Back to Journals » Nature and Science of Sleep » Volume 14
Association Between Sleep Quality and Hypertension in Chinese Adults: A Cross-Sectional Analysis in the Tianning Cohort
Authors Chen S, Song X, Shi H, Li J, Ma S , Chen L , Lu Y, Hong C, Zhu H , Sun H, Zhang M
Received 2 September 2022
Accepted for publication 15 November 2022
Published 28 November 2022 Volume 2022:14 Pages 2097—2105
DOI https://doi.org/10.2147/NSS.S388535
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Shi Chen,1,* Xugui Song,2,* Hongfei Shi,3 Jing Li,4 Shengqi Ma,4 Linan Chen,4 Ying Lu,4 Conglin Hong,4 Hanyun Zhu,4 Hongyan Sun,3 Mingzhi Zhang5
1Department of Nursing, School of Nursing, Suzhou Vocational Health College, Suzhou, People’s Republic of China; 2Shishan Community Health Service Center, Suzhou, People’s Republic of China; 3Center for Disease Prevention and Control of Tianning District, Changzhou, People’s Republic of China; 4Department of Epidemiology, School of Public Health, Medical College of Soochow University, Suzhou, People’s Republic of China; 5Department of Biostatistics, School of Public Health, Medical College of Soochow University, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Mingzhi Zhang, Department of Biostatistics, School of Public Health, Medical College of Soochow University, 199 Renai Road, Industrial Park, Suzhou, People’s Republic of China, 215123, Tel +86 512 6588 0079, Fax +86 512 6588 0052, Email [email protected] Hongyan Sun, Center for Disease Prevention and Control of Tianning District, Changzhou, People’s Republic of China, Email [email protected]
Background: Poor sleep quality is becoming very common in a developed society and relates to many health disorders. However, the association between sleep quality and hypertension has not been well studied in Chinese adults.
Methods: Blood pressure was measured and sleep quality was assessed by the Pittsburgh Sleep Quality Index (PSQI) for 5167 participants (mean aged 51± 15 years, 41.5% males) in the Tianning Cohort. A logistic regression model was constructed to examine the association between sleep quality, as well as its components, and hypertension, adjusting for age, sex, education level, current smoking, current drinking, physical activity, obesity, glucose, and blood lipids.
Results: After multivariate adjustment, a higher score Of the PSQI was significantly associated with an increased risk of prevalent hypertension (OR=1.03, P=0.018). Compared to participants with normal sleep (the PSQI score < 5), those with a poor sleep quality (the PSQI score ≥ 5) had a 17% increased risk of prevalent hypertension (OR=1.17, P=0.042). Three of the seven components of sleep quality, such as subjective sleep quality (OR=1.17, P=0.001), sleep latency (OR=1.11, P=0.010), and sleep disturbances (OR=1.19, P=0.004), were also significantly associated with prevalent hypertension.
Conclusion: Poor sleep quality is increasingly prevalent in developed societies and may be related to an increased risk of hypertension in Chinese adults. The underlying causality is waiting to be studied.
Keywords: sleep quality, hypertension, Pittsburgh Sleep Quality Index
Introduction
Sleep is an important fundamental need and a determinant for human’s optimal health through synchronizing the body’s circadian rhythm with a daily cycle.1,2 Unhealthy sleep patterns, e.g., staying up late and shift work, have been widespread in modern society, affecting approximately 20%~50% of people in the world,3,4 and this number is suggested to be 38.2% in China.5 Sleep dysfunction has been associated with a wide range of metabolic disorders, e.g., obesity,6 diabetes,7 and dyslipidemia,8 all are key contributors to hypertension which is a highly prevalent but modifiable risk factor of cardiovascular disease (CVD) - the leading cause of morbidity and mortality all over the world. The daily fluctuations in blood pressure further suggest a potential role of sleep in blood pressure regulation, where blood pressure decreases during normal sleep with autonomic regulation.9 Indeed, the association between poor sleep quality and hypertension has been extensively studied but with mixed results.10,11 For example, animal studies in rats found that obstructive sleep apnea (OSA)12,13 and sleep deprivation14 resulted in an elevation of blood pressure and hypertension development. Population studies found that patients with hypertension were more common to be companied with shortened sleep duration,15,16 OSA,17 and poor sleep quality.18 Most of these studies focused on one or some aspects of sleep, eg, sleep duration or insomnia. The construct of sleep quality likely incorporates multiple aspects eg, subjective sleep quantity, wakefulness, feeling of refreshment upon awakening, daytime sleepiness, and OSA.19 In fact, not all aspects of sleep quality were believed to play critical roles in hypertension and related complications,18 so it’s urgent to understand their individual contributions to hypertension. However, the contribution of individual aspect of sleep quality to hypertension is still waiting to be studied and whether they could jointly contribute to hypertension is unclear. Here, we used the Pittsburgh Sleep Quality Index (PSQI) to assess seven aspects of sleep quality and examined their associations, individually and jointly, with hypertension in more than five thousand Chinese adults in the Tianning Cohort study.
Methods
Participants
The Tianning Cohort study is an ongoing community-based prospective longitudinal study conducted in an economically developed area of Changzhou city (Tianning District), where the residents maintain a preference for sweet foods, to identify novel risk factors for diabetes and CVD. The study design, survey methods, and laboratory measurements of this study have been reported elsewhere.20 In brief, a total of 5199 participants aged over 18 years were recruited from 9 communities via cluster random sampling after signing a written informed consent from May to June 2018. After excluding 32 individuals with missing data on sleep quality, 5167 participants were included in the final analysis. The protocols of the Tianning Cohort study were approved by the Ethics Committee of Soochow University (approval No. ECSU-201800051). This study complies with the Declaration of Helsinki.
Assessment of Sleep Quality
Sleep quality was assessed by the PSQI questionnaire administered by trained staff. PSQI was a widely-used and effective self-report questionnaire for assessing sleep quality. It assesses sleep quality and disturbances very comprehensively through 19 individual items designed to assess seven components of sleep quality including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction.21 The score of each component is equally on a 0–3 scale with a higher score indicating a poorer sleep quality. The total score of the PSQI ranges from 0 to 21 and poor sleep quality was defined as a PSQI score over 5.22
Measurement of Blood Pressure
All participants were invited to participate in the physical examination provided between 7:00 and 10:00 in the morning. Blood pressure was measured 3 times (at least 30 seconds between each) by trained staff using a standard mercury sphygmomanometer and a cuff of appropriate size, according to a standard protocol,23 after the participants had been resting for at least 5 mins in a relaxed, sitting position. The first and fifth Korotkoff sounds were recorded as systolic blood pressure (SBP) and diastolic blood pressure (DBP), respectively. The mean of the 3 measurements was used in statistical analysis. According to the Chinese guidelines for Prevention and treatment of hypertension, hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg or use of antihypertensive medications in the last 2 weeks.24
Measurement of Risk Factors of Hypertension
Sociodemographic characteristics including age, sex, and educational level were collected by face-to-face interviews using standard questionnaires in Chinese administered by trained staff. Using the key questions from the Global Adult Tobacco Survey (GATS),25 smoking status was classified as current, former, and never smoking. Current smoking was defined as having smoked at least 100 cigarettes in the subject’s entire life, having smoked cigarettes regularly, and smoking currently. Former smoking was defined as having smoked at least 100 cigarettes in the subject’s entire life, having smoked cigarettes regularly in the past, and not smoking currently. Never smoking was defined as never smoking or having smoked fewer than 100 cigarettes in their lifetime. Alcohol consumption was similarly classified as current, former, and never drinking. Current drinking was defined as having consumed alcohol ≥12 times in the past year and drinking currently, former drinking was defined as having stopped drinking alcohol for at least 12 months, and never drinking was defined as never drinking alcohol in their lifetime. Physical activity was assessed by the Global Physical Activity Questionnaire (GPAQ) which collected information on physical activity at work, commuting, and recreational activities as well as sedentary behavior.26 The measured data were processed according to the GPAQ Analysis Guide, and Metabolic Equivalents minutes (MET-min) per week were calculated and used in data analysis. Body weight and height were measured using a regularly calibrated stadiometer and balance-beam scale with participants wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Waist circumference was measured at 1 cm above the umbilicus. Fasting glucose was detected in overnight fasting blood samples by Hexokinase methods (Siemens Healthcare Diagnostic Inc., Co Antrim, UK). Blood lipids including total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were measured by the Siemens ADVIA Chemistry XPT system using commercial reagents (Siemens Healthcare Diagnostic Inc., Co Antrim, UK).
Statistical Analysis
A logistic regression of a binary response variable (hypertension) on a continuous variable (the PSQI score) with a sample size of 5167 observations achieves 100% power at a 0.05 significance level to detect a change in probability of hypertension from the value of 0.05 to 0.07 when the PSQI score is increased to one standard deviation above the mean. This change corresponds to an odds ratio of 1.5. An adjustment was made since a multiple regression of the PSQI score on the covariates in the logistic regression obtained an R-Squared of 0.1.27
Clinical characteristics of study participants were presented in participants with and without hypertension, respectively. The scores of the PSQI and its components in the two groups of participants were compared using the Wilcoxon rank-sum test. To examine the association between sleep quality and hypertension, we constructed a logistic regression model in which prevalent hypertension (y/n) was the dependent variable and sleep quality (continual PSQI score or categorical poor vs normal) was the independent variable, adjusting for age, sex, education level, cigarette smoking, alcohol consumption, physical activity, BMI, glucose, LDL-C, and HDL-C. The association between the individual component of sleep quality and hypertension was similarly examined. To facilitate data visualization, partial effect plots with spline curves were captured to visualize the impact of the PSQI total score on hypertension by constructing a restricted cubic spline regression model. All statistical analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). A two-tailed P value less than 0.05 was considered statistically significant.
Sensitivity Analysis
To examine whether sex moderates the association between sleep quality and hypertension, we conducted a subgroup analysis by sex. To examine whether cardiovascular disorders modify the association between sleep quality and hypertension, we further excluded participants with coronary heart disease or stroke.
Results
Clinical Characteristics of Study Participants
A total of 5167 participants (mean aged 51±15 years, 41.5% males) were included in the current study. Among them, 2046 individuals (39.6%) were diagnosed with hypertension and 1144 individuals (22.1%) suffered from poor sleep quality. Poor sleep quality was more common in participants with hypertension than in those without (25.3% vs 20.1%, P<0.001). Their clinical characteristics were shown in Table 1. As expected, participants with hypertension were more likely to be older and male and have more risk factors, eg, cigarette smoking, alcohol consumption, obesity, blood glucose, and lipids (all P<0.05), compared to those without hypertension.
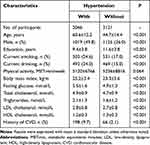 |
Table 1 The Clinical Characteristics of Study Participants According to Prevalent Hypertension |
The PSQI Scores According to Hypertension Status
Participants with hypertension had a significantly higher PSQI score than those without (median: 4 vs 3, P<0.001), as illustrated in Figure 1. Table 2 Additionally presented the distributions of the seven components of PSQI according to hypertension status. Compared to participants free of hypertension, those with hypertension were more likely to have a poorer quality of 5 of the 7 PSQI components, such as subjective sleep quality (P<0.001), sleep latency (P=0.003), habitual sleep efficiency (P=0.016), sleep disturbance (P<0.001), and use of sleeping medicine (P<0.001). These results suggested a probable association between sleep quality and hypertension.
 |
Table 2 The Distribution of the Seven PSQI Components According to Hypertension |
Association Between Sleep Quality and Hypertension
We further examined the association between sleep quality assessed by the PSQI scores and prevalent hypertension. As illustrated in Figure 2, a higher score of the PSQI was significantly associated with an increased risk of prevalent hypertension (OR=1.03, P=0.018), after adjusting for age, sex, education level, current smoking, current drinking, physical activity, BMI, glucose, LDL-C, and HDL-C. Compared to participants with normal sleep (the PSQI score <5), those with a poor sleep quality (the PSQI score ≥5) had a 17% increased risk of prevalent hypertension (OR=1.17, P=0.042). Table 3 presents the associations between the seven components of sleep quality and hypertension. After adjusting for covariates, three components of the PSQI, such as subjective sleep quality (OR=1.17, P=0.001), sleep latency (OR=1.11, P=0.010), and sleep disturbances (OR=1.19, P=0.004), were significantly associated with prevalent hypertension. We failed to find statistically significant associations of other components of sleep quality with prevalent hypertension (all P>0.05).
 |
Table 3 The Associations of the Seven PSQI Components with Hypertension |
Results of Sensitivity Analysis
Subgroup analysis by sex found that the association between subjective sleep quality and hypertension persisted in both males and females (Supplementary Table S1). No significant group-difference in the magnitude of the association was found, suggesting that the association between sleep quality and hypertension was not influenced a lot by sex. After excluding participants with coronary heart disease or stroke, the association between the PSQI components and hypertension did not change a lot (Supplementary Table S2). These results indicated that the association between sleep quality and hypertension may not be driven by cardiovascular disorders.
Discussion
In the community-based study of Tianning Cohort, we found a significant association between sleep quality assessed by the PSQI questionnaire and prevalent hypertension in Chinese adults. Participants with poor sleep quality were more likely to have hypertension, independent of conventional risk factors including other behaviors and metabolic factors. These findings indicate that poor sleep quality may participate in the development of hypertension through mechanisms beyond metabolic factors.
Sleep disorder, including conditions that affect sleep quality, timing, or duration and impact a person’s ability to properly function while they are awake, is becoming a very common unhealthy problem with the rapid economic development in China. Data released by HUAWEI Sports Health in 2017 showed that approximately 69.4% of cell phone users have a not very good sleep quality and 23% of young people had a habit of staying up late.28 Sleep quality is the measurement of how well a person is sleeping – in other words, whether the sleep is restful and restorative. It’s very complicated to be measured and not entirely subjective. The PSQI is a widely-used and effective self-report questionnaire for assessing sleep quality. It assesses sleep quality and disturbances very comprehensively through 19 individual items designed to assess seven components of sleep quality including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction.21 In our study, 22.1% of the participants reported having poor sleep quality assessed by the PSQI questionnaire.
In line with our study, the observed association between poor sleep quality and hypertension has also been found in previous studies. For example, a cross-sectional study including 9404 adults aged 20–93 years in northeastern China found that poor sleep quality defined as the global score of PSQI >5 was significantly associated with an increased risk of prevalent hypertension (OR=2.38, 95% CI:2.13–2.65).29 A similar association was also observed in other cross-sectional studies of Chinese adults.30–32 In addition, sleep duration, an important component of sleep quality, has also been associated with hypertension in varied populations.33–38 Sleep quality represents a complex phenomenon including quantitative and qualitative aspects so it should be assessed comprehensively. Only focusing on sleep duration or any one aspect of sleep quality was insufficient and might be biased to examine the association between sleep quality and hypertension. For example, Bansil et al18 investigated the role of sleep duration and sleep quality in hypertension development separately in participants of the NHANS, and found that sleep duration alone failed to affect the hypertension prevalence. In our study, we further analyzed whether the individual components of sleep quality were associated with hypertension and found that three components of PSQI including subjective sleep quality, sleep latency, and sleep disturbances were associated with hypertension, while the other components including sleep duration were failed to be significantly associated with hypertension. Although the association between sleep duration and hypertension was not significant either in the NHANS participants,18 many studies33,36–38 indicated that sleep duration was associated with hypertension. Anyway, each component of PSQI only reflects one aspect of sleep quality. It’s better to examine the association between sleep quality and hypertension, both individually and jointly.
Some possible mechanisms underlying the association between poor sleep quality and hypertension were considered. Of these, stimulation of the sympathetic activity plays an important role.39,40 Additionally, psychosocial stress, inflammation, oxidative stress, and endothelial dysfunction were reported to link sleep disorders with the development and progression of hypertension.28 Further, a poor sleep quality could predict a significantly increased risk of CVD in the future.41 As the leading risk factor of CVD, hypertension may mediate the contribution of sleep quality to CVD, although such mediating effect has not been systemically examined. Therefore, sleep quality, as a modifiable factor, may be of great significance in the prevention of hypertension and cardiovascular complications.
Some limitations should be mentioned in our study. First, this is a cross-sectional study. The causality of the association between poor sleep quality and hypertension cannot be established. Second, although we used unselected sample, the participants in the Tianning Cohort were of the Han ethnicity and could not represent other ethnic populations. The generalizability of our results should be taken cautiously. Third, only self-reported questionnaires were used to assess sleep quality. Possible misclassification and recall bias might exist and influent our results. Fourth, some sleep-related breathing disorders such as insomnia and obstructive sleep apnea have been associated with hypertension and may influent the association between sleep quality and hypertension. We did not obtain such data and the influence of sleep-related breathing disorders on our results can not be prevented.
In summary, hypertension and poor sleep quality are becoming serious health problems in Chinese adults. Participants with poor sleep quality were more likely to have elevated blood pressure and hypertension. Although we can not establish the causality, sleep quality should have to be monitored and under Control for adults to improve the prevention and management of hypertension, as well as other cardiovascular disorders.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We are deeply appreciative of the participants in this study and thank all staff for their support and assistance. Especially, we thank the Center for Disease Prevention and Control of Tianning District for their support in the recruitment of participants. Shi Chen and Xugui Song are co-first authors for this study.
Funding
This study was supported by the National Natural Science Foundation of China (NO. 81872690 and 82173596), Youth Technology and Science Projects of Suzhou Vocational Health College (NO. SZWZY202216), and a Project of the Priority Academic Program Development of Jiangsu Higher Education Institutions.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Czeisler CA, Weitzman E, Moore-Ede MC, Zimmerman JC, Knauer RS. Human sleep: its duration and organization depend on its circadian phase. Science. 1980;210:1264–1267. doi:10.1126/science.7434029
2. Czeisler CA, Gooley JJ. Sleep and circadian rhythms in humans. Cold Spring Harb Symp Quant Biol. 2007;72:579–597. doi:10.1101/sqb.2007.72.064
3. Kerkhof GA. Epidemiology of sleep and sleep disorders in the Netherlands. Sleep Med. 2017;30:229–239. doi:10.1016/j.sleep.2016.09.015
4. Hublin C, Kaprio J, Partinen M, Koskenvuo M. Insufficient sleep--A population-based study in adults. Sleep. 2001;24:392–400. doi:10.1093/sleep/24.4.392
5. Societies TsMSCoWFoCM. academic reviews of the sleep medicine specialty committee of word federation of Chinese medicine societies. Sleep Med. 2016;2017(4):57–61.
6. Fatima Y, Doi SAR, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17:1154–1166. doi:10.1111/obr.12444
7. Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38:529–537. doi:10.2337/dc14-2073
8. Kruisbrink M, Robertson W, Ji C, Miller MA, Geleijnse JM, Cappuccio FP. Association of sleep duration and quality with blood lipids: a systematic review and meta-analysis of prospective studies. BMJ open. 2017;7:e018585. doi:10.1136/bmjopen-2017-018585
9. Morgan TO. The importance of sleep blood pressure. Expert Rev Cardiovasc Ther. 2010;8:803–809. doi:10.1586/erc.10.60
10. Smolensky MH, Hermida RC, Castriotta RJ, Portaluppi F. Role of sleep-wake cycle on blood pressure circadian rhythms and hypertension. Sleep Med. 2007;8:668–680. doi:10.1016/j.sleep.2006.11.011
11. Sayk F, Teckentrup C, Becker C, et al. Effects of selective slow-wave sleep deprivation on nocturnal blood pressure dipping and daytime blood pressure regulation. Am J Physiol Regul Integr Comp Physiol. 2010;298:R191–197. doi:10.1152/ajpregu.00368.2009
12. Wu H, Lv Q, Zhang H, et al. The reduction of apnea-hypopnea duration ameliorates endothelial dysfunction, vascular inflammation, and systemic hypertension in a rat model of obstructive sleep apnea. Sleep Breath. 2019;23:1187–1196. doi:10.1007/s11325-019-01798-3
13. Troncoso Brindeiro CM, Da Silva AQ, Allahdadi KJ, Youngblood V, Kanagy NL. Reactive oxygen species contribute to sleep apnea-induced hypertension in rats. Am J Physiol Heart Circ Physiol. 2007;293:H2971–2976. doi:10.1152/ajpheart.00219.2007
14. Jiang J, Gan Z, Li Y, et al. Rem sleep deprivation induces endothelial dysfunction and hypertension in middle-aged rats: roles of the enos/no/cgmp pathway and supplementation with l-arginine. PLoS One. 2017;12:e0182746. doi:10.1371/journal.pone.0182746
15. Wang Q, Xi B, Liu M, Zhang Y, Fu M. Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertens Res. 2012;35:1012–1018. doi:10.1038/hr.2012.91
16. Yadav D, Hyun DS, Ahn SV, Koh SB, Kim JY. A prospective study of the association between total sleep duration and incident hypertension. J Clin Hypertens. 2017;19:550–557. doi:10.1111/jch.12960
17. Calhoun DA. Obstructive sleep apnea and hypertension. Curr Hypertens Rep. 2010;12:189–195. doi:10.1007/s11906-010-0112-8
18. Bansil P, Kuklina EV, Merritt RK, Yoon PW. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: results from the national health and nutrition examination survey, 2005 to 2008. J Clin Hypertens. 2011;13:739–743. doi:10.1111/j.1751-7176.2011.00500.x
19. Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: a comparison of individuals with and without insomnia. Sleep. 2008;31:383–393. doi:10.1093/sleep/31.3.383
20. Yu J, Sun H, Shang F, et al. Association between glucose metabolism and vascular aging in Chinese adults: a cross-sectional analysis in the tianning cohort study. Clin Interv Aging. 2019;14:1937–1946. doi:10.2147/CIA.S223690
21. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi:10.1016/0165-1781(89)90047-4
22. Afiat M, Dizavandi FR, Kargarfard L, Vahed SHM, Ghazanfarpour M. Effect of foeniculum vulgare (fennel) on sleep quality of menopausal women: a double-blinded, randomized placebo-controlled trial. J Menopausal Med. 2018;24:204–209. doi:10.6118/jmm.2018.24.3.204
23. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the jnc 7 report. JAMA. 2003;289:2560–2572. doi:10.1001/jama.289.19.2560
24. Liu LS, Wu ZS, Wang JG, et al. 2018 Chinese guidelines for prevention and treatment of hypertension-A report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019;16:182–241. doi:10.11909/j.issn.1671-5411.2019.03.014
25. Li D, Lv J, Liu F, et al. Hypertension burden and control in mainland China: analysis of nationwide data 2003–2012. Int J Cardiol. 2015;184:637–644. doi:10.1016/j.ijcard.2015.03.045
26. Armstrong T, Bull F. Development of the world health organization global physical activity questionnaire (gpaq). J Public Health. 2006;14:66–70. doi:10.1007/s10389-006-0024-x
27. Hsieh FY, Bloch DA, Larsen MD. A simple method of sample size calculation for linear and logistic regression. Stat Med. 1998;14(17):1623–1634. doi:10.1002/(SICI)1097-0258(19980730)17:14<1623::AID-SIM871>3.0.CO;2-S
28. Liu H, Chen A. Roles of sleep deprivation in cardiovascular dysfunctions. Life Sci. 2019;219:231–237. doi:10.1016/j.lfs.2019.01.006
29. Liu R-Q, Qian Z, Trevathan E, et al. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens Res. 2016;39(1):54–59. doi:10.1038/hr.2015.98
30. Lu K, Ding R, Tang Q, et al. Association between self-reported global sleep status and prevalence of hypertension in Chinese adults: data from the kailuan community. Int J Environ Res Public Health. 2015;12:488–503. doi:10.3390/ijerph120100488
31. Zhang H, Li Y, Zhao X, et al. The association between Psqi score and hypertension in a Chinese rural population: the Henan rural cohort study. Sleep Med. 2019;58:27–34. doi:10.1016/j.sleep.2019.03.001
32. Lu K, Chen J, Wang L, et al. Association of sleep duration, sleep quality and shift-work schedule in relation to hypertension prevalence in Chinese adult males: a cross-sectional survey. Int J Environ Res Public Health. 2017;14:210.
33. Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first national health and nutrition examination survey. Hypertension. 2006;47:833–839. doi:10.1161/01.HYP.0000217362.34748.e0
34. Cappuccio FP, Stranges S, Kandala NB, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall ii study. Hypertension. 2007;50:693–700. doi:10.1161/HYPERTENSIONAHA.107.095471
35. Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among us adults varies by age and sex. Am J Hypertens. 2012;25:335–341. doi:10.1038/ajh.2011.201
36. Wu X, Sun Y, Niu K, et al. Association of self-reported sleep duration and hypertension: results of a Chinese prospective cohort study. Clin Exp Hypertens. 2016;38:514–519. doi:10.3109/10641963.2016.1163367
37. Faraut B, Touchette E, Gamble H, et al. Short sleep duration and increased risk of hypertension: a primary care medicine investigation. J Hypertens. 2012;30:1354–1363. doi:10.1097/HJH.0b013e32835465e5
38. Li M, Yan S, Jiang S, Ma X, Gao T, Li B. Relationship between sleep duration and hypertension in northeast China: a cross-sectional study. BMJ open. 2019;9:e023916. doi:10.1136/bmjopen-2018-023916
39. Fisher JP, Paton JF. The sympathetic nervous system and blood pressure in humans: implications for hypertension. J Hum Hypertens. 2012;26:463–475. doi:10.1038/jhh.2011.66
40. Joyner MJ, Charkoudian N, Wallin BG. A sympathetic view of the sympathetic nervous system and human blood pressure regulation. Exp Physiol. 2008;93:715–724. doi:10.1113/expphysiol.2007.039545
41. Heinzer R, Hirotsu C, Marques-Vidal P, et al. 0859 sleep determinants of incident cardiovascular events: a prospective population-based study. Sleep. 2019;42:A344–A345. doi:10.1093/sleep/zsz067.857
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


