Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Androgen Receptor Status in Triple Negative Breast Cancer: Does It Correlate with Clinicopathological Characteristics?
Authors Dubrava AL , Kyaw PSP , Newman J , Pringle J, Westhuyzen J , La Hera Fuentes G, Shakespeare TP, Sakalkale R, Aherne NJ
Received 13 February 2023
Accepted for publication 24 March 2023
Published 11 May 2023 Volume 2023:15 Pages 359—371
DOI https://doi.org/10.2147/BCTT.S405719
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert Clarke
Alex L Dubrava,1,2 Pan Su Pyae Kyaw,1,2 Joseph Newman,1,2 Jarrad Pringle,1,2 Justin Westhuyzen,3 Gina La Hera Fuentes,2 Thomas P Shakespeare,1,2 Renukadas Sakalkale,2,4 Noel J Aherne1– 3
1Department of Radiation Oncology, Mid North Coast Cancer Centre, Coffs Harbour, New South Wales, Australia; 2Coffs Harbour Rural Clinical School, University of New South Wales, Coffs Harbour Health Campus, Coffs Harbour, New South Wales, Australia; 3School of Health and Human Sciences, Southern Cross University, Coffs Harbour, New South Wales, Australia; 4Coffs Harbour Base Hospital Pathology, Coffs Harbour, New South Wales, Australia
Correspondence: Noel J Aherne, Department of Radiation Oncology, Mid North Coast Cancer Centre, Coffs Harbour Hospital, Coffs Harbour, New South Wales, 2450, Australia, Tel + 61 2 6656 5125, Fax +61 2 6656 5855, Email [email protected]
Purpose: Triple negative breast cancer (TNBC) is a breast carcinoma subtype that neither expresses estrogen (ER) and progesterone receptors (PR) nor the human epidermal growth factor receptor 2 (HER2). Patients with TNBC have been shown to have poorer outcomes mainly owing to the limited treatment options available. However, some studies have shown TNBC tumors expressing androgen receptors (AR), raising hopes of its prognostic role.
Patients and Methods: This retrospective study investigated the expression of AR in TNBC and its relationship with known patient demographics, tumor and survival characteristics. From the records of 205 TNBC patients, 36 had available archived tissue samples eligible for AR staining. For statistical purposes, tumors were classified as either “positive” or “negative” for AR expression. The nuclear expression of AR was scored by measuring the percentage of stained tumor cells and its staining intensity.
Results: AR was expressed by 50% of the tissue samples in our TNBC cohort. The relationship between AR status with age at the time of TNBC diagnosis was statistically significant, with all AR positive TNBC patients being greater than 50 years old (vs 72.2% in AR negative TNBC). Also, the relationship between AR status and type of surgery received was statistically significant. There were no statistically significant associations between AR status with other tumor characteristics including “TNM status”, tumor grade or treatments received. There was no statistically significant difference in median survival between AR negative and AR positive TNBC patients (3.5 vs 3.1 years; p = 0.581). The relationship between OS time and AR status (p = 0.581), type of surgery (p = 0.061) and treatments (p = 0.917) were not statistically significant.
Conclusion: The androgen receptor may be an important prognostic marker in TNBC, with further research warranted. This research may benefit future studies investigating receptor-targeted therapies in TNBC.
Keywords: triple negative, breast cancer, androgen receptor
Plain Language Summary
Triple negative breast cancer (TNBC) is an uncommon subtype of breast cancer that is known by its poor prognosis due to limited treatment options available. Androgen receptors (AR) are a type of receptor found in various tissues in the body, including breast tissue. However there are few, well-documented studies in Australia that investigate the relationship between AR expression and TNBC.
Our Australian pilot study investigated the relationship between AR status and TNBC demographic and clinicopathological characteristics. The TNBC tissues of 36 eligible patients, as well as their clinical and pathological data, were collected. Their tissues were analysed for AR expression and staining intensity. Subsequent statistical analyses were then conducted.
Our study found that half of our patients had AR positive TNBC. There was a statistically significant relationship between AR status with age at TNBC diagnosis (p = 0.046) and type of surgery received (p = 0.012). In terms of patient survival, patients with AR negative TNBC had a higher median overall survival OS time when compared with AR positive patients (3.5 vs 3.1 years; p = 0.581). Due to a large proportion of our study group having AR positive TNBC and the potential prognostic value of AR, further studies may be warranted, particularly on AR inhibition therapies for TNBC.
Introduction
Breast cancer is the most prevalent cancer in women worldwide.1 Invasive ductal carcinoma (IDC), no special type and lobular carcinomas are the three most common histological subtypes.2 The biological composition of breast tumors can vary greatly between patients, with subtypes that differ in phenotype and their response to therapy.3 The three main receptor subtypes they express include: the hormone receptors, ER and PR, and a growth factor, HER2.3 Tumors that do not express these three receptors are called TNBC.
Triple Negative Breast Cancer (TNBC) accounts for approximately 15% of all breast cancer subtypes,4,5 with differing demographic and clinicopathological characteristics to other breast cancers.6,7 TNBC has a poorer prognosis, due to fewer pathways for therapeutics to target.4,5,8 TNBCs can be further sub-classified into six different molecular subtypes: two basal-like (BL1 and BL2), mesenchymal, mesenchymal stem-like, immunomodulatory, luminal AR and an unspecified group.9 This study focuses on the luminal AR subtype and its relationship with patient and tumor factors.
There are few published studies regarding TNBC characteristics with AR expression. Therefore, it could be useful to analyze retrospective data to find if AR can be a prognostic marker in TNBC. Hence, for our research question: is there a correlation between AR status in TNBC with patient demographic and clinicopathological characteristics? This study had four objectives: 1) To examine the AR status of TNBC tumors from the study population, 2) To investigate the demographic and clinicopathological characteristics of TNBC in the study cohort, including the age at TNBC diagnosis, histological subtype, laterality, tumor grade, tumor stage, tumor size, nodal status, Ki-67 expression and lymphovascular space invasion (LVSI), 3) To analyze the relationship between AR expression with demographic and clinicopathological characteristics in TNBC, and 4) To investigate patient overall survival (OS) in TNBC and its relationship with AR status and different therapies.
Materials and Methods
Study Population
This retrospective cohort study assessed the electronic medical records from 205 patients that were diagnosed with TNBC between 2010–2020 and referred to the Mid North Coast Cancer Institute, New South Wales, Australia. All patients gave informed consent at the time of treatment delivery for their anonymized data to be used for outcomes, research or educational purposes. Patients were excluded if their TNBC tissues were not available for this study. Further exclusion criteria included patients with metastatic (Stage 4) TNBC or the diagnosis of a non-invasive tumor. Hence, a total of 36 TNBC patients were eligible and included in this study. Ethics approval was obtained from the “North Coast NSW Human Research Ethics Committee” (approval no. 2019/ETH12207).
Patient Data
Patient information was collected from the electronic medical record on the Mid North Coast Cancer Institute database “MOSAIQ version 2.83” (Elekta, Stockholm, Sweden). This included patient demographic and survival data (date of birth, date and age at TNBC diagnosis, survival status, date of last follow-up, date of death where applicable, and overall survival time), tumor characteristics (histological subtype, laterality, tumor grade, tumor size, tumor stage, nodal status, Ki-67 score and LVSI) and therapies received (type of surgery, chemotherapy and/or radiation therapy).10–12
Ki-67 was categorized as “low” (<10%), “intermediate” (10–20%) and “high” (>20%).13 Primary breast tumors were staged according to the “TNM staging” criteria from the American Joint Committee of Cancer (AJCC).14 Types of surgeries that were recorded include whether the patient received a lumpectomy, mastectomy or no surgery. Radiation therapy and chemotherapy treatments received were classified as either “yes” or “no” for each patient.
Tumor Tissue and Triple Negative Status Evaluation
Patient tumor tissues were assessed by an experienced anatomical pathologist for its viability for staining. The pathologist was blinded to all the patients’ characteristics. Determining tissue viability ensured that adequate tumor tissue was present for AR staining. The procedures involved in tissue preparation and immunohistochemical staining are shown in Appendix A. These tissues were assessed for ER, PR and HER2 expression. A tumor was considered negative for ER and PR if staining was present in <1% of tumor cells (at any intensity), with satisfactory positive and negative controls.19 Human epidermal growth factor receptor 2 (HER2) immunohistochemical testing was done against a control, with the membrane intensity and the number of stained cells being analysed. These were given a score of either ‘0’, ‘1+,’ ‘2+’ or 3+. A score of ‘0’ or ‘1+’ was considered negative and a score of ‘3+’ was positive. A score of ‘2+’ required a reflex test (fluorescence in situ hybridisation), or a new test was ordered to discover if the tissue was positive or negative for HER2.20
Androgen Receptor Immunohistochemical Analysis
TNBC tissues were stained with the “anti-Androgen Receptor (SP107) Rabbit Monoclonal Primary Antibody” (Cell Marque, Rocklin, California). Prostate tissue was used as a positive control for AR staining. The steps involved with AR staining are shown in Appendix A. The pathologist then assessed each stained slide against the hematoxylin and eosin slide to evaluate the appropriate tumor area. This tumor area was where the AR score was calculated.
AR-stained nuclei of tumor cells in the tumor area were counted under a light microscope. AR expression was scored as a percentage of AR-stained tumor nuclei from the total number of tumor cells in the tumor area. TNBC tissues were considered negative for AR if no staining was present or <1% of tumor cells were stained. A score of “1+” was given for weakly stained nuclei, “2+” for moderately stained nuclei and “3+” for strong nuclear staining.21–23 Examples of AR scoring in TNBC can be seen in Appendix B.
Statistical Analysis
Descriptive statistics on patient demographic and clinicopathological data were calculated by their AR status. For the statistical analysis, TNBC tumors were classified as either “positive” or “negative” for AR expression. The statistical significance of AR status and patient characteristics were assessed by the “Fisher’s Exact test”, with a probability (p) value of “<0.05” being considered statistically significant. The “Mann–Whitney U-test” was used to find the statistical significance between the mean age at diagnosis and AR status. For the demographic data, mean, 95% confidence intervals (CI) and standard deviations were calculated.
Survival Analysis
Date of TNBC diagnosis was defined as the date of the biopsy report confirming a TNBC tumor. Overall survival time was defined from the date of diagnosis to the date of last follow-up, or if a patient passed away, then the date of last follow-up was the day before the patient’s date of death.24 Kaplan-Meier (KM) curves were created using “MedCalc version 19.0.4” (MedCalc Software Ltd, Ostend, Belgium), to assess the survival function between OS and different parameters. This included the TNBC study population, AR status, type of surgery and treatments. Median OS times with standard error were calculated from the KM curves in “MedCalc”. A 95% CI was included for the median OS time. One-, two- and three-year OS probabilities were derived from the KM curves. The “Log rank test” was used to find the statistical significance between OS and AR status, type of surgery and treatments.
Results
Androgen Receptor Status
Thirty-six TNBC tissues were analyzed. Eighteen (50%) TNBC patients had AR negative tumors and 18 (50%) had AR positive tumors (Table 1). From the 18 AR positive tumors, four had an AR expression between 1–9%, six between 10–50% and eight above 50% (Table 1). In terms of the staining intensity, 17 tumors had “0” staining intensity, four were scored as “1+”, four as “1+ to 2+”, four as “2+” and seven as “3+” (Table 1).
 |
Table 1 Androgen Receptor Expression and Staining Intensity Scores |
Clinicopathological Characteristics in TNBC
In terms of patient demographics in TNBC (Table 2), 31 patients diagnosed with TNBC were 50 years old or more (86.1%). The mean age at TNBC diagnosis was 65.1 years (95% CI: 60.9 – 69.3). In terms of tumor characteristics (Table 2), the majority were IDCs (n = 31; 88.9%), followed by metaplastic (n = 3; 8.3%) and lobular subtypes (n = 1; 2.8%). Regarding breast laterality, 21 were diagnosed in the left breast, while 15 were in the right breast. In terms of the tumor grade, the majority were grade 3 tumors (n = 30; 83.3%), followed by grade 2 (n = 5; 13.9%) and grade 1 (n = 1; 2.8%). There were 20 “T1” TNBC tumors (55.6%) followed by 11 “T2” tumors (30.6%) and five “T3” tumors (8.3%). For lymph node involvement in TNBC, 17 had no nodal involvement (47.2%), followed by those staged as “N1” (n = 13; 36.1%), “N2” (n = 3; 8.3%) and “N3” (n = 1; 2.8%). For the Ki-67 score, 20 tissues were scored as “high” (55.6%), followed by “intermediate” (n = 6; 16.7%) and “low” (n = 3; 8.3%). LVSI was present in 6 of 29 TNBC patients. Regarding AJCC staging, 12 patients (33.3%) were “stage 1”, 15 were “stage 2” (41.7%) and seven were “stage 3” (19.4%) (Table 2).
 |
Table 2 Triple Negative Breast Cancer Characteristics by Androgen Receptor Status |
Regarding patient therapies for TNBC (Table 2), lumpectomy (n = 17; 47.2%) and mastectomy (n = 16; 44.4%) rates were similar, with very few patients not receiving surgery (n = 3; 8.3%). For neoadjuvant or adjuvant therapy, a majority had both radiation therapy and chemotherapy (n = 23; 63.9%), followed by radiation therapy only (n = 7; 19.4%), chemotherapy only (n = 4; 11.1%) and very few patients received no radiation therapy or chemotherapy (n = 2; 5.6%).
Associations Between TNBC Clinicopathological Characteristics and AR Status
For patient demographics (Table 2), all patients diagnosed with AR positive TNBC were aged over 50 years, compared to 13 out of 18 (72.2%) which were AR negative. The relationship between age at TNBC diagnosis and AR status was statistically significant (p = 0.046). The mean age of AR positive patients (mean = 67.2 years; [95% CI: 63.4 – 71.0]) was higher compared to AR negative patients (mean = 63.0 years; [95% CI: 55.4 – 70.6]), however this was not statistically significant (p = 0.317). Also, tumor characteristics were not statistically significant with AR status. This includes histological subtype, laterality, tumor grade, tumor size, tumor stage, nodal status, Ki-67 and LVSI (Table 2). In terms of surgical treatment, AR positive patients had more mastectomies (66.7% vs 22.2%) while having fewer lumpectomies (33.3% vs 61.1%) than AR negative patients. These results were shown to be statistically significant (p = 0.012). However, it is unclear whether tumor staging affects the correlation between type of surgery and AR status. There were no statistically significant correlations between non-surgical treatments received and AR status (Table 2). Table 3 combines the categorical data for certain tumor characteristics. These results also showed no statistically significant relationships between AR status and tumor grade, tumor size, tumor stage, nodal status and Ki-67.
 |
Table 3 Analysis of Triple Negative Breast Cancer Combined Tumor Data by Androgen Receptor Status |
Overall Survival
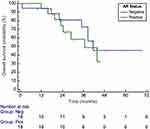
The median OS time for our patients was 41.6 months [95% CI: 29.0 – 43.7]). AR positive TNBC patients had a lower median OS time than AR negative patients, however, the differences were not statistically significant (Table 2). The one-, two- and three-year OS probabilities for the TNBC study population were 94%, 77.5% and 66% respectively (Figure 1). For AR positive patients, the one-, two- and three-year OS probabilities were 94%, 74% and 57.5% respectively. For AR- patients, the one-, two- and three-year OS probabilities were 94.5%, 81% and 72.5% respectively. However, the correlation between OS and AR status were not statistically significant in the KM analysis (Figure 2).
Overall survival times in TNBC were also assessed by the type of therapies received. For types of surgery, the one-, two- and three-year OS probabilities for patients who had a lumpectomy were 100%, 84% and 72% respectively. For mastectomy patients, the one-, two- and three-year OS probabilities were 94%, 72.5% and 57.5% respectively. However, the relationship between OS and type of surgery was not statistically significant (Figure 3). For non-surgical treatments given, the one-, two- and three-year OS probabilities for TNBC patients who only received chemotherapy were 100%, 50% and 50% respectively. The OS probabilities at one-, two- and three-years for patients who only received radiation therapy were 100%, 86% and 86% respectively. The OS probabilities at one-, two- and three-years for patients who received chemotherapy and radiation therapy were 95%, 80% and 61% respectively. However, the correlation between non-surgical treatments received and OS was not statistically significant (Figure 4).
Discussion
There are few, well-documented studies in Australia on how AR plays a role in TNBC. These include the prevalence of AR expression in TNBC and its relationship with patient demographic and clinicopathological characteristics. Hence, this pilot study investigates the data and tissue samples of 36 TNBC patients from the MNCLHD.
AR is a type 1 nuclear receptor and functions as an intracellular transcription factor that is responsible for gene expression.25,26 These receptors are present in both sexes within tissues such as bone, brain, liver and breast.26 In breast tissue, testosterone converts into dihydrotestosterone in the cytoplasm via the enzyme, 5ɑ-reductase.26–28 It then binds to AR with heat shock proteins (HSP), which leads to HSP dissociation, activation via phosphorylation and AR dimerization.26–28 The AR dimer, in the cell nuclei, translocates onto the androgen-response element in the promoter regions of the respective genes.26–28 With the addition of coregulators or transcription factors, the AR dimer-androgen response element promotes up- or down-regulation of DNA transcription.26–28 This leads to either cell cycle regulation and inhibition or stimulation of cell proliferation.26–28 Since AR is expressed on cell nuclei, this is the basis of AR immunohistochemical analysis in TNBC tumor cells.29,30
The expression of AR in TNBC is a novel concept, with studies demonstrating variable conclusions on their relationship (Appendix C). They demonstrate that AR positive expression in TNBC varies from 18.8 to 41% of patients.8,29–34 For patient demographics, research has shown that the mean age at TNBC diagnosis ranges from 45.3–58.4 years old.8,29,31,35–37 In terms of tumor characteristics, the relationship with AR status in TNBC varies between studies. It has been observed that AR negative TNBCs are more likely to have lymph node metastases than AR positive tumors.33,38,39 In addition, multiple studies find that AR negative tumors are more likely to present at a higher grade and stage than AR positive tumors.29,30,34,35,37 From the limited research on TNBC histological subtypes, IDC is the most common, with one paper presenting that AR negative tumors are more likely to be ductal than AR positive tumors.30,35 In our study, three patients had “metaplastic” TNBC. These TNBC morphologies are treated the same as other TNBC morphologies, hence were included in the statistical analyses. Comparison of results from different studies can be seen in Appendix C.
Similarly, there is minimal research to date on Ki-67 and LVSI in TNBC and its relationship with AR status. Ki-67 (a protein present in proliferating cells) is used as a biomarker for tumor proliferation and as a prognostic factor.40 Few studies have highlighted that AR negative tumors are more likely to have a higher Ki-67 expression than AR negative tumors in TNBC.8,37,39,41 Lymphovascular space invasion is the extent of tumor that has invaded neighboring lymphatics or blood vessels in the tissue it resides in and is a predictor of aggressive tumor behaviour.35 One study demonstrates that AR positive tumors are more likely to present with LVSI than AR negative tumors in TNBC.35 However, there are also very few published studies in Australia that investigate TNBC patient survival outcomes and its relationship with AR expression.
An important factor in TNBC patient care is estimating survival times. Some studies conclude that there are no associations between OS in TNBC and AR status.30,31,33 However, multiple papers show that TNBC patients with AR positive tumors have better survival times than those with AR- tumors.8,34,36,41 This includes a better OS time after three and five years for patients with AR+ tumors than AR- tumors.37,38,41 Appendix C compares the OS times of TNBC patients from different studies. However, these studies do not examine whether patient treatment choices affected their respective survival times. For instance, a study has shown that TNBC patients who received radiation therapy and chemotherapy had improved survival outcomes and fewer tumor recurrences42,43 For patient surgical interventions, multiple papers have demonstrated that late-stage TNBC patients who received a mastectomy had poorer survival outcomes than those who received a lumpectomy.24,44,45 Therefore, choice of therapy for TNBC and tumor stages could be an important factor when investigating survival outcomes.
In our research cohort, 50% of TNBC tumors expressed AR. This is a relatively high percentage than the 18.8–41% range seen in similar papers.8,29,30,33,34,37,46,47 Those studies, including ours, use an AR staining cut-off of <1% to define AR negative TNBC tumors. However, other papers defined their AR- staining at <10%. Similarly, the percentage of AR positive TNBC in those studies range from 17.1–38%.31,35,36,38,39,48
The mean age at TNBC diagnosis in our study is 65.1 years, which is older than those seen in similar studies (45.3–58.4 years).6–8,29,31,35–37 However, in one study it was found that with increasing incidences of breast cancer by age and an ageing population, TNBC may become more prevalent in older patients.49 In our study, the majority of TNBC patients had IDC, higher grade tumors, high Ki-67 scores and stage I or II TNBC. Higher tumor grades and Ki-67 scores, as well as ductal TNBC, have been shown to have poorer patient outcomes in TNBC.6–8,30,35,46,48,50,51
The relationship between the age at TNBC diagnosis and AR status was statistically significant. The mean age of AR positive patients was 67.2 years which was older than AR negative patients (63.0 years), however this was not statistically significant. Some studies suggest that there are no associations between AR status and age at TNBC diagnosis.33,34,39,41 Although, a possible factor that should be considered when investigating age at diagnosis and AR status is the study population. A multi-institutional paper found that the majority of TNBC patients in a Nigerian study and United Kingdom (UK) study were diagnosed at less than 50 years old.52 However, only 8.3% of the TNBC patients from the Nigerian study were AR positive, while 54.9% were AR positive in the UK study.52 Hence, demographic factors may play a role in TNBC and its relationship with AR status.
A Malaysian study analyzed the clinicopathological characteristics of 97 TNBC patients, which indicated that tumor characteristics play a prognostic role in TNBC29. However, the results from our study showed no statistical significance between tumor characteristics and AR status. These include the histological subtype, laterality, tumor grade, tumor size, tumor stage, nodal status, Ki-67 score and LVSI. Similar studies which have “1%” as their AR cut-off score show mixed results. The majority suggest that AR negative TNBC tumors are more likely to be bigger, have a higher grade and stage, more lymph node involvement, higher Ki-67 score and present as ductal carcinomas than AR positive tumors.29,30,33,37 However, An American study with 135 TNBC patients proposes that AR positive TNBC tumors are more likely to have a bigger tumor size and lymph node involvement.8 These conflicting results are also seen in other articles that use 10% as their cut-off score for AR staining.31,35,38,39 This variation in results could be due to different methodologies being conducted in this field of research. These include the cut-off for receptor positivity in TNBC and AR, the size of the study population, possible patient selection biases and AR histopathological scoring.37 Consequently, some of these issues can affect other parameters in this type of study, including the survival analysis.
The median OS time for our study cohort is 41.6 months. This is a comparably short time, since other articles report mean and median OS times from 46 to 109.4 months respectively.24,39,45 Furthermore, tumor characteristics such as a higher tumor stage and lymph node metastases result in poorer OS times.44,45 In addition, patient therapies for TNBC may correlate with their survival time. Studies show that mastectomy patients have a worse OS in TNBC, as this surgical approach is recommended for higher T stage breast cancer than a lumpectomy.24,44,45 Hence, in our study, certain tumor factors (such as tumor stage) may explain why AR positive patients had higher rates of mastectomies than AR negative patients. However, this paper demonstrated that there was no statistically significant relationship between OS and the type of surgery. Similarly, we found no statistical significance between different non-surgical treatments and OS.
In our study, there was no statistical significance on the median OS and one-, two- and three-year OS probabilities between AR negative and positive TNBC patients. This emphasises the fact that the relationship between AR status in TNBC and OS still remains controversial, with different conclusions drawn from the current literature.8,33,34,36–39,41 However, tumor characteristics also play a role in OS and TNBC when comparing the two groups.33,37,38,41 Therefore, some papers argue that there is no relationship between survival time and AR status in TNBC, due to the influences that tumor factors, treatments, patient comorbidities and follow-up times can have when investigating patient survival.30,31,53,54 Furthermore, studies show that TNBC patients with different tumor AR expressions does not affect the relationship between AR and patient survival time.53,55 Therefore, the value of AR as a prognostic marker in TNBC requires more investigation.
In our study, 50% of TNBC patients expressed AR, hence it may be useful for AR to be routinely screened when pathologically analyzing TNBC. Apart from being a potential predictive tumor marker, one study presents that AR expression more likely results in breast cancer metastases and increased risk of TNBC recurrences.56 Furthermore, the demand for AR inhibition therapy in TNBC may be warranted if a large proportion of a population expresses AR. Target therapies such as ER and HER2 inhibitors have already been successful in improving patient outcomes in breast cancer, however AR inhibition has become a novel therapeutic target.29,30 Therefore, AR targeted therapies may be useful to investigate in TNBC.
Conclusion
This pilot study demonstrates that a significant number of TNBC patients express AR. The relationships between AR status with age at TNBC diagnosis and type of surgery are statistically significant. Though there are no statistically significant relationships between AR status and tumor characteristics, this is a novel area of research and larger cohort studies are warranted due to the potential role of AR as a prognostic marker. Furthermore, this type of research can complement future research investigating TNBC.
Ethics
This study complies with the Declaration of Helsinki.
Acknowledgments
We would like to acknowledge all of our patients, Trevor Baillie from NSW Health Pathology for his support in tissue specimen collection and processing as well as Matthew Hoffmann, Deputy Chief Radiation Therapist from Mid North Coast Local Health District for assistance with data collection. I would also like to acknowledge the Royal College of Pathologists of Australasia who awarded a 2021 Science Student scholarship to support the completion and presentation of this work. This work was presented in part at the New Zealand Society of Oncology/New Zealand Society of Pathology 2022 Annual Meeting where it won the IGENZ Trainee Oral Presentation prize.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Giovannelli P, Di Donato M, Galasso G, et al. The androgen receptor in breast cancer. Front Endocrinol. 2018;9(492). doi:10.3389/fendo.2018.00492
2. Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and current knowledge of breast cancer. Biol Res. 2017;50(1). doi:10.1186/s40659-017-0140-9
3. Feng Y, Spezia M, Huang S, et al. Breast cancer development and progression: risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes Dis. 2018;5:77–106. doi:10.1016/j.gendis.2018.05.001
4. Mehanna J, Haddad FG, Eid R, Lambertini M, Kourie HR. Triple-negative breast cancer: current perspective on the evolving therapeutic landscape. Int J Womens Health. 2019;11:431–437. doi:10.2147/IJWH.S178349
5. Collignon J, Lousberg L, Schroeder H, Jerusalem G. Triple-negative breast cancer: treatment challenges and solutions. Breast Cancer. 2016;8:93–107. doi:10.2147/BCTT.S69488
6. Naher S, Tognela A, Moylan E, Adams DH, Kiely B. Patterns of care and outcomes among triple-negative early breast cancer patients in South Western Sydney. Intern Med J. 2017;48:567–572. doi:10.1111/imj.13628
7. Siddharth S, Sharma D. Racial disparity and triple-negative breast cancer in African-American women: a multifaceted affair between obesity, biology, and socioeconomic determinants. Cancer Multidisci Digital Publish Ins. 2018;10(12):1–19. doi:10.3390/cancers10120514
8. Astvatsaturyan K, Yue Y, Walts AE, Bose S. Androgen receptor positive triple negative breast cancer: clinicopathologic, prognostic, and predictive features. Public Library Sci One. 2018;13(6). doi:10.1371/journal.pone.0197827
9. Wang DY, Jiang Z, Ben-David Y, Woodgett JR, Zacksenhaus E. Molecular stratification with triple-negative breast cancer subtypes. Sci Rep. 2019;9(19107). doi:10.1038/s41598-019-55710-w
10. Gortman A, Aherne NJ, Westhuyzen J, et al. Metaplastic carcinoma of the breast: clinicopathological features and treatment outcomes with long-term follow up. Molecul Clin Oncol. 2021;15(178). doi:10.3892/mco.2021.2340
11. Shingde R, Salindera S, Aherne NJ, et al. Survival outcomes for breast cancer patients who decline recommended treatment: a propensity score-matched analysis. ANZ J Surg. 2021;91:1766–1771. doi:10.1111/ans.16859
12. Hallenstein LG, Sorensen C, Hodgson L, et al. Assessment of genetic referrals and outcomes for women with triple negative breast cancer in regional cancer centres in Australia. Hered Cancer Clin Pract. 2021;19(19). PMID: 33637119. doi:10.1186/s13053-021-00176z
13. Leung SCY, Nielson TO, Zabaglo L, et al. Analytical validation of a standardized scoring protocol for Ki67: Phase 3 of an international multicenter collaboration. NPJ Breast Cancer. 2016;2(16014). doi:10.1038/npjbcancer.2016.14
14. American College of Surgeons. American Joint Committee on Cancer (AJCC) cancer staging manual; 2018. Available from: https://cancerstaging.org/referencestools/deskreferences/Documents/AJCC%20Breast%20Cancer%20Staging%20System.pdf.
15. Roche Diagnostics. VENTANA anti-estrogen receptor (ER) (SP1) rabbit monoclonal primary antibody; 2020. Available from: https://diagnostics.roche.com/us/en/products/product-category/breast-diagnostic-solutions.html.
16. Roche Diagnostics. VENTANA anti-progesterone receptor (PR) (1E2) rabbit monoclonal primary antibody; 2019. Available from: https://diagnostics.roche.com/us/en/products/productcategory/breast-diagnostic-solutions.html.
17. Roche Diagnostics. VENTANA anti-HER2/neu (4B5) rabbit monoclonal primary antibody; 2020. Available from: https://diagnostics.roche.com/us/en/products/productcategory/breast-diagnostic-solutions.html.
18. Marque C. Anti-androgen receptor (SP107) rabbit monoclonal primary antibody; 2017. Available from: https://www.cellmarque.com/antibodies/CM/2126/Androgen-Receptor_SP107.
19. Allison KH, Hammond MEH, Dowsett M, et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol. 2020;38:1346–1366. doi:10.1200/JCO.19.02309
20. Wolff AC, Hammond MEH, Allison KH, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice guideline focused update. Arch Pathol Lab Med. 2018;142:1364–1382. doi:10.5858/apra.2018-0902-SA
21. Kumar V, Yu J, Phan V, Tudor IC, Peterson A, Uppal H. Androgen receptor immunohistochemistry as a companion diagnostic approach to predict clinical response to enzalutamide in triple-negative breast cancer. J Clin Oncol. 2017;1:1–19. doi:10.1200/PO.17.00075
22. Bronte G, Bravaccini S, Ravaioli S, et al. Androgen receptor expression in breast cancer: what differences between primary tumor and metastases? Transl Oncol. 2018;11(14):950–956. doi:10.1016/j.tranon.2018.05.006
23. Bravaccini S, Ravaioli S, Amadori D, et al. Are there differences in androgen receptor expression in invasive breast cancer in African (Tanzanian) population in comparison with the Caucasian (Italian) population? Front Endocrinol. 2018;9(137):1–6. doi:10.3389/fendo.2018.00137
24. Wen S, Manuel L, Doolan M, Westhuyzen J, Shakespeare TP, Aherne NJ. Effect of clinical and treatment factors on survival outcomes of triple negative breast cancer patients. Dovepress. 2020;12:27–35. doi:10.2147/BCTT.S236483
25. Narayanan R, Dalton JT. Androgen receptor: a complex therapeutic target for breast cancer. Cancer Multidisci Digital Publish Ins. 2016;8(12):1–17. doi:10.3390/cancers8120108
26. Venema CM, Bense RD, Steenbruggen TG, et al. Consideration of breast cancer subtype in targeting the androgen receptor. Pharmacol Ther. 2019;200:135–147. doi:10.1016/j.pharmathera.2019.05.005
27. Anestis A, Zoi I, Papavassiliou AG, Karamouzis MV. Androgen receptor in breast cancer - clinical and preclinical research insights. MDPI. 2020;25(2):1–11. doi:10.3390/molecules25020358
28. Gerratana L, Basile D, Buono G, et al. Androgen receptor in triple negative breast cancer: a potential target for the targetless subtype. Cancer Treat Rev. 2018;68:102–110. doi:10.1016/j.ctrv.2018.06.005
29. Teoh PY, Tan GC, Mahsin H, Wong YP. Androgen receptor expression in triple negative breast carcinoma and its association with the clinicopathological parameters. Malays J Pathol. 2019;41(2):125–132.
30. Sunar V, Dogan HT, Sarici F, et al. Association between androgen receptor status and prognosis in triple negative breast cancer. JBUON. 2018;23(5):1325–1330.
31. McGhan LJ, McCullough AE, Protheroe CA, et al. Androgen receptor-positive triple negative breast cancer: a unique breast cancer subtype. Ann Surg Oncol. 2014;21(2):361–367. doi:10.1245/s10434-013-3260-7
32. Wang C, Pan B, Zhu H, et al. Prognostic value of androgen receptor in triple negative breast cancer: a meta-analysis. Oncotarget. 2016;7(29):46482–46491. doi:10.18632/oncotarget.10208
33. Liu YX, Zhang KJ, Tang L. Clinical significance of androgen receptor expression in triple negative breast cancer-an immunohistochemistry study. Oncol Lett. 2018;15(6):10008–10016. doi:10.3892/ol.2018.8548
34. Riaz N, Idress R, Habib S, Lalani E. Lack of androgen receptor expression selects for basal-like phenotype and is a predictor of poor clinical outcome in non-metastatic triple negative breast cancer. Front Oncol. 2020;10:1–14. doi:10.3389/fonc.2020.01083
35. Jam S, Abdollahi AZ, Khazaeipour Z, Omranipour R, Najafi M. Androgen receptor expression in triple-negative breast cancer. androgen receptor expression in triple-negative breast cancer. Arch Breast Cancer. 2019;6(2):90–94. doi:10.32768/abc.20196292-95
36. Payandeh M, Shazad B, Madani SH, Ramezani M, Sadeghi M. Androgen receptor expression and its correlation with other risk factors in triple negative breast cancers: a report from Western Iran. Asian Pac J Cancer Prev. 2016;17(7):3321–3324.
37. Cabezas-Quintario MA, Zenzola V, Arguelles M, Perez-Fernandez E. Androgen receptor as prognostic marker in triple-negative breast cancer patients. J Med Surg Pathol. 2018;3(4):1–6. doi:10.4172/2472-4971.1000170
38. Lyalkin SA, Verevkina NO, Alekseyenko OO, Syvak LA. Prognostic role of androgen receptor expression in patients with metastatic triple negative breast cancer. Exp Oncol. 2020;42(2):140–143. doi:10.32471/exp-oncology.2312-8852.vol-42-no-2.14579
39. Zakaria F, El-Mashad N, Mohamed D. Androgen receptor expression as a prognostic and predictive marker in triple-negative breast cancer patients. Alexandria J Med. 2016;52(2):131–140. doi:10.1016/j.ajme.2015.06.002
40. Soliman NA, Yussif SM. Ki-67 as a prognostic marker according to breast cancer molecular subtype. Cancer Biol Med. 2016;13(4):496–504. doi:10.20892/j.issn.2095-3941.2016.0066
41. Hu XQ, Chen WL, Ma HG, Jiang K. Androgen receptor expression identifies patient with favorable outcome in operable triple negative breast cancer. Oncotarget. 2017;8(34):56364–56374. doi:10.18632/oncotarget.16913
42. James M, Dixit A, Robinson B, Frampton C, Davey V. Outcomes for patients with non-metastatic triple-negative breast cancer in New Zealand. Clin Oncol. 2019;31(1):17–24. doi:10.1016/j.clon.2018.09.006
43. O’Rorke M, Murray LJ, Brand J, Bhoo-Pathy N. The value of adjuvant radiotherapy on survival and recurrence in triple-negative breast cancer: a systematic review and meta-analysis of 5507 patients. Cancer Treat Rev. 2016;47:12–21. doi:10.1016/j.ctrv.2016.05.001
44. Gonçalves H, Guerra MR, Duarte Cintra JR, Fayer VA, Brum IV, Bustamante Teixeira MT. Survival study of triple-negative and non-triple-negative breast cancer in a Brazilian cohort. Clin Med Insights. 2018;12. doi:10.1177/1179554918790563
45. Chen SS, Tang SC, Li K, et al. Predicting the survival of triple-negative breast cancer in different stages: a SEER population based research referring to clinicopathological factors. Cancer Invest. 2020;38(10):549–558. doi:10.1080/07357907.2020.1831010
46. Asano Y, Kashiwagi S, Goto W, et al. Expression and clinical significance of androgen receptor in triple-negative breast cancer. Cancer Multidisci Digital Publish Ins. 2017;9(1). doi:10.3390/cancers9010004
47. Kneubil MC, Godoy AEG, Coelho GP, et al. Androgen receptor expression in triple negative breast cancer and its relationship to prognostic factors. Mastology. 2017;27(3):199–205. doi:10.5327/Z2594539420170000205
48. Adamo B, Ricciardi GRR, Ieni A, et al. The prognostic significance of combined androgen receptor, E-Cadherin, Ki67 and CK5/6 expression in patients with triple negative breast cancer. Oncotarget. 2017;8(44):76974–76986. doi:10.18632/oncotarget.20293
49. Tzikas AK, Nemes S, Linderholm BK. A comparison between young and old patients with triple-negative breast cancer: biology, survival and metastatic patterns. Breast Cancer Res Treat. 2020;182(3):643–654. doi:10.1007/s10549-020-05727-x
50. Balkenhol MCA, Vreuls W, Wauters CAP, Mol SJJ, van der Laak JAWM, Bult P. Histological subtypes in triple negative breast cancer are associated with specific information on survival. Ann Diagn Pathol. 2020;46. doi:10.1016/j.anndiagpath.2020.151490
51. Sanges F, Floris M, Cossu-Rocca P, et al. Histologic subtyping affecting outcome of triple negative breast cancer: a large Sardinian population-based analysis. BioMed Central Cancer. 2020;20(1). doi:10.1186/s12885-020-06998-9
52. Bhattarai S, Klimov S, Mittal K, et al. Prognostic role of androgen receptor in triple negative breast cancer: a multi-institutional study. Cancers. 2019;11(7):995. doi:10.3390/cancers11070995
53. Ricciardelli C, Bianco-Miotto T, Jindal S, et al. The magnitude of androgen receptor positivity in breast cancer is critical for reliable prediction of disease outcome. Am Associ Cancer Res. 2018;24(10):2328–2341. doi:10.1158/1078-0432.CCR-17-1199
54. Escala-Garcia M, Morra A, Canisius S, et al. Breast cancer risk factors and their effects on survival: a Mendelian randomisation study. BioMed Central Med. 2020;18(1). doi:10.1186/s12916-020-01797-2
55. Kensler KH, Regan MM, Heng YJ, et al. Prognostic and predictive value of androgen receptor expression in postmenopausal women with estrogen receptor-positive breast cancer: results from the Breast International Group Trial 1-98. Breast Cancer Res. 2019;21(1). doi:10.1186/s13058-019-1118-z
56. Giovannelli P, Di Donato M, Auricchio F, Castoria G, Migliaccio A. Androgens induce invasiveness of triple negative breast cancer cells through AR/Src/PI3-K complex assembly. Sci Rep. 2019;9(1). doi:10.1038/s41598-019-41016-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.