Back to Journals » Clinical Epidemiology » Volume 15
Absence of Coronary Artery Disease is a Strong Negative Predictor of Major Adverse Cardiovascular Events in Patients with Chronic Kidney Disease
Authors Tonnesen PT, Olesen KKW , Thrane PG , Gyldenkerne C , Peters CD , Buus NH , Maeng M
Received 4 August 2023
Accepted for publication 31 October 2023
Published 29 November 2023 Volume 2023:15 Pages 1109—1121
DOI https://doi.org/10.2147/CLEP.S433983
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Pernille Tilma Tonnesen,1 Kevin Kris Warnakula Olesen,1 Pernille Gro Thrane,1 Christine Gyldenkerne,1 Christian Daugaard Peters,2,3 Niels Henrik Buus,2,3 Michael Maeng1,3
1Department of Cardiology, Aarhus University Hospital, Aarhus, Denmark; 2Department of Renal Medicine, Aarhus University Hospital, Aarhus, Denmark; 3Department of Clinical Medicine, Aarhus University Hospital, Aarhus, Denmark
Correspondence: Michael Maeng, Department of Cardiology, Aarhus University Hospital, Palle Juul-Jensens Boulevard 99, Aarhus, 8200, Denmark, Tel +45 26703237, Email [email protected]
Purpose: To investigate the interplay between chronic kidney disease (CKD) and coronary artery disease (CAD) on the incidence of cardiovascular events in patients with suspected chronic coronary syndrome (CCS).
Patients and Methods: Patients with suspected CCS who underwent first-time coronary angiography in Western Denmark between 2003 and 2016 were included in this cohort study. Moreover, an age- and sex-matched general population cohort was established. Patients were stratified according to estimated glomerular filtration rate (eGFR). Presence of CAD was defined as ≥ 1 obstructive stenosis or non-obstructive diffuse disease. Major adverse cardiovascular events (MACE) were defined as a composite of myocardial infarction, ischemic stroke, and cardiac death.
Results: A total of 42,611 patients were included with a median follow-up of 7.3 years. Patients without and with CAD had MACE rates per 100 person-years that were 0.52 and 1.67 for eGFR ≥ 90 mL/min/1.73 m2, 0.68 and 2.09 for eGFR 60– 89 mL/min/1.73 m2, 1.27 and 3.85 for eGFR 30– 59 mL/min/1.73 m2, and 2.27 and 6.92 for eGFR < 30 mL/min/1.73 m2. Comparing to eGFR ≥ 90 mL/min/1.73 m2, the adjusted incidence rate ratios for MACE were 1.29 (1.10– 1.51) for eGFR 60– 89 mL/min/1.73 m2, 1.86 (1.49– 2.33) for eGFR 30– 59 mL/min/1.73 m2, and 3.57 (1.92– 6.67) for eGFR < 30 mL/min/1.73 m2 in patients without CAD, and 1.11 (1.03– 1.20), 1.71 (1.55– 1.90), and 2.46 (1.96– 3.09) in patients with CAD. The inverse relationship between kidney function and risk of MACE was confirmed when comparing patients with and without CAD to matched individuals in the general population.
Conclusion: Absence of CAD is a strong negative predictor of major adverse cardiovascular events in patients with CKD.
Keywords: coronary artery disease, coronary angiography, kidney function, renal insufficiency, chronic kidney disease, chronic coronary syndrome
Introduction
Chronic kidney disease (CKD) is highly prevalent worldwide, it affects 8–16% of the population,1 and CKD is the third fastest growing cause of death globally.2 In high-income countries, CKD is mainly caused by diabetes or hypertension,3 which also represent central risk factors for development of cardiovascular diseases, both individually and synergistically.4,5
Cardiovascular disease and CKD frequently coexist in patients.1 Consequently, the current European Society of Cardiology (ESC) guidelines for chronic coronary syndrome (CCS) recommend that patients with CKD are treated to target values for cardiovascular risk factors such as hyperlipidemia, hypertension, and hyperglycemia.6 Moreover, CKD has previously been established as an important predictor of clinical cardiovascular outcomes, although data are sparse in patients with CCS.7,8 However, strong associations between impaired kidney function and long-term cardiovascular outcomes (risk of death, heart failure and myocardial infarction (MI)) in patients with CCS were recently reported in a Swedish cohort.9
We have previously shown that the absence of CAD eliminates the excess MI risk in patients with diabetes,10–13 reduces the excess risk of stroke and limb amputations in patients with diabetes,14,15 and reduces the risk of stroke in patients with atrial fibrillation.16 In the current study we aimed to investigate if CAD is also a strong negative predictor across different stages of CKD. To answer this question, we used a cohort of CCS patients undergoing coronary angiography (CAG) in Western Denmark and a matched general population comparison cohort.
Methods
Data Collection
Patients were identified from the Western Denmark Heart Registry (WDHR), where patient and procedure data from all cardiac procedures in Western Denmark are prospectively recorded, including CAGs since 1999.17 The WDHR was linked with other registries using the unique, individual Civil Person Register number, assigned to all Danish citizens, and recorded in the Danish Civil Registration System.18 This system allows us to collect long-term follow-up on patients by providing information on emigration and vital status.18
Several registries were used in this study; the Danish National Patient Registry (DNPR),19 the Danish National Prescription Registry,20 and the Danish Register of Causes of Death.21 The DNPR collects primary and secondary discharge diagnoses after patient admissions. These diagnoses are registered in accordance with the International Classification of Diseases, 10th revision.
Patient Selection
We identified all patients undergoing CAG in Western Denmark from January 1, 2003 – December 31, 2016 (Figure 1). Patients below 18 years were excluded. Patients with CAG performed due to acute coronary syndromes or other indications than stable angina pectoris were excluded. We excluded all patients with missing CAD status and estimated glomerular filtration rate (eGFR) data and follow-up <30 days. Patients undergoing dialysis were excluded. Thereby, patients undergoing CAG due to suspicion of CCS were included and stratified on presence of CAD and kidney function.
Exposure
Kidney function was assessed by eGFR, which was estimated according to the most recent plasma creatinine measured before CAG. eGFR was calculated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation and adjusted to body surface area (BSA) as calculated by the Du Bois formula.22 The CKD-EPI equation is validated in a US population.23 Kidney function was classified in CKD stages based on eGFR: eGFR ≥90 mL/min/1.73 m2 as normal or high function; 60–89 mL/min/1.73 m2 as mildly decreased; 30–59 mL/min/1.73 m2 as moderately decreased; and <30 mL/min/1.73 m2 as severely decreased/kidney failure.24
CAD status was evaluated by CAG and recorded in the WDHR. CAD was defined as ≥1 coronary vessel(s) with obstructive stenosis (≥50% lumen narrowing and/or a fractional flow reserve ≤0.80, the latter officially included in the definition in 2014) or diffuse non-significant vessel disease.
Baseline Characteristics
Information on age and sex were collected from the Civil Registration System. The WDHR and the DNPR were used to obtain patient data and information on comorbidities. Diabetes was defined as (1) being in dietary treatment, insulin treatment with or without oral glucose lowering treatment, or oral glucose lowering treatment according to the WDHR, (2) a diabetes diagnosis registered in the DNPR before CAG or within 30 days after CAG, (3) redemption of diabetes medication (being either insulin or non-insulin glucose lowering treatment) within 6 months before CAG to 30 days after as recorded in the Danish National Prescription Registry. Hypertension was defined as a combination of treatment for hypertension in the WDHR and a previous hypertension diagnosis registered in the DNPR. Heart failure with reduced ejection fraction (HFrEF) was characterized as an ejection fraction ≤40% registered in the WDHR or a diagnosis of heart failure in the DNPR, before CAG or within 30 days after CAG. Prescription records on medications (within 6 months before CAG until 30 days after CAG) were obtained from the Danish National Prescription Registry. Charlson Comorbidity Index (CCI) was modified to exclude moderate-to-severe kidney disease.25
Outcomes
Major adverse cardiac events (MACE) were defined as a composite of MI, ischemic stroke, and cardiac death. Data on MI and ischemic stroke were obtained by the primary and secondary discharge diagnoses from hospital admissions in the DNPR (Supplementary Table 1). Information on cardiac death is registered in the Danish Register of Causes of Death. All-cause mortality was determined from the Danish Civil Registration System. Follow-up and registration of events were initiated 30 days after CAG to avoid double recording of procedure-related events.
Statistical Analyses
Follow-up began 30 days after the CAG procedure and end of follow-up was defined as outcome, death, emigration, maximum 10-year follow-up, or at the date of last available data (December 31, 2018). Event rates were estimated per 100 person-years at risk. Information on smoking status was missing in 4% of patients and BMI in 0.1% of patients. These missing data were handled by imputation of 5 datasets using chained equations.26 A modified Poisson regression with a robust variance-covariance estimator was used to compute unadjusted and adjusted incidence rate ratio (IRR), with the eGFR ≥90 mL/min/1.73 m2 stratum as reference.27 Analyses of event rates and IRRs were repeated for patients stratified by CAD status at CAG. IRR was adjusted to potential confounders based on clinical assessment. For MI, IRR were adjusted for age category (<65 years, 65–74 years, and ≥75 years), sex, BMI category (<18.5 kg/m², 18.5–24 kg/m², 25–29 kg/m², and ≥30 kg/m²) (imputed), active smoking (imputed), hypertension, peripheral artery disease (PAD), previous ischemic stroke, diabetes, CAD severity, antiplatelet treatment (aspirin and adenosine-diphosphate receptor inhibitors), oral anticoagulant treatment (vitamin K-antagonists and direct oral anticoagulants), and statin treatment. For the ischemic stroke and MACE outcomes, data were additionally adjusted for HFrEF and atrial fibrillation. For all-cause mortality, data were adjusted for age category (18–64 years, 65–74 years, and ≥75 years), sex, BMI category (<18.5 kg/m², 18.5–24 kg/m², 25–29 kg/m², and ≥30 kg/m²) (imputed), active smoking (imputed), hypertension, CAD severity, modified CCI group, oral anticoagulant treatment, antiplatelet treatment, and statin treatment. We performed Log rank tests for trend to examine the trend between eGFR and any outcome, both with and without stratification for CAD. CAG patients were compared to an age- and sex-matched background population with respect to 10-years MACE using conditional, fixed-effect Poisson regression. Stratified analyses were performed for CAD and eGFR. Stata software, version 16.0 (StataCorp LLC, Texas, USA), was used for statistical analyses.
Ethical Considerations
The study was registered with the Danish Data Protection Agency (record no. 1-16-02-193-18). According to Danish regulation, observational, noninterventional registry-based studies require neither approval from ethics committees nor informed consent from patients.
Results
A total of 42,611 patients were included in the analyses. At the time of CAG, 16,084 (37.7%) had no CAD, while 26,527 (62.3%) patients had obstructive CAD or diffuse non-obstructive vessel disease. Median eGFR was 88 mL/min/1.73 m2 (Q1-Q3: 72–104 mL/min/1.73 m2) and 5014 patients (11.5%) had an eGFR <60 mL/min/1.73 m2. Median follow-up was 7.3 years (Q1-Q3: 4.4–10.0 years) and within this period 4266 MACE were observed.
Baseline Characteristics
Baseline characteristics are presented in Table 1. Overall, declining kidney function was associated with higher prevalence of important risk factors. For example, patients in the lowest eGFR strata <30 mL/min/1.73 m2 were older and had a higher prevalence of previous ischemic stroke, atrial fibrillation, PAD, hypertension, HFrEF, previous MI, microvascular diseases, and diabetes. Additionally, presence and extent of CAD was inversely associated with kidney function. Supplementary Tables 2 and 3 provide baseline characteristics of patients with and without CAD, respectively.
 |
Table 1 Baseline Characteristics of Chronic Coronary Syndrome Patients Undergoing Coronary Angiography in Western Denmark |
Clinical Outcomes
MACE rates are presented in Table 2, further stratification for absence versus presence of CAD is shown in Table 3, and the results are illustrated in Figure 2. The rate of MACE was inversely related to kidney function. When comparing the eGFR <30 mL/min/1.73 m2 stratum (5.73 events per 100 person-years [95% CI, 4.60–7.14]) to the eGFR ≥90 mL/min/1.73 m2 stratum (1.16 events per 100 person-years [95% CI, 1.11–1.22]), the 10-year risk increased with a factor 4.92 [95% CI, (3.92–6.18)] for the overall cohort. Accordingly, Figure 3 displays an increased cumulative incidence proportion of MACE with decreasing eGFR stratum. When stratifying for CAD status, only the eGFR <30 mL/min/1.73 m2 stratum among patients without CAD resulted in an event rate (2.27 [95% CI, 1.13–4.53]) exceeding that of the eGFR ≥90 mL/min/1.73 m2 stratum in patients with CAD (1.67 [95% CI, 1.58–1.76]). After adjustment for potential confounders, the risk of MACE remained incrementally associated with reduced kidney function regardless of CAD status.
 |
Table 2 Incidence Rate Ratios of Major Adverse Cardiovascular Events |
 |
Table 3 Major Adverse Cardiovascular Events Stratified by Coronary Artery Disease |
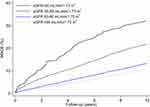 |
Figure 3 Cumulative incidence proportions. Abbreviation: MACE, major adverse cardiovascular events. |
After stratification for kidney function according to eGFR categories G1-G5, the resulting risk of MACE overall supported our previously reported results for patients with and without CAD (Supplementary Table 4). We additionally found a significantly increased risk of MACE for patients with CAD and eGFR 30–44 mL/min/1.73 m2 (1.93 [95% CI, 1.65–2.27]) compared to the eGFR 45–59 mL/min/1.73 m2 stratum (1.42 [95% CI, 1.25–1.60]). However, our data set contains few patients without CAD and eGFR <45 mL/min/1.73 m2 (n=338) as well as patients with CAD and eGFR <30 mL/min/1.73 m2 (n=235), making further interpretation of the sub-analysis challenging. Categorizing patients according to CAD status as diffuse, non-significant CAD, obstructive single-vessel CAD, and obstructive multivessel CAD, we confirmed the inverse relationship between kidney function and risk of MACE for each eGFR stratum (Supplementary Table 5). Additionally, we found that with increased extent of CAD, the rate of MACE overall worsened within equal eGFR strata. Likewise, we confirmed the inverse relationship when stratifying for LVEF>40% or LVEF≤40% within patients with CAD (Supplementary Table 6). Further, we found that patients with CAD, LVEF≤40%, and eGFR <30 mL/min/1.73 m2 had the highest risk of MACE.
Table 4 shows the comparison between patients and their age- and sex-matched individuals from the general population. For patients without CAD and eGFR ≥60 mL/min/1.73 m2, the risk of MACE was comparable to that of the general population, whereas eGFR in the 30–59 mL/min/1.73 m2 range was associated with a 31% (IRR 1.31 (1.04–1.66)) increased relative risk, and eGFR <30 mL/min/1.73 m2 with a >3-fold (IRR 3.11 (0.96–10.05)) increased relative risk when compared with the age- and sex-matched background population. This becomes visible in Figure 4 depicting the cumulative incidence proportions of MACE, which is similar to that of the matched background populations for patients without CAD and eGFR ≥30 mL/min/1.73 m2. Concerning patients with CAD, the cumulative incidence proportions of MACE were increased when comparing to the general population across all eGFR strata (Figure 4). Correspondingly, patients with CAD all had an increased risk of MACE being 2-3-fold higher for eGFR >90 mL/min/1.73 m2, 60–89 mL/min/1.73 m2, and 30–59 mL/min/1.73 m2 than observed in the general population, while a substantial 7.42-fold (IRR 7.42 (4.67–11.81)) increased risk of MACE was observed for patients with eGFR <30 mL/min/1.73 m2 (Table 4). Patients with eGFR <30 mL/min/1.73 m2 had an increased incidence of MACE compared to the respective matched background population regardless of CAD status.
 |
Table 4 Risk of Major Adverse Cardiovascular Events for Patients Compared to a Matched General Population |
For all other clinical outcomes assessed in the current study (including MI, ischemic stroke and all-cause mortality), we found the same trend towards increased incidence across decreasing eGFR strata (p<0.001) (Supplementary Table 7, Supplementary Figures 1 and 2). This was also the case after stratification for presence of CAD (Supplementary Table 8). Supplementary Table 9 displays that risk of MACE was similar irrespectively of using BSA or non-BSA adjusted eGFR. Finally, Supplementary Table 10 shows the risk of MACE without correction for BMI, which was comparable to the results adjusted for BMI.
Discussion
In the current study, we found that the absence of CAD is also a strong negative predictor of MACE in patients with CKD. Even though we observed a similar relative inverse relationship between CKD and risk of MACE in patients with and without CAD, the absence of CAD was associated with a substantially lower absolute risk of events when comparing equal eGFR strata. Moreover, the relationship between CKD and MACE in patients without CAD became more complex when we additionally compared these patients with an age- and sex-matched general population. In the latter comparison, our results revealed no or only a negligible excess risk of MACE for patients without evident CAD and eGFR ≥30 mL/min/1.73 m2 when compared to their matched general population individuals, whilst patients with severely reduced kidney function (eGFR <30 mL/min/1.73 m2) were at increased risk of MACE irrespectively of CAD status. Thus, the absence of CAD is a strong negative predictor of major adverse cardiovascular events in patients with CKD, while severely reduced kidney function is a strong positive predictor irrespectively of CAD status. Contrarily, among patients with either diffuse, single-vessel or multi-vessel CAD, we confirmed the reported inverse relationship between CKD and risk of MACE regardless of extent of CAD and presence or absence of HFrEF.
Our finding is concordant with our previous publications regarding MI in patients with diabetes,10–13 stroke and limb amputations in patients with diabetes,14,15 and stroke in patients with atrial fibrillation.16 There is a paucity of studies examining the association between the presence of CAD, kidney function, and cardiovascular risk. A Swedish cohort study has previously investigated the significance of CAD and CKD in patients with stable CAD and found a similar reverse association between kidney function and risk of MI or all-cause mortality.9 In both the Swedish cohort and the Western Danish patients, the absence of CAD was a strong negative predictor of cardiovascular outcomes when comparing patients within the same kidney function group. Moreover, both studies show an inverse relationship between CKD stage and MACE in patients without CAD. However, this inverse relationship was less evident when we compared CCS patients with age- and sex-matched general population individuals where only those with severe CKD (eGFR <30 mL/min/1.73 m2) had a clinically relevant increased risk of MACE.
In patients with suspected CCS, we found that decreased kidney function was associated with increased presence of HFrEF and extent of CAD at baseline. This is in accordance with previous studies describing the cardio-renal syndrome, constituting a pathophysiologic disorder of the heart and kidneys, where chronic dysfunction in one organ may induce acute or chronic dysfunction in the other.28 Smoking, diabetes, hypertension, dyslipidemia, and obesity are shared risk factors by CAD and CKD.29 Decreased eGFR has also previously been associated with the severity of CAD independently of traditional risk factors for CAD.30 Major non-traditional risk factors include proteinuria, vascular calcification, neurohormonal dysregulation, impaired endothelium-dependent vasodilation, low-grade chronic inflammation, anemia, volume overload, and disturbances in the calcium-phosphate metabolism. The accumulated effect of these factors is often described as early or accelerated vascular aging, and affects most patients progressing to end-stage renal disease.31 The extensive comorbidities of patients with reduced eGFR are also recognized in the high risk of major adverse cardiovascular events found in this study.
CKD causes increased coronary artery calcification even in patients without common cardiovascular risk factors such as dyslipidemia and hypertension, thereby generating reduced coronary flow reserve and increased cardiovascular events.31 Coronary flow reserve is a marker of the coronary microvascular function and has been found significantly lower in patients with CKD compared to patients with eGFR >60 mL/min/1.73 m2 in a cohort of patients without known CAD.32 Therefore, CKD-associated coronary microvascular dysfunction is suggested as a possible explanation for the increased risk of cardiovascular events in patients without evident CAD,31,32 which may explain why patients with eGFR <30 mL/min/1.73 m2 were at the highest risk of MACE irrespectively of CAD status in our dataset.
At baseline, the prevalence of hypertension differed from 62% in the eGFR ≥90 mL/min/1.73 m2 stratum to 89% in the eGFR <30 mL/min/1.73 m2 stratum. Accordingly, patients with eGFR <30 mL/min/1.73 m2 tended to be more likely to receive antihypertensive treatment. Diabetes was also more common in patients with eGFR <30 mL/min/1.73 m2, confirming the known association between CKD and diabetes. The current ESC guidelines recommend that cardiovascular risk factors (hypertension, hyperlipidemia, and hyperglycemia) are medically treated to target values in patients with CCS and concomitant CKD,6 although blood pressure and hemoglobin A1c target values vary depending on severity of CKD and the presence of other cardiovascular risk factors and comorbidities.33,34 The guidelines are, however, not based on studies of patients with established CCS. Instead, they are based on studies either examining the risk of CKD or the risk of cardiovascular outcomes in patients with CKD.
Limitations
The study was conducted in a country with a tax-based health-care system, reducing selection bias caused by selective inclusion of specific hospitals, health insurance systems, or age groups. Follow-up and outcome ascertainment were standardized through high-quality registers, and patients were followed until death, emigration, or end of follow-up. Information bias or differential outcome misclassification are therefore unlikely to have affected our results. The study population consisted of patients referred for elective CAG on suspicion of CAD. Thus, our results may not be directly applicable to patients in the general population, although additional comparison with a matched general population suggest that such a generalization is reasonable. We estimated eGFR based on a single value at the time of CAG, and classified patients in CKD groups accordingly. This could lead to misclassification over time due to deterioration of renal function (CKD progression), which we tried to minimize by excluding patients receiving dialysis and by terminating follow-up after a maximum of 10 years.
Conclusions
The absence of CAD is a strong negative predictor of major adverse cardiovascular events in patients with chronic kidney disease, while severely reduced kidney function is a strong positive predictor irrespectively of CAD status.
Abbreviations
BMI, body mass index; BSA, body surface area; CAD, coronary artery disease; CAG, coronary angiography; CCI, Charlson Comorbidity Index; CCS, chronic coronary syndrome; CKD, chronic kidney disease; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; DNPR, Danish National Patient Registry; eGFR, estimated glomerular filtration rate; ESC, European Society of Cardiology; HFrEF, Heart failure with reduced ejection fraction; IRR, Incidence rate ratio; MACE, major adverse cardiovascular events; MI, myocardial infarction; PAD, peripheral artery disease; WDHR, Western Denmark Heart Registry.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
KKWO has received a research grant from the Danish Cardiovascular Academy (grant no.: CPD5Y-2022001-HF). CDP has received consultancy fees from Astellas and Astra Zeneca (unrelated to this publication). CDP has also received an institutional research grant from Vifor Pharma (unrelated to this publication). CDP received payment from Boehringer Ingelheim for travel and congress fee for the ERA 2023 Conference in Milan, Italy. NHB is supported by the Novo Nordisk Foundation (grant number NNF21OC0071374) and the Augustinus Foundation (grant number 20-1902) (unrelated to this publication). MM is supported by a grant from the Novo Nordisk Foundation (grant number NNF22OC0074083); has received institutional research grants from Novo Nordisk and Bayer; and has received lecture and/or advisory board fees from AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, and Novo Nordisk. The authors report no other conflicts of interest in this work.
References
1. Chen TK, Knicely DH, Grams ME. Chronic kidney disease diagnosis and management: a review. JAMA. 2019;322(13):1294–1304. doi:10.1001/jama.2019.14745
2. Collaborators GBDCo D. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi:10.1016/S0140-6736(17)32152-9
3. Webster AC, Nagler EV, Morton RL, Masson P. Chronic kidney disease. Lancet. 2017;389(10075):1238–1252. doi:10.1016/S0140-6736(16)32064-5
4. Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380(9841):601–610. doi:10.1016/S0140-6736(12)60987-8
5. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83. doi:10.1186/s12933-018-0728-6
6. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477. doi:10.1093/eurheartj/ehz425
7. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. doi:10.1056/NEJMoa041031
8. Vidal-Petiot E, Greenlaw N, Kalra PR, et al. Chronic kidney disease has a graded association with death and cardiovascular outcomes in stable coronary artery disease: an analysis of 21,911 patients from the CLARIFY registry. J Clin Med. 2019;9(1):4. doi:10.3390/jcm9010004
9. Edfors R, Szummer K, Evans M, et al. Renal function is associated with long-term outcomes independent of degree of atherosclerosis: 6-year data from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J Qual Care Clin Outcomes. 2016;2(2):91–98. doi:10.1093/ehjqcco/qcv029
10. Olesen KKW, Madsen M, Gyldenkerne C, et al. Ten-year cardiovascular risk in diabetes patients without obstructive coronary artery disease: a retrospective Western Denmark cohort study. Cardiovasc Diabetol. 2021;20(1):23. doi:10.1186/s12933-021-01212-x
11. Olesen KKW, Madsen M, Egholm G, et al. Patients with diabetes without significant angiographic coronary artery disease have the same risk of myocardial infarction as patients without diabetes in a real-World population receiving appropriate prophylactic treatment. Diabetes Care. 2017;40(8):1103–1110. doi:10.2337/dc16-2388
12. Olesen KKW, Riis AH, Nielsen LH, et al. Risk stratification by assessment of coronary artery disease using coronary computed tomography angiography in diabetes and non-diabetes patients: a study from the Western Denmark Cardiac Computed Tomography Registry. Eur Heart J Cardiovasc Imaging. 2019;20(11):1271–1278. doi:10.1093/ehjci/jez010
13. Gyldenkerne C, Olesen KK, Thrane PG, et al. Diabetes is not a risk factor for myocardial infarction in patients without coronary artery disease: a study from the Western Denmark Heart Registry. Diab Vasc Dis Res. 2020;17(4):1479164120941809. doi:10.1177/1479164120941809
14. Olesen KKW, Madsen M, Gyldenkerne C, et al. Diabetes mellitus is associated with increased risk of ischemic stroke in patients with and without coronary artery disease. Stroke. 2019;50(12):3347–3354. doi:10.1161/STROKEAHA.119.026099
15. Olesen KKW, Gyldenkerne C, Thim T, Thomsen RW, Maeng M. Peripheral artery disease, lower limb revascularization, and amputation in diabetes patients with and without coronary artery disease: a cohort study from the Western Denmark Heart Registry. BMJ Open Diabetes Res Care. 2021;9(1):e001803. doi:10.1136/bmjdrc-2020-001803
16. Steensig K, Olesen KKW, Thim T, et al. CAD is an independent risk factor for stroke among patients with atrial fibrillation. J Am Coll Cardiol. 2018;72(20):2540–2542. doi:10.1016/j.jacc.2018.08.1046
17. Schmidt M, Maeng M, Madsen M, Sorensen HT, Jensen LO, Jakobsen CJ. The Western Denmark Heart Registry: its Influence on cardiovascular patient care. J Am Coll Cardiol. 2018;71(11):1259–1272. doi:10.1016/j.jacc.2017.10.110
18. Schmidt M, Pedersen L, Sorensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
19. Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi:10.2147/CLEP.S91125
20. Pottegard A, Schmidt SAJ, Wallach-Kildemoes H, Sorensen HT, Hallas J, Schmidt M. Data resource profile: the Danish National Prescription Registry. Int J Epidemiol. 2017;46(3):798–798f. doi:10.1093/ije/dyw213
21. Helweg-Larsen K. The Danish Register of causes of death. Scand J Public Health. 2011;39(7_suppl):26–29. doi:10.1177/1403494811399958
22. Verbraecken J, Van de Heyning P, De Backer W, Van Gaal L. Body surface area in normal-weight, overweight, and obese adults. A comparison study. Metabolism. 2006;55(4):515–524. doi:10.1016/j.metabol.2005.11.004
23. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
24. Levin A, Stevens PE. Summary of KDIGO 2012 CKD guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49–61. doi:10.1038/ki.2013.444
25. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
26. Li P, Stuart EA, Allison DB. Multiple imputation: a flexible tool for handling missing data. JAMA. 2015;314(18):1966–1967. doi:10.1001/jama.2015.15281
27. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi:10.1093/aje/kwh090
28. Rangaswami J, Bhalla V, Blair JEA, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2019;139(16):e840–e878. doi:10.1161/CIR.0000000000000664
29. Shiba N, Shimokawa H. Chronic kidney disease and heart failure--bidirectional close link and common therapeutic goal. J Cardiol. 2011;57(1):8–17. doi:10.1016/j.jjcc.2010.09.004
30. Davoodi G, Mehrabi Pari S, Rezvanfard M, et al. Glomerular filtration rate is related to severity of obstructive coronary artery disease in patients undergoing coronary angiography. Int Urol Nephrol. 2012;44(4):1161–1168. doi:10.1007/s11255-011-0070-3
31. Dusing P, Zietzer A, Goody PR, et al. Vascular pathologies in chronic kidney disease: pathophysiological mechanisms and novel therapeutic approaches. J Mol Med (Berl). 2021;99(3):335–348. doi:10.1007/s00109-021-02037-7
32. Bajaj NS, Singh A, Zhou W, et al. Coronary microvascular dysfunction, left ventricular remodeling, and clinical outcomes in patients with chronic kidney impairment. Circulation. 2020;141(1):21–33. doi:10.1161/CIRCULATIONAHA.119.043916
33. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of Blood pressure in chronic kidney disease. Kidney Int Suppl. 2012;2(5): 337–414.
34. Kidney Disease: Improving Global Outcomes Diabetes Work G. KDIGO 2020 Clinical Practice Guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98(4S):S1–S115. doi:10.1016/j.kint.2020.06.019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



