Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Association Between Vitamin D Level and Respiratory Symptoms in Patients with Stable Chronic Obstructive Pulmonary Disease
Authors Lee CY, Shin SH, Choi HS , Im Y, Kim BG , Song JY, Lee D, Park HY, Lim JH
Received 22 June 2021
Accepted for publication 12 February 2022
Published 17 March 2022 Volume 2022:17 Pages 579—590
DOI https://doi.org/10.2147/COPD.S326037
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Min Zhang
Chai Young Lee,1,* Sun Hye Shin,1,* Hye Sook Choi,2 Yunjoo Im,1 Bo-Guen Kim,1 Ju Yeun Song,1 Daegeun Lee,1 Hye Yun Park,1 Jun Hyeok Lim3
1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea; 2Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Kyung Hee University Hospital, Seoul, Republic of Korea; 3Division of Pulmonology, Department of Internal Medicine, Inha University Hospital, Inha University School of Medicine, Incheon, Republic of Korea
*These authors contributed equally to this work
Correspondence: Hye Yun Park, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, Tel +82-2-3410-3429, Fax +82-2-3410-3849, Email [email protected] Jun Hyeok Lim, Division of Pulmonology, Department of Internal Medicine, Inha University Hospital, Inha University School of Medicine, Incheon, Republic of Korea, Tel +82-32-890-1038, Fax +82-32-890-3099, Email [email protected]
Purpose: Vitamin D insufficiency or deficiency is prevalent in patients with chronic obstructive pulmonary disease (COPD). However, the association between vitamin D levels and respiratory symptoms in patients with stable COPD has not been fully investigated. This study evaluated the association between vitamin D levels and respiratory symptoms in patients with stable COPD.
Patients and Methods: Patients with COPD who had their serum 25-hydroxyvitamin D (25-OH vitamin D) level measured within 6 months of spirometry between January 2016 and April 2020 were retrospectively included. Respiratory symptoms were assessed using the modified Medical Research Council (mMRC) scale and COPD assessment test (CAT) score.
Results: Of the 329 included patients, 193, 88, and 48 were categorized as having vitamin D deficiency (< 20 ng/mL), insufficiency (20– 29 ng/mL), and sufficiency (≥ 30 ng/mL), respectively. The mean serum 25-OH vitamin D level of each group was 13.45 ng/mL, 24.61 ng/mL, and 38.90 ng/mL, respectively. Patients with vitamin D insufficiency/deficiency showed higher CAT scores than those with vitamin D sufficiency (p = 0.004). In multivariable adjusted models, vitamin D insufficiency/deficiency was significantly associated with a CAT score of 10 or more (adjusted odds ratio [aOR] = 2.41, 95% confidence interval [CI] = 1.20– 4.82, p = 0.013) and mMRC ≥ 2 (aOR = 2.39, 95% CI = 1.08– 5.32, p = 0.032). Among CAT items, the amount of phlegm (p = 0.008), chest tightness (p = 0.030), breathlessness walking upstairs (p < 0.001), home activity limitations (p = 0.002), and lack of energy (p = 0.003) were significantly associated with vitamin D insufficiency/deficiency after adjustment for age, sex, body mass index, smoking history, Charlson comorbidity index, post-bronchodilator forced expiratory volume in 1 second, and season of blood draw.
Conclusion: Vitamin D insufficiency/deficiency were associated with worse respiratory symptoms in patients with stable COPD.
Keywords: chronic obstructive pulmonary disease, vitamin D, respiratory symptoms, COPD assessment test, modified Medical Research Council
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality and is projected to rise over 5.4 million annual deaths worldwide by 2060.1,2 COPD is a progressive inflammatory lung disease involving the airways, alveoli, and pulmonary vasculature, leading to progressive deterioration of lung function, loss of exercise capacity, and frequent exacerbations.3 These patients often have respiratory symptoms including chronic cough, sputum, breathlessness, and exercise limitations.4,5 Accordingly, the Global Initiative for Chronic Obstructive Lung Disease (GOLD)6 recommends not only measuring lung function but also measuring symptoms of COPD with either the modified Medical Research Council (mMRC) scale or the COPD Assessment Test (CAT).
In recent years, the pleiotropic role of vitamin D has been highlighted in various diseases. As an immunomodulatory effector, vitamin D can boost innate immune responses upon infection and regulate adaptive immune responses.7,8 Vitamin D metabolites support the induction of antiviral and antimicrobial effector mechanisms and attenuate inflammatory responses.9,10 In line with this, a previous study showed that patients with a vitamin D level <10 ng/mL had 2.33-fold increased risk of hospital-acquired bloodstream infection.11 Vitamin D insufficiency/deficiency has been linked to a broad range of diseases, including autoimmune diseases, allergic diseases, endocrine and metabolic disorders, cancer, infections, and cardiovascular disorders.12,13
Vitamin D insufficiency or deficiency is also found in a considerable proportion of patients with COPD. According to previous studies, low vitamin D levels are associated with low lung function,14–16 increased dyspnea,17 unfavorable quality of life assessments,17,18 and increased number of exacerbations16,19–22 in patients with COPD. A systematic review and meta-analysis showed that vitamin D3 administration decreased the rate of moderate/severe exacerbations of COPD in patients with baseline plasma 25-OH vitamin D levels below 25 ng/mL.23 However, there are limited studies regarding the association between vitamin D deficiency and respiratory symptoms in COPD patients.17,18 Moreover, the association between vitamin D insufficiency/deficiency (which is obviously more prevalent than deficiency alone) and detailed respiratory or non-respiratory symptoms has not been investigated. Thus, in this study, we aimed to determine the association between serum vitamin D insufficiency/deficiency (<30 ng/mL) and detailed respiratory and non-respiratory symptoms in stable COPD patients.
Materials and Methods
Study Population
This was a retrospective cohort study of COPD patients conducted at the Samsung Medical Center (a 1979-bed hospital with 11 pulmonary specialists in charge of the outpatient clinic in Seoul, South Korea) between January 2016 and April 2020. Electronic medical records contain routinely collected data on patient demographics, comprehensive clinical parameters, laboratory studies, and prescriptions. COPD was defined as a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio <0.7, and we excluded patients with current asthma.
During the study period, 1025 COPD patients aged 40 years or older were identified, and 416 patients who had their serum 25-hydroxyvitamin D (25-OH vitamin D) levels measured within 6 months of spirometry were included. Among them, 84 patients without CAT scores within 1 month were excluded, and three patients with acute exacerbation at measurement of CAT and serum 25-OH vitamin D were excluded. Finally, 329 stable COPD patients were included in the analysis (Figure 1).
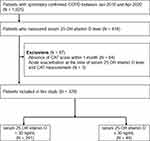 |
Figure 1 Flowchart of study population. Abbreviations: COPD, chronic obstructive pulmonary disease; CAT, COPD assessment test. |
Measurements
We retrospectively obtained data from electronic medical records, including age, sex, smoking history, body mass index (BMI), mMRC dyspnea scale, CAT score, Inhaler use, and comorbidities including cardiovascular disease (CVD), diabetes mellitus, chronic kidney disease, liver disease, dementia, connective tissue disease, and peptic ulcer disease. Patients with CVD were defined as those who had been diagnosed with coronary arterial disease, cerebrovascular disease, congestive heart failure, or peripheral arterial disease. Patients with stable COPD were defined as those without moderate or severe exacerbations when the CAT score and vitamin D were measured. Moderate or severe exacerbations were defined as a worsening of symptoms that required oral corticosteroids and/or antibiotics and/or hospitalization.24 Spirometry was performed and diffusing capacity for carbon monoxide (DLco) and lung volume were measured using Vmax 22 (SensorMedics, Yorba Linda, CA, USA) according to the American Thoracic Society and European Respiratory Society guidelines.25,26 Absolute values of FEV1, FVC, and DLco were obtained, and the percentage of predicted values (% pred) for FEV1, FVC, and DLco were calculated using data obtained from a representative Korean sample.27,28 The severity of COPD was based on the FEV1 (% pred) according to GOLD grades.6 Hyperinflation was measured using residual volume (RV)/total lung capacity (TLC).29
At every outpatient visit, patients were asked to complete the questionnaires for the mMRC dyspnea scale and CAT score, which were validated in the Korean language.30,31 We used the mMRC dyspnea grades and CAT scores assessed on the day that 25-OH vitamin D levels were measured. The mMRC dyspnea scale is graded from 0 to 4, depending on the severity of the dyspnea, defined as mMRC ≥2 indicating more breathlessness.32 The CAT consists of the following eight items: cough frequency, amount of phlegm, chest tightness, breathlessness walking upstairs, home activity limitations, not confident leaving home, sleep disturbance, and lack of energy.33 Each item is presented on a semantic 6-point (0–5) differential scale, providing a total score of 40.33 We defined a total CAT score ≥10 as a significant health impact.34
Patients were categorized into the vitamin D sufficiency group (plasma 25-OH vitamin D ≥30 ng/mL), vitamin D insufficiency group (plasma 25-OH vitamin D 20–29 ng/mL), and vitamin D deficiency group (plasma 25-OH vitamin D <20ng/mL).35 We compared detailed respiratory and non-respiratory symptoms measured using the mMRC scale and CAT among patient groups based on vitamin D level (sufficiency group vs insufficiency/deficiency and sufficiency vs insufficiency vs deficiency group).
Statistical Analyses
All data are expressed as the number (percentage) for categorical variables and as mean ± standard deviation (SD) or median (interquartile range) for continuous variables. The Pearson chi-square test or Fisher’s exact test was used to compare categorical variables, and Student’s t-test, one-way analysis of variance, or Jonckheere trend test was used to compare continuous variables. Spearman correlation test was used to assess the relationship between serum 25-OH vitamin D level (continuous), total CAT score, and lung function parameters. Multivariable logistic regression was used to evaluate the association between serum 25-OH vitamin D level (vitamin D sufficiency group vs insufficiency/deficiency group) and respiratory symptoms (mMRC ≥2 and CAT ≥10). We calculated odds ratios (ORs) and 95% confidence intervals (CIs) after adjustment for age, sex, BMI, smoking history (never vs ever), Charlson comorbidity index (CCI), post-bronchodilator FEV1 (≥50% vs <50% pred), and season of blood draw (spring/fall vs summer vs winter). Multivariable linear regression was used to calculate the difference in scores of each CAT item between the vitamin D sufficiency group and the insufficiency/deficiency group, with adjustment for the same variables as in the logistic regression model. Statistical significance was set at p < 0.05. SPSS (version 27.0; IBM Corp., Armonk, NY, USA) and Stata (version 14.2; StataCorp, College Station, TX, USA) was used for the statistical analyses.
Results
Baseline Characteristics
The mean (SD) serum 25-OH vitamin D level of the total study population (329 patients) was 20.15 (10.44) ng/mL, and levels ranged from 3.0 to 69.9 ng/mL (Figure 2). Using a cutoff value of 30 ng/mL, 281 patients were assigned to the vitamin D insufficiency/deficiency group and 48 patients to the vitamin D sufficiency group, with mean (SD) serum 25-OH vitamin D levels of 16.94 (6.40) ng/mL and 38.90 (9.79) ng/mL, respectively. The baseline characteristics of the 329 patients are summarized in Tables 1 and 2. No statistically significant differences were observed in the clinical characteristics (age, sex, BMI, smoking history, comorbidities, inhaler use, and previous exacerbation history) or pulmonary function parameters between the two groups.
 |
Table 1 Baseline Characteristics of COPD Patients Stratified by Vitamin D Level |
 |
Table 2 Baseline Pulmonary Function Parameters of COPD Patients Stratified by Vitamin D Level |
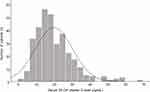 |
Figure 2 Histogram showing the distribution of 25-OH-vitamin D levels (ng/mL). |
In addition, among the 281 patients in the vitamin D insufficiency/deficiency group, 193 were further categorized into the vitamin D deficiency group with a mean (SD) serum 25-OH vitamin D of 13.45 (4.13) ng/mL. There were no statistically significant differences in the clinical characteristics and pulmonary function parameters when the patients were classified into three groups according to serum 25-OH vitamin D levels (Supplementary Table E1) or four groups by further subdividing the vitamin D deficiency group into those with vitamin D levels of 0–10 and 10–20 ng/mL (data not shown).
Vitamin D Levels According to Lung Function Parameters, Total CAT Score, and mMRC Grades
As shown in Figure 3, vitamin D levels showed a decreasing trend as GOLD grades increased (p for trend = 0.010) and total CAT score (p for trend < 0.001) and mMRC grades (p = 0.045) worsened. Analysis of vitamin D level as a continuous variable showed a weak but significant correlation with total CAT scores (rs = −0.193, p < 0.001; Figure 4A) and FEV1 (rs = 0.134, p = 0.015; Figure 5A). However, there was no significant correlation between DLco, RV/TLC, and vitamin D levels (Figure 5B and C).
Association Between Respiratory Symptoms and Vitamin D Insufficiency/Deficiency
As shown in Table 2, the mean CAT score in patients with vitamin D insufficiency/deficiency was higher than in those with vitamin D sufficiency (17.14 ± 8.57 vs 13.31 ± 8.08, p = 0.004). The proportion of patients with a CAT score ≥ 10 was also higher in the vitamin D insufficiency/deficiency group than in the vitamin D sufficiency group (80.4% vs 64.6%, p = 0.014). Similarly, the mean mMRC grade in patients with vitamin D insufficiency/deficiency was higher than in those with vitamin D sufficiency (1.41 ± 0.70 vs 1.19 ± 0.49, p = 0.039), and the proportion of patients with an mMRC ≥ 2 was higher in the vitamin D insufficiency/deficiency group than in the vitamin D sufficiency group (37.4% vs 22.9%, p = 0.053). This association of CAT score and mMRC with vitamin D level was similar when the patients were classified into three groups based on the serum 25-OH vitamin D level (Supplementary Table E2) or four groups by further subdividing the vitamin D deficiency group into those with vitamin D levels of 0–10 and 10–20 ng/mL (data not shown), except that there was no statistically significant difference in the proportion of patients with mMRC ≥2 among three or four groups.
In multivariable adjusted models, vitamin D insufficiency/deficiency was significantly associated with a CAT score ≥10 (adjusted OR [aOR] = 2.41, 95% CI = 1.20–4.82, p = 0.013) and mMRC ≥2 (aOR = 2.39, 95% CI = 1.08–5.32, p = 0.032) (Table 3).
 |
Table 3 The Association Between Respiratory Symptoms and Vitamin D Level < 30ng/mL |
Association Between Individual CAT Items and Vitamin D Insufficiency/Deficiency
When each item constituting the CAT score was analyzed individually, patients with vitamin D insufficiency/deficiency showed higher scores in the amount of phlegm (p = 0.009), chest tightness (p = 0.021), breathlessness walking upstairs (p = 0.001), home activity limitations (p = 0.009), and lack of energy (p = 0.018) than those with vitamin D sufficiency (Table 2). The difference in these five CAT items between the vitamin D insufficiency/deficiency and vitamin D sufficiency groups remained significant even after adjustment for age, sex, BMI, smoking history, CCI, post-bronchodilator FEV1 (≥50% vs <50% pred), and season of blood draw (spring/fall vs summer vs winter) (Table 4). The distribution of the mean score for each CAT item in the three groups classified according to serum 25-OH vitamin D level also showed a prominent difference in breathlessness walking upstairs and limitations in home activities (Figure 4B).
 |
Table 4 The Total Score and Each Item of CAT by Vitamin D Level (< 30ng/mL Vs ≥ 30ng/mL) |
Discussion
In this study, the majority of patients with stable COPD had vitamin D insufficiency/deficiency, and patients with vitamin D insufficiency/deficiency showed worse respiratory symptoms and quality of life than those with vitamin D sufficiency. Vitamin D levels were also positively associated with lung function, as measured by FEV1. In a further analysis of each CAT item according to vitamin D status, vitamin D insufficiency/deficiency was associated with not only respiratory symptoms such as amount of phlegm, chest tightness, and breathlessness walking upstairs, but also non-respiratory symptoms such as home activity limitations and lack of energy, indicating that vitamin D insufficiency/deficiency might reflect poor general health status of COPD patients.
Consistent with previous studies,17,18 our study showed an association between vitamin D deficiency/insufficiency and worse respiratory symptoms and low FEV1. Interestingly, Burkes et al showed that vitamin D levels were associated with respiratory symptoms in middle-aged patients with COPD.18 Contrary to Burkes’ study, we found an association between vitamin D and respiratory symptoms only in older patients, but not in middle-aged patients (Supplementary Tables E3 and E4 and Supplementary Figure 1). This difference might be explained by the difference in COPD severity between middle-aged patients (<65 years old) and older patients (≥65 years old). In the Burkes study, lung function and respiratory symptoms were worse in middle-aged patients than in older patients, whereas they were worse in older patients than in middle-aged patients in our study. Thus, we speculated that the association between vitamin D levels and respiratory symptoms might be more pronounced as a function of COPD severity than as a function of age itself.
Our study further investigated the association between vitamin D levels and individual items constituting the CAT score. In particular, the CAT scores corresponding to sputum, chest tightness, breathlessness going up hills/stairs, home activity limitations, and feeling a lack of energy were significantly higher in patients with vitamin D insufficiency/deficiency than in those with vitamin D sufficiency. In addition to respiratory symptoms, we showed that non-respiratory symptoms such as home activity limitations and feeling a lack of energy were significantly higher in patients with vitamin D insufficiency/deficiency than in those with vitamin D sufficiency. Given the nature of the cross-sectional study, we cannot ascertain the causality between vitamin D and these respiratory and non-respiratory symptoms, but as a lower level of vitamin D might result in poor muscle function, weakness, and myalgia,36 respiratory muscle weakness may contribute to respiratory impairment. Furthermore, skeletal muscle weakness and exertional dyspnea result in decreased outdoor physical activity, which in turn leads to a decrease in sun exposure.
Several other mechanisms could be considered regarding the influence of vitamin D insufficiency or deficiency on respiratory symptoms in COPD patients. Vitamin D has antibacterial and antiviral effects. Several studies have indicated a clinical association between vitamin D insufficiency and respiratory infections. A Finnish study conducted on 800 healthy men reported that subjects with 25-OH vitamin D levels <40 nmol/L had significantly more days of absence from duty because of respiratory infections.37 In a study carried out in 2135 patients with prehospitalization vitamin D measurements, patients with vitamin D <10 ng/mL had 2.33 times more hospital-acquired bloodstream infections.11 A recent meta-analysis of data from 46 randomized controlled trials of vitamin D supplementation for the prevention of acute respiratory infections revealed a protective effect of this intervention.38 Second, vitamin D has various immunomodulatory effects.7–10 The dysregulated immune response attributed to vitamin D insufficiency/deficiency leads to the development of chronic inflammation and aggravation of clinical symptoms.
In addition, among the stable COPD patients included in our study, the median 25-OH vitamin D level was 20.2 ng/mL, and 85.2% had vitamin D insufficiency/deficiency. Various causes, including lower food intake, skin aging with reduced capacity for vitamin D synthesis, absence of sun exposure, increased catabolism by glucocorticoids, impaired activation due to renal dysfunction, and lower storage capacity in muscles or fat could contribute to defective vitamin D status in patients with COPD.13
Our study has several limitations. First, given the observational nature of the study, there is always the possibility that selection bias or confounding might have influenced our findings. Second, this cross-sectional study could not explain the causal relationship between vitamin D levels and COPD. Additional prospective studies are needed to determine whether vitamin D insufficiency/deficiency leads to worsening of clinical symptoms or whether severely symptomatic patients acquire vitamin D insufficiency/deficiency. More prospective studies are necessary to determine whether vitamin D intake improves clinical symptoms.
Conclusion
This study adds to the existing evidence of an association between vitamin D deficiency and worse respiratory symptoms in patients with COPD by demonstrating that vitamin D insufficiency/deficiency (which is obviously more prevalent than deficiency alone) is also associated with more dyspnea and a higher impact of COPD symptoms on health status compared with vitamin D sufficiency. In addition, we showed that increasing levels of vitamin D are significantly correlated with the total CAT score as well as individual CAT items, especially breathlessness, home activity limitations, and lack of energy. Although current GOLD reports recommend assessment of vitamin D status for patients hospitalized for exacerbation of COPD and vitamin D supplementation only for those with severe deficiency, this study suggests that vitamin D supplementation might improve respiratory symptoms and health status in stable COPD patients with vitamin D insufficiency. Further studies are warranted to validate this finding, but meanwhile, clinicians should pay more attention to vitamin D insufficiency/deficiency in stable COPD patients with respiratory symptoms.
Abbreviations
COPD, chronic obstructive pulmonary disease; mMRC, modified Medical Research Council; CAT, COPD assessment test; CVD, cardiovascular disease; DLco, diffusing capacity for carbon monoxide; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; BMI, body mass index; OR, odds ratio; CI, confidence interval; CCI, Charlson comorbidity index.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding authors (Hye Yun Park or Jun Hyeok Lim) in response to reasonable requests.
Ethics Approval
This study was approved by the Institutional Review Board of Samsung Medical Center, and the requirement for informed consent was waived because of the retrospective nature of the study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Author Contributions
Chaiyoung Lee and Sun Hye Shin are co-first authors of this study. Hye Yun Park and Jun Hyeok Lim contributed equally to this work and supervised the work.
All authors made a significant contribution to the work, including the conception, study design, execution, acquisition of data, analysis, and interpretation; participated in drafting, revising, or critically reviewing the manuscript; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5: 691–706.
2. World Health Organization. Projections of mortality and causes of death, 2016 and 2060. Available from: https://www.who.int/healthinfo/global_burden_disease/projections_method.pdf. Accessed February 26, 2022.
3. Barnes P, Celli B. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33(5):1165–1185. doi:10.1183/09031936.00128008
4. Kim V, Criner GJ. The chronic bronchitis phenotype in COPD: features and implications. Curr Opin Pulm Med. 2015;21(2):133. doi:10.1097/MCP.0000000000000145
5. O’donnell DE, Lam M, Webb KA. Measurement of symptoms, lung hyperinflation, and endurance during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158(5):1557–1565. doi:10.1164/ajrccm.158.5.9804004
6. Global initiative for chronic obstructive lung disease global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease; 2021. Available from: http://www.goldcopd.org.
7. Prietl B, Treiber G, Pieber TR, Amrein K. Vitamin D and immune function. Nutrients. 2013;5(7):2502–2521. doi:10.3390/nu5072502
8. Rahman A, Hershey S, Ahmed S, Nibbelink K, Simpson RU. Heart extracellular matrix gene expression profile in the vitamin D receptor knockout mice. J Steroid Biochem Mol Biol. 2007;103(3–5):416–419. doi:10.1016/j.jsbmb.2006.12.081
9. Greiller CL, Martineau AR. Modulation of the immune response to respiratory viruses by vitamin D. Nutrients. 2015;7(6):4240–4270. doi:10.3390/nu7064240
10. Greiller CL, Suri R, Jolliffe DA, et al. Vitamin D attenuates rhinovirus-induced expression of intercellular adhesion molecule-1 (ICAM-1) and platelet-activating factor receptor (PAFR) in respiratory epithelial cells. J Steroid Biochem Mol Biol. 2019;187:152–159. doi:10.1016/j.jsbmb.2018.11.013
11. Cannell JJ, Vieth R, Umhau JC, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134(6):1129–1140. doi:10.1017/S0950268806007175
12. Adams JS, Hewison M. Update in vitamin D. J Clin Endocrinol Metab. 2010;95(2):471–478. doi:10.1210/jc.2009-1773
13. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi:10.1056/NEJMra070553
14. Black PN, Scragg R. Relationship between serum 25-hydroxyvitamin D and pulmonary function in the third national health and nutrition examination survey. Chest. 2005;128(6):3792–3798. doi:10.1378/chest.128.6.3792
15. Berg I, Hanson C, Sayles H, et al. Vitamin D, vitamin D binding protein, lung function and structure in COPD. Respir Med. 2013;107(10):1578–1588. doi:10.1016/j.rmed.2013.05.010
16. Burkes RM, Ceppe AS, Doerschuk CM, et al. Associations among 25-hydroxyvitamin d levels, lung function, and exacerbation outcomes in COPD: an analysis of the spiromics cohort. Chest. 2020;157(4):856–865. doi:10.1016/j.chest.2019.11.047
17. Ghosh AJ, Moll M, Hayden LP, Bon J, Regan E, Hersh CP. Vitamin D deficiency is associated with respiratory symptoms and airway wall thickening in smokers with and without COPD: a prospective cohort study. BMC Pulm Med. 2020;20(1):1–9. doi:10.1186/s12890-020-1148-4
18. Burkes RM, Couper DJ, Barjaktarevic IZ, et al. Age-dependent associations between 25-hydroxy vitamin D levels and COPD symptoms: analysis of SPIROMICS. J COPD Foundation. 2021;8(2):277. doi:10.15326/jcopdf.2020.0180
19. Malinovschi A, Masoero M, Bellocchia M, et al. Severe vitamin D deficiency is associated with frequent exacerbations and hospitalization in COPD patients. Respir Res. 2014;15(1):131. doi:10.1186/s12931-014-0131-0
20. Mekov E, Slavova Y, Tsakova A, et al. Vitamin D Deficiency and Insufficiency in Hospitalized COPD Patients. PLoS One. 2015;10(6):e0129080. doi:10.1371/journal.pone.0129080
21. Ferrari R, Caram LM, Tanni SE, Godoy I, de Paiva SAR. The relationship between Vitamin D status and exacerbation in COPD patients–a literature review. Respir Med. 2018;139:34–38. doi:10.1016/j.rmed.2018.04.012
22. Herr C, Greulich T, Koczulla RA, et al. The role of vitamin D in pulmonary disease: COPD, asthma, infection, and cancer. Respir Res. 2011;12(1):31. doi:10.1186/1465-9921-12-31
23. Jolliffe DA, Greenberg L, Hooper RL, et al. Vitamin D to prevent exacerbations of COPD: systematic review and meta-analysis of individual participant data from randomised controlled trials. Thorax. 2019;74(4):337–345. doi:10.1136/thoraxjnl-2018-212092
24. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117(5, Supplement 2):398S–401S. doi:10.1378/chest.117.5_suppl_2.398S
25. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
26. American Thoracic Society. Single-breath carbon monoxide diffusing capacity (transfer factor). recommendations for a standard technique–1995 update. Am J Respir Crit Care Med. 1995;152(6 Pt 1):2185–2198. doi:10.1164/ajrccm.152.6.8520796
27. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005;58(3):230–242. doi:10.4046/trd.2005.58.3.230
28. Park J, Choi I, Park K. Normal predicted standards of single breath carbon monoxide diffusing capacity of lung in healthy nonsmoking adults. Korean J Intern Med. 1985;28:176–183.
29. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi:10.1183/09031936.05.00035205
30. Kim HJ, Oh Y-M. The diagnosis of chronic obstructive pulmonary disease according to current guidelines. J Korean Med Assoc. 2018;61(9):539–544. doi:10.5124/jkma.2018.61.9.539
31. Hwang YI, Jung KS, Lim SY, Lee YS, Kwon NH. A validation study for the Korean version of chronic obstructive pulmonary disease assessment test (CAT). Tuberc Respir Dis. 2013;74(6):256–263. doi:10.4046/trd.2013.74.6.256
32. Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi:10.1136/thx.54.7.581
33. Jones P, Harding G, Berry P, Wiklund I, Chen W, Leidy NK. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
34. Jones PW, Tabberer M, Chen WH. Creating scenarios of the impact of COPD and their relationship to COPD assessment test (CAT™) scores. BMC Pulm Med. 2011;11:42. doi:10.1186/1471-2466-11-42
35. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30. doi:10.1210/jc.2011-0385
36. Girgis CM, Clifton-Bligh RJ, Hamrick MW, Holick MF, Gunton JE. The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr Rev. 2013;34(1):33–83. doi:10.1210/er.2012-1012
37. Laaksi I, Ruohola JP, Tuohimaa P, et al. An association of serum vitamin D concentrations < 40 nmol/L with acute respiratory tract infection in young Finnish men. Am J Clin Nutr. 2007;86(3):714–717. doi:10.1093/ajcn/86.3.714
38. Jolliffe DA, Camargo CA, Sluyter JD, et al. Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials. Lancet Diab Endocrinol. 2021;9(5):276–292. doi:10.1016/S2213-8587(21)00051-6
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



