrating that circulating CA19-9 might be used as a potential biomarker of DKD in Chinese adults with T2DM. However, more well-designed prospective studies are needed to confirm our findings and further define the role of circulating CA19-9 in DKD.
Data Sharing Statement
All data are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics Approval and Informed Consent
The study protocol complied with the Declaration of Helsinki and was approved by the human research ethics committee of the Affiliated Hospital of Southwest Medical University, and the patients signed an informed consent form.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the key Research and Development Program of Science and Technology Department of Sichuan Province (2022YFS0612).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Williams WW, Salem RM, McKnight AJ, et al. Association testing of previously reported variants in a large case-control meta-analysis of diabetic nephropathy. Diabetes. 2012;61(8):2187–2194. doi:10.2337/db11-0751
2. Feng B, Lu Y, Ye L, Yin L, Zhou Y, Chen A. Mendelian randomization study supports the causal association between serum cystatin C and risk of diabetic nephropathy. Front Endocrinol. 2022;13:1043174. doi:10.3389/fendo.2022.1043174
3. Gan J, Zheng Y, Yu Q, et al. Serum lipocalin-2 levels are increased and independently associated with early-stage renal damage and carotid atherosclerotic plaque in patients with T2DM. Front Endocrinol. 2022;13:855616. doi:10.3389/fendo.2022.855616
4. Reiss AB, Miyawaki N, Moon J, et al. CKD, arterial calcification, atherosclerosis and bone health: inter-relationships and controversies. Atherosclerosis. 2018;278:49–59. doi:10.1016/j.atherosclerosis.2018.08.046
5. Houeiss P, Njeim R, Tamim H, et al. Urinary 20-HETE: a prospective Non-Invasive prognostic and diagnostic marker for diabetic kidney disease. J Adv Res. 2023;44:109–117. doi:10.1016/j.jare.2022.04.013
6. Wei L, Han Y, Tu C. Molecular pathways of diabetic kidney disease inferred from proteomics. Diabetes Metab Syndr Obes. 2023;16:117–128. doi:10.2147/DMSO.S392888
7. Lin Z, Zhang D, Zhang X, et al. Extracellular status of thrombospondin-2 in type 2 diabetes mellitus and utility as a biomarker in the determination of early diabetic kidney disease. BMC Nephrol. 2023;24(1):154. doi:10.1186/s12882-023-03216-z
8. Tu Y, Yu H, Zhang P, et al. Decreased serum CA19-9 is associated with improvement of insulin resistance and metabolic control in patients with obesity and type 2 diabetes after Roux-en-Y gastric bypass. J Diabetes Investig. 2014;5(6):694–700. doi:10.1111/jdi.12200
9. Scarà S, Bottoni P, Scatena R. CA 19-9: biochemical and clinical aspects. Adv Exp Med Biol. 2015;867:247–260. doi:10.1007/978-94-017-7215-0_15
10. Li Z, Wang J, Han X, et al. Association between cancer antigen 19-9 and diabetes risk: a prospective and Mendelian randomization study. J Diabetes Investig. 2020;11(3):585–593. doi:10.1111/jdi.13166
11. Sharma JB, Sharma S, Usha BR, Gupta A, Kumar S, Mukhopadhyay AK. A cross-sectional study of tumor markers during normal and high-risk pregnancies. Int J Gynaecol Obstet. 2015;129(3):203–206. doi:10.1016/j.ijgo.2014.12.014
12. Zayed AA, Beano AM, Amer FN, et al. Serum levels of carcinoembryonic antigen in patients with type 2 diabetes. Endocr Pract. 2016;22(11):1310–1318. doi:10.4158/EP161221.OR
13. Du R, Cheng D, Lin L, et al. Association between serum CA 19-9 and metabolic syndrome: a cross-sectional study. J Diabetes. 2017;9(11):1040–1047. doi:10.1111/1753-0407.12523
14. Son DH, Lee HS, Lee YJ. Association between serum carbohydrate antigen 19-9 levels and leukoaraiosis in middle-aged and older adults: a cross-sectional study. Atherosclerosis. 2020;292:188–192. doi:10.1016/j.atherosclerosis.2019.11.003
15. Park B, Lee YJ. Association of serum carbohydrate antigen 19-9 level with arterial stiffness and coronary artery calcification in middle-aged and older adults: a cross-sectional study. J Hypertens. 2020;38(1):95–101. doi:10.1097/HJH.0000000000002217
16. Lin B, Ma YY, Wang JW. Nano-technological approaches for targeting kidney diseases with focus on diabetic nephropathy: recent progress, and future perspectives. Front Bioeng Biotechnol. 2022;10:870049. doi:10.3389/fbioe.2022.870049
17. Lee KY, Sohn YH, Baik JS, Kim GW, Kim JS. Arterial pulsatility as an index of cerebral microangiopathy in diabetes. Stroke. 2000;31(5):1111–1115. doi:10.1161/01.str.31.5.1111
18. Nakamura N, Aoji O, Yoshikawa T, et al. Elevated serum CA19-9 levels in poorly controlled diabetic patients. Jpn J Med. 1986;25(3):278–280. doi:10.2169/internalmedicine1962.25.278
19. Gul K, Nas S, Ozdemir D, Gumus M, Ersoy R, Cakir B. CA 19-9 level in patients with type 2 diabetes mellitus and its relation to the metabolic control and microvascular complications. Am J Med Sci. 2011;341(1):28–32. doi:10.1097/MAJ.0b013e3181f0e2a0
20. Kim SH, Baek CO, Lee KA, et al. Clinical implication of elevated CA 19-9 level and the relationship with glucose control state in patients with type 2 diabetes. Endocrine. 2014;46(2):249–255. doi:10.1007/s12020-013-0058-0
21. Cui L, Lv N, Li B, et al. Serum CA 19-9 level is correlated to the clinical characteristics and chronic complications of patients newly diagnosed with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2021;129(8):581–586. doi:10.1055/a-0994-9970
22. Tong W, Gao H, Wei X, et al. Correlation of serum CA199 levels with glycemic control and microvascular complications in patients with type 2 diabetes mellitus. Am J Transl Res. 2021;13(4):3302–3308.
23. Turgutalp K, Ozhan O, Helvacı I, et al. Serum levels of cancer biomarkers in diabetic and non-diabetic proteinuric patients: a preliminary study. Clin Chem Lab Med. 2013;51(4):889–895. doi:10.1515/cclm-2012-0657
24. Guo J, Sun C, Wang B, et al. Associations between vitamin D and β-cell function and colorectal cancer-associated tumor markers in Chinese type 2 diabetic patients with albuminuria. Clin Lab. 2019;65(4):641–649. doi:10.7754/Clin.Lab.2019.181111
25. Wu Y, Wan Q, Xu Y, et al. Lower visceral fat area in patients with type 2 diabetic peripheral neuropathy. Diabetes Metab Syndr Obes. 2022;15:3639–3654. doi:10.2147/DMSO.S388330
26. Fitch KV, Stanley TL, Looby SE, Rope AM, Grinspoon SK. Relationship between neck circumference and cardiometabolic parameters in HIV-infected and non-HIV-infected adults. Diabetes Care. 2011;34(4):1026–1031. doi:10.2337/dc10-1983
27. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
28. Yan P, Zhang Z, Wan Q, et al. Association of serum uric acid with bone mineral density and clinical fractures in Chinese type 2 diabetes mellitus patients: a cross-sectional study. Clin Chim Acta. 2018;486:76–85. doi:10.1016/j.cca.2018.07.033
29. Feng F, Tian Y, Xu G, et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer. 2017;17(1):737. doi:10.1186/s12885-017-3738-y
30. Chen MM, Jia JH, Tan YJ, et al. Shen-Qi-Jiang-Tang granule ameliorates diabetic nephropathy via modulating tumor necrosis factor signaling pathway. J Ethnopharmacol. 2023;303:116031. doi:10.1016/j.jep.2022.116031
31. Tahrani AA, Ali A, Raymond NT, et al. Obstructive sleep apnea and diabetic nephropathy: a cohort study. Diabetes Care. 2013;36(11):3718–3725. doi:10.2337/dc13-0450
32. Yu H, Li R, Zhang L, Chen H, Bao Y, Jia W. Serum CA19-9 level associated with metabolic control and pancreatic beta cell function in diabetic patients. Exp Diabetes Res. 2012;2012:745189. doi:10.1155/2012/745189
33. Shang X, Song C, Du X, Shao H, Xu D, Wang X. The serum levels of tumor marker CA19-9, CEA, CA72-4, and NSE in type 2 diabetes without malignancy and the relations to the metabolic control. Saudi Med J. 2017;38(2):204–208. doi:10.15537/smj.2017.2.15649
34. Du R, Sun W, Lin L, et al. Serum CA 19-9 and risk of incident diabetes in middle-aged and elderly Chinese: a prospective cohort study. Acta Diabetol. 2017;54(2):201–208. doi:10.1007/s00592-016-0937-y
35. Huang Y, Xu Y, Bi Y, et al. Relationship between CA 19-9 levels and glucose regulation in a middle-aged and elderly Chinese population. J Diabetes. 2012;4(2):147–152. doi:10.1111/j.1753-0407.2011.00179.x
36. Cheng YC, Li YH, Hsu CY, Lee IT. Synergistic association of carcinoembryonic antigen and carbohydrate antigen 19-9 on the risk of abnormal glucose regulation. Diabetes Metab Syndr Obes. 2020;13:1933–1942. doi:10.2147/DMSO.S256223
37. Ankit BS, Agrawal R, Gadhwal A, Chahar C, Agrawal RP. The influence of metformin on serum carbohydrate antigen 19-9 (CA 19-9) levels in type 2 diabetes mellitus patients. J Assoc Physicians India. 2018;66(3):38–41.
38. Liu XY. The high prevalence of short-term elevation of tumor markers due to hyperglycemia in diabetic patients. Diabetes Metab Syndr Obes. 2022;15:1113–1122. doi:10.2147/DMSO.S350599
39. Hao M, Head WS, Gunawardana SC, Hasty AH, Piston DW. Direct effect of cholesterol on insulin secretion: a novel mechanism for pancreatic beta-cell dysfunction. Diabetes. 2007;56(9):2328–2338. doi:10.2337/db07-0056
40. Li Z, Huang Q, Sun L, Bao T, Dai Z. Atherogenic index in type 2 diabetes and its relationship with chronic microvascular complications. Int J Endocrinol. 2018;2018:1765835. doi:10.1155/2018/1765835
41. Sakashita M, Tanaka T, Inagi R. Metabolic changes and oxidative stress in diabetic kidney disease. Antioxidants. 2021;10(7):1143. doi:10.3390/antiox10071143
42. Bjornstad P, Wiromrat P, Johnson RJ, et al. Serum uromodulin predicts less coronary artery calcification and diabetic kidney disease over 12 years in adults with type 1 diabetes: the CACTI study. Diabetes Care. 2019;42(2):297–302. doi:10.2337/dc18-1527
43. Harkin C, Cobice D, Brockbank S, et al. Biomarkers for detecting kidney dysfunction in type-2 diabetics and diabetic nephropathy subjects: a case-control study to identify potential biomarkers of DN to stratify risk of progression in T2D patients. Front Endocrinol. 2022;13:887237. doi:10.3389/fendo.2022.887237
44. Weir MR. Microalbuminuria and cardiovascular disease. Clin J Am Soc Nephrol. 2007;2(3):581–590. doi:10.2215/CJN.03190906
45. Lee SP, Sung IK, Kim JH, Lee SY, Park HS, Shim CS. Usefulness of carbohydrate antigen 19-9 test in healthy people and necessity of medical follow-up in individuals with elevated carbohydrate antigen 19-9 level. Korean J Fam Med. 2019;40(5):314–322. doi:10.4082/kjfm.18.0057
46. Varol E, Ozaydin M, Dogan A, Kosar F. Tumour marker levels in patients with chronic heart failure. Eur J Heart Fail. 2005;7(5):840–843. doi:10.1016/j.ejheart.2004.12.008
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.