Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Assessment of Knowledge, Attitude, Practice and Associated Factors Towards Post-Exposure Prophylaxis for HIV/AIDS among Health Professionals in Health Centers Found in Harari Region, Eastern Ethiopia
Authors Shamil M, Legese N , Tadiwos Y
Received 21 August 2020
Accepted for publication 29 December 2020
Published 14 January 2021 Volume 2021:13 Pages 41—51
DOI https://doi.org/10.2147/HIV.S278150
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Mohammed Shamil, Nanati Legese, Yohannes Tadiwos
School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Yohannes Tadiwos
School of Pharmacy, College of Health and Medical Sciences, Haramaya University, P.O. Box 235, Harar, Ethiopia
Email [email protected]
Background: Healthcare workers are at risk of acquiring human immunodeficiency virus (HIV) infections, because of occupational exposure to blood and other body fluids. Post-exposure prophylaxis (PEP) is a short-term antiretroviral treatment used to reduce the likelihood of viral infection after exposure to the blood or body fluids of an infected person. Timely PEP after exposure to high-risk body fluids in the working area can reduce the rate of transmission of HIV significantly.
Objective: To assess the knowledge, attitude, practice, and associated factors towards PEP for HIV/AIDS among health professionals in health centers in the Harari region, Eastern Ethiopia.
Methodology: A retrospective cross-sectional study was conducted using structured questionnaires from March to April 2019. The collected data were analyzed by using SPSS version 20, and the result was presented in the form of tables and figures.
Results: Of 217 participants, 51.6% were male and 75.2% were in the age group of 20– 30 years. One hundred thirty (59.9%) respondents had a year of service less than 5 years, and nearly half (45.2%) of the participants had a Diploma. The study revealed that 35.02% of the participants had inadequate knowledge of PEP. About 32.26% had an unfavorable attitude towards PEP. Of 124 (57.1%) exposed respondents, 54 (68.4%) tried to get PEP service and 49 (90.7%) started to use PEP. Twenty-six (48.1%) respondents started to use PEP within 6 to 24 hours after exposure. Sex, qualification, and attitude status were found to have a significant association with knowledge regarding PEP.
Conclusion: The findings of this study indicated that a significant number of health professionals had poor knowledge and poor attitude towards PEP. Occupational exposures were common among health professionals. However, the practice of using PEP was low among health professionals. As a result, health facilities should strengthen and integrate routine PEP services by providing training to all health professionals.
Keywords: knowledge, attitude, practice, post-exposure prophylaxis, HIV/AIDS, health professionals, Harari region
Background
The major mode of transmission for Human Immunodeficiency Virus (HIV) is sexual contact, but the various modes of transmission may be classified as occupational (work setting at health care) and non-occupational. Occupational or workplace exposure is when someone who works in a healthcare setting is potentially exposed to material infected with HIV.1 Healthcare workers (HCW) can be exposed to HIV by needle stick injuries or cut blood or fluid splash to their eye, mouth, and injured skin. The risk for occupational transmission varies with the type, severity of the exposure, stage of disease of source patient, length of time of contact, the potential port of entry, and presence of more virulent strains of the virus. Research findings revealed that the estimated risk for HIV transmission after injury through a needle contaminated with HIV/Acquired Immune Deficiency Syndrome (AIDS) infected blood and after mucous membrane, exposure is 0.3% and 0.1%, respectively.2
Post-exposure prophylaxis (PEP), is a short-term anti-retroviral (ARV) treatment applied to reduce the likelihood of HIV infection after potential exposure to HIV either occupationally or non-occupationally. Within the health sector, PEP should be provided as a compressive universal precaution package; that reduces staff exposure to infectious hazards at the workplace.2
The US guidelines outline several requirements in determining whether the HCW should receive PEP and in choosing the type of PEP regimen. For most HIV exposures, for which PEP is given, a basic 4 weeks and two drug regimen is recommended. For HIV exposures that put an increased risk of transmission, a three-drug regimen may be recommended.3
The efficacy of PEP is related to the specific regimen, timing of PEP, and exposed workers’ adherence to the PEP regimen. To be effective, it should be initiated within 72 hours of exposure, but more likely effective if initiated within 1 to 2 hours and not considered beyond 72 hours. However, it is not 100% effective and does not guarantee someone exposed to HIV will not become infected with HIV.4,5 The uses of PEP after exposure depend on the knowledge and attitude of HCWs about it.5
However, a study regarding knowledge, attitude, and practice (KAP) about PEP was lacking in health professionals working in health centers (HCs) at Harar region, the Eastern part of Ethiopia. This would help in reducing the risk of infection for the health professionals while rendering service to the patients and help to plan and implement interventions to reduce the chance of infection and better utilization of PEP. Thus, this study was aimed at assessing the KAP of health professionals about PEP against HIV/AIDS in HCs to fill the gap on the KAP of healthcare professionals for HIV/ADIS prevention and treatment.
Methods
Study Setting
This study was conducted in Harari regional state, eastern Ethiopia. There are four governmental hospitals and eight health centers from which, 4 of them are found in Harar town and the rest in the rural part of the town. This study was conducted on health professionals of the health centers in the Harari region, from March 15 to April 1, 2019.
Study Design and Period
A cross-sectional study design was employed to assess the KAP of health professionals about PEP against HIV infection in the eight health centers of the Harari region, Eastern Ethiopia.
Sample Size Determination and Sampling Technique
The sample size was calculated using the single population proportion formula, with 50% prevalence, 5% marginal error, 95% confidence interval and since the exact number of source population was less than 10,000, correction formula was used and a sample of 197 was reached. After adding a 15% non-response rate, a final sample of 227 was found. The total number of health professionals in the health centers was 402. The sample size was then allocated proportionally to the eight health centers based on the number of health professionals in each health center (Figure (Supplementary)). Finally, participants who met the inclusion criteria were selected from the HCs using simple random sampling by using the lottery method.
Data Collection Tools and Procedures
A self-administered questionnaire was used to collect information on the KAP of healthcare professionals towards PEP. The data collection tool was adapted after reviewing different literature, guidelines, and previous studies, which were organized according to the objectives of the study. The data collection tools contain four different parts which include socio-demographic characteristics; existing knowledge about PEP, attitude, and practice towards PEP. The prepared questionnaire was pre-tested on 5% of the respondents. Before starting data collection, a brief explanation was given by the principal investigator on how to fill the questionnaire to avoid any ambiguity and misconception.
Data Processing and Analysis
The collected data was checked at the end of each data collection day for completeness and consistency and data analysis was done by using statistical package for social science (SPSS) version 20 software. Logistic regression was done to determine any association and a P-value of <0.05 was considered statistically significant. Finally, obtained results were presented using tables and charts.
Operational Definitions
Risk of exposure while at work – Exposure of HCW to blood, patient body fluids or needle prick injury or sharp injury at the workplace
HIV PEP: An anti-retroviral therapy, given in different forms after occupational exposure (OE) to HIV and will be given to HCWs if there is a percutaneous injury (for example, needle-stick or cut with a sharp object), contact with a mucous membrane or non-intact skin (for example, skin chapped or abraded or dermatitis) or prolonged contact with skin or contact that involves an extensive area of skin.2
Good knowledge: When the respondent correctly answers ≥75% of knowledge questions.6
Moderate knowledge: When the respondent correctly answers 50% to 74% of knowledge questions.6
Poor knowledge: When respondents correctly answer <50% of knowledge questions.6
Good attitude: When the respondents correctly answer >70% of attitude questions.7
Poor attitudes: When respondents correctly answer <70% of attitudes questions.7
Regimen: A course of treatment, possibly combination drugs, exercises; diets, etc. designed to bring about an important improvement in health.8
Universal precautions: Universally adopted measures taken before the medical procedure to avoid the risk of exposures while on work.8
Results
Socio-Demographic Characteristics of the Study Sample
Out of 227 participants, 217 took part in this study, with a response rate of 95.6%. More than half of the respondents 112 (51.6%) were male. Ninety-six (44.2%) were in the age range of 26–30 years. The majority of the respondents 77 (35.5%) were nurses and 124 (57.1%) had a year of service of fewer than 5 years (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Healthcare Professionals, in Health Centers of Harari Region, Eastern Ethiopia, March–April 2019 |
Knowledge About Occupational Exposure and Universal Precaution
Most of the participants, 209 (96.3%) had information about the risk of OE. Exposures by sharp cut 171 (78.8%) and needle stick injury 167 (76.9%) were considered by the majority. Most of the respondents 207 (95.3%) have heard about universal precaution (UP) and 201 (92.6%) knew at least one type of UP. Of these, 190 (87.5%) considered hand washing before and after any procedure as one way of UP. When asked about the different measures to be taken by the health professional immediately after OE, 89 (41.0%) of the health professionals consider washing the exposed area with soap and water whereas 46 (21.2%) consider washing with alcohol and iodine (Table 2).
 |
Table 2 Knowledge About Occupational Exposure, and Universal Precaution and Measures to Be Taken Among Health Professionals in HC in the Harari Region, Eastern Ethiopia, March–April, 2019 |
Knowledge About Post-Exposure Prophylaxis
Almost all 210 (96.7%) of respondents had information about PEP, of these, 158 (72.8%) knew the availability of PEP in their facility, and the majority 149 (68.6%) knew PEP as the combinations of three drugs. Seventy-eight (35.9%) of the respondents mentioned that they know the regimen Tenofovir (TDF) + Lamivudine (3TC)+ Efavirenz (EFV) and/or Zidovudine (AZT)+ Lamivudine (3TC)+ Nevirapine (NVP). 53% of the respondent mentioned that the period for initiation of PEP is within 24 hours after exposure, whereas 50.7% of the respondents mentioned that PEP should be initiated within 24–72 hours after exposure. One hundred and fourteen (52.5%) of the respondents knew the recommended duration of treatments (4 weeks) (Table 3).
 |
Table 3 Knowledge About PEP Among Health Professionals in Health Centers in the Harari Region, Eastern Ethiopia, March–April 2019 |
The overall score of knowledge questions revealed that 85 (39.17%) of the respondents had moderate knowledge about PEP followed by 76 (35.02%) who had poor knowledge and 56 (25.81%) who had good knowledge (Figure 1).
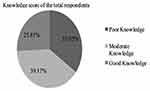 |
Figure 1 Overall knowledge score of health professionals in health centers in the Harari region, Eastern Ethiopia, March–April 2019. |
Multinomial logistic regression analysis was done to see the association among variables by using the poor knowledge category as a baseline outcome. According to the multinomial logistic regression result, sex, qualification, and attitude status were found to have a significant association with knowledge regarding PEP. Those who have a good attitude had 2.25 and 2.89 times higher chance of having moderate and good knowledge (RRR=2.25, 95% CI 1.09–4.67) and (RRR= 2.89, 95% CI 1.19–7.02) respectively. On the other hand, variables, like age, year of service, and taking training did not show significant association with knowledge about PEP (Table 4).
Attitude Towards Post-Exposure Prophylaxis
Most of the respondents 193 (88.9%) believed that HIV would be acquired occupationally. The self-risk perception question showed that 173 (79.7%) of the respondents believe that they have a risk of acquiring HIV infection occupationally. Of the total respondents, 83 (38.2%) agree that initiation of PEP after 72 hours of exposure would be effective while 59 (27.2%) disagree that staff should start PEP even if they are not willing to have an HIV test after occupational exposure (Table 5).
 |
Table 5 Attitudes of Health Professionals Towards PEP, in Health Centers of Harari Region, Eastern Ethiopia, March–April 2019 |
The overall score of attitude questions results showed that the majority of respondents 147 (67.74%) have a good attitude towards HIV PEP (Figure 2). Multivariate logistic regression analysis was done to see the association among variables. According to the multivariate logistic regression result, knowledge status was found to have a significant association with the attitude towards PEP. The odd of PEP’s good attitude were 2.29 and 2.32 times higher among those who had moderate and good knowledge when compared with those who had poor knowledge about PEP, respectively (AOR=02.29, 95% CI 1.07–4.91) and (AOR=2.32, 95% CI 1.03–5.38). On the other hand, variables, like age, sex and qualification did not show a significant association with an attitude towards PEP (Table 6).
 |
Table 6 Multiple Logistic Regression Analysis of Attitude and Associated Factors for Healthcare Professionals Towards PEP in Health Centers in the Harari Region, Eastern Ethiopia, March–April 2019 |
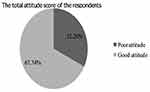 |
Figure 2 Overall attitude score toward PEP against HIV among health professionals in health centers in the Harari region, Eastern Ethiopia, March–April 2019. |
The Practice of Post-Exposure Prophylaxis
From the total respondent, 128 (59.0%) reported that they had been exposed to HIV risk factors while they are at the workplace. Of these, 71 (55.5%) were exposed once. The two common types of encountered exposures by the respondents were needle stick injury 111 (86.7%) followed by sharp cuts 52 (40.6%) (Table 7). Of those who had exposure, 37 (28.9%) of the respondents were exposed from source patient confirmed HIV positive, 42 (32.8%) from unknown serostatus, and 49 (38.3%) from HIV negative patients. Of 79 of the health professionals exposed to unknown and sero reactive patients, 54 (68.4%) tried to get PEP service and of those 49 (90.7%) started to use PEP. Out of 49 respondents who took PEP, 42 (85.7%) had taken PEP once, and 5(10.2%) reported to use PEP two times. The major reason for not starting PEP was the fear of its adverse effects 13 (52%) (Table 8).
 |
Table 7 Exposure and Measures Taken by the Health Professionals After Exposure in Health Centers in the Harari Region, Eastern Ethiopia, March–April 2019 |
 |
Table 8 Distribution of Serostatus of Source Patient and Practice of HCWs Towards PEP, Among Health Centers in Harari Region, Eastern Ethiopia, March 2019 |
The majority 143 (65.8%) of respondents reported that they have had on/off service training on HIV PEP. The perceived reasons for OE to HIV/AIDS among respondents were negligence of HCWs 135 (62.2%), followed by multiple procedures at the same time/heavy workloads 121 (55.7%) (Table 9).
 |
Table 9 Distribution of Previous Training on PEP and Perceived Reason for Occupational Exposure, Among Health Professionals in Health Centers in the Harari Region, Eastern Ethiopia, March–April 2019 |
Discussion
The present study assessed KAP regarding PEP against HIV/AIDS. Almost all of the participants in the present study had information about the risk of OE, which is almost comparable with studies conducted in Woldia General Hospital, North-Eastern Ethiopia (95.28%),9 Southwestern Nigeria (93.3%)6 and Princess Marina Hospital Gaborone (97.4%),10 but higher than the study conducted in Asella Teaching Hospital, South-East Ethiopia (88.8%).11 The higher result observed in the current study could be due to the time gap and difference in study participants, with the majority of the participant in the current survey had a Diploma. Regarding types of exposure they knew, the majority identified the high-risk exposure of sharp cut and needle stick injury, which is similar to a finding reported in a study conducted in Nigeria (81.7% and 88.5% identified mucocutaneous exposure and percutaneous exposures as high risk, respectively).12
In the current study, less than half of the respondents had poor knowledge, which is slightly higher than a study conducted among HCWs in public health institutions in Debre Markos town (36.1%),7 a study conducted in Gondor, northwest Ethiopia (36.9%)13 and a study conducted in Hiwot Fana Specialized University Hospital in Harar (17%),14 but much lower than the study conducted in Nigeria (57%)6 and a study conducted at Jigme Dorji Wangchuck National Referral Hospital, Bhutan (80.1%).15 This could be due to the difference in the knowledge assessment like the availability of PEP service and training in this survey and also a difference in the study setting and the difference in health professionals involved in the study.
Self-risk perception question in the present study showed that the majority of the respondents believe that they have a risk of acquiring HIV infection occupationally which is in line with a study conducted in India where 89% of respondents considered themselves to be at risk of HIV acquisition at their workplace.17 Almost one-fourth of the respondents did not believe that OE to HIV/AIDS is avoidable which is much higher than a study in China which showed that 10% of respondent believes OE was unavoidable.18 More than half of respondents accept that ARV drugs are effective after OE; however, this is lower than a similar study conducted in Lagos University Teaching Hospital in Nigeria (73%).19 This huge gap could be due to differences in knowledge and training they had since in the present study, one-third of the professionals did not attain any training. This study found that the majority of the respondents had a favorable attitude towards PEP for HIV which is comparable with the study conducted among HCW in Debre Markos town (69.8%).7
Practice Towards PEP
In this study, more than half of the respondents reported that they have been exposed to HIV risk conditions while they are at the workplace. This finding is higher than the study done in Botswana (53.7%),10 Gondar (33.8%),13 Gimbi town (50%)16 and Cameroon (50.8%).20 Whereas, it is much lower than a study done in Ghana (83.2%).21 This could be because of the difference in the study area and population and the difference in the workload.
Regarding immediate measures taken after exposure, half of the respondents in the current study reported that they washed the exposed area with water and soap and one-fourth washed the exposed area with alcohol and iodine, whereas a study conducted in Debre Markos revealed that 68.6% of respondents washed the wound with soap and water and 14.9% squeezed and washed with alcohol.7
In the present study, almost one-tenth of the study participants did not use PEP, which is lower when compared with a study conducted in Botswana (74.8%),10 a study in Bhutan (97.9%)15 and a study from Debre Markos town (56.7%).7 This might be due to differences in the number of those individuals who were exposed and in general due to the difference in the number of the study participants and the difference in the percentile calculation of this result being from the exposed participant who tried to get the service.
In this study, the major reasons for not taking PEP were fear of its adverse effects and lack of information about the existence of service. A similar study in Debre Markos Ethiopia revealed that 52.6% did not take PEP because the source patient was HIV negative and 31.5% because of negligence and unaware of PEP.7 The study in Bhutan however showed that the major reasons were the absence of PEP service (30.2%) and lack of support to report incidents (22.6%).15 Whereas a study from Jimma reported that 33.8% of the respondents were unaware of the existence of PEP service and protocol, 23.2% had a lack of understanding on the value of reporting exposures, and 32.2% had a fear stigma and discrimination.22 Reasons for the observed differences of findings between different research results could be due to the differences in the level of awareness between the different population, economic status, qualification of the study population and time difference of the studies, sample size differences, and study setting difference (most of the literature compared with the current study were conducted in a hospital).
According to the present study, sex, qualification, and attitude status were found to have a significant association with knowledge regarding PEP. On the other hand, the study in Debre Markos shows a strong association of profession and attitude with knowledge,7 the study in Asella shows an association of young age, female gender, low educational status, low work experience with knowledge regarding PEP,11 the study in Kenya shows the association of gender, level of education and job cadre with knowledge8 whereas the study in Gimbi,16 Jimma zone22 and Buhta15 has shown no association between knowledge and other variables (attitude).
Conclusion
The majority of health professionals have heard about OC, UP, and PEP and have a good attitude towards PEP. However, the majority had moderate and poor knowledge and also poor practice regarding PEP, as is evidenced by unnecessary measures taken and under and/or improper utilization of PEP. In general, the findings of this study revealed there is a gap in the KAP of health professionals towards PEP for HIV. The information gap present with the professional can be enhanced by training the professionals more about PEP and awareness programs and a proper guideline should be implemented for better utilization of the PEP. Besides, more efforts should be done by the institutions as well as the health professionals to reduce the risk of exposure while rendering service.
Abbreviations
AIDS, acquired immune deficiency syndrome; ARV, anti retroviral; HCWs, healthcare workers; HCs, health centers; HIV, human immunodeficiency virus; KAP, knowledge, attitude and practice; OE, occupational exposure; PEP, post-exposure prophylaxis; UP, universal precaution.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
A letter of clearance was obtained from Haramaya University, College of Medical and Health Science, School of Pharmacy, and submitted to the Harari Health Biro to obtain permission to conduct the research. All data obtained in the course of the study were kept confidential and used solely for the study. Moreover, the questioner was given to the health professionals based on informed consent and their will. Further, they were able to choose which questions to answer. The respondents were informed that the results of the study would be analyzed at the group level; that no individual would be able to be identified; and that data would be used for research purposes only.
Consent for Publication
Not applicable
Acknowledgments
The authors are thankful to all individuals who were involved in the research.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study received no support from a funding agency.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. UNAIDS.Joint UN Program on HIV/AIDS, report on global HIV epidemics. 2012. Available from: https://www.unaids.org/sites/default/files/media_asset/AIDSbythenumbers2012en.
2. Merkelz AE, Okulic JF, Bartlet J. Post-exposure HIV prophylaxis in physician and medical personnel. Medscape. 2019. Available from: https://emedicine.medscape.com/article/1991375-overview.
3. Panilion AL, Cardo DM, Grohskopf LA, Heneine W, Ross CS Updated US Public Health Service Guidelines. For the management of occupational exposure to HIV and recommendations for PEP. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm.
4. US Department of Health and Human Services. Post exposure prophylaxis. 2011: 12–124 Available from: http://www.aids.gov/hiv.aids-basics/prevention/postexposureproph.
5. CDC. Occupational HIV transmission and prevention among health care worker workers: center for disease control: HIV in health care setting. 2016; 24–26. Available from: www.cdc.gov/mmwr.
6. Adebimpe WO. Knowledge and Practice of Health Care Workers Towards Post-Exposure Prophylaxis in the Era of Low and Stable HIV Prevalence in Southwestern Nigeria. Bulletin of Faculty of Pharmacy, Cairo University; 2018:104–108.
7. Biyadgie A, Tamir Y, Alem G. Knowledge, attitude, practice, and associated factors towards post-exposure prophylaxis to HIV infection among health care professionals in Debre Markos town public health institutions, Northwest Ethiopia. Clin Pract. 2017;14(6):385–395.
8. Eumice W. Factors contributing for the uptake and compliance with HIV PEP at Kenyatta National Hospital Nairobi Kenya. 2011;4(3):231–435.
9. Erukeya H, Baye F, Awole S, Abebe MS. Assessment of knowledge, attitude & practice of health professionals towards post exposure prophylaxis of HIV/AIDS in Woldia General Hospital, Woldia, North-Eastern Ethiopia. Int J Biosci Healthcare Technol Manage. 2018;8(1):1–10.
10. Bareki P, Tenego T. Assessment of knowledge attitudes and practice of HIV post-exposure prophylaxis among the doctors and nurses in Princess Marina Hospital. Pan Afr Med J. 2018;30:233.
11. Birhanu A, Demessie A, Fantahun A, Gebrekirstos K. Awareness of post-exposure prophylaxis of HIV among health care personnel in Asella Teaching Hospital, Asella Town, South-East Ethiopia. Clin Med Res. 2014;4(3):69–74.
12. Agaba PA, Agaba EI, Ocheke AN, Daniyam CA, Akanbi MO, Okeke EN. Awareness and knowledge of HIV post exposure prophylaxis among nigerian family physicians. Niger Med J. 2012;53(3):15560. doi:10.4103/0300-1652.104386
13. Mathewos B, Birhan W, Kinfe S, et al. Assessment of knowledge, attitude and practice towards post-exposure prophylaxis for HIV among health care workers in Gondar, North West Ethiopia. BMC Public Health. 2013;13(508). doi:10.1186/1471-2458-13-508
14. Eticha EM, Gemeda AB. Knowledge, attitude, and practice of postexposure prophylaxis against HIV infection among Healthcare workers in Hiwot Fana Specialized University Hospital, Eastern Ethiopia. AIDS Res Treat. 2019;2019:7947086. doi:10.1155/2019/7947086
15. Tshering K, Wangchuk K, Letho Z. Assessment of knowledge, attitude, and practice of post-exposure prophylaxis for HIV among nurses at Jigme Dorji Wanghuck National Referral Hospital, Bhutan. PLoS One. 2020;15(8):e0238069. doi:10.1371/journal.pone.0238069
16. Tesfaye G, Gebeyehu H, Likisa J. Knowledge, attitude and practice towards HIV post-exposure prophylaxis of health professionals of Gimbi town in Ethiopia: a cross-sectional study. Int J Res Med Sci. 2014;2(2):468–471. doi:10.5455/2320-6012.ijrms20140517
17. Dulcie CA, Mohamed TS, Meenakshi B, Ezhil RJ. Assessment of knowledge about post-exposure prophylaxis of HIV among medical, nursing, and paramedical students in hospital and laboratory practice. Int J Basic Clin Pharmacol. 2017;6(10):2408–2413. doi:10.18203/2319-2003.ijbcp20174368
18. Lin CH, Li L, Wu Z, Wu S, Jia M. Occupational exposure To HIV among health care providers: a qualitative study in Yunnan, China. Int Assoc Phys AIDS Care. 2008;7(1):35–41. doi:10.1177/1545109707302089
19. Ajibola S, Akinbami A, Elikwu C, Odesanya M, Uche E. Knowledge, attitude, and practices of HIV post-exposure prophylaxis amongst health workers in Lagos University Teaching Hospital. Pan Afr Med J. 2018;19:172.
20. Ngwa CH, Ngoh EA, Cumber SN. Assessment of the knowledge, attitude, and practice of health care workers in Fako Division on post-exposure prophylaxis to bloodborne viruses: a hospital-based cross-sectional study. Pan Afr Med J. 2018;31:108. doi:10.11604/pamj.2018.31.108.15658
21. Babanawo F. Assessment of Knowledge and Use of HIV Post-Exposure Prophylaxis and Healthcare Workers’ Risk to Occupational Exposure in New Juabeng Municipality, University of Ghana, Legon. University of Ghana; 2016:23–84. http://ugspace.ug.edu.gh.
22. Bosena T, Hailu C. Assessment of HIV post-exposure prophylaxis use among health workers of governmental health institutions in Jimma zone, Oromiya region, southwest Ethiopia. Ethiop J Health Sci. 2014;20(1):53–64.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

