Back to Journals » Nature and Science of Sleep » Volume 14
All-Cause Mortality in People with Co-Occurring Insomnia Symptoms and Sleep Apnea: Analysis of the Wisconsin Sleep Cohort
Authors Lechat B , Loffler KA , Wallace DM, Reynolds A, Appleton SL , Scott H , Vakulin A, Lovato N, Adams R , Eckert DJ , Catcheside PG, Sweetman A
Received 3 August 2022
Accepted for publication 30 September 2022
Published 13 October 2022 Volume 2022:14 Pages 1817—1828
DOI https://doi.org/10.2147/NSS.S379252
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Bastien Lechat,1 Kelly A Loffler,1 Douglas M Wallace,2,3 Amy Reynolds,1 Sarah L Appleton,1 Hannah Scott,1 Andrew Vakulin,1,4 Nicole Lovato,1,4 Robert Adams,1,4 Danny J Eckert,1 Peter G Catcheside,1 Alexander Sweetman1,4
1Adelaide Institute for Sleep Health and FHMRI Sleep Health, Flinders University, Adelaide, South Australia, Australia; 2Department of Neurology, Sleep Medicine Division, University of Miami Miller School of Medicine, Miami, FL, USA; 3Neurology Service, Bruce W. Carter Department of Veterans Affairs Medical Centre, Miami, FL, USA; 4National Centre for Sleep Health Services Research: A NHMRC Centre of Research Excellence, Flinders University, Adelaide, South Australia, Australia
Correspondence: Bastien Lechat, Adelaide Institute for Sleep Health and Flinders Health and Medical Research Institute: Sleep Health, Level 2A, Mark Oliphant Building, 5 Laffer Drive, Flinders University, Bedford Park, South Australia, 5042, Australia, Email [email protected]
Purpose: Insomnia symptoms and sleep apnea frequently co-occur and are associated with worse sleep, daytime function, mental health and quality of life, compared to either insomnia or obstructive sleep apnea (OSA) alone. This study aimed to investigate the association of symptoms of co-morbid insomnia and sleep apnea (COMISA) with all-cause mortality.
Patients and Methods: Wisconsin Sleep Cohort data were analysed to assess potential associations between COMISA symptoms and all-cause mortality. Nocturnal insomnia symptoms were defined as difficulties initiating sleep, maintaining sleep, and/or early morning awakenings “often” or “almost always”, and/or regular sedative-hypnotic medicine use. OSA was defined as an apnea-hypopnea index ≥ 5/hr sleep. Participants were classified as having neither insomnia symptoms nor OSA, insomnia symptoms alone, OSA alone, or COMISA symptoms. Associations between the four groups and all-cause mortality over 20 years of follow-up were examined via multivariable adjusted Cox regression models.
Results: Among 1115 adult participants (mean ± SD age 55 ± 8 years, 53% males), 19.1% had COMISA symptoms. After controlling for sociodemographic and behavioral factors, COMISA symptoms were associated with an increased risk of all-cause mortality compared to no insomnia symptoms or OSA (HR [95% CI]; 1.71 [1.00– 2.93]). OSA alone (0.91 [0.53, 1.57]) and insomnia symptoms alone (1.04 [0.55, 1.97]) were not associated with increased mortality risk.
Conclusion: Co-morbid insomnia symptoms and sleep apnea is associated with increased all-cause mortality risk. Future research should investigate mechanisms underpinning COMISA and the effectiveness of different treatment approaches to reduce mortality risk for this common condition.
Keywords: sleep disordered breathing, Wisconsin Sleep Cohort, COMISA, obstructive, sleep apnea, insomnia, respiratory
Plain Language Summary
The co-occurrence of insomnia symptoms in people with obstructive sleep apnea (COMISA) is highly prevalent and is associated with poorer cardio-metabolic and mental health. This study investigated the association between COMISA and all-cause mortality over a 19-year follow-up in 1115 adult participants (number of deaths: 108). COMISA was associated with poorer cardiovascular and metabolic health at baseline, with higher prevalence of cardiovascular diseases, hypertension and diabetes compared to participants with neither sleep disorder. Participants with COMISA also had more depression and anxiety symptoms than participants with no sleep disorders. COMISA was also associated with a ~70% increased risk in all-cause mortality compared to control; further suggesting that people with insomnia symptoms and obstructive sleep apnea may be a specific group at higher risk of poor health.
Introduction
Obstructive sleep apnea (OSA) and insomnia are the two most common clinical sleep disorders, and frequently co-occur.1–3 OSA is characterized by brief closure (apnea) and narrowing (hypopnea) of the upper airway during sleep, which results in frequent cortical arousals from sleep, non-restorative sleep, worse physical/mental health, and reduced quality of life.2,4,5 It is estimated that 20% of people worldwide have OSA.6 Insomnia is characterized by difficulties initiating sleep, maintaining sleep or early morning awakenings from sleep, which results in daytime impairment.2 Approximately 25–50% of the general adult population report infrequent or acute insomnia symptoms, and 6–20% experience chronic insomnia disorder (symptoms persisting for ≥ 3 months).7–11
Co-morbid insomnia and sleep apnea (COMISA) is a prevalent condition that is associated with greater morbidity compared to either insomnia or sleep apnea alone.1 For example, approximately 30–50% of people with OSA report insomnia symptoms, and 30–40% of people with insomnia symptoms have co-morbid OSA.12 People with COMISA report worse sleep,13 daytime function,14,15 mental health16,17 and quality of life,5 compared to people with insomnia alone or OSA alone.18 Furthermore, people with COMISA have worse cardiovascular health compared to people with insomnia alone or neither insomnia nor sleep apnea.19–21 Associations between COMISA and morbidity have been reported using a wide range of diagnostic tools and severity/frequency criteria for both insomnia and OSA.1 Even when COMISA is defined as mild/moderate OSA and less frequent insomnia symptoms (eg ≥5 nights/month), associations with worse mental/physical health persist.20,22–24
Previous studies have investigated independent associations between insomnia and mortality25,26 as well as OSA and mortality27,28 and continuous positive airway pressure therapy and mortality.29 To our knowledge, only two studies have investigated the association between COMISA and all-cause mortality. Using the Sleep Heart Health Study dataset, mortality risk was determined in people with insomnia-alone, OSA-alone, COMISA, or neither disorder, over 15 years of follow-up.30 Insomnia was defined as difficulties initiating and/or maintaining sleep ≥16 nights/month and daytime impairment, and OSA was defined according to an apnea-hypopnea index (AHI) 15≥/hr sleep. COMISA was associated with a 47% increased risk of mortality compared to no insomnia/OSA after controlling for sociodemographic, behavioral factors and chronic conditions. Neither insomnia alone, nor OSA alone, were associated with mortality. However, a single study applying the traditional p<0.05 threshold of significance should not be accepted as absolute truth of a probable relationship between COMISA and mortality.31 A recent study by Sweetman et al used the National Health and Nutrition Examination Survey to investigate the association of COMISA (co-morbid insomnia and high-risk OSA assessed with the STOP-Bang) and mortality, over 11 years of follow-up.32 Among 6877 participants, those in the COMISA group experienced a 56% increased risk of all-cause mortality compared to those with neither insomnia nor high-risk OSA, after controlling for sociodemographic factors, behavioral factors, chronic conditions, and potential mediators. Insomnia alone and OSA alone were not associated with increased mortality risk in fully adjusted models. Replication in independent samples, and with different insomnia and OSA threshold is critical to confirm a probable relationship, and to facilitate future systematic integration of cumulative evidence to inform health research and policy. Indeed, the mean age of the Sleep Heart Health cohort was ~65 years and it is therefore unclear if the previous findings are generalizable to other younger, healthier community samples. Thus, this study sought to determine the relative mortality risk over 19 years of follow-up in individuals with COMISA symptoms, OSA alone or insomnia symptoms alone compared to individuals with neither OSA nor insomnia symptoms in the Wisconsin Sleep Cohort.
Material and Methods
Study Design and Participants
This study used data from the Wisconsin Sleep Cohort (WSC), an ongoing longitudinal study of the consequences of sleep disorders.33–36 The WSC originally recruited ~1500 participants in 1988 from a random sample of employees aged 30–60 years from five Wisconsin state agencies. The data in the current study represent a sub-sample of the original WSC study (n= 1123), accessed through the National Sleep Research Resources37 in September 2021. The protocol, including flow diagram, study design, as well as main results of the Wisconsin Sleep Cohort are available elsewhere.33–36 Accordingly, details below are restricted to those pertinent to the current study. Overnight in-laboratory polysomnography recordings were undertaken by the participant at the University of Wisconsin–Madison Hospital and Clinics. Most sleep studies (88.1%) were conducted prior to 2005, however, a few participants (11.9%) had a sleep study between 2005 and 2014. This report uses de-identified data from a historical cohort study of participants that previously gave informed consent. Hence, this study was exempted from ethical approval (Paragraph 5.1.22 of the Australian National Statement on Ethical Conduct in Human Research).
Insomnia Symptoms Definition
Standardized interviews about sleep quality at the time of the polysomnography sleep study were administered by trained personnel. For the primary definition of insomnia, insomnia symptoms were defined either by the presence of self-reported nocturnal symptoms (difficulties falling asleep, waking up in the middle of the night and having difficulty returning to sleep, and/or waking up too early and being unable to resume sleep; DIMS) at least “often” (≥5 nights/month) or “almost always” (≥16 nights/month); or self-reported regular use of sedative-hypnotic medicine use (yes/no). While a definition including chronic (≥3 months) nocturnal symptoms on at least 16 nights per month, and associated daytime impairments would most accurately reflect “chronic insomnia” criteria,2 data on insomnia “chronicity” was unavailable and there were insufficient cases to reliably investigate associations with mortality when using more conservative symptom frequency criteria (See Supplementary Table 2). Importantly, our operationalization of insomnia symptoms is similar to previous studies investigating the prevalence and associations of COMISA symptoms in population-based and sleep clinic cohorts.20,22–24
We also conducted several sensitivity analyses to investigate associations of COMISA symptoms and mortality according to more conservative definitions of insomnia symptoms including removal of the “sedative-hypnotic use” criterion, increasing the nocturnal insomnia symptom threshold to at least 16 nights per month, and defining insomnia according to the presence of both nocturnal and daytime impairments. Daytime impairment was considered present if the participant answered “often” or “almost always” to the question: “How often do you not feel rested during the day no matter how many hours of sleep you had?” (Never [Never], Rarely [Once a month], Sometimes [1–5 times a month], Often [5–15 times a month], or Almost always [16–30 times a month]). Supplementary Table 2 includes the number of exposure cases and mortality events per group when using the primary and sensitivity definitions of insomnia symptoms.
Obstructive Sleep Apnea Definition
Sleep and respiratory events were scored according to standard criteria at the time of testing.38 Apnea was defined as cessation of airflow for ≥ 10 seconds and hypopnea was defined as a discernible reduction in breathing with a reduction in oxyhemoglobin saturation ≥ 4%. The average number of apnea and hypopnea events per hour of sleep (apnea-hypopnea index, AHI) was calculated to define OSA according to an AHI of ≥5 events/h sleep. Alternative cut-offs (≥10 and 15 events per hour) were investigated in secondary analyses. In addition, OSA was characterized as “symptomatic” or “asymptomatic” based on self-reported daytime impairment (similar question used for insomnia). Percentage of total sleep time with less than 90% of oxygen saturation were also used to characterize nocturnal hypoxia.
COMISA Definition
COMISA was defined if both insomnia symptoms and OSA were present. Participants who did not meet criteria for either insomnia symptoms or OSA were categorized with no insomnia symptoms/OSA (control).
Outcome Assessment
Deaths from any cause, up until 2020, were identified by matching social security numbers with 2 death record sources: the US Social Security Death Index and the Wisconsin State Bureau of Health Information and Policy, Vital Records Section. More information on data matching is available elsewhere.33 Only the year of death was available through the National Sleep Research Resources. The time to event was defined as the time difference between the sleep study and the date of death.
Covariates
At the time of the polysomnography study, participants were asked about lifestyle, sleep habits, and medical history. Weight, height, and blood pressure were assessed. A wide range of covariates were collected (all of which are available for browsing here: https://sleepdata.org/datasets/wsc/variables) during the initial study, and few covariates were retained for statistical analysis, based on previous literature.30 The retained covariates and their definitions and are presented in Supplementary Table 1. Depression symptoms score were assessed using the Zung depression scale (score range from 20 to 100).39 Anxiety symptoms score were assessed using the Trait Anxiety questionnaire (score range from 20 to 80).40
Statistical Analysis
Distributions of covariates were summarized by sleep disorder group. Differences in covariates between sleep disorder groups were examined using unadjusted logistic or linear regression, as appropriate. Kaplan-Meier survival estimates were analysed for visual interpretation of the crude probability of mortality over time. Cox regression models were conducted to assess all-cause mortality risk of a sleep disorder group compared to control (absence of either sleep disorder). Results are summarized using hazard ratios (HRs) and 95% confidence intervals (CIs). Four models were constructed to further explore the impact of potential confounders. Models’ confounders were chosen based on previous studies that investigated the association between COMISA and mortality,30 OSA and mortality,27,33 and insomnia and mortality.26 The first model was unadjusted. The second model was adjusted for socio-demographic factors, including age, race, sex, and the highest education level completed. The third model was additionally adjusted for body mass index, smoking status and alcohol intake. The fourth model was additionally adjusted for potential mediators including pre-existing cardio-metabolic conditions (diabetes, cardiovascular disease, hypertension), anti-depressant medication, and polysomnography-derived total sleep time. The fifth model additionally controlled for anxiety and depression symptoms. The main model of interest was Model 3, given that Models 4 and 5 adjusted for additional covariates that are potential mediators of sleep disorder group on mortality, which may have confounded effect estimates.
Sensitivity Analysis
Most sleep studies (~88%) were conducted before 2005, however, to further validate our findings and to account for different year of baseline sleep study, we conducted a sensitivity analysis by removing any participants with a baseline PSG after 2005 (N = 132). We conducted an additional sensitivity analysis removing participants that died within the first 3 years (N=18) of follow-up to minimize the influence of terminal illnesses and pre-existing conditions. We conducted a third sensitivity analysis that removed participants with sleep apnea treatment at baseline (N = 112). Finally, we conducted a fourth sensitivity analysis by further adjusting for percentage of total sleep time spent with less than 90% of oxygen saturation, to further control for potentially worse nocturnal hypoxia in participants with COMISA.
Results
Baseline Characteristics
A total of 1115 participants were available for the final analysis after exclusion of eight participants due to missing values for education status. The median of follow-up time was 19 years (range: 0 to 20 years). The baseline characteristics of participants with insomnia symptoms alone (17.2%), OSA alone (34.2%), COMISA (19.3%), and neither disorder (29.3%, control) are shown in Table 1. A total of 52.2% of all participants with insomnia symptoms had co-morbid OSA, and 36% of all participants with OSA had co-morbid insomnia symptoms. Participants with COMISA or OSA alone had lower polysomnography total sleep time compared to the control group (Table 1), but there was no evidence of differences in total sleep time between the three sleep disorder groups (all p-values > 0.20).
 |
Table 1 Baseline Characteristics |
Cardiometabolic and Mental Health Conditions
Cardiovascular disease was more common in participants with COMISA symptoms (ORs [95% CI]; 2.28 [1.28, 4.07]) and to some extent OSA alone (1.68 [0.98, 2.89]), but not insomnia symptoms alone (1.08 [0.54, 2.17]) compared to control (no OSA or insomnia symptoms). There was no evidence of a difference in cardiovascular disease prevalence between participants with OSA alone and COMISA (p-value = 0.237). Both OSA alone and COMISA symptoms were associated with a greater prevalence of cardiovascular disease at baseline compared to insomnia symptoms alone (both p-values < 0.001). Compared to the control group, hypertension was more prevalent in participants with COMISA symptoms (2.04 [1.41, 2.96]) and OSA alone (1.85 [1.34, 2.56]). Diabetes was also more prevalent in COMISA symptoms (2.97 [1.68, 5.25]) and OSA alone (2.26 [1.33, 3.86]) compared to the control group.
Compared to the control group, participants with OSA alone did not have higher anxiety scores on the Trait scale (β [95% CI], 0.03 [−1.2, 1.3]) or depression scores on the Zung index (0.9 [−0.3, 2.1]). However, anxiety and depression symptoms scores were increased in both the insomnia symptoms alone (anxiety: 4.0 [2.5, 5.5], depression: 4.4 [3.0, 5.9]) and COMISA symptoms groups (anxiety: 2.8 [1.4, 4.3], depression: 5.5 [4.1, 6.9]), compared to the control group. Those with insomnia symptoms alone and COMISA symptoms had higher anxiety scores and higher depression scores, compared to participants with OSA alone (p-values <0.001).
All-Cause Mortality
The crude mortality rate was larger for the COMISA symptoms group (9.5 deaths/1000 participant years) compared to insomnia symptoms alone (4.5), OSA alone (5.2), or control groups (4.0). Kaplan-Meier curves also suggested a lower survival probability for participants with COMISA symptoms compared to control, insomnia symptoms or OSA groups (Figure 1). In the unadjusted Cox-model, the COMISA group had a 2.3-fold increase in all-cause mortality risk compared to the control group (Table 2). COMISA symptoms were associated with increased risk of all-cause mortality compared to control after adjustment for socio-demographic factors (HR 95% CI; 1.89 [1.11, 3.20]), behavioral factors (1.71 [1.00, 2.93]; primary model of interest), and chronic conditions and potential mediators (1.71 [1.00, 2.97]), but not when additionally controlling for mental health symptoms (1.63 [0.94, 2.82]; Table 2). Neither insomnia symptoms alone nor OSA alone were associated with all-cause mortality compared to the control group in any crude or adjusted models. Furthermore, the COMISA symptoms group had an 89% (1.89 [1.17, 3.06]) increase in mortality risk compared to OSA-alone and a marginal 68% (1.68 [0.91, 3.10]) increase compared to insomnia symptoms alone in model 3 (primary model).
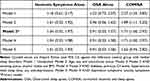 |
Table 2 Associations Between Sleep Disorder Group and All-Cause Mortality |
 |
Figure 1 Unadjusted Kaplan-Meier curve across sleep disorder categories for all-cause mortality. Abbreviations: OSA, Obstructive sleep apnea; COMISA, co-morbid insomnia and sleep apnea. |
Increasing the AHI threshold to define OSA beyond 5 events/h did not change the main findings (Table 3). COMISA defined using an AHI cut-off of either ≥10 or ≥15 events/h was associated with a 1.86 (1.09, 3.19) and 1.86 (1.02, 3.41)-fold increase in mortality risk respectively compared to the control group (Table 3). However, insomnia symptoms defined without the sedative-hypnotic criterion reduced the apparent prevalence of insomnia symptoms and of COMISA, but only marginally attenuated the mortality risk in the COMISA symptoms group compared to the control group (1.66 [0.97, 2.83]). Other definitions of insomnia (inclusion of daytime impairments and increasing the frequency of nocturnal insomnia symptoms to at least 16/month) did not change the main findings (Table 3). More conservative definitions of OSA and insomnia symptoms should be interpreted with caution, due to the lower number of deaths in the COMISA symptoms group for these secondary analyses (Supplementary Table 2). When OSA was further categorized as “symptomatic” and “asymptomatic”, no associations were observed with all-cause mortality compared to control (Table 3), although care should be taken in the interpretation of these findings given that there were only 71 patients with symptomatic OSA and 8 deaths (Supplementary Table S2). Further adjusting for % of total sleep time spent with less than 90% of oxygen in Model 4 did not change the main findings. In this model, COMISA remained associated with mortality (HR 95% CI; 1.73 [1.00, 3.00]). OSA (0.92 [0.53; 1.60]) and insomnia-alone (1.05 [0.55, 2.00]) were not associated with increased mortality risk. The findings remained the same in sensitivity analysis once the 132 participants (11.8%) who had a polysomnography after 2006 were removed (Supplementary Table S3). Similar results were also observed when participants that died within the first 3 years were excluded (Supplementary Table S4). The effect also remained relatively similar when participants using sleep apnea treatment at baseline were excluded, although with wider 95% CIs (Supplementary Table S5).
 |
Table 3 Adjusted Associations Between Sleep Disorder Group and All-Cause Mortality |
Discussion
Co-morbid insomnia symptoms and sleep apnea (COMISA) at baseline was associated with increased risk of all-cause mortality over 19 years of follow-up compared to insomnia symptoms alone, OSA alone, and the absence of either disorder. The association between COMISA symptoms and mortality persisted after controlling for sociodemographic factors, behavioral factors, and chronic conditions, and remained quite consistent across multiple definitions of insomnia and OSA. These findings support previous reports that COMISA is associated with impaired sleep, mental health, physical health, quality of life and longevity.12,30
The results of the current study are consistent with our recent work that indicated that COMISA is associated with a 47–56% increase in all-cause mortality risk compared to no insomnia/OSA30,32 in the Sleep Heart Health Study and National Health and Nutrition Examination Survey cohorts. Participants in the WSC sample were younger and relatively healthy at baseline compared to the Sleep Heart Health Study cohort, and slightly older than the National Health and Nutrition Examination Survey cohort. Furthermore, our previous analyses of mortality outcomes used definitions of insomnia that included both frequent nocturnal insomnia symptoms and daytime impairment, that may more closely reflect diagnostic criteria. This may explain the larger prevalence of COMISA symptoms in the current study compared to our earlier reports in the Sleep Heart Health Study and National Health and Nutrition Examination Survey data. Indeed, daytime impairments were not included in the primary definition of insomnia in the present study. However, sensitivity analyses suggested that inclusion of daytime impairment in the definition of insomnia did not substantially change the main findings. Taken together, these three studies suggest that COMISA is consistently associated with all-cause mortality with robust associations across multiple definitions of insomnia and OSA frequency and severity.
Previous cross-sectional studies have reported that COMISA is associated with increased rates of cardiovascular events compared to insomnia alone or controls.19–21,41 Indeed, we observed that the COMISA symptoms and OSA alone groups generally had higher rates of hypertension, diabetes, and cardiovascular events compared to the insomnia alone or control group. A recent paper by Lechat et al used the Sleep Heart Health Study cohort to investigate the association between COMISA with prevalent cardiovascular disease and incident cardiovascular events.21 COMISA was associated with increased odds of cardiovascular disease at baseline, and a two-fold increase in incident cardiovascular events over 11-years of follow-up, compared to participants with neither insomnia nor OSA. However, COMISA was not associated with incident cardiovascular events in fully controlled models. Furthermore, consistent with previous literature, we also observed more severe depression and anxiety symptoms in the COMISA, and insomnia symptoms alone groups compared to the OSA alone or control groups.16,19 It is likely that mental health symptoms mediate the relationship between COMISA and mortality.16,42 Insomnia and OSA are longitudinally associated with worse mental health, and treatment of sleep disorders improves mental health.42–44 Indeed, the association between COMISA and mortality was no longer significant in model 5 which additionally controlled for depression and anxiety symptoms as a potential mediator. Future research should investigate the effect of COMISA treatment including CBTi,45 CPAP therapy,29 and surgical interventions46 on reducing potential mediators of mortality risk such as mental health symptoms.47
OSA was defined according to several thresholds. Previous COMISA studies have adopted a range of AHI scoring criteria and thresholds to define OSA.1 In this study, we found an association between COMISA and all-cause mortality with OSA defined as AHI ≥ 5, 10, and 15 events per hour of sleep. Hypopneas were defined according to more stringent criteria in the current study (≥ 4% oxygen desaturation), compared the Sleep Heart Health Study report, which relied on the more recent ≥ 3% desaturation (or arousal) criterion for defining hypopneas.27 AHI calculated using a ≥ 4% cut-off is usually between 5 to 10 events per hour lower than AHI calculated using a ≥ 3% oxygen cut-off.48 Therefore, our results are consistent with the previous study suggesting an increased mortality risk in participants with co-morbid insomnia and moderate OSA compared to control.30 Our results that OSA-alone, with or without daytime impairment, is not associated with all-cause mortality is somewhat surprising given that previous studies, including from the WSC, have reported associations between OSA and all-cause mortality.27,33,49 However, these previous reports usually only found an association between moderate and severe OSA and all-cause mortality,33,49 and sometimes only in men.27 In this study, we did not have the power to further categorize OSA as moderate and severe and to test for a sex-interaction effect. Furthermore, these previous studies did not control for insomnia symptoms, and thus COMISA was not accounted for. It is possible that the association between COMISA and mortality may be partially explained by more severe OSA, through increased cardiovascular responses to apneic events,50,51 high levels of hypoxia,52 sleep fragmentation,53,54 or other co-morbidities. Future research trials should investigate the contribution of each to these OSA traits and clinical phenotypes to the increased mortality risk. Finally, the increase in mortality risk for people with COMISA, including in this study, has only been investigated in general population studies.30,32 Future studies should investigate association between COMISA and health outcomes in sleep clinic populations.
After removing 112 participants with positive airway pressure use at baseline, there was an association between COMISA and mortality in the unadjusted model, but not after adjusting for co-variates. As OSA treatment may be protective against mortality risk,55 this is somewhat surprising. Attenuation of the relationship between COMISA and mortality may have been due to the reduction in sample size, or more complex relationships between rates of positive airway pressure therapy acceptance, use and rejection/survival between people with OSA alone and COMISA.1 Future studies should investigate the effect of nightly positive airway pressure use, other OSA therapies, and insomnia treatment on the association of COMISA and mortality.
The findings of this study highlight the importance of routinely screening for insomnia symptoms in sleep clinics that current specialize in the diagnosis and management of OSA-alone, and to develop more effective and tailored treatment approaches for patients with COMISA. Current evidence suggests that combining targeted treatments for each disorder results in the best overall treatment outcomes in people with COMISA.1,56 Cognitive behavioral therapy for insomnia is the recommended “first line” treatment for insomnia,57 is effective in the presence of un-treated OSA, and may improve subsequent acceptance and long-term use of positive airway pressure therapy.18 Positive airway pressure therapy is the most effective treatment for moderate and severe OSA, and improves co-morbid insomnia symptoms in a sub-sample of people with COMISA.12 Future studies should investigate the potential effect of combination treatment approaches for COMISA on improving mental and physical health outcomes.
Limitations
This study should be interpreted in light of several limitations. Although a higher frequency of nocturnal insomnia symptoms, associated daytime impairments, and information about chronicity of insomnia symptoms would have reflected conservative diagnostic criteria for “chronic insomnia”, these data were either unavailable, or reduced the size of the COMISA group to the point where there were insufficient outcome cases available for reliable analysis and interpretation of associations with mortality. Furthermore, given previous COMISA literature reporting associations with worse physical and mental health when using less conservative insomnia criteria,20,22–24 we sought to determine if associations between COMISA and mortality were also present when defining insomnia according to different criteria and threshold. Consequently, a threshold of nocturnal insomnia symptoms on at least five nights per month (associated with a frequency descriptor of “Often”) and/or regular sedative-hypnotic use was selected as the primary definition of insomnia symptoms. In this study, associations with mortality persisted for several more conservative “insomnia symptom” definitions, however these were based on very few deaths (See Table S2).
Regular use of sedative-hypnotic medicines was used to define insomnia symptoms and ~20% of participants with COMISA/insomnia reported using sedative medication. Use of sleeping medication has also been used to define insomnia in a previous report from the Sleep Heart Health Study.26 It is possible that some people in our study were using sedative or hypnotic medicines for indications other than insomnia (eg, anxiety, epilepsy, muscle spasms). A sensitivity analyses indicated that the association between COMISA and mortality was attenuated to non-significance after removing the “sedative hypnotic” criterion from the insomnia symptoms definition, likely due to a reduced number of participants (and deaths) in the COMISA group (Table 2).
Furthermore, OSA was defined based using an AHI measured on a single night. There is increased evidence that OSA is highly variable from night-to-night, which may have induced some noise in the association between COMISA, OSA-alone and all-cause mortality.6,58 Finally, racial-ethnic sleep disparities have been reported in others cohorts59 and our results remain to be validated in a more diverse population than the one presented in this study.
Conclusions
This study found that people with co-morbid insomnia symptoms and sleep apnea are at increased risk of all-cause mortality compared to people without either sleep disorder. Insomnia symptoms alone and OSA alone were not associated with increased mortality risk. It is important to investigate mechanisms contributing to worse mental and physical health in people with COMISA, and to develop more effective treatments for this prevalent and debilitating condition.
Acknowledgments
The authors gratefully acknowledge the prior work and open-data resources made available through the National Sleep Research Resources. The Wisconsin Sleep Cohort Study was supported by the US National Institutes of Health, National Heart, Lung, and Blood Institute (R01HL62252), National Institute on Aging (R01AG036838, R01AG058680), and the National Center for Research Resources (1UL1RR025011). The National Sleep Research Resource was supported by the US National Institutes of Health, National Heart Lung and Blood Institute (R24 HL114473, 75N92019R002). DJE is supported by a National Health and Medical Research Council of Australia (NHMRC) Senior Research Fellowship (1116942) and an Investigator Grant (1196261).
Author Contributions
All authors have contributed to the study design, data analysis and interpretation, and drafting of the manuscript. All authors have contributed and approved the final version of the manuscript. All authors agree to take responsibility and be accountable for the contents of the article.
Disclosure
Outside the submitted work, AS, RA, AV and NL have received research grant funding and equipment from ResMed and Philips Respironics. Outside the submitted work, PC and NL have received research funding from Defence Science and Technology and research grant funding and equipment from Philips Respironics. NL and HS have received research funding from Re-Timer Pty. Ltd. Outside the submitted work, DJE has a Collaborative Research Centre (CRC-P) Grant, a consortium grant between the Australian Government, Academia and Industry (Industry partner: Oventus Medical) and has research grants from Bayer, Apnimed, Invicta Medical and Takeda and serves on the Scientific Advisory Boards for Invicta Medical and Apnimed. None of the other authors have any relevant conflicts to declare. Outside the submitted work, ACR has received research funds from the Australian Sleep Health Foundation, Compumedics and consultancy fees from Sealy Australia.
References
1. Sweetman A, Lack LC, Catcheside PG, et al. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev. 2017;33:28–38. doi:10.1016/j.smrv.2016.04.004
2. The American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3), Diagnostic and Coding Manual.
3. Berry RB, Brooks R, Gamaldo C, et al. AASM scoring manual updates for 2017 (Version 2.4). J Clin Sleep Med. 2017;13(5):665–666. doi:10.5664/jcsm.6576
4. Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118(2):372–379. doi:10.1378/chest.118.2.372
5. Björnsdóttir E, Keenen BT, Eysteinsdottir B, et al. Quality of life among untreated sleep apnea patients compared with the general population and changes after treatment with positive airway pressure. J Sleep Res. 2014;24:328–338. doi:10.1111/jsr.12262
6. Lechat B, Naik G, Reynolds A, et al. Multinight prevalence, variability, and diagnostic misclassification of obstructive sleep apnea. Am J Respir Crit Care Med. 2022;205(5):563–569. doi:10.1164/rccm.202107-1761OC
7. Reynolds A, Appleton S, Gill T, Adams R. Chronic insomnia disorder in Australia: a report to the Sleep Health Foundation. Sleep Health Foundation Special Report; 2019.
8. Ohayon M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi:10.1053/smrv.2002.0186
9. Ohayon MM, Reynolds CF. Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD). Sleep Med. 2009;10:952–960. doi:10.1016/j.sleep.2009.07.008
10. Riemann D, Benz F, Dressle RJ, et al. Insomnia disorder: state of the science and challenges for the future. J Sleep Res. 2022;31(4):e13604. doi:10.1111/jsr.13604
11. Baglioni C, Altena E, Bjorvatn B, et al. The European academy for cognitive behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. 2020;29(2):e12967. doi:10.1111/jsr.12967
12. Sweetman A, Lack L, McEvoy RD, et al. Bi-directional relationships between co-morbid insomnia and sleep apnea (COMISA). Sleep Med Rev. 2021;60:101519. doi:10.1016/j.smrv.2021.101519
13. Bianchi M, Williams K, McKinney S, Ellenbogen J. The subjective-objective mismatch in sleep perception among those with insomnia and sleep apnea. J Sleep Res. 2013;22(5):557–568. doi:10.1111/jsr.12046
14. Sweetman A, Lack L, Lambert S, Gradisar M, Harris J. Does co-morbid obstructive sleep apnea impair the effectiveness of cognitive and behavioral therapy for insomnia? Sleep Med. 2017;39:38–46. doi:10.1016/j.sleep.2017.09.003
15. Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923–1929. doi:10.1378/chest.120.6.1923
16. Jeon B, Luyster FS, Callan JA, Chasens ER. Depressive symptoms in comorbid obstructive sleep apnea and insomnia: an integrative review. West J Nurs Res. 2021;193945921989656. doi:10.1177/0193945921989656
17. Lang CJ, Appleton SL, Vakulin A, et al. Co‐morbid OSA and insomnia increases depression prevalence and severity in men. Respirology. 2017;22:1407–1415. doi:10.1111/resp.13064
18. Sweetman A, Lack L, Bastien C. Co-Morbid Insomnia and Sleep Apnea (COMISA): prevalence, consequences, methodological considerations, and recent randomized controlled trials. Brain Sci. 2019;9(12):371. doi:10.3390/brainsci9120371
19. Sweetman A, Melaku Y, Lack L, et al. Prevalence and associations of co-morbid insomnia and sleep apnoea (COMISA) in an Australian population-based sample. Sleep Med. 2021;82:9–17. doi:10.1016/j.sleep.2021.03.023
20. Vozoris NT. Sleep apnea-plus: prevalence, risk factors, and association with cardiovascular diseases using United States population-level data. Sleep Med. 2012;13(6):637–644. doi:10.1016/j.sleep.2012.01.004
21. Lechat B, Appleton S, Melaku YA, et al. The association of co-morbid insomnia and sleep apnea with prevalent cardiovascular disease and incident cardiovascular events. J Sleep Res. 2022:e13563. doi:10.1111/jsr.13563
22. Hayley AC, Williams LJ, Venugopal K, Kennedy GA, Berk M, Pasco JA. The relationships between insomnia, sleep apnoea and depression: findings from the American national health and nutrition examination survey, 2005–2008. Aust N Z J Psychiatry. 2015;49(2):156–170. doi:10.1177/0004867414546700
23. Chung KF. Insomnia subtypes and their relationships to daytime sleepiness in patients with obstructive sleep apnea. Respiration. 2005;72(5):460–465. doi:10.1159/000087668
24. Krell SB, Kapur VK. Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath. 2005;9(3):104–110. doi:10.1007/s11325-005-0026-x
25. Lovato N, Lack L. Insomnia and mortality: a meta-analysis. Sleep Med Rev. 2019;43:71–83. doi:10.1016/j.smrv.2018.10.004
26. Bertisch SM, Pollock BD, Mittleman MA, et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep. 2018;41:6. doi:10.1093/sleep/zsy047
27. Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6(8):e1000132. doi:10.1371/journal.pmed.1000132
28. Butler MP, Emch JT, Rueschman M, et al. Apnea-hypopnea event duration predicts mortality in men and women in the Sleep Heart Health Study. Am J Respir Crit Care Med. 2019;199(7):903–912. doi:10.1164/rccm.201804-0758OC
29. Adegunsoye A, Neborak JM, Zhu D, et al. CPAP adherence, mortality, and progression-free survival in interstitial lung disease and OSA. Chest. 2020;158(4):1701–1712. doi:10.1016/j.chest.2020.04.067
30. Lechat B, Appleton S, Melaku YA, et al. Co-morbid insomnia and obstructive sleep apnoea is associated with all-cause mortality. Eur Respir J. 2021;60:2101958.
31. Nosek BA, Hardwicke TE, Moshontz H, et al. Replicability, robustness, and reproducibility in psychological science. Annu Rev Psychol. 2022;73:719–748. doi:10.1146/annurev-psych-020821-114157
32. Sweetman A, Lechat B, Appleton S, Reynolds A, Adams R, Melaku YA. Association of co-morbid insomnia and sleep apnoea symptoms with all-cause mortality: analysis of the NHANES 2005–2008 data. Sleep Epidemiol. 2022;2:100043.
33. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–1078.
34. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–1384. doi:10.1056/NEJM200005113421901
35. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi:10.1056/NEJM199304293281704
36. Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009;108(5):246–249.
37. Dean DA 2nd, Goldberger AL, Mueller R, et al. Scaling up scientific discovery in sleep medicine: the national sleep research resource. Sleep. 2016;39(5):1151–1164. doi:10.5665/sleep.5774
38. American Academy of Sleep Medicine Task Force. Sleep–related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22(5):667–689. doi:10.1093/sleep/22.5.667
39. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi:10.1001/archpsyc.1965.01720310065008
40. Spielberger CD. State-Trait Anxiety Inventory: Bibliography (2nd ed.). Palo Alto, CA: Consulting Psychologists Press; 1983.
41. Luyster FS, Kip KE, Buysse DJ, Aiyer AN, Reis SE, Strollo PJ Jr. Traditional and nontraditional cardiovascular risk factors in comorbid insomnia and sleep apnea. Sleep. 2014;37(3):593–600. doi:10.5665/sleep.3506
42. Sweetman A, Lack L, Van Ryswyk E, et al. Co-occurring depression and insomnia in Australian primary care: recent scientific evidence. Med J Aust. 2021;215(5):230–236. doi:10.5694/mja2.51200
43. Edwards C, Almeida OP, Ford AH. Obstructive sleep apnea and depression: a systematic review and meta-analysis. Maturitas. 2020;142:45–54. doi:10.1016/j.maturitas.2020.06.002
44. McEvoy RD, Antic NA, Heeley E, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–931. doi:10.1056/NEJMoa1606599
45. Sweetman A, Lovato N, Micic G, et al. Do symptoms of depression, anxiety or stress impair the effectiveness of cognitive behavioural therapy for insomnia? A chart-review of 455 patients with chronic insomnia. Sleep Med. 2020;75:401–410. doi:10.1016/j.sleep.2020.08.023
46. Iannella G, Lechien JR, Perrone T, et al. Barbed reposition pharyngoplasty (BRP) in obstructive sleep apnea treatment: state of the art. Am J Otolaryngol. 2022;43(1):103197.
47. Sweetman A, Adams RJ. Comorbid insomnia and sleep apnea as a potential predictor of suicide and self-harm. Commentary on Udholm et al. Obstructive sleep apnea and risk of suicide and self-harm: a Danish Nationwide Cohort Study. Sleep. 2022;45(6). doi:10.1093/sleep/zsac043
48. Duce B, Milosavljevic J, Hukins C. The 2012 AASM respiratory event criteria increase the incidence of hypopneas in an adult sleep center population. J Clin Sleep Med. 2015;11(12):1425–1431. doi:10.5664/jcsm.5280
49. Marshall NS, Wong KKH, Cullen SRJ, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study Cohort. J Clin Sleep Med. 2014;10(04):355–362. doi:10.5664/jcsm.3600
50. Azarbarzin A, Sands SA, Younes M, et al. The sleep apnea-specific pulse rate response predicts cardiovascular morbidity and mortality. Am J Respir Crit Care Med. 2021;203:1546–1555. doi:10.1164/rccm.202010-3900OC
51. Kwon Y, Wiles C, Parker BE, et al. Pulse arrival time, a novel sleep cardiovascular marker: the multi-ethnic study of atherosclerosis. Thorax. 2021;76(11):1124–1130. doi:10.1136/thoraxjnl-2020-216399
52. Azarbarzin A, Sands SA, Stone KL, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the osteoporotic fractures in Men Study and the Sleep Heart Health Study. Eur Heart J. 2019;40(14):1149–1157. doi:10.1093/eurheartj/ehy624
53. Lechat B, Hansen KL, Melaku YA, et al. A novel electroencephalogram-derived measure of disrupted delta wave activity during sleep predicts all-cause mortality risk. Ann Am Thorac Soc. 2022;19(4):649–658. doi:10.1513/AnnalsATS.202103-315OC
54. Lechat B, Scott H, Naik G, et al. New and emerging approaches to better define sleep disruption and its consequences. Front Neurosci. 2021;15:751730. doi:10.3389/fnins.2021.751730
55. Pepin JL, Bailly S, Rinder P, et al. Relationship between CPAP termination and all-cause mortality: a French nationwide database analysis. Chest. 2022;161(6):1657–1665. doi:10.1016/j.chest.2022.02.013
56. Ong JC, Crawford MR, Wallace DM. Sleep apnea and insomnia: emerging evidence for effective clinical management. Chest. 2020;159:2020–2028. doi:10.1016/j.chest.2020.12.002
57. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2016;165(2):125. doi:10.7326/M15-2175
58. Punjabi NM, Patil S, Crainiceanu C, Aurora RN. Variability and misclassification of sleep apnea severity based on multi-night testing. Chest. 2020;158(1):365–373. doi:10.1016/j.chest.2020.01.039
59. Chung J, Goodman M, Huang T, et al. Racial-ethnic differences in actigraphy, questionnaire, and polysomnography indicators of healthy sleep: the Multi-Ethnic Study of atherosclerosis. Am J Epidemiol. 2021. doi:10.1093/aje/kwab232
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
