Back to Journals » Journal of Inflammation Research » Volume 16
A Predictive Model of New-Onset Atrial Fibrillation After Percutaneous Coronary Intervention in Acute Myocardial Infarction Based on the Lymphocyte to C-Reactive Protein Ratio
Authors Gao Z , Bao J, Wu L, Shen K, Yan Q , Ye L, Wang L
Received 5 October 2023
Accepted for publication 3 December 2023
Published 13 December 2023 Volume 2023:16 Pages 6123—6137
DOI https://doi.org/10.2147/JIR.S443319
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Zhicheng Gao,1,2,* Jiaqi Bao,1,2,* Liuyang Wu,2 Kaiyu Shen,1 Qiqi Yan,2 Lifang Ye,2 Lihong Wang2
1The Second Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou, 310053, People’s Republic of China; 2Heart Center, Department of Cardiovascular Medicine, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital), Hangzhou Medical College, Hangzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lihong Wang, Heart Center, Department of Cardiovascular Medicine, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital), Hangzhou Medical College, Hangzhou, Zhejiang, People’s Republic of China, Tel +86 85894275, Email [email protected]
Purpose: Lymphocyte to C-reactive protein ratio (LCR) is a recognized systemic inflammatory marker and novel prognostic indicator for several cancers. This study investigated the relationship between preoperative LCR and new-onset atrial fibrillation (NOAF) in patients with acute myocardial infarction (AMI) after percutaneous coronary intervention (PCI).
Patients and Methods: Patients with AMI (n=662) with no history of atrial fibrillation (AF) were enrolled and classified into NOAF and non-NOAF groups based on the occurrence of postoperative NOAF during hospitalization. Logistic regression models were used to analyze NOAF risk factors and to assess the association between preoperative LCR and NOAF incidence. We constructed a new nomogram from the selected NOAF risk factors, and tested its predictive performance, degree of calibration, and clinical utility using receiver operating characteristic and calibration curves, decision curve analysis, and clinical impact curves.
Results: Overall, 84 (12.7%) patients developed NOAF during hospitalization. The LCR was significantly lower in the NOAF group. Preoperative LCR accurately predicted NOAF after AMI and was correlated with increased NOAF risk. Age, body mass index, diabetes, serum albumin levels, uric acid levels, left atrium (LA) diameter, left ventricular ejection fraction, left circumflex artery stenosis > 50%, and Killip class II status were independent predictors of NOAF after AMI. In addition, a new nomogram combined with LCR was constructed to stratify the risk of NOAF in patients with AMI. The performance of the new nomogram was satisfactory, as shown by the receiver operating characteristic curve, calibration curve, decision curve analysis and clinical impact curve.
Conclusion: Preoperative LCR was an independent predictor of NOAF in patients with AMI after PCI. The novel nomogram combined with LCR could rapidly and individually identify and treat patients at a high risk of NOAF.
Keywords: C-reactive protein, acute myocardial infarction, atrial fibrillation, nomogram, left ventricular ejection fraction
Introduction
Atrial fibrillation (AF) is among the most common clinical arrhythmias, and new-onset atrial fibrillation (NOAF) is the most common complication after acute myocardial infarction (AMI), with an incidence rate of 6–21%.1 NOAF increases in-hospital mortality and is associated with poor long-term prognosis.2,3 Although many factors play a role in the occurrence and development of NOAF, the exact mechanisms remain unclear.4,5 Therefore, early identification of AMI patients who are at a higher risk of developing NOAF is critical.
The lymphocyte to C-reactive protein ratio (LCR) is a recognized marker reflecting a systemic inflammatory state, and it has been identified as a novel prognostic indicator for gastric cancer,6 hepatocellular carcinoma,7 intrahepatic cholangiocarcinoma,8 gallbladder cancer,9 and colorectal cancer.10 It can also effectively predict the mortality rate of hemodialysis patients.11 Recent studies have revealed LCR as a potential independent predictor of poor prognosis in ST-segment elevation myocardial infarction (STEMI) patients after percutaneous coronary intervention (PCI).12 This suggests that the relationship between lymphocytes and C-reactive protein is beginning to be evaluated as a marker of inflammation in cardiovascular events. Inflammation plays a crucial role in the occurrence and development of NOAF.13 Systemic immune- inflammation index14 and systemic inflammatory response index15 have been shown to be associated with the development of AF. The novel inflammatory marker fibrinogen- to-albumin ratio can also predict NOAF after PCI in patients with AMI.16 However, to the best of our knowledge, the value of LCR in predicting NOAF in AMI patients after PCI has not yet been studied.
Therefore, this study aimed to evaluate the value of LCR in predicting NOAF in AMI patients after PCI. Additionally, we developed a simple nomogram for clinicians to better predict the incidence of NOAF in AMI patients and optimize their clinical management.
Materials and Methods
Study Population
This single-center, retrospective study was performed at the Zhejiang Provincial People’s Hospital (Hangzhou, China). We included 755 AMI patients without a history of AF who had undergone PCI at Zhejiang Provincial People’s Hospital between January 2019 and January 2021. The included AMI patients met the diagnostic criteria of AMI set by the European College of Cardiology/American College of Cardiology.17,18 We excluded the following participants: (1) age < 18 years; (2) congenital heart disease or severe valvular heart disease; (3) severe liver insufficiency; (4) end-stage renal disease (estimated glomerular filtration rate [eGFR] < 15 mL/min/1.73 m2); (5) malignant tumor, severe infection, or hematological disease; (6) death during hospitalization; and (7) lack of data. Finally, 662 patients were included in the analysis (Figure 1).
 |
Figure 1 Flow chart of the study population. Abbreviations: AMI, acute myocardial infarction; NOAF, new-onset atrial fibrillation. |
Definitions
NOAF was defined as a type of AF that occurred during postoperative hospitalization in patients without a previous history of AF. It was defined using AF episodes (≥ 30 seconds in duration) that were recorded using continuous telemetry, 12-lead electrocardiogram (ECG), or Holter monitoring throughout the duration of hospitalization. Further, LCR was defined as the lymphocyte count/C-reactive protein count in laboratory tests performed on the day of admission. Body mass index (BMI) was defined as weight (kg) divided by the square of the height (m). Coronary artery stenosis was defined as coronary angiography showing ≥ 50% stenosis of any coronary artery (including the left main artery, left anterior descending branch, left circumflex branch, and right coronary artery). The Killip class was defined as follows: class I, no signs of heart failure; class II, the lungs had rales, but the scope of the rales was less than 1/2 the lung field; class III, the range of pulmonary rales was greater than 1/2 the lung field; and class IV, cardiogenic shock with varying degrees of hemodynamic change.19
Data Collection
The following clinical information was obtained from the patient’s medical records: demographic data (age, sex, height, weight, BMI, heart rate, systolic blood pressure, diastolic blood pressure, current smoking and drinking status, and drug use); laboratory test results on the day of admission (leukocytes, neutrophils, monocytes, lymphocytes, C-reactive protein, LCR, platelets, red blood cells, hemoglobin, serum albumin, total cholesterol, triglycerides, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, creatinine, uric acid, eGFR, B-type natriuretic peptide [BNP], and cardiac troponin I [cTnI]); presence of comorbidities (hypertension, diabetes, history of stroke, history of coronary heart disease, and chronic obstructive pulmonary disease [COPD]); echocardiographic results (left atrium [LA] diameter and left ventricular ejection fraction [LVEF]); AMI type; coronary artery stenosis type; and Killip class. NOAF was recorded using continuous telemetry, ECG, or dynamic electrocardiography during postoperative hospitalization.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics (version 25.0; SPSS Inc., Chicago, IL, USA) and R version 4.1.0 (The R Project for Statistical Computing, Vienna, Austria). GraphPad Prism (version 8.0.0) was used to create the graphics. The Kolmogorov–Smirnov test was used to evaluate the normality of the distribution for continuous variables, and those with a normal distribution were described as mean ± standard deviation and analyzed by Student’s t-test. Continuous variables with non-normal distributions were described as median (interquartile range [IQR]) and analyzed using the Mann–Whitney U-test. The classified variables were described as frequency (percentage) and analyzed by the χ2 test or Fisher’s exact test. Univariate and multivariate logistic regression models were used to determine the relationship between the variables and NOAF. Potential risk factors determined by the univariate analysis were tested using multicollinearity analysis. For variables with tolerances < 0.2 or a variance inflation factor (VIF) > 5, more meaningful variables were incorporated into multivariate analysis according to experience to determine the independent risk factors related to NOAF after AMI. Furthermore, we divided the LCR levels into quartiles and performed the Mantel–Haenszel χ2 test to evaluate whether the relationship between LCR levels and the incidence of NOAF was linear. Pearson’s correlation coefficient was used to analyze the correlation between the two variables. Through logical regression analysis, the median value of the quartile was used as a quasi-continuous variable to calculate the P-value of the trend. The receiver operating characteristic (ROC) curve was used to determine the predictive performance of LCR for NOAF after AMI. We further evaluated the predictive performance of LCR using a subgroup analysis of AMI.
In this study, R version 4.1.0 was used to construct the novel nomogram. The ROC curve analysis was used to evaluate the predictive ability of the nomogram. The consistency between actual and predicted probabilities was evaluated using a calibration curve. Decision curve analysis (DCA) and clinical impact curves (CICs) were used to evaluate the clinical practicability of the novel nomograms. All statistical analyses were two-tailed with 95% confidence intervals (CI). A two-tailed P-value < 0.05 was considered statistically significant.
Results
Baseline Characteristics
The baseline data of all the patients are summarized in Table 1. A total of 662 AMI patients with no history of AF were included in this study, including 325 (49.1%) patients with STEMI and 337 (50.9%) patients without STEMI. Eighty-four (12.7%) patients developed NOAF during hospitalization, whereas 578 (87.3%) patients did not. Killip class > II was found in 31 patients (36.9%) in the NOAF group and in only 20 patients (3.5%) in the non-NOAF group (P < 0.05). There were 35 (41.7%) patients with diabetes and 4 (4.8%) patients with COPD in the NOAF group and 144 (24.9%) and 6 (1.0%) patients in the non-NOAF group, respectively. In the NOAF group, 74 patients (88.1%) had left circumflex artery stenosis > 50% and 52 patients (61.9%) had left anterior descending artery stenosis > 50%, while in the non-NOAF group, there were 438 patients (75.8%) and 286 patients (49.5%) respectively. Moreover, compared to patients in the non-NOAF group, those in the NOAF group were older; had a faster heart rate; had a larger LA diameter; and had higher levels of neutrophils, high-sensitivity C-reactive protein, serum creatinine, uric acid, and BNP (P < 0.05). Body weight, BMI, systolic blood pressure, diastolic blood pressure, lymphocyte and red blood cell counts, LCR, hemoglobin, serum albumin, total cholesterol, triglyceride, low-density lipoprotein cholesterol, eGFR, and LVEF were lower in the NOAF group than that in the non-NOAF group (P < 0.05). There were no statistically significant differences between the two groups with respect to sex, height, current smoking or drinking status, history of hypertension, stroke, coronary heart disease, current medication, white blood cells, neutrophils, platelet count, high-density lipoprotein cholesterol, cTnI, AMI type, or the proportion of patients with left main and right coronary artery stenosis > 50%.
 |
Table 1 Patients Characteristics |
Clinical Predictors of NOAF After AMI
The test variables were included in the univariate logistic regression analysis, and a multicollinearity analysis was performed. The results are shown in Table 2. The risk of NOAF was associated with a higher prevalence of type 2 diabetes (odds ratio [OR] = 2.153, 95% confidence interval [CI]:1.342–3.455, P < 0.001) and COPD (OR = 4.767, 95% CI: 1.317–17.258, P = 0.017). Moreover, the risk of NOAF in patients with left circumflex artery stenosis > 50% (OR = 2.365, 95% CI: 1.190–4.703, P = 0.014), left anterior descending artery stenosis > 50% (OR = 1.659, 95% CI: 1.037–2.653, P = 0.035), and Killip class > II (OR = 16.319, 95% CI: 8.702–30.603, P < 0.001) was higher than that of patients with left circumflex artery stenosis ≤ 50%, left anterior descending artery stenosis ≤ 50%, and Killip class ≤ II, respectively. Further, continuous variables such as age, BMI, heart rate, systolic blood pressure, diastolic blood pressure, LCR, neutrophil count, red blood cell count, hemoglobin, albumin, total cholesterol, triglyceride, low-density lipoprotein cholesterol, serum creatinine, uric acid, eGFR, BNP, LA diameter, and LVEF were potential clinical predictors of NOAF after AMI. Multicollinearity analysis revealed multicollinearity between red blood cells and hemoglobin and between total cholesterol and low-density lipoprotein cholesterol (tolerance < 0.200, VIF > 5). Therefore, we selected hemoglobin, low-density lipoprotein cholesterol, and other variables for the multivariate analysis. After adjusting for confounding factors, we found that a lower LCR was an important independent risk factor for NOAF after AMI (OR = 0.470, 95% CI: 0.234–0.942, P = 0.033). Simultaneously, multivariate analysis revealed other important predictors as follows: age (OR = 1.081, 95% CI: 1.038–1.127, P < 0.001), BMI (OR = 0.751, 95% CI: 0.661–0.852, P < 0.001), diabetes (OR = 2.406, 95% CI: 1.144–5.059, P = 0.021), serum albumin (OR = 0.888, 95% CI: 0.801–0.985, P=0.024), uric acid (OR = 1.007, 95% CI: 1.003–1.010, P < 0.001), LA diameter (OR = 1.234, 95% CI: 1.144–1.332, P < 0.001), LVEF (OR = 0.966, 95% CI: 0.934–0.999, P = 0.045), left circumflex artery stenosis > 50% (OR = 5.564, 95% CI: 1.794–17.257, P = 0.003), and Killip class > II (OR = 5.052, 95% CI: 1.909–13.371, P = 0.001) (Table 3).
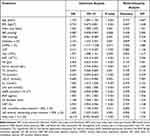 |
Table 2 Potential Clinical Predictors for NOAF After AMI |
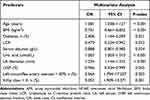 |
Table 3 Independent Clinical Predictors for NOAF After AMI |
LCR: A Good Predictor of NOAF After AMI
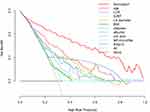
The ROC curve of LCR (Figure 2) could accurately predict the occurrence of NOAF after AMI (area under the curve [AUC]=0.756, 95% CI: 0.703–0.808). An LCR < 0.197 could distinguish patients at risk for NOAF with a sensitivity of 67.9% and specificity of 73.7% (maximum Youden index J, 0.416). Furthermore, its predictive ability was better than that of lymphocytes (AUC=0.698, 95% CI: 0.638–0.757) and CRP (AUC=0.712, 95% CI: 0.656–0.768) (Figure 2). Simultaneously, according to the AMI type, we analyzed the ROC curves of the two subgroups (Figure 3). Notably, LCR exhibited consistently good predictive performance in both the subgroups: AUC=0.786 (95% CI: 0.720–0.852) in the STEMI subgroup and AUC=0.735 (95% CI: 0.648–0.822) in the NSTEMI subgroup. We then divided LCR levels into quartiles to evaluate whether there was a linear relationship between LCR levels and the incidence of NOAF after AMI. The incidence was 3.0% in patients with an LCR > 1.207, 6.0% in patients with an LCR of 0.434–1.207, 14.5% in patients with an LCR of 0.137–0.434, and 27.3% in patients with an LCR < 0.137 (trend, P < 0.001), which was consistent with our assumption that LCR levels are associated with an increased risk of NOAF (Table S1). Moreover, the Mantel–Haenszel χ2 test revealed a linear relationship between the two parameters, χ2 = 49.010 (P < 0.001). Graphics were used to visualize the results, as shown in Figure S1. Pearson’s correlation analysis revealed a decrease in the incidence of NOAF with an increase in LCR (R= −0.272, P < 0.001).
 |
Figure 2 Receiver operating characteristic (ROC) curves of lymphocyte to C-reactive protein ratio (LCR), C-reactive protein (CRP) and lymphocyte (Lym). Abbreviation: AUC, area under curve. |
Nomogram for NOAF After AMI
In our study, age, BMI, diabetes, LCR, serum albumin, uric acid, LA diameter, LVEF, left circumflex artery stenosis > 50%, and Killip class > II were important predictors of NOAF after AMI (Table 3), and they were combined to construct a novel nomogram (Figure 4). The ROC curve was used to evaluate the performance of the model, and the AUC of the nomogram was 0.909 (95% CI: 0.875–0.944), indicating a good predictive performance (Figure 5). The calibration curve revealed a high fit between the predicted and observed risks of NOAF, with an average absolute error of 0.008 (Figure 6). DCA revealed that under the threshold probability of the main cohort, a greater net benefit could be obtained when using the predictive model to make clinical decisions, indicating the clinical practicability of the novel nomogram (Figure 7). Similarly, CIC confirmed that the predictive model had a high clinical efficacy rate (Figure 8).
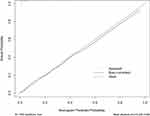 |
Figure 6 Calibration curve for the nomogram to predict the incidence of new-onset atrial fibrillation (NOAF) in patients with acute myocardial infarction (AMI). |
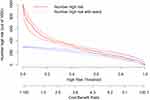 |
Figure 8 Clinical impact curve (CIC) for the incidence of new-onset atrial fibrillation (NOAF) in patients with acute myocardial infarction (AMI), demonstrating the net benefit of using the nomogram. |
Discussion
Our study analyzed the potential independent risk predictors of NOAF in 662 AMI patients treated with PCI at the Zhejiang Provincial People’s Hospital (Hangzhou, China). After adjusting for the confounding factors, we found that age, BMI, diabetes, LCR, serum albumin levels, uric acid levels, LA diameter, LVEF, left circumflex artery stenosis > 50%, and Killip class > II (Table 3) were independently associated with NOAF in AMI patients. Among them, LCR exhibited a good ability to predict NOAF after AMI (AUC=0.756; 95% CI: 0.703–0.808); in addition, LCR exhibited good predictive ability in the AMI subgroup. Our results also revealed that the incidence of NOAF after AMI decreased with an increase in LCR at admission. Furthermore, we established a novel nomogram including LCR, which performed well in predicting the incidence of NOAF after AMI (AUC=0.909, 95% CI: 0.875–0.944). Calibration curves, DCA, and CICs revealed that our nomogram had excellent clinical effectiveness. To the best of our knowledge, this is the first study to build a nomogram incorporating LCR to predict NOAF in AMI patients.
NOAF is the most common complication after AMI, which prolongs the length of hospital stay and increases the in-hospital mortality of patients, and is also associated with poor long-term prognosis.2,3 The prevalence of NOAF in AMI patients is approximately 6–21%.1 In our study, approximately 12.7% of AMI patients developed NOAF, which was consistent with previous research results.
Previous studies have found that the incidence of AF increases with age, and that advanced age is a clear risk factor for AF.20 Other studies have found that older age is associated with an increased risk of NOAF in AMI patients,21 which aligns with the findings of our study.
BMI is an important standard used internationally to measure the degree of obesity in humans. Numerous studies have shown that elevated BMI is associated with an increased short- and long-term risk of developing AF, both in healthy populations and in patients with diabetes.22–25 However, some studies have concluded that in patients with advanced heart failure, obesity is not only associated with increased mortality but may also be associated with higher survival rates.26 Among patients with stable coronary artery disease and those with acute coronary syndrome undergoing PCI, patients who are obese may have a more favorable prognosis.27,28 In a cohort study, Liu et al29 found a negative correlation between BMI and NOAF after AMI; that is, a lower BMI was associated with a higher risk of NOAF. Our results also support this “obesity paradox”.
It is well known that diabetes is significantly associated with a higher risk of developing AF,30,31 and the risk of developing AF increases by 3% for each additional year of treatment in patients with diabetes.32 Similar to previous findings, we found that after adjusting for confounding factors, diabetes was still an independent predictor of NOAF in AMI patients, which may be due to hyperglycemia directly reducing parasympathetic activity, resulting in cardiac autonomic neuropathy with relatively high sympathetic nervous system activity.33,34 Concurrently, diabetic patients are often complicated by metabolic syndrome, which causes myocardial inflammation, myocardial steatosis, and endothelial dysfunction, resulting in atrial structure and electrical remodeling and eventually, NOAF.35
Serum albumin is a protein that reflects the nutritional status of an individual. Previous studies found that low albumin levels increased the risk of coronary heart disease.36 Other studies have revealed that low albumin levels may be associated with the occurrence and development of AF.37 A recent meta-analysis found a negative linear relationship between serum albumin levels and the risk of AF,38 which was similar to our results. We clearly recognized the anti-inflammatory properties of albumin. Lower albumin levels may have a negative effect on anti-inflammatory properties and oxidative stress; thus, albumin plays a role in the occurrence and development of NOAF.39
Increasing studies have found that there is an association between uric acid levels and cardiovascular diseases, including AF.40,41 When the baseline uric acid level is low, a slight increase in uric acid level can lead to an increased incidence of AF in women. In men, an increase in uric acid level (ΔUA ≥ 0.3 mg/dL) was significantly associated with the incidence of AF when the baseline uric acid level was ≥ 6.5 mg/dL.42 Wang et al found that uric acid level was an independent risk factor for NOAF in older adult patients with acute non-STEMI.43 Similar to the findings of previous studies, we found that after excluding confounding factors such as age, high uric acid levels still promoted the occurrence of NOAF after AMI. Inflammation, oxidative stress, and fibrosis may be the molecular mechanisms of uric acid-induced AF.44
Reportedly, LA diameter can be used to predict the occurrence and progression of AF.45–47 In our study, LA diameter in the NOAF group was significantly larger than that in the non-NOAF group, which was consistent with the results of a retrospective study by Li et al48 in 4713 AMI patients without a history of AF, wherein LA diameter enlargement was significantly associated with increased risk of NOAF even after adjusting for confounding risk factors. The left atrial myocardium is the substrate for the occurrence and maintenance of AF;49 however, after progressive expansion and remodeling of the left atrial myocardium, the diameter of the LA increases, which indicates increased susceptibility to AF. Furthermore, LVEF was an independent predictor of NOAF after AMI in this study, which was consistent with previous studies.50,51
In our study, left circumflex artery stenosis > 50% was an independent risk factor for NOAF after AMI, which has been poorly studied. Kang et al reported in their study that AF was more common in older adult AMI patients with left circumflex artery involvement.52 The underlying mechanisms are unclear. When this vessel is large and compromised in its proximal third, it causes probably transient or permanent mitral insufficiency that acutely overloads the LA and I speculate this would be the most probable mechanism for the incidence of NOAF when left circumflex artery stenosis > 50%.53 Moreover, it is plausible that the LA is involved when the left circumflex artery is occluded, and that atrial ischemia may promote the occurrence of AF.54 Restoration of the sinus rhythm by reversal of left atrial ischemia has been reported in a patient with NOAF and proximal left circumflex occlusion.55 However, the effect of early revascularization on NOAF in AMI patients requires further investigation.
Killip classes are a diagnostic criterion for evaluating cardiac function in AMI patients. Compared with Killip classes I and II, Killip classes III and IV represent worse cardiac function. In our study, Killip class > II was an independent risk factor for NOAF, which was consistent with the results of previous studies.52,56–58 A higher Killip class may reflect more severe cardiovascular disease in these patients.
The inflammatory response after myocardial infarction is critical for cardiac repair.59 However, inflammation also plays an important role in the development and progression of NOAF after myocardial infarction.60 Lymphocytes are involved in the inflammatory response during AMI,61 which reflects the inflammatory response and stress stages of the body. In myocardial infarction, the body is in a state of stress, and elevated levels of catecholamines and cortisol lead to increased lymphocyte apoptosis, resulting in a decrease in lymphocyte count.62 Furthermore, decreased lymphocyte count has been associated with poor prognosis in patients with chronic coronary artery disease,63 unstable angina,64 and STEMI.65 Moreover, CRP, which is a typical inflammatory marker, is involved in the pathogenesis of myocardial infarction. It promotes atherosclerosis and plaque rupture by activating the complement system and inducing endothelial dysfunction, which eventually leads to myocardial infarction.66 High CRP levels are reportedly a good predictor of death in patients with acute coronary syndrome.67 CRP levels were also identified as useful for predicting NOAF.68 Therefore, LCR, which represents the ratio of the lymphocyte count to CRP level, can better reflect the degree of inflammation and the immune status of the body during myocardial infarction. Compared to lymphocytes or CRP alone, LCR can more accurately predict adverse events after PCI in patients with myocardial infarction.12 However, research on the value of LCR in predicting NOAF after PCI in AMI patients remains limited. We found that a negative correlation between LCR and NOAF after PCI in AMI patients persisted even after adjusting for the influence of confounding factors. In the subgroup analysis, the predictive performance of LCR for NOAF in the STEMI group (AUC = 0.786, 95% CI: 0.720–0.852) was better than that in the NSTEMI group (AUC = 0.735, 95% CI: 0.648–0.822), which may be due to a greater inflammatory response in STEMI.69 Additionally, the LCR levels correlated with the risk of NOAF. A lower LCR correlated with a more intense inflammatory response as well as more severe damage to the immune status, and a higher incidence of NOAF.
Nomograms are widely used to predict individual probabilities of clinical events by integrating multiple variables.70 In this study, we constructed a novel nomogram combining LCR and nine other risk factors for NOAF. Our nomogram exhibited a high clinical predictive performance and was a practical fit. Furthermore, DCA and CICs revealed greater net benefits and extremely high clinical efficiencies when the predictive model was used to make clinical decisions. The nomogram could identify patients who were truly at a high risk of NOAF and facilitate early intervention in these patients to improve clinical outcomes.
Limitations
First, this was a single-center retrospective study with a small sample size that might not have been representative of the entire population. Therefore, the association between LCR and NOAF after AMI requires further verification in a large multicenter study. Moreover, some patients were not included because of missing data, which resulted in a selection bias. Second, although we adjusted for confounding factors, other factors that were not included, such as myocardial injury markers, might also have played a role. Third, although AMI patients with lower preoperative LCR levels were more likely to develop AF after PCI, we did not explore whether anti-inflammatory therapy could reduce the risk of NOAF in these patients. In the future, anti-inflammatory therapies may be used to explore this relationship in AMI patients. Finally, we did not perform external validation of the nomogram; therefore, external validation is required to determine the applicability of the model to other patient populations.
Conclusion
A low preoperative LCR may be an independent risk factor for NOAF after PCI in AMI patients. Moreover, the novel nomogram constructed in this study exhibited a satisfactory predictive effect for NOAF, which will help develop individualized primary prevention programs for AMI patients.
Ethics Approval and Informed Consent
This study protocol was reviewed and approved by the Institutional Review Committee of the Zhejiang Provincial People’s Hospital, registration number: QT2023256. Informed consent was waived due to the retrospective nature of the study. At the same time, patient data was anonymized or maintained with confidentiality and this study was in line with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the report has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81670447), the Medicine and Health Project of Zhejiang Province (No. 2023KY531) and the Traditional Chinese Medicine Program of Zhejiang Provincial (No. 2022ZZ003, No. 2023ZL248, 2022ZB024). LW was sponsored by Ten-thousand Talents Program of Zhejiang Province (No. 2021R52025).
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could appear to influence the work reported in this paper.
References
1. Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009;30(9):1038–1045. doi:10.1093/eurheartj/ehn579
2. Morishima I, Tomomatsu T, Okumura K, et al. New-onset atrial fibrillation may be a more important predictor of cardiac mortality in acute myocardial infarction patients than preexisting atrial fibrillation. Int J Cardiol. 2015;187:475–477. doi:10.1016/j.ijcard.2015.03.379
3. Petersen JK, Butt JH, Yafasova A, et al. Incidence of ischaemic stroke and mortality in patients with acute coronary syndrome and first-time detected atrial fibrillation: a nationwide study. Eur Heart J. 2021;42(44):4553–4561. doi:10.1093/eurheartj/ehab575
4. Kornej J, Hanger VA, Trinquart L, et al. New biomarkers from multiomics approaches: improving risk prediction of atrial fibrillation. Cardiovasc Res. 2021;117(7):1632–1644. doi:10.1093/cvr/cvab073
5. Boriani G, Vitolo M, Diemberger I, et al. Optimizing indices of atrial fibrillation susceptibility and burden to evaluate atrial fibrillation severity, risk and outcomes. Cardiovasc Res. 2021;117(7):1–21. doi:10.1093/cvr/cvab147
6. Okugawa Y, Toiyama Y, Yamamoto A, et al. Lymphocyte-to-C-reactive protein ratio and score are clinically feasible nutrition-inflammation markers of outcome in patients with gastric cancer. Clin Nutr. 2020;39(4):1209–1217. doi:10.1016/j.clnu.2019.05.009
7. Minici R, Siciliano MA, Ammendola M, et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio (NLR), Lymphocyte-to-Monocyte Ratio (LMR), Platelet-to-Lymphocyte Ratio (PLR) and Lymphocyte-to-C Reactive Protein Ratio (LCR) in Patients with Hepatocellular Carcinoma (HCC) undergoing Chemoembolizations (TACE) of the Liver: the Unexplored Corner Linking Tumor Microenvironment, Biomarkers and Interventional Radiology. Cancers. 2022;15(1):257. doi:10.3390/cancers15010257
8. L-H L, Zhong C, Wei W, et al. Lymphocyte-C-reactive protein ratio as a novel prognostic index in intrahepatic cholangiocarcinoma: a multicentre cohort study. Liver Int. 2021;41(2):378–387. doi:10.1111/liv.14567
9. Yao W-Y, X-S W, Liu S-L, Z-Y W, Dong P, Gong W. Preoperative lymphocyte to C-reactive protein ratio as a new prognostic indicator in patients with resectable gallbladder cancer. Hepatobiliary Pancreat Dis Int. 2022;21(3):267–272. doi:10.1016/j.hbpd.2021.08.006
10. Okugawa Y, Toiyama Y, Yamamoto A, et al. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Ann Surg. 2020;272(2):342–351. doi:10.1097/SLA.0000000000003239
11. Chen X, Guo W, Diao Z, Huang H, Liu W. Lymphocyte-to-C reactive protein ratio as novel inflammatory marker for predicting outcomes in hemodialysis patients: a multicenter observational study. Front Immunol. 2023;14:1101222. doi:10.3389/fimmu.2023.1101222
12. Liu Y, Ye T, Chen L, Xu B, Wu G, Zong G. Preoperative lymphocyte to C-reactive protein ratio: a new prognostic indicator of post-primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction. Int Immunopharmacol. 2023;114:109594. doi:10.1016/j.intimp.2022.109594
13. Ruiz LA, Serrano L, España PP, et al. New-onset atrial fibrillation in patients with pneumococcal pneumonia. Impact of timing and duration on short- and medium-term mortality. J Infect. 2021;82(1):67–75. doi:10.1016/j.jinf.2020.11.005
14. Bağcı A, Aksoy F. Systemic immune-inflammation index predicts new-onset atrial fibrillation after ST elevation myocardial infarction. Biomark Med. 2021;15(10):731–739. doi:10.2217/bmm-2020-0838
15. Wang J, Hu S, Liang C, Ling Y. The association between systemic inflammatory response index and new-onset atrial fibrillation in patients with ST-elevated myocardial infarction treated with percutaneous coronary intervention. BMC Cardiovasc Disord. 2022;22(1):525. doi:10.1186/s12872-022-02989-9
16. Bao J, Gao Z, Hu Y, Liu W, Ye L, Wang L. Serum fibrinogen-to-albumin ratio predicts new-onset atrial fibrillation risk during hospitalization in patients with acute myocardial infarction after percutaneous coronary intervention: a retrospective study. BMC Cardiovasc Disord. 2023;23(1):432. doi:10.1186/s12872-023-03480-9
17. Collet J-P, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289–1367. doi:10.1093/eurheartj/ehaa575
18. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368–e454. doi:10.1161/CIR.0000000000001029
19. Mercado-Martínez J, Rivera-Fernández R, Aguilar-Alonso E, et al. APACHE-II score and Killip class for patients with acute myocardial infarction. Intensive Care Med. 2010;36(9):1579–1586. doi:10.1007/s00134-010-1832-6
20. Kornej J, Börschel CS, Benjamin EJ, Schnabel RB. Epidemiology of atrial fibrillation in the 21st Century: novel methods and new insights. Circ Res. 2020;127(1). doi:10.1161/CIRCRESAHA.120.316340
21. He J, Yang Y, Zhang G, Lu X-H. Clinical risk factors for new-onset atrial fibrillation in acute myocardial infarction: a systematic review and meta-analysis. Medicine. 2019;98(26):e15960. doi:10.1097/MD.0000000000015960
22. Tedrow UB, Conen D, Ridker PM, et al. The long- and short-term impact of elevated body mass index on the risk of new atrial fibrillation the WHS (women’s health study). J Am Coll Cardiol. 2010;55(21):2319–2327. doi:10.1016/j.jacc.2010.02.029
23. Aune D, Sen A, Schlesinger S, et al. Body mass index, abdominal fatness, fat mass and the risk of atrial fibrillation: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2017;32(3):181–192. doi:10.1007/s10654-017-0232-4
24. Singleton MJ, German CA, Soliman EZ, et al. Body mass index, sex, and incident atrial fibrillation in diabetes: the ACCORD trial. JACC Clin Electrophysiol. 2020;6(13):1713–1720. doi:10.1016/j.jacep.2020.08.008
25. Berkovitch A, Kivity S, Klempfner R, et al. Body mass index and the risk of new-onset atrial fibrillation in middle-aged adults. Am Heart J. 2016;173:41–48. doi:10.1016/j.ahj.2015.11.016
26. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Woo MA, Tillisch JH. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001;38(3):789–795.
27. Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39(4):578–584.
28. Angerås O, Albertsson P, Karason K, et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34(5):345–353. doi:10.1093/eurheartj/ehs217
29. Liu L, Liu X, Ding X, Chen H, Li H. Body Mass Index and New-Onset Atrial Fibrillation in patients with acute myocardial infarction. Int J Gen Med. 2022;15:5717–5728. doi:10.2147/IJGM.S367868
30. Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271(11):840–844.
31. Wang A, Green JB, Halperin JL, Piccini JP. Atrial fibrillation and diabetes mellitus: JACC review topic of the week. J Am Coll Cardiol. 2019;74(8):1107–1115. doi:10.1016/j.jacc.2019.07.020
32. Dublin S, Glazer NL, Smith NL, et al. Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J Gen Intern Med. 2010;25(8):853–858. doi:10.1007/s11606-010-1340-y
33. Olshansky B, Sabbah HN, Hauptman PJ, Colucci WS. Parasympathetic nervous system and heart failure: pathophysiology and potential implications for therapy. Circulation. 2008;118(8):863–871. doi:10.1161/CIRCULATIONAHA.107.760405
34. Pappachan JM, Sebastian J, Bino BC, et al. Cardiac autonomic neuropathy in diabetes mellitus: prevalence, risk factors and utility of corrected QT interval in the ECG for its diagnosis. Postgrad Med J. 2008;84(990):205–210. doi:10.1136/pgmj.2007.064048
35. Bell DSH, Goncalves E. Atrial fibrillation and type 2 diabetes: prevalence, etiology, pathophysiology and effect of anti-diabetic therapies. Diabetes Obes Metab. 2019;21(2):210–217. doi:10.1111/dom.13512
36. Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279(18):1477–1482.
37. Schillinger M, Exner M, Mlekusch W, et al. Serum albumin predicts cardiac adverse events in patients with advanced atherosclerosis - interrelation with traditional cardiovascular risk factors. Thromb Haemost. 2004;91(3):610–618.
38. Wang Y, Du P, Xiao Q, et al. Relationship between serum albumin and risk of atrial fibrillation: a dose-response meta-analysis. Front Nutr. 2021;8:728353. doi:10.3389/fnut.2021.728353
39. Korantzopoulos P, Kolettis TM, Galaris D, Goudevenos JA. The role of oxidative stress in the pathogenesis and perpetuation of atrial fibrillation. Int J Cardiol. 2007;115(2):135–143.
40. Saito Y, Tanaka A, Node K, Kobayashi Y. Uric acid and cardiovascular disease: a clinical review. J Cardiol. 2021;78(1):51–57. doi:10.1016/j.jjcc.2020.12.013
41. Hisatome I, Li P, Miake J, et al. Uric Acid as a risk factor for chronic kidney disease and cardiovascular disease- Japanese Guideline on the management of asymptomatic hyperuricemia. Circ J. 2021;85(2):130–138. doi:10.1253/circj.CJ-20-0406
42. Kawasoe S, Kubozono T, Yoshifuku S, et al. Uric acid level and new-onset atrial fibrillation in the Japanese General Population- Longitudinal Study. Circ J. 2018;83(1):156–163. doi:10.1253/circj.CJ-18-0508
43. Wang Y, Wang X-D, Yao J-W, et al. The impact of the duration of cardiac troponin I elevation on the clinical prognosis as well as incidence of new-onset atrial fibrillation respectively in elderly Non-ST-Elevation Acute Myocardial Infarction Patients without PCI. J Inflamm Res. 2021;14:6907–6916. doi:10.2147/JIR.S345576
44. Deng Y, Liu F, Yang X, Xia Y. The key role of uric acid in oxidative stress, inflammation, fibrosis, apoptosis, and immunity in the pathogenesis of atrial fibrillation. Front Cardiovasc Med. 2021;8:641136. doi:10.3389/fcvm.2021.641136
45. Malavasi VL, Fantecchi E, Tordoni V, et al. Atrial fibrillation pattern and factors affecting the progression to permanent atrial fibrillation. Intern Emerg Med. 2021;16(5):1131–1140. doi:10.1007/s11739-020-02551-5
46. Losi M-A, Izzo R, De Marco M, et al. Cardiovascular ultrasound exploration contributes to predict incident atrial fibrillation in arterial hypertension: the Campania Salute Network. Int J Cardiol. 2015;199:290–295. doi:10.1016/j.ijcard.2015.07.019
47. Vaziri SM, Larson MG, Benjamin EJ, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation. 1994;89(2):724–730.
48. Li Z, Liu Q, Liu F, et al. Atrial cardiomyopathy markers and new-onset atrial fibrillation risk in patients with acute myocardial infarction. Eur J Intern Med. 2022;102:72–79. doi:10.1016/j.ejim.2022.04.019
49. Brundel BJJM, Ai X, Hills MT, Kuipers MF, Lip GYH, de Groot NMS. Atrial fibrillation. Nat Rev Dis Primers. 2022;8(1):21. doi:10.1038/s41572-022-00347-9
50. Luo J, Xu S, Li H, et al. Long-term impact of new-onset atrial fibrillation complicating acute myocardial infarction on heart failure. ESC Heart Fail. 2020;7(5):2762–2772. doi:10.1002/ehf2.12872
51. Raczkowska-Golanko M, Raczak G, Gruchała M, Daniłowicz-Szymanowicz L. Comprehensive use of routine clinical parameters to identify patients at risk of new-onset atrial fibrillation in acute myocardial infarction. J Clin Med. 2021;10(16). doi:10.3390/jcm10163622
52. Kang L, Yong H, Ding YS. Clinical profile and outcomes of atrial fibrillation in elderly patients with acute myocardial infarction. Chin Med J. 2008;121(23):2388–2391.
53. Bahouth F, Mutlak D, Furman M, et al. Relationship of functional mitral regurgitation to new-onset atrial fibrillation in acute myocardial infarction. Heart. 2010;96(9):683–688. doi:10.1136/hrt.2009.183822
54. Alasady M, Abhayaratna WP, Leong DP, et al. Coronary artery disease affecting the atrial branches is an independent determinant of atrial fibrillation after myocardial infarction. Heart Rhythm. 2011;8(7):955–960. doi:10.1016/j.hrthm.2011.02.016
55. Blanton RM, Nappi A, Kimmelstiel CD. Conversion of infarction-associated atrial fibrillation by restoration of atrial perfusion. Clin Cardiol. 2010;33(12):E79–E81. doi:10.1002/clc.20573
56. Lehto M, Snapinn S, Dickstein K, Swedberg K, Nieminen MS. Prognostic risk of atrial fibrillation in acute myocardial infarction complicated by left ventricular dysfunction: the OPTIMAAL experience. Eur Heart J. 2005;26(4):350–356.
57. Crenshaw BS, Ward SR, Granger CB, Stebbins AL, Topol EJ, Califf RM. Atrial fibrillation in the setting of acute myocardial infarction: the GUSTO-I experience. Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries. J Am Coll Cardiol. 1997;30(2):406–413.
58. Rathore SS, Berger AK, Weinfurt KP, et al. Acute myocardial infarction complicated by atrial fibrillation in the elderly: prevalence and outcomes. Circulation. 2000;101(9):969–974.
59. Frangogiannis NG. The inflammatory response in myocardial injury, repair, and remodelling. Nat Rev Cardiol. 2014;11(5):255–265. doi:10.1038/nrcardio.2014.28
60. Frederiksen TC, Dahm CC, Preis SR, et al. The bidirectional association between atrial fibrillation and myocardial infarction. Nat Rev Cardiol. 2023. doi:10.1038/s41569-023-00857-3
61. Pan L, Li Z, Li C, et al. Stress hyperglycemia ratio and neutrophil to lymphocyte ratio are reliable predictors of new-onset atrial fibrillation in patients with acute myocardial infarction. Front Cardiovasc Med. 2022;9:1051078. doi:10.3389/fcvm.2022.1051078
62. Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36(3):959–969.
63. Ommen SR, Gibbons RJ, Hodge DO, Thomson SP. Usefulness of the lymphocyte concentration as a prognostic marker in coronary artery disease. Am J Cardiol. 1997;79(6):812–814.
64. Zouridakis EG, Garcia-Moll X, Kaski JC. Usefulness of the blood lymphocyte count in predicting recurrent instability and death in patients with unstable angina pectoris. Am J Cardiol. 2000;86(4):449–451.
65. Núñez J, Núñez E, Bodí V, et al. Low lymphocyte count in acute phase of ST-segment elevation myocardial infarction predicts long-term recurrent myocardial infarction. Coron Artery Dis. 2010;21(1):1–7.
66. Fordjour PA, Wang Y, Shi Y, et al. Possible mechanisms of C-reactive protein mediated acute myocardial infarction. Eur J Pharmacol. 2015;760:72–80. doi:10.1016/j.ejphar.2015.04.010
67. De Servi S, Mariani M, Mariani G, Mazzone A. C-reactive protein increase in unstable coronary disease cause or effect? J Am Coll Cardiol. 2005;46(8):1496–1502.
68. Ren Y, Zeng R-X, J-J L, et al. Relation of C-reactive protein and new-onset atrial fibrillation in patients with acute myocardial infarction: a systematic review and meta-analysis. Int J Cardiol. 2015;190:268–270. doi:10.1016/j.ijcard.2015.04.152
69. MacNeill BD, Jang I-K, Bouma BE, et al. Focal and multi-focal plaque macrophage distributions in patients with acute and stable presentations of coronary artery disease. J Am Coll Cardiol. 2004;44(5):972–979.
70. Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–e180. doi:10.1016/S1470-2045(14)71116-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.