Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
Acute Exacerbation and Longitudinal Lung Function Change of Preserved Ratio Impaired Spirometry
Authors Yoon SM, Jin KN, Lee HJ, Lee HW , Park TY, Heo EY, Kim DK, Lee JK
Received 18 October 2023
Accepted for publication 15 February 2024
Published 23 February 2024 Volume 2024:19 Pages 519—529
DOI https://doi.org/10.2147/COPD.S445369
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Si Mong Yoon,1 Kwang Nam Jin,2 Hyo Jin Lee,3 Hyun Woo Lee,3 Tae Yun Park,3 Eun Young Heo,3 Deog Kyeom Kim,3 Jung-Kyu Lee3
1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Republic of Korea; 2Department of Radiology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Republic of Korea; 3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Republic of Korea
Correspondence: Jung-Kyu Lee, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, 20 Boramaero-5-Gil, Dongjak-Gu, Seoul, 07061, Republic of Korea, Tel +82-2-870-2235, Email [email protected]
Background: Preserved ratio impaired spirometry (PRISm) is a heterogeneous disease entity. Limited data are available regarding its prevalence, clinical course, or prognosis. We aimed to evaluate the longitudinal clinical course of patients with PRISm compared with chronic obstructive pulmonary disease (COPD).
Methods: A retrospective study enrolled PRISm and COPD patients who underwent chest computed tomography and longitudinal pulmonary function tests between January 2013 and December 2020. We compared the incidence of acute exacerbations and lung function changes between PRISm and COPD patients.
Results: Of the 623 patients, 40 and 583 had PRISm and COPD, respectively. Compared to COPD patients, PRISm patients were younger, more likely to be female and have a history of tuberculosis, and less likely to be smokers. They also had less severe comorbidities, lower forced vital capacity (FVC) and diffusing capacity of the lungs for carbon monoxide (DLCO). The clinical course was not significantly different between the PRISm and COPD patients in terms of the risk of moderate-to-severe acute exacerbations or proportion of frequent exacerbators. During follow-up, PRISm patients had a significantly slower annual decline of forced expiratory volume in 1 second, FVC, and DLCO than COPD patients.
Conclusion: PRISm patients had no significant difference in the risk of acute exacerbations, but a significantly slower decline of lung function during longitudinal follow-up, compared with COPD patients.
Plain Language Summary: We evaluated the longitudinal clinical course of patients with preserved ratio impaired spirometry (PRISm) compared to patients with chronic obstructive pulmonary disease (COPD). PRISm and COPD patients showed no significant differences in the risk of moderate-to-severe acute exacerbations or frequent exacerbations, but the former group showed a significantly slower annual decline of lung function during longitudinal follow-up.
Keywords: preserved ratio impaired spirometry, chronic obstructive pulmonary disease, exacerbation, lung function
Introduction
Preserved ratio impaired spirometry (PRISm) is characterized by a forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio ≥0.7 (or ≥ lower limit of normal) and FEV1 <80% of the predicted normal value.1 PRISm is a heterogenous disease entity with a spirometric pattern not compatible with fixed airflow limitation due to a relative decrease in FVC and was previously defined as “unclassified” by the Global Initiative for Obstructive Diseases (GOLD); it is thus distinct from of chronic obstructive pulmonary disease (COPD).2
The prevalence of PRISm is approximately 10%,1,3,4 and female sex, older age, cigarette exposure, higher body mass index (BMI), diabetes mellitus, and history of tuberculosis (TB) are its risk factors.5,6 PRISm is associated with a reduced quality of life, frequent respiratory complaints and drug use, cardiovascular comorbidities, and hospitalizations for pneumonia.3,7 In particular, compared to individuals with normal spirometry, those with PRISm have higher all-cause and cardiovascular mortality rates.8,9 The long-term prognosis of patients with PRISm depends on longitudinal changes in the spirometric pattern.4,10
Although the long-term prognosis of PRISm differs from that of conventional COPD, few studies have evaluated this. Therefore, we compared the longitudinal disease course between patients with PRISm and COPD.
Methods
Study Population
This retrospective study was conducted at the Seoul Metropolitan Government–Seoul National University Boramae Medical Center, a tertiary referral hospital in South Korea, from January 1, 2013, to December 31, 2020. We enrolled adult patients diagnosed with PRISm (post-bronchodilator FEV1/FVC ratio ≥ 0.7 and FEV1 < 80%) or COPD (post-bronchodilator FEV1/FVC ratio < 0.7) on spirometry. Patients who underwent at least one chest computed tomography (CT) scan and two or more lung function tests were included to evaluate restrictive spirometry-associated structural abnormalities and longitudinal changes in lung function. Patients with a follow-up duration <1 year were excluded. We retrospectively collected blood test results performed within 6 months of each participant’s initial study date. The analysis focused on the value closest to the first study date among these collected results.
We recorded the history of medication prescriptions, including inhalers, antitussives, and mucolytics. Drug use was defined as continuous drug use for >3 months during the study period. The medication possession ratio (MPR) was defined as the ratio between the duration of medication administration and duration of the follow-up period. The Charlson Comorbidity Index was used to estimate the severity of underlying comorbidities.11 According to the recent GOLD guidelines, patients with COPD were classified into GOLD stages 1–4 (FEV1 ≥ 80% predicted; 50% ≤ FEV1 < 80% predicted; 30% ≤ FEV1 < 50% predicted; and FEV1 < 30% predicted, respectively) on the basis of spirometry stage.12
This study was approved by the Institutional Review Board of Seoul Metropolitan Government–Seoul National University Boramae Medical Center (no: 30–2021-29). The requirement for informed patient consent was waived due to the retrospective nature of the study without participant intervention or interaction, and this study was conducted in accordance with the principles stated in the Declaration of Helsinki.
Outcomes
We evaluated demographic and clinical characteristics of PRISm compared to COPD. The primary outcome was the annual incidence of moderate-to-severe acute exacerbations. An acute exacerbation was defined as acute clinical deterioration of respiratory symptoms, leading to the requirement for additional therapy. We classified the severity of acute exacerbations as moderate (requiring treatment with oral antibiotics and/or oral corticosteroids) or severe (requiring hospitalization or an emergency room visit). Frequent exacerbators were patients with a history of ≥2 moderate-to-severe exacerbations per year. This definition of acute exacerbation was commonly applied to COPD, and the same definition was applied to PRISm. Although there is no specific definition with consensus for acute exacerbation of PRISm, previous study reported that PRISm stage represents an intermediate phase transitioning from COPD GOLD stage 0, which is considered a pre-COPD state, to a definite COPD with an airway-predominant pattern.13 A recent proposal suggested to define COPD through a more expanded concept, taking into account various risk factors and clinical phenotypes of COPD.14 This was the rationale for applying the criteria for acute exacerbations in PRISm in the same way as in COPD.
The secondary outcome was a decline in lung function over time. We investigated the results of lung function tests performed during the study period and evaluated the longitudinal changes in lung function trajectory.
Radiological Findings
Baseline CT scans performed during the study period were analyzed. The chest CT findings were assessed via visual inspection by three readers; two pulmonologists (S.M.Y. and J.K.L.) under the supervision and consensus reading of a chest radiologist (K.N.J.). We evaluated the images for emphysema as a typical finding of COPD, and for findings associated with restrictive spirometry, such as bronchiectasis, TB-destroyed lung, interstitial lung abnormalities (ILA), and interstitial lung disease (ILD). Bronchiectasis was diagnosed on chest CT in accordance with the criteria proposed by McGuinness et al, ie, lack of bronchial tapering, bronchial dilation with internal diameter larger than the diameter of the adjacent pulmonary artery, or visualization of peripheral bronchi within 1 cm of the costal pleural surface or adjacent mediastinal pleural surface.15 TB-destroyed lung refers to the destruction of lung parenchyma (more than one lobe) due to a history of pulmonary TB.16 In accordance with a position paper from the Fleischner Society, ILA was defined as non-dependent abnormalities affecting >5% of any lung zone, including ground glass or reticular abnormalities, non-emphysematous cysts, traction bronchiectasis, honey combing, and architectural distortion.17
Statistical Analysis
Continuous variables are presented as means and standard deviations and categorical variables as numbers and percentages. The χ2 test, Fisher’s exact test, and t-test were used to compare the groups. Subgroup analysis was performed using analysis of variance. Linear and binary logistic regression analyses were performed to estimate the risks of acute and frequent exacerbations, respectively. Multivariable analysis of the risk of acute exacerbations was adjusted for age, sex, smoking intensity, the Charlson Comorbidity Index, FVC, diffusing capacity of the lungs for carbon monoxide (DLCO), serum protein level, ILA, and inhaler MPR. Linear mixed regression models adjusted for age, sex, height, smoking intensity, baseline lung function (FEV1, FVC, or DLCO), and inhaler MPR were constructed to examine the annual rate of decline in lung function. Statistical analyses were conducted using SPSS software (version 26.0; IBM Corp., Armonk, NY, USA).
Results
Baseline Characteristics
Of the 885 patients assessed for eligibility, 623 with chest CT and follow-up pulmonary function tests were included in the study (Figure 1). Of these patients, 40 (6.4%) had PRISm and 583 (93.6%) had COPD. Table 1 presents the baseline demographic and clinical characteristics of the study participants. The mean follow-up duration was 5.3 years. Compared to COPD patients, those with PRISm were significantly younger, and were more likely to be female and have a history of TB. They also had less severe comorbidities. Furthermore, patients with PRISm were significantly less likely to be ever-smokers (65% vs 87.1%) and had a lower smoking intensity (23.8 vs 36.9 pack-years) compared to COPD patients. The mean BMI of the study participants was 22.4 ± 3.4 kg/m2, and BMI was not significantly different between the groups.
 |
Table 1 Baseline Characteristics of the Study Participants |
 |
Figure 1 Flow diagram of the study population. |
PRISm patients had lower FVC and DLCO %predicted, and higher FEV1/FVC ratio and forced expiratory flow between 25% and 75% of vital capacity (FEF25–75%), compared with COPD patients. However, there was no group difference in FEV1. There was a significant difference between the groups in the protein level, but not in the neutrophil-to-lymphocyte ratio or eosinophil count. PRISm patients were significantly less likely to have emphysema than COPD patients (35.0% vs 72.2%; P < 0.001). Although TB-destroyed lung, bronchiectasis, ILA, and ILD were more frequently observed in PRISm compared to COPD patients, the differences were not statistically significant.
All PRISm patients and 92.8% of COPD patients used inhalers including inhaled corticosteroids, long-acting β2-agonists, or long-acting muscarinic antagonists (Table S1). The inhaler MPR was lower in PRISm than COPD patients (0.49 ± 0.36 vs 0.64 ± 0.35; P = 0.017). The proportions of antitussive and mucolytic users were not significantly different between the groups.
A sensitivity analysis focusing on ever-smokers within our study cohort was conducted (Table S2). This result showed that the previously observed significant differences between PRISm and COPD patients in sex proportion, DLCO %predicted, and serum protein level were no longer evident. On the other hand, PRISm patients had a significantly higher proportion of ILD compared to COPD patients.
Incidence of Acute Exacerbations
The annual incidence of moderate-to-severe exacerbations was 0.56 and 0.62 in patients with PRISM and COPD, respectively (Table 2). The annual incidence of moderate, severe, and moderate-to-severe acute exacerbations did not significantly differ between the groups. The proportion of frequent exacerbators was similar between the PRISm and COPD groups (7.5% vs 8.7%; P = 0.786). When analyzed according to spirometric stage, the annual rate of acute exacerbations and proportion of frequent exacerbators were significantly different between the groups. The annual rate of exacerbations and proportion of frequent exacerbators gradually increased with increasing GOLD spirometric stage and was significantly different between GOLD stages 2 and 3. The average FEV1 of PRISm patients was 66%, which corresponded to GOLD stage 2. Furthermore, the annual rate of exacerbations and proportion of frequent exacerbators in PRISm patients were similar to those of GOLD stage 2 patients.
 |
Table 2 Annual Incidence Rates of Acute Exacerbations and Proportions of Frequent Exacerbators |
Risk of Acute Exacerbations
Multivariable analysis showed that FVC, DLCO, and the serum protein level were positively associated, whereas smoking intensity, ILA, and inhaler MPR were negatively associated, with the risk of moderate-to-severe acute exacerbations (Table 3). After adjusting for the aforementioned factors, there was no significant difference in the risk of moderate-to-severe acute exacerbations between patients with PRISm and COPD. Similar results were obtained when acute exacerbations were classified as moderate or severe. Comparison of the PRISm group with the spirometric stages of COPD showed that PRISm was associated with a significantly lower risk of severe acute exacerbations compared to GOLD stage 4 (Table S3).
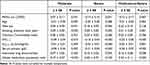 |
Table 3 Risk Factors for Acute Exacerbations in PRISm and COPD Patients |
The proportion of frequent exacerbators increased in the GOLD spirometric stage in COPD patients. The PRISm group had a lower proportion of frequent exacerbators compared to the GOLD stage 3 and 4 subgroups, although the differences were not statistically significant (Table 4). In the univariable analysis, the proportion of frequent exacerbators was 5.4−fold higher in COPD GOLD stage 4 patients than PRISm patients; however, this relationship was not observed in the multivariable analysis.
 |
Table 4 Risk of Frequent Exacerbation in PRISm Patients and GOLD Spirometric Stage Subgroups |
Lung Function Changes
Patients with PRISm had a significantly slower decline of FEV1 (−2.80 ± 2.83 vs −27.6 ± 2.48 mL; P < 0.001), FVC (−10.5 ± 4.03 vs −33.0 ± 3.87 mL; P < 0.001), and DLCO (−0.01 ± 0.04 vs −0.25 ± 0.03 mL/mmHg/min; P < 0.001) compared to patients with COPD (Table 5). Patients with COPD, but not those with PRISm, exhibited progression toward obstructive ventilatory disorders, as evaluated by the FEV1/FVC ratio.
 |
Table 5 Annual Change Rates of Lung Function in PRISm and COPD Patients |
Subgroup analysis according to spirometric stage showed that the annual decline of FEV1, FVC, the FEV1/FVC ratio, and DLCO in COPD patients was slower at higher spirometric stages (Table S4). The aforementioned lung parameters were significantly different between PRISm and COPD patients according to the spirometric stage. The annual changes of FEV1 and FVC in PRISm patients were compatible with those between the GOLD stage 3 and 4 subgroups. PRISm patients had smaller changes in the FEV1/FVC ratio and DLCO than any COPD subgroup.
Longitudinal Changes of Lung Function Trajectory
Figure 2 presents the longitudinal changes of lung function trajectory (ie, difference between the initial and final pulmonary function tests) during an average follow-up period of 5.3 years. PRISm was maintained in 40% of cases, converted to COPD in 32.5%, and converted to normal in the remaining 27.5%. COPD was maintained in 91.8% of patients, converted to PRISm in 4.5%, and converted to normal in 3.8%.
 |
Figure 2 Longitudinal changes of lung function trajectories. |
PRISm patients were classified into subgroups according to longitudinal changes: “persistent PRISm”, “PRISm to normal”, and “incident COPD”. The persistent PRISm group significantly had a higher proportion of ever-smokers and higher smoking intensity, and lower FEV1 and FVC (Table S5). Although not statistically significant, the persistent PRISm group exhibited a higher prevalence of radiological findings (TB-destroyed lung, bronchiectasis, and ILA) that could potentially induce restrictive ventilatory disorder. On the other hand, the incident COPD group, while not statistically significant, had a higher proportion of physician-diagnosed asthma, lower FEF25–75%, and a higher blood eosinophil count. The persistent PRISm group tended to show a higher incidence of moderate-to-severe exacerbations and a higher proportion of frequent exacerbators compared to other subgroups (Table S6). In the analysis of longitudinal change of lung function, the persistent PRISm group showed a significantly faster decline in FEV1, an even more rapid decline in FVC, and faster decline in DLCO compared to other subgroups (Table S7). On the other hand, the incident COPD group exhibited a slight decrease in both FEV1 and FVC, but with a slightly faster decline in FEV1 compared to FVC, indicating a significantly more pronounced progression of an obstructive ventilatory disorder.
Discussion
In this study, patients with PRISm were significantly younger and more likely to be female and have a history of TB, compared to COPD patients; they also had a lower smoking intensity, less severe comorbidities, and lower FVC and DLCO. The radiological findings were analyzed to investigate why PRISm patients had lower FVC and DLCO despite a similar FEV1 to COPD patients. COPD patients were more likely to have emphysema and small airway dysfunction, as suggested by a relatively low FEF25–75% (a feature consistent with progression of smoking-related disease), compared to PRISm patients. In contrast, PRISm patients were more likely to have a TB-destroyed lung, bronchiectasis (which may be due to the history of TB documented in more than half of the patients), ILA, and ILD compared to COPD patients, although the differences were not statistically significant due to the small number of PRISm patients. The comorbid respiratory conditions observed in patients with PRISm may lead to a restrictive ventilatory disorder, because TB-destroyed lung and bronchiectasis are associated with persistent destructive lesions of the airways and lung parenchyma (which are commonly associated with past infection). Furthermore, ILA and ILD may progress to parenchymal fibrosis with disease progression.
A study using the COPDGene cohort, a major cohort study of smokers, classified PRISm into restrictive, COPD, and metabolic subtypes using clustering analysis. According to that classification system, the PRISm patients in our study were most compatible with the restrictive subtype.3 Although metabolic diseases and obesity are risk factors for PRISm,1 this was not verified in our study. In a recent study of an East Asian population, BMI was higher in PRISm than COPD patients; however, the average BMI of PRISm patients was normal (24.1 kg/m2).9 In contrast, in a UK cohort study, the average BMI of PRISm patients was 29.1, ie, the patients were overweight.4 In addition, in our study, PRISm patients were more likely to have a TB history than COPD patients, possibly because the study was conducted in an intermediate-burden country for active TB (ie, South Korea). Our results suggest that the characteristics of PRISm patients may vary depending on demographic and clinical characteristics of PRISm subgroup.
Our major findings indicated that PRISm and COPD patients had a similar risk of moderate-to-severe acute exacerbations and frequent exacerbations, regardless of lung function. In COPD patients, acute exacerbation is the most important risk factor for future exacerbations, and is also associated with lung function decline, hospitalization, and mortality.18–20 Patients with PRISm experience frequent respiratory exacerbations, similar to COPD patients,8 which may lead to increased all-cause mortality compared to individuals with normal spirometry.5 Therefore, PRISm patients have a risk of acute exacerbations commensurate with their level of lung function.10
There have been various clinical trials on the optimal treatment of COPD. However, because PRISm does not fulfil the conventional spirometric criteria of COPD, it was often overlooked or excluded from previous studies. As a result, there is no direct evidence regarding the optimal treatment of PRISm. In our study, PRISm patients did not differ significantly from COPD patients in terms of the use of inhalers, antitussives, or mucolytics. In particular, all PRISm patients used inhalers suggesting that, similar to COPD patients, they have a considerable burden of respiratory symptoms requiring treatment. Previous studies have confirmed that PRISm patients have significant symptoms and functional limitations along with various underlying etiologies.2 Although this study is limited to confirm the efficacy of treatment in PRISm patients, it highlights the need for further research to determine whether drugs can improve the outcomes of PRISm patients, and which drugs are most useful for specific subgroups of patients.
PRISm patients had a significantly slower annual decline of FEV1, FVC, and DLCO compared to COPD patients. In a previous long-term study of the lung function of COPD patients, the annual decline thereof was slower in patients with poor lung function.21 Considering that the mean FEV1 of PRISm patients was within the range for GOLD stage 2, the rate of change of lung function may be slower in PRISm than GOLD stage 1 and 2 patients, consistent with the results of previous studies.1,10 However, in the PRISm patients in our study, the annual rate of decline of lung function was similar between GOLD stage 3 and 4 patients, and was slower than the rate expected according to the level of lung function. These findings may be explained by the increased prevalence of comorbid respiratory conditions that can induce restrictive spirometry in PRISm patients. Common lung diseases in PRISm patients include TB-destroyed lung, bronchiectasis, ILA, and ILD. Longitudinal changes of these diseases are relatively indolent and less variable; the lung function of PRISm patients with comorbid lung diseases may be already low due to preceding parenchymal loss, but its subsequent changes may be relatively small compared to the actual lung function.
The longitudinal changes of lung function trajectory showed that approximately one-third of PRISm patients remained as PRISm, while one-third converted to normal and another third to COPD. However, most COPD patients remained as COPD, whereas a small proportion changed to PRISm or normal spirometry. Our study found that COPD patients had significantly more annual decline in both FEV1 and FEV1/FVC ratio compared to PRISm patients. A recent study in a smoker cohort demonstrated that changes of both FEV1 and FEV1/FVC ratio were significant predictors of COPD progression.22 This indicates that the progression to obstructive ventilatory disorder is more pronounced in COPD, compared to PRISm. In the general population, PRISm with normal lung function and persistent PRISm are risk factors for cardiovascular disease and death.23 In a previous longitudinal follow-up study, PRISm patients had a higher risk of incident airflow limitation compared to individuals with normal spirometry.9 This suggests that the fixed cut-off value to define COPD is insufficient to reflect the diverse clinical course of patients. Additionally, even if the initial lung function test exhibits spirometry parameters compatible with PRISm, patients with risk factors for COPD or comorbid conditions that may accompany a restrictive ventilatory disorder should undergo careful follow-up.
Subgroup analysis according to the longitudinal change of PRISm patients, the persistent PRISm group exhibited a significantly faster decline in FEV1 and DLCO, along with a more rapid decline in FVC compared to FEV1. This may be associated with the higher prevalence of respiratory diseases such as TB-destroyed lung, bronchiectasis, and ILA observed in this group. On the other hand, the group transitioning from PRISm to COPD had more asthma, elevated blood eosinophil count, and lower FEF25-75%, suggesting that asthma and the accompanying eosinophilic inflammation and small airway disease may influence the progression to COPD. These results indicate that comorbid respiratory diseases in PRISm patients are important factors in the assessment of the current disease state and the prediction of future prognosis.
This study had several limitations. First, it used a single-center, observational, retrospective design that provided moderate-level evidence. Second, the results of this study are limited in generalizability as it focused on a single racial group (Asian) and targeted patients receiving follow-up observations and treatment at a tertiary referral hospital (because PRISm is a heterogenous disease entity that may have different characteristics depending on the study population). As mentioned earlier, South Korea is an intermediate-burden country for active TB, which should be taken into account when interpreting the results related to TB history. Third, the small number of PRISm patients reduced the statistical power of our results. In particular, we identified that PRISm patients have a variety of comorbid respiratory diseases, each with its unique characteristics and prognosis. However, due to the small number of study subjects, it was limited to comprehensively evaluate these heterogenous conditions. Fourth, in assessing the clinical course of PRISm, we applied the criteria for acute exacerbations in the same way as in COPD. There is currently no expert consensus on the criteria for acute exacerbations in PRISm, and these criteria may change as the characteristics of PRISm are more clarified through further research.
In conclusion, PRISm patients had no significant difference in the risk of moderate-to-severe acute exacerbations or frequent exacerbations, but a significantly lower annual decline of lung function during follow-up, compared with COPD patients. PRISm and COPD may have an indistinguishable long-term clinical course. It is important to recognize that PRISm patients, like COPD patients, have significant symptom complaints and unmet needs for treatment. Therefore, we should not exclude PRISm patients simply because they do not meet the criteria for COPD. Instead, we should maintain ongoing interest in the course of the disease and the potential for treatment in PRISm patients. Further studies are required to identify the most appropriate evaluation and treatment strategies for these patients.
Abbreviations
BMI, body mass index; COPD, chronic obstructive pulmonary disease; CT, computed tomography; DLCO, diffusing capacity of the lungs for carbon monoxide; FEF25–75%, forced expiratory flow between 25% and 75% of vital capacity; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; GOLD, Global Initiative for Obstructive Diseases; ILA, interstitial lung abnormality; ILD, interstitial lung disease; MPR, medication possession ratio; PRISm, preserved ratio impaired spirometry; TB, tuberculosis.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article and its Supplementary Information.
Ethics Approval and Consent to Participate
This study was approved by the Institutional Review Board of Seoul Metropolitan Government–Seoul National University Boramae Medical Center (no: 30-2021-29). The requirement for informed consent from study participants was waived by the institutional review board, and this decision was based on the following reasons: 1) This study was conducted retrospectively, involving no intervention or interaction with study participants, and relied solely on existing medical records. It did not compromise the safety, welfare, and rights of the participants. 2) This study focused on the past data, it was impractical to obtain consent from all participants. 3) There was no apparent reason to anticipate refusal of consent from participants, and even if consent were waived, the study posed minimal risk to the participants. The conduct of this study and the confidentiality of patient data were maintained in accordance with the Declaration of Helsinki. The result of this study has not been published elsewhere in whole or in part and is not under consideration by another journal. The interim findings of this study were presented orally at the KATRD International Conference 2021 on November 11, 2021.
Author Contributions
All authors had access to the data, had a role in writing this manuscript, including critical review of the manuscript, and made significant contributions to this work. All authors agreed on the journal submission choice, have agreed on all revisions, gave final approval for the version to be published, and agreed to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no potential conflicts of interest in this work.
References
1. Wan ES, Fortis S, Regan EA, et al. Longitudinal phenotypes and mortality in preserved ratio impaired spirometry in the copdgene study. Am J Respir Crit Care Med. 2018;198:1397–1405. doi:10.1164/rccm.201804-0663OC
2. Wan ES, Hokanson JE, Murphy JR, et al. Clinical and radiographic predictors of GOLD–unclassified smokers in the COPDGene study. Am J Respir Crit Care Med. 2011;184(1):57–63. doi:10.1164/rccm.201101-0021OC
3. Wan ES, Castaldi PJ, Cho MH, et al. Epidemiology, genetics, and subtyping of preserved ratio impaired spirometry (PRISm) in COPDGene. Respir Res. 2014;15:89. doi:10.1186/s12931-014-0089-y
4. Higbee DH, Granell R, Davey Smith G, Dodd JW. Prevalence, risk factors, and clinical implications of preserved ratio impaired spirometry: a UK Biobank cohort analysis. Lancet Respir Med. 2022;10:149–157. doi:10.1016/S2213-2600(21)00369-6
5. Wijnant SRA, De Roos E, Kavousi M, et al. Trajectory and mortality of preserved ratio impaired spirometry: the Rotterdam study. Eur Respir J. 2020;2020:55.
6. Sood A, Petersen H, Qualls C, et al. Spirometric variability in smokers: transitions in COPD diagnosis in a five-year longitudinal study. Respir Res. 2016;17:147. doi:10.1186/s12931-016-0468-7
7. Jankowich M, Elston B, Liu Q, et al. Restrictive spirometry pattern, cardiac structure and function, and incident heart failure in African Americans. The Jackson heart study. Ann Am Thorac Soc. 2018;15:1186–1196. doi:10.1513/AnnalsATS.201803-184OC
8. Woodruff PG, Barr RG, Bleecker E, et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N Engl J Med. 2016;374:1811–1821. doi:10.1056/NEJMoa1505971
9. Washio Y, Sakata S, Fukuyama S, et al. Risks of mortality and airflow limitation in Japanese with preserved ratio impaired spirometry. Am J Respir Crit Care Med. 2022. doi:10.1164/rccm.202110-2302OC
10. Dransfield MT, Kunisaki KM, Strand MJ, et al. Acute exacerbations and lung function loss in smokers with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;195:324–330. doi:10.1164/rccm.201605-1014OC
11. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi:10.1016/0021-9681(87)90171-8
12. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease; 2023.
13. Young KA, Strand M, Ragland MF, et al. Pulmonary subtypes exhibit differential global initiative for chronic obstructive lung disease spirometry stage progression: the COPDGene(R) study. Chronic Obstr Pulm Dis. 2019;6:414–429. doi:10.15326/jcopdf.6.5.2019.0155
14. Stolz D, Mkorombindo T, Schumann DM, et al. Towards the elimination of chronic obstructive pulmonary disease: a lancet commission. Lancet. 2022;400:921–972. doi:10.1016/S0140-6736(22)01273-9
15. McGuinness G, Naidich DP, Leitman BS, McCauley DI. Bronchiectasis: CT evaluation. AJR Am J Roentgenol. 1993;160:253–259. doi:10.2214/ajr.160.2.8424327
16. Rhee CK, Yoo KH, Lee JH, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis. 2013;17:67–75. doi:10.5588/ijtld.12.0351
17. Hatabu H, Hunninghake GM, Richeldi L, et al. Interstitial lung abnormalities detected incidentally on CT: a position paper from the Fleischner Society. Lancet Respir Med. 2020;8:726–737. doi:10.1016/S2213-2600(20)30168-5
18. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57:847–852. doi:10.1136/thorax.57.10.847
19. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391:1076–1084. doi:10.1016/S0140-6736(18)30206-X
20. Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003;124:459–467. doi:10.1378/chest.124.2.459
21. Kim J, Yoon HI, Oh YM, et al. Lung function decline rates according to GOLD group in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1819–1827. doi:10.2147/COPD.S87766
22. Strand M, Khatiwada A, Baraghoshi D, et al. Predicting COPD progression in current and former smokers using a joint model for forced expiratory volume in 1 second and forced expiratory volume in 1 second to forced vital capacity ratio. Chronic Obstr Pulm Dis. 2022;9:439–453. doi:10.15326/jcopdf.2022.0281
23. Marott JL, Ingebrigtsen TS, Colak Y, Vestbo J, Lange P. Trajectory of preserved ratio impaired spirometry: natural history and long-term prognosis. Am J Respir Crit Care Med. 2021;204:910–920. doi:10.1164/rccm.202102-0517OC
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
