Back to Journals » Journal of Inflammation Research » Volume 16
Age–Bilirubin–International Normalized Ratio (INR)–Creatinine (ABIC) Score, a Potential Prognostic Model for Long-Term Mortality of CAD Patients After PCI
Authors Wu TT, Pan Y, Zheng YY, Yang Y, Hou XG, Deng CJ, Ma YT, Xie X
Received 22 October 2022
Accepted for publication 30 December 2022
Published 26 January 2023 Volume 2023:16 Pages 333—341
DOI https://doi.org/10.2147/JIR.S394502
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Adam D Bachstetter
Ting-Ting Wu,* Ying Pan,* Ying-Ying Zheng, Yi Yang, Xian-Geng Hou, Chang-Jiang Deng, Yi-Tong Ma, Xiang Xie
Department of Cardiology, First Affiliated Hospital of Xinjiang Medical University, Urumqi, 830054, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yi-Tong Ma; Xiang Xie, Department of Cardiology, First Affiliated Hospital of Xinjiang Medical University, Urumqi, 830054, People’s Republic of China, Tel/Fax +86-991-4366893, Email [email protected]; [email protected]
Background: Given that age, international normalized ratio (INR), total bilirubin, and creatinine are reported to be independent risk factors for predicting outcome in patients with coronary artery disease (CAD), it is possible that the age–bilirubin–INR–creatinine (ABIC) score might be a potential prognostic model for patients with CAD.
Methods: A total of 6046 CAD patients after percutaneous coronary intervention (PCI) from the retrospective cohort study (Identifier: ChiCTR-ORC-16010153) were evaluated finally. The primary outcome long-term mortality and secondary endpoints mainly major adverse cardiovascular and cerebrovascular events (MACCEs) were recorded. Multivariate Cox regression models were used to determine risk factors for mortality and MACCEs.
Results: The ABIC score was significantly higher in the death group than in the survival group. After adjusting for other CAD risk factors, the ABIC score was identified to be an independent risk factor for long-term mortality by multivariate Cox analysis. When in the high ABIC group, the incidence of all-cause mortality would increased 1.7 times (adjusted HR=1.729 (1.347– 2.218), P< 0.001), and 1.5 times for cardiac death (adjusted HR=1.482 (1.126– 1.951), P=0.005).
Conclusion: The present study indicated that ABIC score≥ 7.985 predicts high long-term mortality and cardiac death risk for PCI patients. The ABIC score might be a potential prognostic model for patients with PCI.
Keywords: age–bilirubin–international normalized ratio–creatinine score, ABIC score, coronary artery disease, mortality, prognosis
Introduction
Cardiovascular disease (CVD) is considered as the leading cause of death (accounting for approximately 31% of all global deaths) and is expected to remain so until 2030.1 Percutaneous coronary interventions (PCI) are increasingly used in patients with coronary artery disease (CAD). Despite the improvement of medical level, CAD is still one of the leading causes of disability and death worldwide, leading to a large consumption of health resources.2 People with cardiovascular disease or who are at high cardiovascular risk (due to the presence of one or more risk factors such as hypertension, diabetes, hyperlipidemia, or already established disease), are considered as a high-risk group and have certain adverse effects on the prognosis of CAD.3–5 There are also several other biomarkers which are useful in CAD, such as serological biomarkers of atherosclerosis as well as genetic and imaging markers.6,7 However, few simple and effective tools are available for determining the prognosis of CAD after PCI and validated in an external data set.
The age–bilirubin–INR–creatinine (ABIC) score, based on age and parameters indicating hepatic function, coagulation, and renal function, was originally proposed as a tool to assess survival in alcoholic hepatitis (AH) and used to identify patients’ responding to corticosteroid therapy.8 It was confirmed by subsequent studies that the ABIC score to be a useful tool that allows the stratification of risk of death in patients with AH at 90 days and 1 year.8,9 It offers a simple and practical method for alcoholic hepatitis and liver failure. Given that age, INR,10,11 total bilirubin,12,13 and creatinine14 are reported to be independent risk factors for predicting outcome in patients with CAD, it is possible that the ABIC score might be a potential prognostic model for patients with CAD. We therefore designed this study with the aim of investigating the value of the ABIC score for predicting the prognosis of CAD patients after PCI based on data collected from our retrospective study.
Methods
Patients in Study Cohort
A total of 6050 CAD patients who underwent PCI in the First Affiliated Hospital of Xin jiang Medical University from January 2008 and December 2016, registered as “The Clinical Outcomes and Risk Factors of patients with Coronary Heart Disease after PCI (CORFCHD-PCI) study”, were included. The details of the design can be found on http://www.chictr.org.cn (Identifier: ChiCTR-ORC-16010153). More details have been described somewhere else.15 Four patients were excluded due to data not available, and 6046 patients with CAD after PCI were finally evaluated. The flow chart of inclusion and exclusion of participants is shown in Figure 1. The ethics committee of the First Affiliated Hospital of Xinjiang Medical University approved the study protocol. Due to the retrospective design of the study, the need to obtain informed consent from eligible patients was waived by the ethics committee.
 |
Figure 1 The flow chart of participant inclusion. |
Definition
We generated the age, serum bilirubin, INR, and serum creatinine to define the ABIC score: (age×0.1)+(serum bilirubin×0.08)+(serum creatinine×0.3)+(INR×0.8). Hypertension was defined as systolic blood pressure of >140 mm/Hg and/or diastolic blood pressure of >90 mm/Hg, measured at least twice or with any anti-hypertensive medication. Diabetes is defined as a fasting blood glucose level of 126 mg/dL as measured multiple times or as currently administered anti-diabetic drugs. Hypercholesterolemia is considered to have serum total cholesterol of >200 mg/dL or to be treated with lipid-lowering drugs. The primary outcome is long-term mortality after PCI. The secondary endpoint was major adverse cardiac and cerebrovascular event (MACCE), which was defined as a combination of stroke, cardiac death, stent thrombosis, recurrent myocardial infarction, and target vessel remodeling. The end date of follow-up for each participant’s primary study was recorded as the date of occurrence of the identified primary or secondary endpoint event, or the end date of follow-up at the participating evaluation center, whichever came first. More details have been described somewhere else.15
Data Collection
Peripheral venous blood samples were taken upon admission. Echocardiogram and laboratory data were recorded, and all variables were measured on fresh samples using an automated, clinically validated collimator. Baseline data including age, sex, history of hypertension and diabetes, smoking, alcohol consumption, and other clinical and demographic characteristics were recorded by two professionals. During follow-up, beta-blocker, angiotensin converting enzyme inhibitor (ACEI), angiotensin II receptor blocker (ARB), statins, aspirin, collateral, and calcium channel blocker (CCB) were recorded. Clinical follow-up data for participating patients were obtained through outpatient examinations and/or telephone interviews with patients or family members.
Statistics Analysis
All analyses were performed using SPSS 22.0 (SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test is used to evaluate the normality of the distribution. Continuous variables with a normal distribution were specified as the mean±standard deviation, and categorical variables were specified with number and percentage. To compare parametric continuous variables, the Student’s t-test was used, and to compare nonparametric continuous variables, the Mann–Whitney U-test was applied. Chi-square (χ2) tests were used to compare the categorical variables. The results were reported as hazard ratios (HRs), together with 95% confidence intervals. Multivariate Cox proportional hazard models were used to determine independent parameters for long-term mortality and MACCE. The cumulative survival curves were constructed using the Kaplan–Meier method for both primary and secondary endpoints and compared using log rank tests. P<0.05 is considered significant.
Results
According to the receiver operating curve (ROC), the best cut-off value was defined as high ABIC score ≥7.985 and low ABIC score <7.985, after which patients were divided into groups with high and low ABIC scores. Numerous variables vary significantly between patients in different ABIC score groups. Participants with higher ABIC score were also elder with additional morbidity of essential hypertension and diabetes mellitus, higher level of blood urea nitrogen (BUN), creatinine (Cr), total bilirubin (TBIL), and INR. There are more males, more likely to drink, smoke, and higher level of uric acid (UA) and triglyceride (TG) in the low ABIC group (Table 1). The primary comparison was long-term mortality, when ABIC score ≥7.985, long-term mortality, and cardiac death incidences occurred more regularly (P<0.001). In total, 309 patients died during follow-up. There was significantly higher mortality in the elevated group compared to that in the lower group with 192 (6.8%) vs 117 (3.6%), cardiac death 148 (5.3%) vs 103 (3.2%) and MACCE 422 (15.0%) vs 440 (13.6%) respectively. However, the frequency of secondary endpoints named MACCEs did not differ significantly between the two groups (Table 2). After adjusting for gender, smoking, drinking, diabetes, hypertension, BUN, UA, and TG, the multivariate Cox proportional hazards model showed that when ABIC score ≥7.985, the incidence of all-cause mortality would be increased 1.7 times (adjusted HR=1.729 (1.347–2.218), P<0.001) (Table 3), and 1.5 times in cardiac death (adjusted HR=1.482 (1.126–1.951), P=0.005) (Table 4). We also found that increased BUN was a weak independent risk factor for predicting long-term death. Using the Kaplan–Meier analysis with the cut off values of 7.985, the ABIC score stratified patients according to their risk of all-cause mortality and cardiac death (Figure 2).
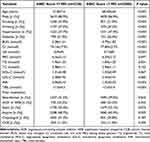 |
Table 1 Baseline Characteristics of Study Patients |
 |
Table 2 Long-Term Cardiac Events |
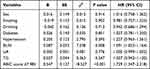 |
Table 3 Cox Regression Analysis Results for Long-Term Mortality |
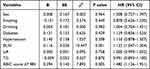 |
Table 4 Cox Regression Analysis Results for Cardiac Death |
 |
Figure 2 Cumulative Kaplan–Meier estimates of the time to the first adjudicated occurrence of all-cause mortality and cardiac death. |
Discussion
The present study indicated that ABIC score ≥7.985 increases the risk of all-cause mortality and cardiac death risk for PCI patients. The ABIC score could be a potential prognostic model for PCI patients. Over the past few decades, cardiovascular disease has become an epidemic. Considering population shift (population growth, aging population) and risk factors are still rising, the burden on CAD is expected to increase more in the future.16 Therefore, the burden of this epidemic must continue to be monitored and useful tools should be established to predict the real needs in terms of staff and infrastructure.17,18 In patients diagnosed with cardiovascular disease, where early detection and management using counseling and medication as appropriate is required, accurate prognostic stratification would undoubtedly be helpful in the clinical management of these patients as well as in the design of clinical trials.
Since Framingham first proposed the need for a cardiovascular risk score, numerous studies have followed to construct a primary score to stratify the risk of CAD and its associated cardiovascular adverse events. Daly et al established a simple score which was constructed using six clinical and investigative variables parameters to discriminate effectively between really low risk and extremely elevated risk patients and to estimate the probability of death or non-fatal myocardial infarction over one year.19 A large multicenter trial was designed to derive a risk score combining 16 routinely available clinical variables for the combination of all-cause mortality, myocardial infarction (MI), and disabling stroke in patients with stable symptomatic angina.20 Based on outcomes in 8557 patients in the LIPID study, a prognostic strategy for quantifying the long-term risk of CAD events in survivors of acute coronary syndromes (ACS) was developed.21 Rapsomaniki et al22 developed a comprehensive model by 102,023 stable coronary artery disease (SCAD) patients from the CALIBER program to predict the poor prognostic. Subsequently, several studies suggested that the age, creatinine, and ejection fraction (ACEF) score to be a prediction model. Lee et al23 suggested the ACEF score to be a novel valid model to stratify the 1-year mortality risk in 30-day survivors who underwent PCI after acute myocardial infarction. In Di Serafino et al's24 and Deng et al’s studies,25 the ACEF score represents a simple tool in the prognostication of patients successfully treated with PCI of coronary chronic total occlusion. ACEF score ≥1.20 was also found to be significantly associated with MACEs in patients with acute coronary syndrome.26 In ST-elevation myocardial infarction patients undergoing primary PCI, the novel ACEF-STEMI score provided strong prognostic value.27
Although the previous models above19–21 had acceptable calibration and discrimination in internal (external) validation for all-cause mortality and non-fatal MI or coronary death, however, there are a variety of parameters that need to be fully considered. Compared with the more complicated model evaluation in previous study, the score described in the current study includes parameters easy to obtain at admission and our validation model is simple, which can quickly identify patients with extreme risk and allow a rapid identification of the prognosis, so as to guide further evaluation or prevention. Unlike the broader population with additional non-CVD comorbidities included in Rapsomaniki et al’s study,22 the population included in our study has more restrictive conditions, thus compared with 20.6% all-cause mortality of patients with SCAD, our all-cause mortality of patients with PCI was significantly lower and our study is more population-specific. In addition, although the ACEF score is simple, however, the previous studies had a limited number of subjects or duration of follow-up, which lowers the confidence sufficiently. Overcoming the limitations, we did determine the efficacy of the ABIC score in a long-term follow-up study of 6046 subjects, providing a reliable tool and new sight for assessing the long-term outcome of PCI patients.
Some mechanisms may explain the association between bilirubin, INR, creatinine, and mortality and cardiac death in PCI patients. Research conducted in the last few decades has revealed that bilirubin, a heme catabolism product with antioxidant, anti-inflammatory, and anti-apoptotic properties, may be implicated in the prognosis of CAD.28,29 Li et al29 performed a meta-analysis, finding that total bilirubin levels were positively correlated with myocardial infarction (MI) severity, and higher total bilirubin levels were associated with a greater odds of adverse outcomes in MI patients. Bilirubin acts as an antioxidant, scavenging peroxyl radicals as efficiently as alpha-tocopherol at concentrations in human plasma. Both free and bound forms of bilirubin can inhibit the oxidation of low-density lipoproteins act as an critical initial step in atherogenesis that can stimulate platelet aggregation and can alter vasomotor properties.30 As CAD is regularly accompanied by an elevated risk of thrombosis and bleeding, it has been revealed by previous studies that its of great significant relationship between prothrombin time–international normalized ratio (PT-INR) level and CAD processes.31,32 Lower PT-INR levels reflect a higher risk of blood clots, while higher PT-INR levels indicate a higher risk of bleeding. The lower risk of bleeding may help limit the formation of bleeding within the plaque, which further stabilizes the atherosclerotic plaque and reduces the risk of cardiovascular events and death. Moreover, the activation of inflammation and blood clotting pathways play a crucial role in the pathogenesis of cardiovascular disease, and they can activate each other and affect the outcome of cardiovascular disease. Inflammation may prolong PT and increase the risk of bleeding, so higher PT-INR may reflect the active state of inflammation. At the same time, activation of the clotting system may also hasten the onset of inflammation and lead to a poor prognosis.33,34 Patients with reduced kidney function are susceptible to cardiovascular disease, due to their own common risk factors, such as old age, diabetes, hypertension, and hyperuricemia. Chronic kidney disease commonly causes patients to develop proteinuria, anemia, metabolic disorders of calcium and phosphorus, diuretic resistance, systemic edema, and cellular edema, which significantly aggravate heart damage. In addition, rapid activation of the angiotensin and aldosterone systems, disturbance of the endothelial system, and oxidation and antioxidant systems are common pathological bases of heart and kidney injury. Heart and kidney injuries can cause each other and the superposition of injuries is amplified.35,36 As serum creatinine levels are the most commonly used measure of kidney function, it may have an influential impact on cardiovascular disease.
Study Limitations
There are some limitations to this study. First, the retrospective design of the study. Second, inflammation markers such as C-reactive protein, brain natriuretic peptide, pro-inflammatory cytokines, angiotensin II, and norepinephrine levels, etc. were not evaluated to address the additional confounding factors. The biggest restriction of this study is that we only used a limited number of individual risk factors to do a model validation, failing to incorporate the “broad range of relevant data” identified as essential in the guidelines, such as sociodemographic characteristics, cardiovascular (CVD) and non-CVD comorbidities, mental health, symptom severity, and clinically available biomarkers. Thus, this can be further clarified by more rigorous multicenter, prospective studies.
Conclusion
Assessment of prognosis is a critical step in evaluating the need for treatment and lifestyle modifications to manage the risk of future coronary events. ABIC score was applicable to the prediction of long-term mortality risk after PCI, when patients are stratified into high and low mortality risk groups, it should then define different investigation and treatment pathways.
Data Sharing Statement
Data of this study were available from the corresponding author upon request.
Ethics Approval and Informed Consent
The ethics committee of the First Affiliated Hospital of Xinjiang Medical University approved the study protocol. The current study complies with the Helsinki Declaration. Due to the retrospective design of the study, the need to obtain informed consent from eligible patients was waived by the ethics committee. The privacy of the participants is maintained with confidentiality.
Consent to Publish
This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal. All authors agree to the publication of this work.
Author Contributions
T-TW and YP drafted the manuscript. Y-YZ and YY, designed the study and provided methodological expertise. X-GH and C-JD drafted the tables and figures and performed the statistical analysis. XX and Y-TM read and approved the final manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (grant No. 82170345).
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi:10.1371/journal.pmed.0030442
2. Steg PG, Bhatt DL, Wilson PW, et al.; REACH Registry Investigators. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297(11):1197–1206. doi:10.1001/jama.297.11.1197
3. Bettinger N, Palmerini T, Caixeta A, et al. Risk stratification of patients undergoing medical therapy after coronary angiography. Eur Heart J. 2016;37(40):3103–3110. doi:10.1093/eurheartj/ehv674
4. Levelt E, Rodgers CT, Clarke WT, et al. Cardiac energetics, oxygenation, and perfusion during increased workload in patients with type 2 diabetes mellitus. Eur Heart J. 2016;37(46):3461–3469. doi:10.1093/eurheartj/ehv442
5. Tada H, Kawashiri MA, Nohara A, Inazu A, Mabuchi H, Yamagishi M. Impact of clinical signs and genetic diagnosis of familial hypercholesterolaemia on the prevalence of coronary artery disease in patients with severe hypercholesterolaemia. Eur Heart J. 2017;38(20):1573–1579. doi:10.1093/eurheartj/ehx004
6. Tibaut M, Caprnda M, Kubatka P, et al. Markers of atherosclerosis: part 1 - serological markers. Heart Lung Circ. 2019;28(5):667–677. doi:10.1016/j.hlc.2018.06.1057
7. Tibaut M, Caprnda M, Kubatka P, et al. Markers of atherosclerosis: part 2 - genetic and imaging markers. Heart Lung Circ. 2019;28(5):678–689. doi:10.1016/j.hlc.2018.09.006
8. Dominguez M, Rincón D, Abraldes JG, et al. A new scoring system for prognostic stratification of patients with alcoholic hepatitis. Am J Gastroenterol. 2008;103(11):2747–2756. doi:10.1111/j.1572-0241.2008.02104.x
9. Chen L, Zheng J, Cai J, et al. Age-bilirubin-international normalized ratio-creatinine score in short-term survival of acute-on-chronic hepatitis B liver failure. Cell Physiol Biochem. 2018;51(5):2484–2495. doi:10.1159/000495904
10. Kerneis M, Yee MK, Mehran R, et al. Association of international normalized ratio stability and bleeding outcomes among atrial fibrillation patients undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2019;12(2):e007124. doi:10.1161/CIRCINTERVENTIONS.118.007124
11. Gajanana D, Rogers T, Iantorno M, et al. Antiplatelet and anticoagulation regimen in patients with mechanical valve undergoing PCI - state-of-the-art review. Int J Cardiol. 2018;264:39–44. doi:10.1016/j.ijcard.2018.03.107
12. Chung SR, Yang TH, Shin HC, et al. Initial total bilirubin and clinical outcome in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention with drug-eluting stents. Circ J. 2016;80(6):1437–1444. doi:10.1253/circj.CJ-15-1397
13. Zhang MM, Gao Y, Zheng YY, et al. Association of fasting serum bilirubin levels with clinical outcomes after percutaneous coronary intervention: a prospective study. Cardiovasc Toxicol. 2017;17(4):471–477. doi:10.1007/s12012-017-9405-3
14. Guo XS, Chen SQ, Duan CY, et al. Association of post-procedural early (within 24h) increases in serum creatinine with all-cause mortality after coronary angiography. Clin Chim Acta. 2017;474:96–101. doi:10.1016/j.cca.2017.08.036
15. Zheng YY, Wu TT, Chen Y, et al. Resting heart rate and long-term outcomes in patients with percutaneous coronary intervention: results from a 10-year follow-up of the CORFCHD-PCI study. Cardiol Res Pract. 2019;2019:5432076. doi:10.1155/2019/5432076
16. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
17. Mezue K, Rangaswami J. Directly observed therapy: a possible tool to tackle medication nonadherence in the CVD epidemic. J Am Coll Cardiol. 2017;69(24):3009. doi:10.1016/j.jacc.2017.02.076
18. Castellano JM, Sanz G, Fernandez Ortiz A, Garrido E, Bansilal S, Fuster V. A polypill strategy to improve global secondary cardiovascular prevention: from concept to reality. J Am Coll Cardiol. 2014;64(6):613–621. doi:10.1016/j.jacc.2014.06.009
19. Daly CA, De Stavola B, Sendon JL, et al.; Euro Heart Survey Investigators. Predicting prognosis in stable angina--results from the Euro heart survey of stable angina: prospective observational study. BMJ. 2006;332(7536):262–267. doi:10.1136/bmj.38695.605440.AE
20. Clayton TC, Lubsen J, Pocock SJ, et al. Risk score for predicting death, myocardial infarction, and stroke in patients with stable angina, based on a large randomised trial cohort of patients. BMJ. 2005;331(7521):869. doi:10.1136/bmj.38603.656076.63
21. Marschner IC, Colquhoun D, Simes RJ, et al.; LIPID Study Investigators. Long-term risk stratification for survivors of acute coronary syndromes. Results from the Long-term Intervention with Pravastatin in Ischemic Disease (LIPID) Study. J Am Coll Cardiol. 2001;38(1):56–63. doi:10.1016/S0735-1097(01)01360-2
22. Rapsomaniki E, Shah A, Perel P, et al. Prognostic models for stable coronary artery disease based on electronic health record cohort of 102 023 patients. Eur Heart J. 2014;35(13):844–852. doi:10.1093/eurheartj/eht533
23. Lee JH, Bae MH, Yang DH, et al.; Korea Acute Myocardial Infarction Registry Investigators. Prognostic value of the age, creatinine, and ejection fraction score for 1-year mortality in 30-day survivors who underwent percutaneous coronary intervention after acute myocardial infarction. Am J Cardiol. 2015;115(9):1167–1173. doi:10.1016/j.amjcard.2015.02.001
24. Di Serafino L, Borgia F, Maeremans J, et al. The age, creatinine, and ejection fraction score to risk stratify patients who underwent percutaneous coronary intervention of coronary chronic total occlusion. Am J Cardiol. 2014;114(8):1158–1164. doi:10.1016/j.amjcard.2014.07.034
25. Deng J, Wang X, Shi Y, Zhao X, Han Y. Prognostic value of the age, creatinine, and ejection fraction score for non-infarct-related chronic total occlusion revascularization after primary percutaneous intervention in acute ST-elevation myocardial infarction patients: a retrospective study. J Interv Cardiol. 2018;31(1):33–40. doi:10.1111/joic.12448
26. Nakahashi T, Tada H, Sakata K, et al. Additive prognostic value of carotid plaque score to enhance the age, creatinine, and ejection fraction score in patients with acute coronary syndrome. J Atheroscler Thromb. 2018;25(8):709–719. doi:10.5551/jat.42317
27. Reindl M, Reinstadler SJ, Tiller C, et al. ACEF score adapted to ST-elevation myocardial infarction patients: the ACEF-STEMI score. Int J Cardiol. 2018;264:18–24. doi:10.1016/j.ijcard.2018.04.017
28. Yao ME, Su MY, Huang Y, Chen W. Physiologically increased total bilirubin is associated with reduced risk of first myocardial infarction: a meta-analysis and dose-response analysis. Nutr Metab Cardiovasc Dis. 2021;31(4):1016–1026. doi:10.1016/j.numecd.2021.01.002
29. Li XL, Zhao CR, Pan CL, Jiang G, Zhang B. Role of bilirubin in the prognosis of coronary artery disease and its relationship with cardiovascular risk factors: a meta-analysis. BMC Cardiovasc Disord. 2022;22(1):458. doi:10.1186/s12872-022-02899-w
30. Neuzil J, Stocker R. Free and albumin-bound bilirubin are efficient co-antioxidants for alpha-tocopherol, inhibiting plasma and low density lipoprotein lipid peroxidation. J Biol Chem. 1994;269(24):16712–16719. doi:10.1016/S0021-9258(19)89449-8
31. Campo G, Pavasini R, Pollina A, Tebaldi M, Ferrari R. Coagulation factors and recurrence of ischemic and bleeding adverse events in patients with acute coronary syndromes. Thromb Res. 2013;132(2):151–157. doi:10.1016/j.thromres.2013.06.007
32. Liu L, Ying M, Chen S, et al. The association between prothrombin time-international normalized ratio and long-term mortality in patients with coronary artery disease: a large cohort retrospective study with 44,662 patients. BMC Cardiovasc Disord. 2022;22(1):297. doi:10.1186/s12872-022-02619-4
33. Dorgalaleh A, Favaloro EJ, Bahraini M, Rad F. Standardization of Prothrombin Time/International Normalized Ratio (PT/INR). Int J Lab Hematol. 2021;43(1):21–28. doi:10.1111/ijlh.13349
34. Levi M, van der Poll T, Büller HR. Bidirectional relation between inflammation and coagulation. Circulation. 2004;109(22):2698–2704. doi:10.1161/01.CIR.0000131660.51520.9A
35. Di Mauro M, Fiorentini V, Mistrulli R, Veneziano FA, De Luca L. Acute coronary syndrome and renal impairment: a systematic review. Rev Cardiovasc Med. 2022;23(2):49. doi:10.31083/j.rcm2302049
36. Sarnak MJ, Amann K, Bangalore S, et al.; Conference Participants. Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74(14):1823–1838. doi:10.1016/j.jacc.2019.08.1017
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
