Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Assessment of Quality of Diabetic Care in Teaching Hospitals in Ethiopia: In Comparison to International Guidelines
Authors Akale M , Tadesse T , Arega B
Received 27 October 2023
Accepted for publication 2 February 2024
Published 9 February 2024 Volume 2024:17 Pages 691—700
DOI https://doi.org/10.2147/DMSO.S441764
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Mengesh Akale,1 Tirhas Tadesse,2 Balew Arega1
1Department of Internal Medicine, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia; 2Department of Public Health, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia
Correspondence: Mengesh Akale, Email [email protected]
Background: Comprehensive high quality of care is critical in preventing diabetic complications and improving quality of life. This needs compliance with guidelines and focused therapy. There is no data in Ethiopia evaluating the quality of diabetes care using standard guidelines (American diabetic association and international diabetic federation) as a reference.
Methods: A cross-sectional study was conducted at Yekatit 12 Hospital Medical College (YHMC) to assess the process and outcome quality indicators of diabetic patients. Data were collected from outpatient clinics between May and July 2022 over a period of 3 months. Diabetic patients with at least one year since diagnosis were selected using systematic random sampling. Both the process and outcome of diabetic quality care indicators were measured and compared with standard guidelines (ADA and IDF). Both descriptive statistics and logistic regression were used for data analysis. The P-value < 0.05 was used as statistical significance.
Results: About 250 diabetic patients with a mean age of 53± 15 were included. The majority were type 2 diabetes mellitus (83.2%). HbA1c was determined for 128 (51.2%) patients with the recent mean value of 8± 1.6. Only 52 (40.6%) of patients achieved target HbA1c. Annual comprehensive feet examination, urine albuminuria test, and retinal examination were done for 54 (21.6%), 52 (20.8%), and 122 (48.8%), respectively. Single marital status (AOR = 5.76; 95% CI; 1.02– 32.36) P = 0.047, determining HbA1c level at least twice a year (AOR = 6.27; 95% CI; 2.18– 17.73) P = 0.001, and medication adherence (AOR = 7.1; 95% CI; 2.61– 19.01)P = 0.001, were significantly associated with good glycemic control.
Conclusion: The overall quality of diabetic care was found suboptimal both in process and outcome quality indicators. Thus, awareness creation about quality indicators for caregivers, compliance with guidelines, wise resource utilization, and cooperation with different stakeholders like hospital management teams, and government officials is needed.
Keywords: quality care, process and outcome indicators, diabetes mellitus, glycemic control
A Letter to the Editor has been published for this article.
Introduction
Diabetes mellitus (DM) is a chronic metabolic disease that can lead to a major cause of blindness, kidney failure, heart attacks, stroke, and lower limb amputation.1 DM is becoming a huge burden, affecting 422 million people globally, the majority of whom live in low- and middle-income countries, and it is directly responsible for the deaths of 1.5 million people per year.1–3 Poor quality of care is strongly associated with considerable diabetic-related mortality and costs of US$ 1.4–1.6 trillion in low- and middle-income countries each year.4 Optimizing diabetic good quality care has a paramount role in reducing diabetic-related complications, mortality, national expenditure, and overall quality of life.5
Donabedian proposed that one could assess whether high-quality care is provided by examining the structure in which care is provided, measuring the actual process of care, and assessing the outcomes of care.6 Comprehensive diabetes management, which includes focused guidelines-based treatment, lifestyle change, patient education, and influences on patients’ self-care behavior, can improve DM quality of care. However, regardless of a country’s degree of development or healthcare system, the quality of diabetic care remains inadequate worldwide.7 There is a room for improvement in quality performance indicators and considered as the main focus in the modern era.8,9
According to the international diabetic federation (IDF) in 2017, Ethiopia had 2.57 million (5.2%) adult people aged 20–79 years with diabetes, making it the largest diabetes population in sub-Saharan Africa. Systematic review shows the prevalence of diabetes mellitus in Ethiopia ranged from 2.0% to 6.5%, with significant diabetic complications. The most common reported diabetic complications are retinopathy (2.7–25%), neuropathy (4.8–35%), kidney disease (18.2–23.2%), hypertension (23–54.8%) and depression (13–61%).10
Despite Ethiopia’s high diabetes burden with significant morbidity and mortality, there is a shortage of data evaluating diabetic patients’ quality of care about internationally referenced and commonly used diabetic management recommendations. As a result, this study aimed to assess the proportion of diabetic patients treated according to international diabetic management guidelines, as well as to identify potential factors influencing the quality of care.
Materials and Methods
A cross-sectional study was conducted at Yekatit 12 Hospital Medical College (YHMC). YHMC is a teaching governmental hospital in Addis Ababa, the capital city of Ethiopia. It serves around 230,000 people annually both in the emergency and outpatient departments. Diabetes care is provided by 15 general practitioners, 35 internal medicine residents, 19 internists, and one endocrinologist. The study was conducted from May to July 2022. The study included all adult (>18 years) diabetic patients who had been followed in outpatient clinics for at least 12 months; however, it excluded patients with gestational diabetes mellitus and patients diagnosed with diabetes mellitus within the recent one year.
The sample size was calculated using the single population proportion approach, based on previous research at Tikur Anbesa Hospital, which found that 26.2% of patients had satisfactory glycemic control (HbA1c < 7%).11 After taking into account a 10% nonresponse rate, the final sample size was 250 patients. All eligible patients who agreed to take part in the study were selected using a systematic random sampling technique. The sample was taken every 4(K) values from the sampling frame among 952 diabetic patients registered on the follow-up sheet in the study period.
The data was collected using content and language-validated structured questionnaires. It was modified from the previous studies.8 Patients were asked about demographics, medicine adherence, lifestyle, and other factors in the private room. Clinical data including medication lists, lab results (HbA1c, renal function test, urine analysis, lipid profile, etc), comorbidities, blood pressure, and diabetes complications (Retinopathy, Neuropathy, Nephropathy, stroke, etc) were retrieved from the patient’s medical record. Medical interns and residents conducted both the interviews and the record reviews.
Measurement of Outcome and Process Variables
This study assessed the quality of diabetic care in two ways. As outcome variables, the achievement of the desired glycated hemoglobin level (HbA1c) was used. In addition, process variables that assess clinical patient evaluation and regular screening for complications were used. All of these variables’ definitions and target levels are based on the most recent publication of the American Diabetes Association (ADA)12 and the International Diabetic Federation (IDF).13 In this study, patients with HbA1c less than 7 are considered to have well-controlled diabetes. The patient who took oral hypoglycemic drugs or insulin daily for 7 days/week without missing was considered adherent to medication. Systolic blood pressure of less than 130mmhg and Diastolic blood pressure of less than 80mmhg were taken as well controlled.12 Supplement 1 contains operational definitions for the variables chosen.
Data Analysis
The data were entered, coded, cleaned, and analyzed using the SPSS window program version 25. Descriptive statistics were done to calculate the frequency, percentage, mean, and range. Bivariate and multivariate analyses were utilized in finding factors linked with the outcome variable. A variable with a P -a value <0.25 in the bivariate logistic regression was used in the multivariate regression. An odds ratio with a 95% confidence interval was used to determine the existence, strength, and direction of the relationship between the independent and the outcome variable when P-values were less than 0.05, which was considered statistically significant.
Results
Socio-Demographic Variables
About 250 patients were included in the study, and 141 (56.4%) of them were female. The mean age was 53 (SD±15). Of the total participants, 144 (57.6%) were married, 98 (39.2%) attended secondary school, and 82 (32.8%) worked in a private setting. Table 1 provides the sociodemographic details of the study participants.
 |
Table 1 Socio-Demographic Characteristics of Diabetic Patients in Yekatit 12 Hospital, Addis Ababa |
Comorbidities and Medications of Diabetic Patients
Type II diabetes Mellitus accounted for 208 (80.32%) and the remaining 42 (16.8%) were type 1 diabetes Mellitus. One hundred and three (41.2%) patients have a family history of DM. Of the total participants, 168 (64.2%) had been diabetic for more than five years, 161 (64.4%) were involved in regular exercise, 77 (30.8%) had an alcoholic history and 168 (67.2%) had comorbidities. Most of the patients were on metformin (63.2%), insulin (55.9%), and metformin and insulin combination (19.2%) therapy. We present the detailed comorbidities and medications used in Table 2.
 |
Table 2 Comorbidities and Medications Used Among Adult Diabetic Patients at Yekatit 12 Hospital Medical College, Addis Ababa |
Diabetic Quality Care for Process and Outcome Indicators
Blood pressure was checked on 247 (98.8%) of the patients at each appointment. One hundred and thirty-three (53.2%) had SBP of <130 and 123 (49.2%) had DBP of <80. The most prevalent diabetic complication was neuropathy, which made up 68 (27.2%) of all reported cases. Clinical and laboratory parameters used to assess the quality of diabetic care are depicted in Supplement 2.
HbA1c was measured in 128 (51.2%) diabetic patients over the course of a year, with 43 (33.6%) having it measured twice. The mean HbA1c level was 8 ±1.6.
Among those with known HbA1c levels, 52 (40.6%) had good glycemic control, while 76 (59.4%) had uncontrolled diabetes. Figure 1 illustrates the Hb1AC levels. In the past year, 54 (21.6%) patients had yearly foot exams, 122 (48.8%) eye examinations, and 190 (76%) had serum creatinine determined. The majority, 222 (81.6%), had no lipid profile in one year. Process and outcome indicators are summarized in Table 3.
 |
Table 3 Result of Diabetic Quality of Care Indicator as Referenced to the International Guideline, Yekatit 12 Hospital, Addis Ababa |
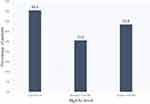 |
Figure 1 Level of HbA1c level among diabetic patient, Yekatit 12 Hospital, May–July 202. |
Factors That Can Affect Outcome Indicator
Bivariate regression was initially used to examine potential influences on diabetic control, including sociodemographic traits, types and duration of diabetes mellitus, alcohol and smoking histories, regular physical activity, drug adherence, and frequency of HbA1C measurement. Accordingly, it found that single marital status, doing exercise, taking medications as prescribed, and frequent HbA1c measurements were significantly associated with maintaining diabetic control (Table 4).
 |
Table 4 Bivariate and Multivariate Logistic Regression Analysis of Factors Associated with Glycemic Control Among Diabetic Patients in Yekatit 12 Hospital, Addis Ababa |
Single marital status, medication adherence, and frequency of hemoglobin A1C testing were all significantly associated with good HbA1c control in the multivariate logistic regression model. Being Single was associated with good glycemic control (AOR = 5.76; 95% CI; 1.02–32.36) p = 0.047. Checking of HgA1c level at least twice per year was 6.27 times more likely to have controlled diabetes (AOR = 6.27; 95% CI; (2.17–17.73) p = 0.001). A person’s chance of achieving adequate glucose control was 7.11 times higher if they are adherent to medication (COR = 7.11; 95% CI; 2.61–19.01) p = 0.001 (Table 4).
Discussion
Implementing high-quality care is crucial to a patient outcome, which necessitates adherence to international guidelines and looking to best practices in other countries or institutions. Continuous evaluation and research about what is currently being done and what needs to be improved are necessary to boost the level of care.
The main aim of this study was to assess the quality of diabetic care using referenced guidelines and to investigate factors that influence glycemic control. Accordingly, the finding revealed that 59.4% of study participants had uncontrolled diabetes, which is nearly comparable to studies from Kuwait (55%)14 and USA (50.2%)15 but lower than many other studies conducted in Tikur Anbesa Hospital (73.8%),11 70.8% in Northeast Ethiopia,16 Saudi Arabia (74.9%),17 and, Uganda (73.52%).18 However, it is higher than the study conducted in Eastern Ethiopia (45.2%),19 and Qatar (35.5%).20 This difference might be associated with the definition, the study population, the study setting, and the availability of experts, particularly endocrinologists and diabetologists. HbA1c level can falsely high in low turnover anemia (Vitamin B12 or folate deficiency) or falsely low with increased red blood cell turnover, such as sickle cell disease, glucose-6-phosphate dehydrogenase deficiency, hemodialysis, recent blood loss or transfusion, or erythropoietin therapy.12 Furthermore, the amount of HbA1c may vary between laboratories because they use assays that are not recognized by the “National Glycohemoglobin Standardization Programme (NGSP)”, which delivers falsely high or low readings in persons with hemoglobin variants.
In our study, nearly half of diabetes mellitus patients (51.2%) had their Hb1Ac levels tested at least once a year, which is significantly lower than the results of comparable studies in Kuwait (63%)14 and Switzerland (90%).21 However, only one-third (33.6%) of patients had their Hb1Ac measured twice a year, as recommended by the ADA. This is lower than the study done in Australia,22 where half of diabetic individuals (50%) had their Hb1Ac measured twice a year. This substantial gap could be attributed to the scarcity of resources, financial constraints, lack of medical insurance to cover investigation costs, lack of commitment to update the investigation as per guidelines, or poor documentation by care givers.
In terms of risk screening, 21.6% of diabetic patients had an annual foot examination. This is lower than the results of a similar study conducted in Australia (68%),22 and Qatar (89.6%).20 It could be because there is no specialized foot clinic and the patient burden per physician to undertake a comprehensive foot examination. In this study, annual screening for urine microalbuminuria and retinal examination was 20.8% and 48.8%, respectively. The retinal examination was better than the result from Japan (35.5%)23 but still far behind those from the United States (73.4%),15 Qatar (72.3%),20 and European nations (74.8%).24
Nephropathy screening was reported low in Kuwait14 and Japan23 consistent with this study and high performance in the UK (75.6%).25 This disparity may be due to differences in the healthcare system. The presence of full health insurance coverage in Western countries may provide favorable conditions even expensive investigations could be done. In addition, the lower rate of risk screening in our study may be in part due to the lack of certain laboratory tests like HbA1c and 24-hour urine protein.
Checking HbA1c at least twice per year, medication adherence, and being single all showed a statistically significant relationship with controlled diabetes. The majority of single people in this study are younger, adhere to medications, and have type 1 diabetes. Aside from high adherence, young people are more likely to engage in lifestyle changes such as exercise, which has a significant impact on glycemic control. Contrary to earlier research conducted in Egypt,26 some factors like education level, certain lifestyles (smoking, exercise), and duration of diabetes did not demonstrate statistically significant association with glycemic control.
This is the first study in Ethiopia to assess the quality of diabetic care using Donabedian quality assessment tools. This tries to assess the actual practices compare it with international guidelines and determine both process and outcome variables. However, the findings of this study should be interpreted with caution given that significant participants had unknown HbA1c status (48.8%). This might underestimate or overestimate our current findings. This unknown Hb1Ac might be due to two conditions. First, the HbA1c might not be conducted. Second, the HbA1c which is usually done outside of the hospital might not be documented by the attending physician.
Conclusion
This study revealed that both process quality (frequency of HbA1c determination, screening for nephropathy, retinopathy and neuropathy) and outcome quality indicator (glycemic control) at Yekatit 12 teaching Hospital are unsatisfactory. Despite current advanced diagnostic and therapeutic options, providing the required quality of care for diabetic patients remains a challenge. Possible reasons for such poor performances might be clinical inertia to intensify treatment, poor guideline adherence, or lack of resources. Thus, awareness creation about quality indicators for healthcare providers and compliance with international or national guidelines has a paramount role for quality improvement. Furthermore, wise resource allocation and utilization help for sustainable availability of investigation like HbA1c, renal function test, urine analysis, and lipid profile. Healthcare professionals and other stakeholders must work together to maintain and improve care quality, which reduces disease morbidity and death.
Data Sharing Statement
All relevant data are included in this submitted manuscript. All data are fully available upon reasonable request.
Ethical Approval and Informed Consent
The study was approved by the Ethics Committee of Yekatit 12 Hospital Medical College. The patients’ data are anonymous, and written informed consent was obtained from each participant. This study complied with the Declaration of Helsinki.
Acknowledgment
The authors thank the participants of the study.
Funding
The authors have declared that there is no specific grant for this research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019. Results. Institute for Health Metrics and Evaluation; 2020.
2. Sun H, Saeedi P, Karuranga S, et al. Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi:10.1016/j.diabres.2021.109119
3. Zimmermann M, Bunn C, Namadingo H, et al. Experiences of type 2 diabetes in sub-Saharan Africa: a scoping review. Global Health Res Pol. 2018;3(1):1–3. doi:10.1186/s41256-018-0082-y
4. Stark Casagrande S, Fradkin JE, Saydah SH, et al. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36(8):
5. Afroz A, Chowdhury HA, Shahjahan M, Hafez MA, Hassan MN, Ali L. Association of good glycemic control and cost of diabetes care: experience from a tertiary care hospital in Bangladesh. Diabetes Res Clin Pract. 2016;1(120):142–148. doi:10.1016/j.diabres.2016.07.030
6. Donabedian A. Evaluating the quality of medical care. Milbank Quart. 2005;83(4):691. doi:10.1111/j.1468-0009.2005.00397.x
7. Unwin N, Whiting D, Guariguata L, Ghyoot G. Gan De: IDF Diabetes Atlas. Brussels: International Diabetes Federation; 2009.
8. Meier R, Valeri F, Senn O, Rosemann T, Chmiel C. Quality performance and associated factors in Swiss diabetes care–A cross-sectional study. PLoS One. 2020;15(5):e0232686. doi:10.1371/journal.pone.0232686
9. Alencherry B, Bruemmer D. Quality of diabetes care in the USA. Curr Cardiol Rep. 2021;23(7):73. doi:10.1007/s11886-021-01503-5
10. Bishu KG, Jenkins C, Yebyo HG, et al. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obesity Med. 2019;15(15):100132. doi:10.1016/j.obmed.2019.100132
11. Abera RG, Demesse ES, Boko WD. Evaluation of glycemic control and related factors among outpatients with type 2 diabetes at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: a cross-sectional study. BMC Endocr Disord. 2022;22(1):1. doi:10.1186/s12902-022-00974-z
12. American diabetic association. Standards of medical care in diabetes. J Clin Appl Res Educ. 2022;2022:1.
13. International Diabetes Federation. Clinical practice recommendations for managing type 2 diabetes in primary care; 2017.
14. Badawi D, Saleh S, Natafgi N, et al. Quality of type II diabetes care in primary health care centers in Kuwait: employment of a diabetes quality indicator set (DQIS). PLoS One. 2015;10:e0132883. doi:10.1371/journal.pone.0132883
15. Ali Mohammed K, Bullard KM, Saaddine JB, et al. Achievement of goals in US diabetes care, 1999–2010. N Engl J Med. 2013;368(17):1613–1624. doi:10.1056/NEJMsa1213829
16. Fiseha T, Alemayehu E, Kassahun W, et al. Factors associated with glycemic control among diabetic adult out-patients in Northeast Ethiopia. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3423-5
17. Badedi M, Solan Y, Darraj H, et al. Factors associated with long-term control of type 2 diabetes mellitus. J Diab Res. 2016;2016:2109542. doi:10.1155/2016/2109542
18. Kibirige D, Akabwai GP, Kampiire L, et al. Frequency and predictors of suboptimal glycemic control in an African diabetic population. Internat J Gen Med. 2017;10:33.
19. Nigussie S, Birhan N, Amare F, Mengistu G, Adem F, Abegaz TM. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: a cross-sectional study. PLoS One. 2021;16(5):e0251506. doi:10.1371/journal.pone.0251506
20. Attal S, Mahmoud MH, Aseel MT, et al. Indicators of quality of clinical care for type 2 diabetes patients in primary health care centers in Qatar: a retrospective analysis. J Endocrinol. 2019;2019:3519093.
21. Peytremann-Bridevaux I, Bordet J, Burnand B. Diabetes care in Switzerland: good, but perfectible: a population-based cross-sectional survey. BMC Health Serv Res. 2013;13(1):1. doi:10.1186/1472-6963-13-232
22. Imai C, Li L, Hardie R-A, et al. Adherence to guideline-recommended HbA1c testing frequency and better outcomes in patients with type 2 diabetes: a 5-year retrospective cohort study in Australian general practice. BMJ Qual Saf. 2021;30(9):706–714. doi:10.1136/bmjqs-2020-012026
23. Tanaka H, Tomio J, Sugiyama T, et al. Process quality of diabetes care under favorable access to healthcare: a 2-year longitudinal study using claims data in Japan. BMJ Open Diabetes Res Care. 2016;4.1:e000291. doi:10.1136/bmjdrc-2016-000291
24. Stone Margaret A, Charpentier G, Doggen K, et al. Quality of care of people with type 2 diabetes in eight European countries: findings from the Guideline Adherence to Enhance Care (GUIDANCE) study. Diabetes Care. 2013;36(9):2628–2638. doi:10.2337/dc12-1759
25. Liang H, Kennedy C, Manne S, et al. Monitoring for proteinuria in patients with type 2 diabetes mellitus. BMJ Open Diabetes Res Care. 2015;3(1):e000071. doi:10.1136/bmjdrc-2014-000071
26. Azzam MM, Ibrahim AA, Abd El-Ghany MI, et al. Factors affecting glycemic control among Egyptian people with diabetes attending primary health care facilities in Mansoura District. Egypt J Inter Med. 2021;33(1):1–10. doi:10.1186/s43162-021-00065-w
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
