Back to Journals » International Journal of Women's Health » Volume 15
Association Between Endometriosis and Mental Disorders Including Psychiatric Disorders, Suicide, and All-Cause Mortality -A Nationwide Population-Based Cohort Study in Taiwan
Authors Wang TM , Lee YL, Chung CH , Sun CA, Kang CY , Wu GJ, Chien WC
Received 12 July 2023
Accepted for publication 8 November 2023
Published 28 November 2023 Volume 2023:15 Pages 1865—1882
DOI https://doi.org/10.2147/IJWH.S430252
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Tsan-Min Wang,1 Yi-Liang Lee,2,3 Chi-Hsiang Chung,1,4,5 Chien-An Sun,6,7 Chieh-Yi Kang,8 Gwo-Jang Wu,1,2,9 Wu-Chien Chien1,4,5,10
1Department of Medical Research, Tri-Service General Hospital, Taipei, 11490, Taiwan; 2Department of Obstetrics and Gynecology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China; 3Department of Obstetrics and Gynecology, Kang Ning Hospital, Taipei, Taiwan, Republic of China; 4School of Public Health, National Defense Medical Center, Taipei, 11490, Taiwan; 5Taiwanese Injury Prevention and Safety Promotion Association (TIPSPA), Taipei, 11490, Taiwan; 6Department of Public Health, College of Medicine, Fu-Jen Catholic University, New Taipei City, Taiwan, Republic of China; 7Big Data Research Center, College of Medicine, Fu-Jen Catholic University, New Taipei City, Taiwan, Republic of China; 8Department of Obstetrics & Gynecology, Chi Mei Medical Center Gynecologic Oncologist Division, Tainan City, Taiwan, Republic of China; 9Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei, 11490, Taiwan; 10Graduate Institute of Life Sciences, National Defense Medical Center, Taipei, 11490,Taiwan
Correspondence: Wu-Chien Chien; Gwo-Jang Wu, Email [email protected]; [email protected]
Objective: A multitude of previous studies has substantiated that endometriosis correlated highly with psychiatric health. This study aims to investigate the association between endometriosis and psychiatric health.
Methods: Utilizing the National Health Insurance Research Database of Taiwan, 100,770 enrolled participants, including 20,154 patients with endometriosis and 80,616 in the control group (1:4), matched for age, and index date from Taiwan’s Longitudinal Health Insurance Database between January 1, 2000, and December 31, 2015. The Cox proportional regression model was used to compare the risk of mental disorders during the 16 years of follow-up after adjusting for confounding factors.
Results: Of the study patients, 4083 (20.26%) developed mental disorders; 9225 of the 80,616 controls (11.44%) developed mental disorders. The Cox regression demonstrated that, after adjusting for age, monthly income, urbanization level, etc., people with endometriosis are more likely to suffer from mental disorders compared to those without endometriosis (hazard ratio [HR]=2.131; 95% confidence interval [CI]= 1.531– 2.788; p< 0.001). The result illustrated that women over 40 years old had a more significant risk.
Conclusion: Compared to people without endometriosis, this study provides evidence that patients with endometriosis are at a 2.131-fold higher risk of developing mental disorders, especially in elder women. Regular psychiatric follow-up might be needed for those patients.
Keywords: endometriosis, mental disorders, national health insurance research database, cohort study, Taiwan, women
Introduction
Endometriosis is an estrogen-dependent common gynecological disease, characterized by the presence of endometrial tissue in sites other than the uterine cavity.1,2 Estimates of prevalence are approximately 10% in the general population; for women with reduced fertility, the prevalence rate ranges from 25% to 40%.3 Nevertheless, visitation of the disease is required for a diagnosis; for the reason that, these values are potentially underestimated. According to the classification of the American Society for Reproductive Medicine, there are four different stages of endometriosis; stages I and II represent initial stages, while stages III and IV are advanced stages.4,5 The stage of endometriosis is based on the location, amount, depth, and size of the endometriotic foci.4–6 Even though some patients may be asymptomatic, common clinical manifestations may encompass chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, subfertility, and infertility.7–9Due to the range of symptoms, endometriosis is often diagnosed later in the disease process, resulting in delayed treatment, which negatively affects the quality of patients’ life.7,10 The high risk of recurrence is a major challenge for females with endometriosis.3,11 After treatment, the symptomatic recurrence rates of endometriosis have been reported to range from 21.5% at two years to 50% at five years.1,12
Psychiatric, or mental disorders, are defined as being clinically significant behavioral or psychological syndromes, which are associated with present distress, disability, or an increased risk of suffering death, pain, or disability, and subsequent behavioral, psychological, or biological dysfunctions.13,14 Psychiatric disorders are associated with suicide and all-cause mortality.15,16 In our study, mental disorders encompass psychiatric disorders, suicide, and all-cause mortality. In addition, we also analyzed some details covering anxiety, depression, bipolar, sleep disorders, etc.
Previous literature proved that people with endometriosis had an increased risk of anxiety, bipolar disorders, and suicide.12,17,18 Under these circumstances, we hypothesized that endometriosis is associated with mental disorders which include psychiatric disorders, suicide, and all-cause mortality, conducted a nationwide, population-based, cohort study, and utilized the National Health Insurance Research Database (NHIRD). According to recent literature, endometriosis may have a negative impact on patients’ low quality of life as well as psychiatric health, similar to that for chronic pelvic pain.19,20 Simultaneously, pain in endometriosis serve as a risk factor for subsequent psychiatric disorders.20 In the discussion part, we state the association between chronic pelvic pain and subsequent psychiatric disorders. However, there is a lack of study directly utilizing large databases to examine patients with endometriosis and the risk of mental disorders in Taiwan. Therefore, it is needed to verify the association between them.
Materials and Methods
Data Source
In 1995, the National Health Insurance (NHI) program was launched, and it has included contracts with 97% of medical providers with approximately a 23million beneficiaries, or more than 99% of the entire population, as of June 2009.21,22 The NHIRD contains all claims data of the beneficiaries, using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes to record diagnoses.23,24 The details of this program have been documented in a previous study.22
In this study, we used data from the NHIRD to investigate the association between subjects with endometriosis over a 16-year period.25 As a subset of the NHIRD, the Longitudinal Health Insurance Database of a two million randomized sampled population in 2000–2015, was used to study the association between endometriosis and the risk of mental disorders, including psychiatric disorders, suicide, all-cause mortality.26
In this study, we used data from the NHIRD to investigate the association between patients with endometriosis (ICD-9-CM:617) and patients suffering from mental disorders, encompassing all-cause mortality (ICD-9-CM: 800–999), suicide (ICD-9-CM: E950-E959), and psychiatric disorders (ICD-9-CM: 290–319) over a 16-year period, from the total hospitalization Longitudinal Health Insurance Database in Taiwan (2000–2015).
All procedure concerning human participants in this study were carried out in accordance with the Declaration of Helsinki and institutional research council and similar relevant ethical standards. The study was approved by the Institution Review Board of Tri-Service General Hospital at the National Defense Medical Center in Taipei, Taiwan. (TSGH IRB No. B-111-19) Additionally, on account of the regulations in Taiwan, our ethics committee waived the need for informed consent.
Study Design and Sampled Participants
Figure 1 is the flowchart of this study, illustrating the case-screening process (inclusion and exclusion criteria) and the follow-up results, as well as the risk of mental disorders between patients with endometriosis and the reference cohort. After the exclusion criteria took effect, a total of 100,770 participants, encompassing 20,154 in the study group and 80,616 in the comparison group (1:4), were enrolled during the study period (2000–2015). The mental disorders incidence of the endometriosis group is 20.26%; nevertheless, the control group showed mental disorders incidence of 11.44%.
 |
Figure 1 The flowchart of this study. |
This study was of a population-based, matched-cohort design. Patients with newly diagnosed endometriosis were selected from the Longitudinal Health Insurance Database from January 1, 2000, to December 31, 2015. The patients with endometriosis before 2000 were excluded. This method could function as a way to make sure that these diseases were recent-onset with references from other studies for the association between endometriosis and mental disorders, utilizing the NHIRD.27
Additionally, the patients diagnosed with mental disorders (including anxiety, depression, bipolar, sleep disorders, posttraumatic stress disorder (PTSD)/ acute stress disorder (ASD), dementia, eating disorders, substance-related disorders (SRD), psychotic disorders, autism, and other mental disorders) suicide, all-caused mortality, sleep disorders, and psychotic disorders, before 2000, or before their first visit for endometriosis were also excluded.28 A total of the patients who were enrolled, covering 20,154 participants in the study cohort and 80,616 controls without endometriosis, were matched for age and index date.28,29 Each enrolled participant was required to have made at least three outpatient visits or one inpatient episode in the 1-year study period for endometriosis according to these ICD-9-CM codes.29(Table S1)
Covariates
The covariates included age groups (<=19, 20–44, 45–64, ≥65 years), geographical area of residence (north, center, south, and east of Taiwan), urbanization level of residence (levels 1 to 4), and monthly income (in New Taiwan Dollars [NT$]; < 18,000, 18,000–34,999, ≥35,000; approximately 30 New Taiwan Dollars to US dollar). The urbanization level of residence was defined according to the population and various indicators of the level of development.30 Level 1 was defined as a population of > 1,250,000, and a specific designation as political, economic, cultural, and metropolitan development. Level 2 was defined as a population between 500,000 and 1,249,999, and as playing an important role in politics, economy, and culture. Urbanization levels 3 and 4 were defined as a population between 149,999 and 499,999, and <149,999, respectively.31
Major Outcome
All of the study participants were followed from the index date until the onset of, mental disorders (ICD-9-CM: 290–319) (including anxiety (ICD-9-CM: 300), depression (ICD-9-CM: 296.2–296.3, 300.4, 311), bipolar (ICD-9-CM: 296.0, 296.4–296.8), sleep disorders (ICD-9-CM: 307.4, 780.5), PTSD/ASD (ICD-9-CM: 308, 309.81), dementia (ICD-9-CM: 290.0–290.4, 290.8–290.9, 331.0), eating disorders (ICD-9-CM: 307.1, 307.5), SRD (ICD-9-CM: 291–292, 303.3, 303.9, 304–305), psychotic disorders (ICD-9-CM: 295, 297–298), autism (ICD-9-CM: 299.0), and other mental disorders (ICD-9-CM: 290–319 excluding listed above)), suicide (ICD-9-CM: E950-E959), all-cause mortality (ICD-9-CM: 800–999), withdrew from the NHI program, or the end of 2015. In addition, each psychiatric diagnosis was required to have made at least three outpatient visits within the 1-year study period for psychiatric disorders according to these ICD-9-CM codes.27,32
Statistical Analyses
All statistical analyses were performed using the SPSS for Windows, version 22.0 (IBM Corp., Armonk, NY, USA). χ2 and t-tests were used to evaluate the distributions of the categorical and continuous variables, respectively. The results were presented as hazard ratio (HR) with a 95% confidence interval (CI).25 The differences in the risk of subsequent mental disorders between the endometriosis and non-endometriosis cohorts were estimated via the Kaplan-Meier method and Log rank tests. A two-tailed p-value < 0.05 was considered to indicate the statistical significance.32,33
Results
Of a total of 100,770 participants, Kaplan-Meier survival analysis revealed that there was a statistically significant difference in the development of mental disorders, including psychiatric disorders and suicide besides, at the 1st year of follow-up, the difference between the two groups became significant (long-rank, p<0.001) (Figure 2).
 |
Figure 2 Kaplan-Meier for survival of mental disorders among aged 18–49 women stratified by endometriosis with Log rank test. |
The average follow-up period for the diagnosis of endometriosis to mental disorders was 7.21±5.34 years, which is less than the comparison group (7.84±5.80 years). Besides, we also studied the incidence and prevalence of mental disorders among different cohorts (Tables 1 and S2).
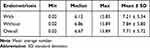 |
Table 1 Years to Mental Disorders |
Table 2 shows age groups, monthly insured premiums, comorbidities, season of medical visits, geographical area of residence, urbanization, level of care, of the study subjects, and controls. The distribution of age, pneumonia, injury, tumor, and season of medical visits between these two groups was not a statistically significant difference. The majority of participants were above 40 (48.55%) for the endometriosis group and the control group. The patients suffering from endometriosis were more likely to live in northern and southern Taiwan and urbanization level 1 and 2, receiving medical care from the hospital centers and regional hospitals, paying the less insured premium. The endometriosis cohort tended to have more diabetes mellitus (DM), hypertension (HTN), renal disease, hyperlipidemia, thyrotoxicosis, chronic liver disease (CLD) than the non-endometriosis control cohort.
 |
Table 2 Characteristics of Study in the Baseline |
Table 3 demonstrated the result of Cox regression analysis of some factors associated with the risk to developmental disorders. The crude HR is 2.978 (95% CI= 2.237–3.865, p<0.001). After adjusting for age, monthly insured premium, comorbidities, season of medical visits, geographical area of residence, and urbanization level of the residence, the adjusted HR is 2.131 (95% CI= 1.531–2.788, p<0.001). For the subgroup aged≥40 of the endometriosis group, the risk of developing mental disorders is 2.251 times higher than the participants aged≤19.
 |
Table 3 Factors of Mental Disorders by Using Cox Regression |
In Table 4, by stratification with age, monthly insured premiums, comorbidities, season of medical visits, urbanization levels, levels of care from medical visits, etc., the risk to develop mental disorders in the endometriosis cohort is higher than the control group. In different urbanization levels, geographic areas of residence, monthly income, levels of care, seasons of visit, the subjects were associated with an increased risk of mental disorders, encompassing psychiatric disorders, suicide, and all-cause mortality.
 |
Table 4 Factors of Mental Disorders Stratified by Variables Listed in the Table by Using Cox Regression |
Table 5 revealed the adjusted HR of suicide with adjusted HR: 1.447, p=0.009, all-cause mortality with adjusted HR: 2.315, p<0.001, psychiatric disorders with adjusted HR: 2.125, p<0.001, depression with adjusted HR: 2.773, p<0.001, anxiety with adjusted HR: 2.494, p<0.001, sleep disorders with adjusted HR: 2.295, p<0.001 in the study cohort, in comparison with participants without endometriosis. Besides, we found a surprising thing that PTSD/ASD was statistically significant on the whole. When the first year was excluded, PTSD/ASD was statistically significant as well. Nevertheless, there is no statistically significant when the first five years were excluded.
 |
Table 5 Factors of Mental Disorders Subgroups by Using Cox Regression |
Discussions
In our study, by using two million NHIRD with the advantage of a large dataset, we investigated the association between endometriosis and mental disorders covering psychiatric disorders, suicide, and all-cause mortality. In our study, we have excluded the patients and controls with psychiatric disorders before the follow-up period. After adjusting for comorbidities and other covariates, the overall adjusted HR was 2.131 (95% CI =1.531–2.788, p<0.001) when compared to the comparison cohort. To put it differently, patients with endometriosis had a 2.1-fold risk of developing mental disorders. Participants with endometriosis are associated with an increased risk of mental disorders, especially in depression and anxiety in this group. As a consequence, a regular psychiatric follow-up might be important for the patients who received endometriosis. The Kaplan–Meier analysis demonstrated that the study group had a significantly higher 16-year mental disorders-free survival rate than the controls.
In our study, mental disorders encompassing psychiatric disorders,34,35 suicide,36,37 and all-cause mortality are associated with endometriosis. Menghan (2020) carried out a cohort study in Sweden, which showed that for those with endometriosis, the adjusted HR of depressive disorders was 1.89, the adjusted HR of anxiety and stress-related disorders was 1.82, and the adjusted HR of bipolar and other affective psychotic disorders was 1.62.38 Another cross-section study in the United States demonstrated that anxiety disorders predominated at 45% in patients with endometriosis, and this was followed by depressive disorders (31.3%).1 By conducting a retrospective matched cohort study in the United States, comparing patients with documented endometriosis to those without, the adjusted HR of anxiety, depression, and self-directed violence were 1.38, 1.48, and 2.03, respectively.12 In the same vein, after adjusting for other factors, the adjusted HR of depression was 2.494, the adjusted HR of anxiety was 2.773 in our study, similar to a previous study, utilizing the NHIRD as well.39 Besides, Chen (2020) claimed that patients with endometriosis were more likely to suffer from bipolar disorders.17 However, further studies are needed to clarify the underlying mechanism. Psychiatric disorders have an association with suicide and all-cause mortality.15,40,41 Previous studies demonstrated the association between endometriosis and suicide. Endometriosis may be a risk factor to increase patients’ suicide ideation.36,42,43 Our study is the first general population-based cohort study to investigate the associations between endometriosis and suicide. In our study, after adjusting for covariates and comorbidities, the adjusted HR of suicide was 1.447. Conversely, Saavalainen (2019) argues that the association between all-cause mortality and endometriosis remains uncertain and is needed to carry out further studies to identify the association.44 Nevertheless, in our study, patients with endometriosis have a 2.315-fold risk for developing all-cause mortality. It is needed to conduct further studies to clarify the underlying mechanisms.
Endometriosis is a risk factor for affecting patients’ psychiatric health.45,46 Mental disorders covering psychiatric disorders, suicide, all-cause mortality were most common in women of reproductive age and from low socioeconomic.5 Due to the repetitive and consistent menstrual cycle, the menstrual cycle could maximize the endometriosis symptoms for reproductive age of women.47 The underlying pathopsychological mechanism of the increased risk of mental disorders in people with endometriosis remains unclarified. The relationship between endometriosis and mental disorders is based on the symptoms of endometriosis.10 Chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, subfertility, and infertility are features of endometriosis.48–50 When estimating the association between endometriosis and psychiatric health, chronic pelvic pain is a critical variable needed to be taken into account, defined as a nonmalignant pain perceived in pelvic areas that is constant or recurs over 6 months.51–53 Psychological factors should be involved, serving as an important factor to affect pain experience in people with endometriosis.35,54 Chronic pain is a well-known mediator of sleep disorders, anxiety, and depression.55,56 Chronic pain also function as a risk factor for suicide and all-cause mortality.18,57 The previous study suggested that psychopathological diseases amplify pain symptoms in patients with endometriosis.54 In this way, patients with psychiatric diseases may influence the severity of chronic pelvic pain, and chronic pelvic pain contributes to worsen psychiatric disorders, which created a vicious circle. The association between dysmenorrhea and stress is bidirectional.58 Experiencing monthly repeated menstrual pain might increase the risk of experiencing psychiatric disorders especially depression and anxiety, or stress and vice versa.58–60 Having these psychiatric disorders may exacerbate the severity of menstrual pain.59,61 Tayyeb (2022) points out that dyspareunia, painful sexual intercourse, affecting approximately 10 to 28% of the population in a lifetime is a common female health problem.62 The previous studies suggested that dyspareunia and dysuria have a significant effect on physical as well as mental health, contributing to depression, anxiety, etc.62–65 Infertility is a common medical condition, leading to mental, psychological, physical detriments to the patients.66,67 According to statistics, up to 30–40% of women who have endometriosis also have a problem with fertility.68 Infertility and associated diagnoses have overall health implications.69 It has been considered as a social stigma, treated as a physically, mentally, socially damaging experience.8,66
Sexuality is a fundamental dimension of human life with critical implications for psychiatry health and global quality of life.70,71 Nevertheless, female sexuality can be influenced by chronic gynecological diseases such as endometriosis.70–72 As demonstrated by several previous studies, women with endometriosis tend to have a more significant risk of deep dyspareunia; additionally, endometriosis is also associated with an increased risk of mental and psychosexual disorders.73–75 Chronic pelvic pain is one of the clinical manifestations of endometriosis which might contribute to the decreasing number of sexual relations.72 Montanari argues that endometriosis-related dyspareunia may lead to less sexual satisfaction and an inability to reach orgasm during intercourse.76 The high prevalence of sexual dysfunctions in women with endometriosis, including potential and ovarian endometriosis and deep infiltrating endometriosis, is alarming. (About two-thirds of women with endometriosis)73,75 Dyspareunia may negatively affect the mental health and psychical health of women.75 Besides, a meta-analysis suggests a bidirectional association between depression and sexual dysfunction.77 However, we do not take sexual dysfunction into consideration in our study.
There are several clinical implications for the knowledge from the knowledge in this study. In the beginning, in this endometriosis group of women, conversation respecting psychiatric disorders, suicide, mortality should be included into the daily care. Providing a platform is necessary for those women who worsens the psychological disorder owing to pain perception. Additionally, for those with endometriosis, routine and active screening for psychiatric disorders could facilitate in diagnosis and manage the potential underlying psychological illness processes which could influence the quality of health, life, and social. Furthermore, both physical symptoms and emotion regulation difficulties should be incorporated into the therapy alternatives. In comparison with women without endometriosis, the significant presence of psychiatric disorders in women with endometriosis reveals that the association between endometriosis and mental disorders should be emphasized rather than consider subsequent psychiatric disorders as a common occurrence.
The strengths of this study encompass the following reasons. First of all, one of the primary strengths is the use of a database with a large, nationwide cohort of insured individuals. Besides, we have the ability to adjust for lots of potential confounders, and the implementations of multiple sensitive analyses contributing to increase the confidence in the results. Furthermore, for the first time, utilizing the large, nationwide database, we conducted a cohort study to examine the association between endometriosis and mental disorders including psychiatric disorders, suicide, all-cause mortality.
There are several limitations to this study. In the beginning, patients with endometriosis could be identified by the NHIRD; however, data on severity and impact were not available. Second, the previous study demonstrated that women with higher education levels were more likely to understand endometriosis and have recourse to a specialist for their endometriosis.67,78 Although we took other socioeconomic such as urbanization levels, geographic areas of residence, and monthly insured premium into consideration, potential selection bias could exist due to the difference in education levels. Third, other confounding factors, such as genetic, environmental, diet factors are also not encompassed in the NHIRD. Fourth, as there are no images or other laboratory data recorded in the NHIRD, we could only base on the professional diagnosis for mental disorders covering psychiatric disorders, suicide, and all-cause mortality. Fifth, endometriosis is often diagnosed later; hence, it is possible that mental disorders occurred before people with endometriosis were diagnosed.10,79 Nevertheless, in our study, that cases would be removed, which may contribute to potential bias. Sixth, the NHI program started in 1995; nonetheless, in our study, the data we used contained only a database of 16 years. Seventh, because of the use of NHIRD, there is a lack of stratified analysis to investigate the association between the different treatment of endometriosis and mental disorders. Eighth, although sexual dysfunction may negatively impact on subsequent psychiatric disorders, this factor is not taken into account in this study. Finally, this result is only limited to Taiwan, not necessarily representing other nations or regions.
Conclusions
In conclusion, the present study was designed to determine the association between endometriosis and mental disorders, including psychiatric disorders and suicide, especially in elder females. These experiments confirmed that endometriosis may be a risk factor for mental disorders by multiple regression analysis. Women with endometriosis were nearly twofold inclined to develop mental disorders. This project is the first comprehensive investigation to examine the association between endometriosis and mental disorders; nevertheless, the study was limited by the absence of the data from other nations and regions. We recommend that Health Promotion Administration complete of scales, advocate, and form the medical policies for the physical and mental health of women.
Data Sharing Statement
Data are available from the National Health Insurance Research Database (NHIRD) published by the Taiwan National Health Insurance (NHI) Administration; nevertheless, data cannot be made publicly available due to legal restrictions imposed by the government of Taiwan under the “Personal Information Protection Act”. Requests for data can be sent as a formal proposal to the NHIRD (http://www.mohw.gov.tw).
Institutional Review Board Statement
The study was carried out in accordance with the Declaration of Helsinki’s and was approved by the Institution Review Board of Tri-Service General Hospital at the National Defense Medical Center in Taipei, Taiwan. (TSGH IRB No. B-111-19).
Acknowledgments
The National Health Insurance Research Database was provided by the Health and Welfare Data Science Center, Ministry of Health and Welfare (HWDC, MOHW), Taiwan (NHIRD).
Funding
The study was supported by the Medical Affairs Bureau, the Ministry of Defense of Taiwan (MND-MAB-D–111134), the Tri-Service General Hospital Research Foundation (TSGH-B-112020; TSGH-A-112003), and by research grants from the Chi Mei Medical Center (CMNDMC10208; CMNDMC10304), and the sponsor has no role in study design, data collection and analysis, preparation of the manuscript, and decision to publish.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Robert CA, Caraballo-Rivera EJ, Isola S, et al. Demographics and hospital outcomes in American women with endometriosis and psychiatric comorbidities. Cureus. 2020;12(8):e9935. doi:10.7759/cureus.9935
2. Mehedintu C, Plotogea MN, Ionescu S, Antonovici M. Endometriosis still a challenge. J Med Life. 2014;7(3):349–357.
3. Brown J, Farquhar C. Endometriosis: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2014;2014(3):Cd009590. doi:10.1002/14651858.CD009590.pub2
4. Laganà AS, La Rosa VL, Rapisarda AMC, et al. Anxiety and depression in patients with endometriosis: impact and management challenges. Int J Women's Health. 2017;9:323–330. doi:10.2147/ijwh.S119729
5. Society for Reproductive Medicine A. Revised American society for reproductive medicine classification of endometriosis: 1996. Fertil Steril. 1997;67(5):817–821. doi:10.1016/s0015-0282(97)81391-x
6. Haas D, Shebl O, Shamiyeh A, Oppelt P. The rASRM score and the Enzian classification for endometriosis: their strengths and weaknesses. Acta Obstet Gynecol Scand. 2013;92(1):3–7. doi:10.1111/aogs.12026
7. Colette S, Donnez J. Endometriosis. N Engl J Med. 2009;360(18):1911–1912. doi:10.1056/NEJMc090328
8. Gruber TM, Mechsner S. Pathogenesis of endometriosis: the origin of pain and subfertility. Cells. 2021;10(6):1381. doi:10.3390/cells10061381
9. Greene AD, Lang SA, Kendziorski JA, Sroga-Rios JM, Herzog TJ, Burns KA. Endometriosis: where are we and where are we going? Reproduction. 2016;152(3):R63–R78. doi:10.1530/rep-16-0052
10. Bulun SE, Yilmaz BD, Sison C, et al. Endometriosis. Endocr Rev. 2019;40(4):1048–1079. doi:10.1210/er.2018-00242
11. Falcone T, Flyckt R. Clinical management of endometriosis. Obstet Gynecol. 2018;131(3):557–571. doi:10.1097/aog.0000000000002469
12. Estes SJ, Huisingh CE, Chiuve SE, Petruski-Ivleva N, Missmer SA. Depression, anxiety, and self-directed violence in women with endometriosis: a Retrospective Matched-Cohort Study. Am J Epidemiol. 2021;190(5):843–852. doi:10.1093/aje/kwaa249
13. Stein DJ, Phillips KA, Bolton D, Fulford KW, Sadler JZ, Kendler KS. What is a mental/psychiatric disorder? From DSM-IV to DSM-V. Psychol Med. 2010;40(11):1759–1765. doi:10.1017/s0033291709992261
14. Happé F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child Adolesc Psychiatry. 2011;50(6):540–542. doi:10.1016/j.jaac.2011.03.015
15. Wasserman D, Carli V, Iosue M, Javed A, Herrman H. Suicide prevention in psychiatric patients. Asia Pac Psychiatry. 2021;13(3):e12450. doi:10.1111/appy.12450
16. Ojansuu I, Putkonen H, Tiihonen J. Mortality among forensic psychiatric patients in Finland. Nord J Psychiatry. 2015;69(1):25–27. doi:10.3109/08039488.2014.908949
17. Chen SF, Yang YC, Hsu CY, Shen YC. Risk of bipolar disorder in patients with endometriosis: a nationwide population-based cohort study. J Affect Disord. 2020;270:36–41. doi:10.1016/j.jad.2020.03.047
18. Racine M. Chronic pain and suicide risk: a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):269–280. doi:10.1016/j.pnpbp.2017.08.020
19. Kalfas M, Chisari C, Windgassen S. Psychosocial factors associated with pain and health-related quality of life in endometriosis: a systematic review. Eur J Pain. 2022;26(9):1827–1848. doi:10.1002/ejp.2006
20. Muharam R, Amalia T, Pratama G, et al. Chronic pelvic pain in women with endometriosis is associated with psychiatric disorder and quality of life deterioration. Int J Women's Health. 2022;14:131–138. doi:10.2147/ijwh.S345186
21. Ho Chan WS. Taiwan’s healthcare report 2010. EPMA J. 2010;1(4):563–585. doi:10.1007/s13167-010-0056-8
22. Lin LY, Warren-Gash C, Smeeth L, Chen PC. Data resource profile: the National Health Insurance Research Database (NHIRD). Epidemiol Health. 2018;40:e2018062. doi:10.4178/epih.e2018062
23. Hsieh CY, Su CC, Shao SC, et al. Taiwan’s national health insurance research database: past and future. Clin Epidemiol. 2019;11:349–358. doi:10.2147/clep.S196293
24. Tzeng NS, Chung CH, Lin FH, et al. Risk of dementia in adults with ADHD: a Nationwide, Population-Based Cohort Study in Taiwan. J Atten Disord. 2019;23(9):995–1006. doi:10.1177/1087054717714057
25. Chien WC, Chung CH, Lin FH, et al. The risk of injury in adults with attention-deficit hyperactivity disorder: a nationwide, matched-cohort, population-based study in Taiwan. Res Dev Disabil. 2017;65:57–73. doi:10.1016/j.ridd.2017.04.011
26. Chao PC, Chien WC, Chung CH, et al. Pinworm infections associated with risk of psychiatric disorders-A nationwide cohort study in Taiwan: pinworm infections and psychiatric disorders. Compr Psychiatry. 2019;93:14–19. doi:10.1016/j.comppsych.2019.02.002
27. Yeh TC, Chien WC, Chung CH, et al. Psychiatric disorders after traumatic brain injury: a Nationwide Population-Based Cohort Study and the effects of rehabilitation therapies. Arch Phys Med Rehabil. 2020;101(5):822–831. doi:10.1016/j.apmr.2019.12.005
28. Tzeng NS, Yeh HW, Chung CH, et al. Risk of psychiatric morbidity in psychosexual disorders in male patients: a Nationwide, Cohort Study in Taiwan. Am J Mens Health. 2019;13(2):1557988319842985. doi:10.1177/1557988319842985
29. Tzeng NS, Chung CH, Lin FH, et al. Anti-herpetic medications and reduced risk of dementia in patients with herpes simplex virus infections-a Nationwide, Population-Based Cohort Study in Taiwan. Neurotherapeutics. 2018;15(2):417–429. doi:10.1007/s13311-018-0611-x
30. Shi Y, Zhu Q, Xu L, et al. Independent or influential? Spatial-temporal features of coordination level between urbanization quality and urbanization scale in China and its driving mechanism. Int J Environ Res Public Health. 2020;17(5):1587. doi:10.3390/ijerph17051587
31. Kung LY, Li TI, Chung CH, et al. Risk of depression in patients with oral cancer: a nationwide cohort study in Taiwan. Sci Rep. 2021;11(1):23524. doi:10.1038/s41598-021-02996-4
32. Wan FJ, Chien WC, Chung CH, Yang YJ, Tzeng NS. Association between traumatic spinal cord injury and affective and other psychiatric disorders-a nationwide cohort study and effects of rehabilitation therapies. J Affect Disord. 2020;265:381–388. doi:10.1016/j.jad.2020.01.063
33. Huang JL, Chen WK, Lin CL, Kao CH, Shih HM. Preeclampsia and the risk of pancreatitis: a Nationwide, Population-Based Cohort Study. Gastroenterol Res Pract. 2020;2020:3261542. doi:10.1155/2020/3261542
34. Škegro B, Bjedov S, Mikuš M, et al. Endometriosis, pain and mental health. Psychiatr Danub. 2021;33(Suppl 4):632–636.
35. Facchin F, Barbara G, Saita E, et al. Impact of endometriosis on quality of life and mental health: pelvic pain makes the difference. J Psychosom Obstet Gynaecol. 2015;36(4):135–141. doi:10.3109/0167482x.2015.1074173
36. Tulandi T. Endometriosis and pelvic pain awareness: infertility, suicidal ideation, and cancer. J Obstet Gynaecol Can. 2021;43(5):543–544. doi:10.1016/j.jogc.2021.03.001
37. Lee SM, Park JK. Dienogest-induced major depressive disorder with suicidal ideation: a case report. Medicine. 2021;100(40):e27456. doi:10.1097/md.0000000000027456
38. Gao M, Koupil I, Sjöqvist H, et al. Psychiatric comorbidity among women with endometriosis: nationwide cohort study in Sweden. Am J Obstet Gynecol. 2020;223(3):415.e1–415.e16. doi:10.1016/j.ajog.2020.02.033
39. Chen LC, Hsu JW, Huang KL, et al. Risk of developing major depression and anxiety disorders among women with endometriosis: a longitudinal follow-up study. J Affect Disord. 2016;190:282–285. doi:10.1016/j.jad.2015.10.030
40. Appleby L. Suicide in psychiatric patients: risk and prevention. Br J Psychiatry. 1992;161(6):749–758. doi:10.1192/bjp.161.6.749
41. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi:10.1001/jamapsychiatry.2014.2502
42. Soliman AM, Rahal Y, Robert C, et al. Impact of endometriosis on fatigue and productivity impairment in a cross-sectional survey of Canadian women. J Obstet Gynaecol Can. 2021;43(1):10–18. doi:10.1016/j.jogc.2020.06.022
43. Calati R, Laglaoui Bakhiyi C, Artero S, Ilgen M, Courtet P. The impact of physical pain on suicidal thoughts and behaviors: meta-analyses. J Psychiatr Res. 2015;71:16–32. doi:10.1016/j.jpsychires.2015.09.004
44. Saavalainen L, But A, Tiitinen A, et al. Mortality of midlife women with surgically verified endometriosis-a cohort study including 2.5 million person-years of observation. Hum Reprod. 2019;34(8):1576–1586. doi:10.1093/humrep/dez074
45. Delanerolle G, Ramakrishnan R, Hapangama D, et al. A systematic review and meta-analysis of the endometriosis and mental-health sequelae; The ELEMI project. Women's Health. 2021;17:17455065211019717. doi:10.1177/17455065211019717
46. Facchin F, Barbara G, Dridi D, et al. Mental health in women with endometriosis: searching for predictors of psychological distress. Hum Reprod. 2017;32(9):1855–1861. doi:10.1093/humrep/dex249
47. Bhimanadham NN, Mainali P, Robert CA, et al. Hospital outcomes in antepartum mental disorders: a Study on 897,397 pregnant inpatients. Behav Sci. 2019;9(10). doi:10.3390/bs9100105
48. Sachedina A, Todd N. Dysmenorrhea, endometriosis and chronic pelvic pain in adolescents. J Clin Res Pediatr Endocrinol. 2020;12(Suppl 1):7–17. doi:10.4274/jcrpe.galenos.2019.2019.S0217
49. Tanbo T, Fedorcsak P. Endometriosis-associated infertility: aspects of pathophysiological mechanisms and treatment options. Acta Obstet Gynecol Scand. 2017;96(6):659–667. doi:10.1111/aogs.13082
50. Vercellini P, Buggio L, Frattaruolo MP, Borghi A, Dridi D, Somigliana E. Medical treatment of endometriosis-related pain. Best Pract Res Clin Obstet Gynaecol. 2018;51:68–91. doi:10.1016/j.bpobgyn.2018.01.015
51. Speer LM, Mushkbar S, Erbele T. Chronic pelvic pain in women. Am Fam Physician. 2016;93(5):380–387.
52. Adamian L, Urits I, Orhurhu V, et al. A comprehensive review of the diagnosis, treatment, and management of urologic chronic pelvic pain syndrome. Curr Pain Headache Rep. 2020;24(6):27. doi:10.1007/s11916-020-00857-9
53. Fall M, Baranowski AP, Elneil S, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010;57(1):35–48. doi:10.1016/j.eururo.2009.08.020
54. Cavaggioni G, Lia C, Resta S, et al. Are mood and anxiety disorders and alexithymia associated with endometriosis? A preliminary study. Biomed Res Int. 2014;2014:786830. doi:10.1155/2014/786830
55. Haack M, Simpson N, Sethna N, Kaur S, Mullington J. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology. 2020;45(1):205–216. doi:10.1038/s41386-019-0439-z
56. Siqueira-Campos VME, Da Luz RA, de Deus JM, Martinez EZ, Conde DM. Anxiety and depression in women with and without chronic pelvic pain: prevalence and associated factors. J Pain Res. 2019;12:1223–1233. doi:10.2147/jpr.S195317
57. Smith D, Wilkie R, Uthman O, Jordan JL, McBeth J. Chronic pain and mortality: a systematic review. PLoS One. 2014;9(6):e99048. doi:10.1371/journal.pone.0099048
58. Pakpour AH, Kazemi F, Alimoradi Z, Griffiths MD. Depression, anxiety, stress, and dysmenorrhea: a protocol for a systematic review. Syst Rev. 2020;9(1):65. doi:10.1186/s13643-020-01319-4
59. Hu Z, Tang L, Chen L, Kaminga AC, Xu H. Prevalence and risk factors associated with primary dysmenorrhea among Chinese female university students: a Cross-sectional Study. J Pediatr Adolesc Gynecol. 2020;33(1):15–22. doi:10.1016/j.jpag.2019.09.004
60. Brasil DL, Montagna E, Trevisan CM, et al. Psychological stress levels in women with endometriosis: systematic review and meta-analysis of observational studies. Minerva Med. 2020;111(1):90–102. doi:10.23736/s0026-4806.19.06350-x
61. Ambresin AE, Belanger RE, Chamay C, Berchtold A, Narring F. Body dissatisfaction on top of depressive mood among adolescents with severe dysmenorrhea. J Pediatr Adolesc Gynecol. 2012;25(1):19–22. doi:10.1016/j.jpag.2011.06.014
62. Tayyeb M, Gupta V. Dyspareunia. In: StatPearls. StatPearls Publishing LLC; 2022.
63. Seehusen DA, Baird DC, Bode DV. Dyspareunia in women. Am Fam Physician. 2014;90(7):465–470.
64. Mehta P, Leslie SW, Reddivari AKR. Dysuria. In: StatPearls. StatPearls Publishing LLC; 2022.
65. Michels TC, Sands JE. Dysuria: evaluation and differential diagnosis in adults. Am Fam Physician. 2015;92(9):778–786.
66. Hanson B, Johnstone E, Dorais J, Silver B, Peterson CM, Hotaling J. Female infertility, infertility-associated diagnoses, and comorbidities: a review. J Assist Reprod Genet. 2017;34(2):167–177. doi:10.1007/s10815-016-0836-8
67. Zhou Z, Zheng D, Wu H, et al. Epidemiology of infertility in China: a population-based study. BJOG. 2018;125(4):432–441. doi:10.1111/1471-0528.14966
68. Hodgson RM, Lee HL, Wang R, Mol BW, Johnson N. Interventions for endometriosis-related infertility: a systematic review and network meta-analysis. Fertil Steril. 2020;113(2):374–382.e2. doi:10.1016/j.fertnstert.2019.09.031
69. Sharma RS, Saxena R, Singh R. Infertility & assisted reproduction: a historical & modern scientific perspective. Indian J Med Res. 2018;148(Suppl):S10–S14. doi:10.4103/ijmr.IJMR_636_18
70. Giudice LC. Clinical practice. Endometriosis. N Engl J Med. 2010;362(25):2389–2398. doi:10.1056/NEJMcp1000274
71. Sajdlova R, Fiala L. Psychological hallmarks of endometriosis with emphasis on sexual dysfunction, stress, anxiety and depression. Eur Psychiatry. 2023;66(S1):S646–S647. doi:10.1192/j.eurpsy.2023.1345
72. Porpora MG, Koninckx PR, Piazze J, Natili M, Colagrande S, Cosmi EV. Correlation between endometriosis and pelvic pain. J Am Assoc Gynecol Laparosc. 1999;6(4):429–434. doi:10.1016/s1074-3804(99)80006-1
73. La Rosa VL, De Franciscis P, Barra F, et al. Sexuality in women with endometriosis: a critical narrative review. Minerva Med. 2020;111(1):79–89. doi:10.23736/s0026-4806.19.06299-2
74. La Rosa VL, Barra F, Chiofalo B, et al. An overview on the relationship between endometriosis and infertility: the impact on sexuality and psychological well-being. J Psychosom Obstet Gynaecol. 2020;41(2):93–97. doi:10.1080/0167482x.2019.1659775
75. Barbara G, Facchin F, Buggio L, et al. What is known and unknown about the association between endometriosis and sexual functioning: a systematic review of the literature. Reprod Sci. 2017;24(12):1566–1576. doi:10.1177/1933719117707054
76. Vercellini P, De Giorgi O, Mosconi P, Stellato G, Vicentini S, Crosignani PG. Cyproterone acetate versus a continuous monophasic oral contraceptive in the treatment of recurrent pelvic pain after conservative surgery for symptomatic endometriosis. Fertil Steril. 2002;77(1):52–61. doi:10.1016/s0015-0282(01)02951-x
77. Fiala L, Lenz J, Bob P. Effect of psychosocial trauma and stress on sexual dysfunction in women with endometriosis. Medicine. 2021;100(31):e26836. doi:10.1097/md.0000000000026836
78. Szymańska J, Dąbrowska-Galas M. An assessment of Polish women’s level of knowledge about endometriosis: a pilot study. BMC Women's Health. 2021;21(1):404. doi:10.1186/s12905-021-01556-2
79. Kiesel L, Sourouni M. Diagnosis of endometriosis in the 21st century. Climacteric. 2019;22(3):296–302. doi:10.1080/13697137.2019.1578743
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
