Back to Journals » Vascular Health and Risk Management » Volume 19
Assessment of Lower Limb Deep Vein Thrombosis: Characterization and Associated Risk Factors Using Triplex Doppler Imaging
Authors Abdelmalik BHA , Leslom MMA, Gameraddin M , Alshammari QT , Hussien R , Alyami MH, Salih M, Yousef M , Yousif E
Received 9 March 2023
Accepted for publication 25 April 2023
Published 4 May 2023 Volume 2023:19 Pages 279—287
DOI https://doi.org/10.2147/VHRM.S409253
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Bushra HA Abdelmalik,1 Musleh Mohammed Ali Leslom,2 Moawia Gameraddin,3,4 Qurain T Alshammari,1 Rehab Hussien,1 Mansour Hussain Alyami,5 Mohammed Salih,1 Mohamed Yousef,6 Elgeili Yousif1
1Diagnostic Radiology Department, College of Applied Medical Sciences, University of Hail, Hail, Saudi Arabia; 2Najran-Hubuna Thar General Hospital, Ministry of Health, Najran, Saudi Arabia; 3Department of Diagnostic Radiology Technology, College of Applied Medical Sciences, Taibah University, Al-Madinah, Saudi Arabia; 4Department of Diagnostic Radiology, Faculty of Radiological Sciences and Medical Imaging, Alzaiem Alazhari University, Khartoum, Sudan; 5King Khalid Hospital, Health Affairs of Najran Region, Najran, Saudi Arabia; 6Radiological Sciences Program, Batterjee Medical College, Jeddah, 21442 Saudi Arabia
Correspondence: Moawia Gameraddin, Department of Diagnostic Radiology Technology, College of Applied Medical Sciences, Taibah University, Al-Madinah, Saudi Arabia, Email [email protected]
Background: Deep vein thrombosis (DVT) is a common health problem. Accurate diagnosis of DVT is essential to avoid potentially fatal acute consequences of pulmonary embolism.
Aim: The study aims to assess deep venous thrombosis (DVT) of the lower limbs and to analyze the related risk factors.
Methods: This is a retrospective study including 60 patients who were examined using Triplex Doppler imaging. The patients were referred to the imaging departments with symptoms of lower limb DVT. The risk of DVT was expressed as an odds ratio (OR) with 95% confidence interval. Multiple logistic regression analysis was used to detect the independent risk factors. P value < 0.05 was considered a significant statistic.
Results: Among the Saudi patients in Najran, acute DVT was more prevalent than chronic one (56.7% vs 38.3%), while subacute is less frequent (5%). DVTs are more prevalent in females than males (60% vs 40%) and most commonly affect patients older than 40. DVTs affect the left lower limb veins more than the right limb (75% vs 15%) and are less frequent on both sides (10%). The left popliteal vein (PV) and left common femoral vein (CFV) were the most common sites for acute DVTs. Binary logistic analysis revealed the independent risk factors for developing lower extremity DVT; malignancy (OR = 2.84, 95% CI = 0.518– 15.513), surgery (OR = 2.66, 95% CI = 0.411– 17.281), trauma (OR = 2.30, 95% CI = 0.452– 11.658), and diabetes and hypertension (OR = 1.53, 95% CI = 0.335– 6.969).
Conclusion: Acute lower limb DVT was more prevalent than chronic one. Malignancy, surgery, trauma, diabetes mellitus, and hypertension were the most common risk factors for lower limb DVTs. Left popliteal and left common femoral veins were the most common sites of acute DVTs.
Keywords: DVT, malignancy, pregnancy, popliteal vein, acute, surgery
Introduction
Deep vein thrombosis (DVT) is a potentially fatal complication that can develop early during hospitalization. Choosing patients at risk of DVT and starting prophylaxis early are crucial steps in improving outcomes.1 It is a severe disorder that can result in pulmonary embolism, which can be fatal or long-lasting harm to the vein (PE). Particularly in the calves, DVT typically starts around the leaflets of venous valves and might advance superiorly.2 The annual incidence is 1 per 1000 people worldwide.3 After the age of 45 years, the incidence rises sharply, and the entry is closely correlated with the patient’s age.4
The main risk factors are surgery, trauma, pregnancy and puberty, immobility, hospitalization, hormone usage, cancer, obesity, and inherited and acquired hypercoagulable conditions.5 A study in Saudi Arabia demonstrated that the most frequent contributing factors for lower limb DVTs were pregnancy and oral contraceptive use, trauma and surgery, and immobility. Infections, neoplasms, traumatic injuries, and vascular conditions may also cause6 DVT of the lower extremities.7
DVT affects various veins of the lower extremities, such as PV, CFV, superficial FV, and iliac veins. Ultrasound (US) is the first‐line examination for evaluating DVT due to its accuracy, non-invasiveness, and safety.8,9 The US can distinguish between acute and chronic thrombus. In acute thrombosis, the vein exhibits partial or no compressibility in the absence of collaterals and is slightly distended by a hypoechoic thrombus. In chronic DVTs, the vein is non-compressible, irregular, and narrow, and an echogenic thrombus connected to the walls of veins is present, along with collaterals.10
There is a lack of studies in Najran distinct on lower limb DVTs. The aim of this study is to evaluate lower limb DVTs and related factors which predict the status of acute and chronic DVT.
Materials and Methods
The Population
In this retrospective study, 60 patients from the Najran region of Saudi Arabia were included who had signs and symptoms of DVT pathology and had visited King Khalid Hospital and Najran General Hospital. The study was conducted from the period of June to December 2022, including every patient. The study population were 36 females and 24 males who presented with different forms of DVT pathologies. Their age ranged between 30 and 90 years. Patients who had Baker’s tumors, as determined by examination and clinical history were excluded. Data gathering sheets were used to collect the demographic information, and a picture archive and communication system (PACS) was used to gather the sonographic information (PACS). The ethical committee of king Khalid Hospital and Najran General Hospital made ethical considerations.
The Sonographic Procedure
The sonographic procedure was explained to the patients. A high-frequency linear probe with a 7.5 MHz frequency was used to evaluate the patients. The common femoral vein (CFV) was identified on a transverse scan at the groin, where the examination started. The CFV, deep femoral vein, and superficial femoral vessels up to the level of the adductor hiatus were all evaluated. Compression was applied in both transverse and longitudinal projections when the veins were immediately observed. The final sonographic reports were written by two expert Radiologists.
Ethical Considerations
Participants’ privacy was protected while the study was being analyzed. The subjects’ written, fully informed permission was acquired. The college of applied medical sciences’ ethical committee of Hail University granted the study the green light before it began, and it was assigned the identification code H- 2022-181.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).
Statistical Analysis
Statistical analysis was performed using a statistical package for social science software (SPSS) and excel programs. Descriptive statistics such as frequency and percentage were used to describe the qualitative data, such as the prevalence of DVT. A binary logistic regression test was applied to assess for factors that predict acute and chronic DVT. The risk of DVT was expressed as an odds ratio (OR) with 95% confidence interval (CI). The crude and adjusted OR and their respective 95% CI were provided to assess the contribution of each factor in the outcome of DVTs. P value <0.05 was considered a significant statistic.
Results
A total of 60 patients were examined by Duplex ultrasound for assessing DVTs. The DVT was more prevalent in females than males (60% vs 40%) and most commonly affected patients older than 40, more specifically in those 41–50 years old and those above 60 years old (Table 1). The sonographic examinations revealed that 34 (56.7%) were acute DVTs, 23 (38.3%) were chronic, and 3(5%) were subacute (Figure 1). The DVT affects the left lower limb more than the right one (75% vs 15%) and is less frequent on both sides (10%), as shown in Figure 2. Most acute DVT was present in one vein, while chronic DVT affected one or more equally (Figure 3).
 |
Table 1 Demographic Characteristics of the Study Population |
 |
Figure 1 Characterization of lower limb DVTs in the study sample. |
 |
Figure 2 Laterality of lower limb DVTs in the study sample. |
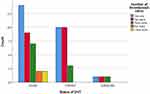 |
Figure 3 Lower limb thrombosed veins and characterization of DVTs. |
Table 2 summarizes the clinical history and risk factors of DVT. Obesity (15%), trauma (13.3%), DM & HTN 16.6%, surgery (10%), and malignancy (13.3%) were the most risk factors for lower limb DVT. Table 3 summarizes the clinical symptoms of patients diagnosed with lower limb DVT. Pain (31.7%), pain and swelling (25%), and Swelling alone (23.3%) are the most prevalent symptoms of lower limb DVTs. Table 4 summarizes the distribution of veins with DVT in the study sample. Twenty percent of the DVTs were present in the Left popliteal vein, left CFV, and superficial FV. DVTs were less frequent in the right PV (3.14%), right common iliac vein (1.7%), right anterior tibial vein (1.7%), and left external iliac vein (3.3%), as shown in Table 4.
 |
Table 2 Clinical History of Lower Limb DVTs in the Study Sample |
 |
Table 3 Clinical Symptoms of Patients Diagnosed with Lower Limb DVT |
 |
Table 4 Distribution of DVT Sites Within Lower Limb Veins in the Study Sample |
Table 5 summarizes the Logistic regression analysis for factors predicting the lower limb DVTs. The results revealed that malignant patients were 2.84 more likely to have acute lower limb DVT than non-malignant ones (OR= 2.84, 95% CI = 0.518–15.513). In contrast, patients with a history of surgery had 2.66 increased odds of being affected with acute DVT than chronic DVT. Traumatic patients had 2.30 increased Odds compared to non-traumatic ones to have acute DVT rather than chronic DVT (OR= 2.30, 95% CI = 0.452–11.658). Diabetic and hypertensive patients were 1.53 more likely to have acute DVT than chronic one compared to non-diabetic and hypertensive ones (OR = 1.53, 95% CI = 0.335–6.969)).
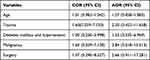 |
Table 5 Logistic Regression Analysis for Risk Factors of Lower Limb DVTs |
Discussion
A proper diagnosis of lower DVT is needed to alleviate symptoms and save the injured limb. Early thrombus, when properly managed, rapidly alleviate the symptoms of venous blockage, returns valve functionality, and reduces the risk of post-thrombotic syndrome. This study showed that the US plays an influential role in differentiating DVT as acute, subacute, and chronic. Moreover, the study clarified the acquired risk factors predicting acute and chronic lower limb DVT.
The present study found that lower limb DVT affected mostly the left popliteal vein (PV) and left common femoral vein (CFV), most of which were acute and affected the left lower extremity more than the right lower one. In agreement with this finding, Alshoabi and Mothanna reported that DVT mainly affects the CFV, superficial femoral vein (SFV), and PV.11 Consistently, they stated that lower limb DVT affects left lower extremity more than suitable and more prevalent in females than males.11 Interestingly, our study found that acute DVT is located in one vein more than multiple veins, as it is located in the left CFV and left popliteal veins. This is in agreement with Brohom et al, who stated that thrombus was more likely to involve the CFV than iliac veins.12 In contrast, Yoshimura et al reported that the muscular calf vein was the most common site of DVT.13
According to the sonographic criteria and assessment, this study found that most DVT was acute more than chronic ones. Secondary diagnostic chrematistics for acute DVT include echogenic thrombus inside lumen of the vein, venous distention, complete lack of spectral or color Doppler signal within the vein lumen, loss of flow phasicity, and loss of responsiveness to Valsalva or augmentation.14
The study showed that pain and swelling were the most frequent symptoms in patients with lower limb DVT. This is in agreement with Huang et al, who reported severe pain associated with iliofemoral DVT.15 Additionally, Alsheef et al reported that lower leg pain and lower limb swelling were the most common symptoms of DVT in pregnancy.16
The present study showed that lower limb DVTs affect patients aged 41–50 years and those older than 60 years old. This finding agreed with other studies that stated that older people are riskier of developing DVTs, specifically those who are older than 60 years, in part because older people are more likely to have health issues, less mobility, and other risk factors. Patients who are older than 60 have a 2-fold increased likely of developing DVT after surgery.17,18 Additionally, it was noted that DVT affected females more than males, and this agreed with Trinchero et al who reported that women presented with distal DVT were more prevalent than males among patients with initial symptomatic isolated acute DVT.19 Additionally, Roach et al found first venous thrombosis occurred 2.1 times more often in males than in females without reproductive risk factors.20 In contrast, this finding contradicts with Bauersachs et al and who reported that the prevalence of confirmed leg DVT was higher in men than women with significant difference.21 This contradiction in our finding is attributed to the factor of considerable number of pregnancies in the study sample. In our study, the presence of reproductive variables among women (pregnancy) conceals a gender-based risk difference.
The study demonstrated the risk factors contributing to acute and chronic lower limb DVTs. It was shown that obesity, trauma, diabetes mellitus and hypertension, malignancy, and surgery are the most risk factors. The previous studies demonstrated these factors as contributors to thrombus formation rather than the characterization of DVT. So, the study differentiated the acute and chronic DVT in the examined patients. The study found that patients with malignancies were more likely to develop DVT than those without malignancies. In literature, most cancer associated with a high risk of developing DVT as malignancies is linked with hypercoagulability.22 Generally, the risk increases with tumor size and cell line differentiation. Additional factors that increase the chance of thromboembolic events include the use of various chemotherapy drugs, central venous catheters, and the requirement for surgery for malignancies.17,23
The current study showed that patients with previous surgery were more likely to have lower extremity DVT. Irmac et al consistently reported that surgical patients are at a higher risk of developing DVT in the postoperative period.24 In addition, Kim et al found an incidence of 20–49% following total knee arthroplasty and an incidence of 18–24% following total hip arthroplasty as a result of prolonged surgical times and post-surgical immobilization.25 Therefore, lower limb surgery has been noted as a risk factor for the emergence of severe lower-limb DVT. Conversely, significant and small trauma carries a considerable risk for DVTs due to immobility. Our study found trauma increased the risk of acute DVTs by 2.30, which is consistent with McLaughlin et al, who found the same finding.26
The present study found that diabetes and hypertension were risk factors for lower limb DVTs. A challenging clinical course was more likely to occur in diabetic individuals with venous thromboembolism. Recurrent DVT was predictably associated with diabetes independently.27 Moreover, hypertension is also a considerable risk factor for DVT. Numerous co-morbidities are frequently present in DVT patients. Studies on the link between DVT and hypertension have been reported during the past few years. However, the findings are conflicting. According to several research studies, hypertension may promote the growth of DVT.28,29 According to Wang et al30 and Song et al,31 there was no statistically significant link between DVT and hypertension. As a result, further research is still needed on this controversial issue.
Obesity is an essential factor for developing lower limb DVT. Our findings showed that 15% of the patients with DVT were obese, and 26.7% were >60 years. This is in consistent with Hotoleanu et al, who reported that obesity is a moderate and independent risk factor for venous thromboembolism (VTE).32 It has been reported that the risk of VTE increases with increasing body mass index (BMI).33 The risk is higher when obesity interacts with other thrombotic risk factors. The risk rises as age increases, increasing BMI and other acquired risk factors.
Limitations of the Study
The current study faced some limitations. The size of sample is not large enough to represent the population. This limitation decreased sample size might cause a slight bias in increasing p-values and make them insignificant (>0.05). As it is retrospective and a single study, it needs to be more generalizable and include some crucial data. For example, the patient’s history did not include the inherited factors of thromboembolism. These limitations did not affect the intended results, consistent with the literature findings.
Conclusion
Acute DVTs were identified in 60 patients using triplex ultrasound. The incidence of acute lower limb DVT was higher than chronic one, and it is more prevalent in females than males. The most frequent locations for DVTs were the left popliteal and left common femoral veins. The most frequent risk factors for DVTs were cancer, surgery, trauma, diabetes mellitus, and hypertension.
Funding
This study has no grant or funding, and it is not supported by any organizations or institutes.
Disclosure
The authors declared no conflicts of interest in this study.
References
1. Ruskin KJ. Deep vein thrombosis and venous thromboembolism in trauma. Curr Opin Anaesthesiol. 2018;31(2):215–218. doi:10.1097/ACO.0000000000000567
2. Divittorio R, Bluth EI, Sullivan MA. Deep vein thrombosis: diagnosis of a common clinical problem. Ochsner Journal. 2002;4(1):14–17.
3. Adhikari S, Zeger W. Non thrombotic abnormalities on lower extremity venous duplex ultrasound examinations. West J Emerg Med. 2015;16(2):250. doi:10.5811/westjem.2014.12.24170
4. Ten Cate-Hoek AJ, van der Velde EF, Toll DB, et al. Common alternative diagnoses in general practice when deep venous thrombosis is excluded. Neth J Med. 2012;70(3):130–135.
5. Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379:1835–1846. doi:10.1161/01.CIR.0000031167.64088.F6
6. Igbinovia A, Malik GM, Grillo IA, et al. Deep venous thrombosis in Assir region of Saudi Arabia. Case-control study. Angiology. 1995;46(12):1107–1113. doi:10.1177/000331979504601206
7. Douketis JD. Deep venous thrombosis (DVT); 2022. Available from: https://www.msdmanuals.com/professional/cardiovascular-disorders/peripheral-venous-disorders/deep-venous-thrombosis-dvt.
8. Canty D, Mufti K, Bridgford L, Denault A. Point-of-care ultrasound for deep venous thrombosis of the lower limb. Australas J Ultrasound Med. 2019;23(2):111–120. doi:10.1002/ajum.12188
9. Needleman L, Cronan JJ, Lilly MP, et al. Ultrasound for lower extremity deep venous thrombosis: multidisciplinary recommendations from the Society of Radiologists in Ultrasound Consensus Conference. Circulation. 2018;137(14):1505–1515. doi:10.1161/CIRCULATIONAHA.117.030687
10. Karande GY, Hedgire SS, Sanchez Y, et al. Advanced imaging in acute and chronic deep vein thrombosis. Cardiovasc Diagn Ther. 2016;6(6):493–507. doi:10.21037/cdt.2016.12.06
11. Alshoabi SA, Mothanna A. Deep venous thrombosis: commonly affected veins in the lower limbs. J Biosci Med. 2019;7:12–19. doi:10.4236/jbm.2019.73002
12. Broholm R, Bækgaard N, Hansen S, et al. Significance of partial or complete thrombosis of the common and deep femoral vein in patients with deep vein thrombosis. Eur J Vasc Endovasc Surg. 2019;58(4):570–575. doi:10.1016/j.ejvs.2019.06.016
13. Yoshimura N, Hori Y, Horii Y, et al. Where is the most common site of DVT? Evaluation by CT venography. Jpn J Radiol. 2012;30(5):393–397. doi:10.1007/s11604-012-0059-6
14. Tapson VF, Carroll B, Davidson B, et al. The diagnostic approach to acute venous thromboembolism, clinical practice guideline. American Thoracic Society. Am J Respir Crit Care Med. 1999;160:1043–1066. doi:10.1164/ajrccm.160.3.16030
15. Huang MH, Benishay ET, Desai KR. Endovascular management of acute iliofemoral deep vein thrombosis. Semin Intervent Radiol. 2022;39(5):459–463. doi:10.1055/s-0042-1757935
16. Alsheef MA, Alabbad AM, Albassam RA, et al. Pregnancy and venous thromboembolism: risk factors, trends, management, and mortality. Biomed Res Int. 2020;2020:4071892. doi:10.1155/2020/4071892
17. McLendon K, Goyal A, Attia M. Deep venous thrombosis risk factors. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470215/#:~:text=Deep%20Venous%20Thrombosis,Maximos%20Attia.
18. Bui MH, Hung DD, Vinh PQ, et al. Frequency and risk factor of lower-limb deep vein thrombosis after major orthopedic surgery in Vietnamese patients. Open Access Maced J Med Sci. 2019;7(24):4250–4254. doi:10.3889/oamjms.2019.369
19. Trinchero A, Scheres LJJ, Prochaska JH, et al. Sex-specific differences in the distal versus proximal presenting location of acute deep vein thrombosis. Thromb Res. 2018;172:74–79. doi:10.1016/j.thromres.2018.10.025
20. Roach REJ, Lijfering WM, Rosendaal FR, et al. Sex difference in risk of second but not of first venous thrombosis. Circulation. 2014;129(1):51–56. doi:10.1161/circulationaha.113.004768
21. Bauersachs RM, Riess H, Hach-Wunderle V, et al. Impact of gender on the clinical presentation and diagnosis of deep-vein thrombosis. Thromb Haemost. 2010;103(4):710–717. doi:10.1160/TH09-10-0705
22. Sørensen HT, Mellemkjaer L, Steffensen FH, et al. The risk of a diagnosis of cancer after primary deep venous thrombosis or pulmonary embolism. N Engl J Med. 1998;338(17):1169–1173. doi:10.1056/NEJM199804233381701
23. Fernandes CJ, Morinaga LTK, Alves JL, et al. Cancer-associated thrombosis: the when, how and why. Eur Respir Rev. 2019;28(151):180119. doi:10.1183/16000617.0119-2018
24. Irmak B, Karadag M, Emre NY. The risk factors for preoperative and postoperative deep vein thrombosis in surgical patients. Clin Exp Health Sci. 2022;12:120–127. doi:10.33808/clinexphealthsci.839430
25. Kim KI, Kang DG, Khurana SS, et al. Thromboprophylaxis for deep vein thrombosis and pulmonary embolism after total joint arthroplasty in a low incidence population. Knee Surg Relat Res. 2013;25(2):43–53. doi:10.5792/ksrr.2013.25.2.43
26. McLaughlin DF, Wade CE, Champion HR, et al. Thromboembolic complications following trauma. Transfusion. 2009;49(Suppl 5):256S–63S. doi:10.1111/j.1537-2995.2008.01989.x
27. Piazza G, Goldhaber SZ, Kroll A, et al. Venous thromboembolism in patients with diabetes mellitus. Am J Med. 2012;125(7):709–716. doi:10.1016/j.amjmed.2011.12.004
28. Nazarzadeh M, Pinho-Gomes AC, Mohseni H, et al. Blood pressure and risk of venous thromboembolism: a large-scale prospective cohort analysis and a Mendelian randomization study. J Hypertens. 2019;37:e95. doi:10.1097/01.hjh.0000571236.67392.7c
29. Lind MM, Johansson M, Själander A, et al. Incidence and risk factors of venous thromboembolism in men and women. Thromb Res. 2022;214:82–86. doi:10.1016/j.thromres.2022.04.014
30. Wang CJ, Wang JW, Chen LM, et al. Deep vein thrombosis after total knee arthroplasty. J Formos Med Assoc. 2000;99(11):848–853.
31. Song EK, Kim JK, Lee KB, et al. Deep vein thrombosis after total knee replacement: incidence and correlation with clinical risk factors. J Korean Knee Soc. 1998;10(1):18–22.
32. Hotoleanu C. Association between obesity and venous thromboembolism. Med Pharm Rep. 2020;93(2):162–168. doi:10.15386/mpr-1372
33. Blokhin IO, Lentz SR. Mechanisms of thrombosis in obesity. Curr Opin Hematol. 2013;20:437–444. doi:10.1097/MOH.0b013e3283634443
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
