Back to Journals » Journal of Inflammation Research » Volume 17
A Prediction Model Based on Systemic Immune-Inflammatory Index Combined with Other Predictors for Major Adverse Cardiovascular Events in Acute Myocardial Infarction Patients
Authors Li X , Yu C, Liu X, Chen Y, Wang Y, Liang H, Qiu S, Lei L, Xiu J
Received 4 October 2023
Accepted for publication 6 February 2024
Published 22 February 2024 Volume 2024:17 Pages 1211—1225
DOI https://doi.org/10.2147/JIR.S443153
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Tara Strutt
Xiaobo Li,1,2 Chen Yu,1 Xuewei Liu,3 Yejia Chen,1 Yutian Wang,1 Hongbin Liang,1 ShiFeng Qiu,1 Li Lei,1 Jiancheng Xiu1
1Department of Cardiology, Nanfang Hospital, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 2Department of Cardiology, Xiangdong Hospital, Hunan Normal University, Liling, Hunan, People’s Republic of China; 3The Tenth Affiliated Hospital of Southern Medical University (Dongguan People’s Hospital), Southern Medical University, Dongguan, Guangdong, People’s Republic of China
Correspondence: Jiancheng Xiu, Tel +8613903064940, Email [email protected]
Objective: To evaluate the prognostic value of the systemic immune-inflammatory index (SII) for predicting in-hospital major adverse cardiovascular events (MACEs) in patients with acute myocardial infarction (AMI) and establish a relevant nomogram.
Methods: This study included 954 AMI patients. We examined three inflammatory factors (SII, platelet to lymphocyte ratio (PLR) and neutrophil to lymphocyte ratio (NLR)) to see which one predicts in-hospital MACEs better. The predictors were subsequently screened using bidirectional stepwise regression method, and a MACE nomogram was constructed via logistic regression analysis. The predictive value of the model was evaluated using the area under the curve (AUC), sensitivity and specificity. In addition, the clinical utility of the nomogram was evaluated using decision curve analysis. We also compared the nomogram with the Global Registry of Acute Coronary Events (GRACE) scoring system.
Results: 334 (35.0%) patients had MACEs. The SII (AUC =0.684) had a greater predictive value for in-hospital MACEs in AMI patients than the PLR (AUC =0.597, P< 0.001) or NLR (AUC=0.654, P=0.01). The area under the curve (AUC) of the SII-based multivariable model for predicting MACEs, which was based on the SII, Killip classification, left ventricular ejection fraction, age, urea nitrogen (BUN) concentration and electrocardiogram-based diagnosis, was 0.862 (95% CI: 0.833– 0.891). Decision curve and calibration curve analysis revealed that SII-based multivariable model demonstrated a good fit and calibration and provided positive net benefits than the model without SII. The predictive value of the SII-based multivariable model was greater than that of the GRACE scoring system (P< 0.001).
Conclusion: SII is a promising, reliable biomarker for identifying AMI patients at high risk of in-hospital MACEs, and SII-based multivariable model may serve as a quick and easy tool to identify these patients.
Keywords: systemic immune-inflammatory index, major adverse cardiovascular events, inflammation, acute myocardial infarction
Introduction
Acute myocardial infarction (AMI) is a major cause of mortality worldwide and accounts for one-third of deaths in developed countries.1 AMI results from acute and persistent ischemia and hypoxia of the coronary arteries caused by rupture or erosion of unstable atherosclerotic plaques, leading to myocardial necrosis.2 Although the application of interventional therapy and improvements in drug treatments have reduced the mortality of AMI patients, the residual risk of cardiovascular events in patients remains high.3,4 The number of hospitalized AMI patients has generally increased in the past decade, while the hospitalization mortality rate has not decreased.5–7 Early identification of high-risk patients who may develop major adverse cardiac events (MACEs) after AMI is crucial for enhancing patient prognosis.
Traditional risk scoring systems, such as the Global Registry of Acute Coronary Events (GRACE), have been used to predict in-hospital death, recurrence of myocardial infarction (MI) and other MACEs in AMI patients.8 However, the predictive effectiveness of these systems, which were developed in clinical trials more than 20 years ago, may be limited due to their lack of consideration of currently widely used therapies such as drug-eluting stents (DESs) and new-generation antiplatelet therapies.9 Discovering new predictors and developing new reliable risk scoring systems for AMI patients are necessary.
Time is life, and time is the myocardium. For AMI patients, emergency treatment is often needed, especially for patients at high risk of in-hospital MACEs. However, there are few indicators that can be used to predict in-hospital MACEs in patients with AMI due to the urgency of timely diagnosis. Cardiovascular diseases are characterized by a high inflammatory burden, stable coronary artery disease and acute coronary syndrome can both lead to an increase in inflammatory markers in the blood.10–12 Additionally, risk factors for the occurrence and development of coronary artery disease are closely associated with inflammation.13–15 Acute myocardial infarction (AMI), a severe acute coronary event, has been shown to play a crucial role in inflammation during its occurrence and development.16–18 Recent clinical studies have confirmed that anti-inflammatory drugs can reduce the residual risk of cardiovascular events.19 Moreover, the Food and Drug Administration (FDA) approval of colchicine for use in patients with coronary heart diseases has further clarified that inflammation may be a valuable predictor.
However, as time is urgent in the field of AMI, only a few studies have used inflammatory indicators to predict patient prognosis. Clinically, we previously found that AMI patients exhibit changes in neutrophil, lymphocyte, and platelet counts at onset.20 These indicators can be obtained by routine blood tests, which are among the preferred laboratory tests for AMI patients, and the results can be obtained rapidly, in as little as 10 minutes.21 Increasing evidence has shown that markers of the systemic inflammatory response, such as the neutrophil (NEU) to lymphocyte (LYM) ratio (NLR) and platelet (PLT) to LYM ratio (PLR), are predictors of MACEs, such as death, MI recurrence and heart failure in AMI patients.22–25
Acute myocardial infarction not only increases inflammatory factor levels but also causes platelet activation.26 The systemic immune inflammation index (SII), which includes not only inflammatory cells (NEU and LYM) but also the PLT, was proposed as a novel and sensitive prognostic marker.22–25 Previous studies have indicated that SII is associated with inflammatory diseases such as coronary heart disease, diabetic nephropathy, and hypertension.27,28 However, only a few articles have reported the predictive value of the SII for in-hospital MACEs in patients with myocardial infarction, and no articles have included the SII in relevant predictive models.
In the present study, the association between SII and in-hospital MACEs in patients with AMI was evaluated, and prediction models based on SII and other predictors associated with in-hospital MACEs were constructed for predicting in-hospital MACEs in patients with AMI.
Methods
Study Design and Participants
This cohort study enrolled 1197 AMI patients from Xiangdong Hospital Affiliated with Hunan Normal University between Dec. 30, 2016, and Oct. 8, 2021. AMI was diagnosed based on the presence of acute myocardial injury detected from abnormal cardiac biomarkers, especially cardiac troponin (cTn), in the identification of evidence for acute myocardial ischemia according to the fourth Universal Definition of Myocardial Infarction (2018), which includes an increase and/or decrease in cardiac biomarkers with at least one value above the 99th percentile upper reference limit together with clinical symptoms of myocardial ischemia, development of pathological Q waves, new ischemic electrocardiogram (ECG) changes, or imaging evidence of myocardial ischemia.29
The inclusion criteria were as follows: (1) diagnosed with AMI according to the 4th Universal Definition of Myocardial Infarction at admission;29 (2) had complete clinical data; and (3) were aged ≥18 years.
The exclusion criteria were as follows: (1) severe uncontrolled infection (including active infection, serious systemic inflammation, and autoimmune diseases); (2) history of malignant tumors; (3) other severe cardiovascular diseases (including severe congenital heart disease, valvular heart disease, cardiomyopathy); (4) routine blood examination not completed before hospitalization intervention; (5) no high-sensitivity cTn I (hs-cTn I) records prior to hospitalization intervention; (6) referral from our hospital to other medical institutions; and (7) coronary stenting performed directly without passing through the emergency ward.
After excluding specific patients, 954 patients were ultimately included for analysis. Participants were divided into two groups based on the occurrence of MACEs: the MACEs group (n=334) and the no MACEs group (n=620). The detailed screening process is shown in Figure 1.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Xiangdong Hospital Affiliated with Hunan Normal University (No. 2021010). This clinical study has a retrospective research design, and relevant patient indicators were collected for statistical analysis, without any additional intervention measures. The risks to the subjects were caused by routine treatment, which was not considered in this study. The only risk of this study comes from the protection of privacy, so all the research materials had all identifiable patient information removed. This study was exempt from informed consent.
Data Collection
Basic information and physical examination variables included age (years), gender, systolic blood pressure (SBP), diastolic blood pressure (DBP), respiratory rate (beat/min), temperature (°C), heart rate (beat/min), and smoking history [non-smoker, former smoker (non-smoker in last year), current smoker].
Previous disease information included diabetes mellitus (yes or no), hypertension (yes or no), hyperlipidemia (yes or no), history of stroke or transient ischemic attacks (TIA) (yes or no), AMI history (yes or no).
Treatments included PCI or coronary artery bypass grafting (CABG) history (yes or no), medication history (aspirin, clopidogrel, ticagrelor, beta-blockers, statins, antihypertensive drugs, or hypoglycemic agents), interventions in other hospital (yes or no), PCI in our hospital (yes or no), thrombolytic therapy in our hospital (yes or no), and medications during hospitalization in our hospital [aspirin, clopidogrel, ticagrelor, tirofiban, anticoagulant drugs, statins, nitrate, beta-blockers, angiotensin converting enzyme inhibitor or angiotensin receptor blocker (ACEI/ARB)].
Laboratory indices included alanine aminotransferase (U/L), aspartate aminotransferase (U/L), total bilirubin (μmol/L), albumin (g/L), urea nitrogen (mmol/L), creatinine (μmol/L), uric acid (μmol/L), total cholesterol (mmol/L), triglyceride (mmol/L), low density lipoprotein (mmol/L), high-density lipoprotein (mmol/L), blood glucose (mmol/L), creatine kinase isoenzyme (ng/mL), NLR, PLR, SII, and hs-cTn I (ng/L).
Surgery-related information included thrombus formation in coronary artery, TIMI flow grade, GRACE risk score and thrombus aspiration.
Data from hospital transfers included whether the patients were transferred from another hospital, the time from onset to admission to our hospital and the intervention at another hospital (whether antiplatelet medications were taken).
Clinical data, including basic information, physical examination variables, laboratory indices, previous disease information, surgery-related information, and treatments information use within 24 hours of patient admission, were extracted from the electronic medical records. Data from hospital transfers were collected through the chest pain table The left ventricular ejection fraction was measured by Simpson’s variant method via two-dimensional echocardiography, and two experienced experts evaluated the results.30 The SII was the main variable in this study and was calculated as follows: SII=PLT×NEU/LYM. The PLT, NEU and LYM data were obtained at admission. The GRACE score is derived from eight variables that are readily available at hospital admission (age, heart rate, systolic blood pressure, serum creatinine concentration, Killip class, cardiac arrest, presence of ST-segment deviation, and elevated cardiac enzymes/markers). We classified AMIs into ST-segment elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI) based on ECG-based diagnosis. The Killip classification was determined by clinical signs of Heart Failure (HF) at admission (blood pressure, rales, pulmonary edema, cardiogenic shock). Specifically, Killip class I patients had no clinical signs of HF; Killip class II patients had mild HF with rales involving one-third or less of the posterior lung fields and/or S3 gallop; Killip class III patients presented severe HF with overt pulmonary edema; and Killip class IV patients had cardiogenic shock with a systolic blood pressure lower than 90 mmHg.31
Coronary Angiography
Standard Judkins technique was used for coronary artery visualization. At least two orthogonal plane images were acquired for each coronary artery. The coronary angiography images of each patient were independently evaluated by two experienced interventional cardiologists, and if the two experts had disparities, a third expert with more experience was consulted.
Clinical Endpoints
The primary outcome was the occurrence of MACEs during hospitalization. The MACEs analyzed in this study were all-cause death, cardiogenic shock, target vessel re-revascularization, recurrent MI after treatment during the hospitalization, unstable angina pectoris, malignant arrhythmia, heart failure, stroke or transient ischemic attack (TIA), and stent thrombosis events.32,33 All-cause death was defined as a death during hospitalization or abandonment of treatments at discharge due to a terminal condition. In China, many severe patients are reluctant to die in the hospital,5,34,35 and they choose to abandon their treatments at discharge if they are in terminal condition. These patients were grouped into the all-cause mortality group. The follow-up period was started from the admission to our hospital and ended when they discharged from hospital. During hospitalization, irrespective of the occurrence of multiple types or instances of the same MACE we categorize them uniformly as occurrences of MACE event. The median hospital stays of the MACE group was 8 days, and the non-MACE group was 7 days.
Statistical Analysis
Multiple imputation was used to fill in any missing values. Continuous data were tested for Normality using Skewness and Kurtosis, the normally distributed quantitative data are presented as the means ± standard deviations (SDs), and the nonnormally distributed quantitative data are presented as medians and quartiles [M (Q1, Q3)]. Qualitative data are described using case numbers and percentages (n %). The t-test was used for quantitative data subject to a normal distribution; the rank-sum test was used for variables with a nonnormal distribution; The chi-square test or Fisher’s exact probability method was used for qualitative data. To identify distinct groups based on the SII, an RCS curve was plotted. The dataset was completely and randomly divided into a training set and a testing set, and a prediction model was constructed with the training set and validated with the testing set. Predictors were screened by bidirectional stepwise regression method, and prediction models were constructed using logistic regression analysis. The predictive value of the model was evaluated using the area under the curve (AUC), sensitivity and specificity. The confidence level was set to 0.05, and all analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA) and R version 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Participant Characteristics
All 954 participants were enrolled and divided into a MACE group (n=620, 483 males) and a no-MACEs group (n=334, 219 males). The mean age of the MACE group was greater than that of the non-MACE group (69.19 years vs 62.58 years, p<0.001). The Killip classification significantly differed between the MACE group and the non-MACE group (p<0.001). The mean left ventricular ejection fraction in the MACE group was lower than that in the no-MACEs group (55.35 vs 60.95). The proportion of patients who received PCI was lower in the MACE group than in the non-MACE group (59.88% vs 78.06%). The median hs-cTnI level (2.34 ng/L vs 0.79 ng/L, p<0.001) and GRACE score (173.87 vs 133.46) were greater in the MACE group than in the non-MACE group. Finally, the mean SII, NLR and PLR were greater in the MACE group than in the non-MACE group (1469.55 vs 829.60, 7.01 vs 4.06, 157.34 vs 127.26). These results are summarized in Table 1.
 |
Table 1 Comparisons of Characteristics of Participants with and without MACEs |
Comparison the Predictive Value of NLR, PLR, and SII
The predictive value of the SII for MACEs in AMI patients was assessed. The restricted cubic spline (RCS) curve indicated that when the SII was ≥970 (Supplementary Figure 1), the NLR was ≥5.10, and the PLR was ≥138, the OR for MACEs in AMI patients was >1, indicating that the risk of MACEs in these patients might increase. We found that a SII≥970 (OR=4.87, 95% CI=3.62–6.55), a NLR≥5.10 (OR=3.60, 95% CI=2.71–4.78) and a PLR≥138 (OR=2.19, 95% CI=1.67–2.88) were associated with an increased risk of MACEs. The AUC values of the SII, NLR and PLR for predicting MACEs in AMI patients were 0.684 (95% CI=0.654–0.714), 0.654 (95% CI=0.623–0.685) and 0.597 (95% CI=0.564–0.629), respectively. The results of the DeLong test revealed that the AUC of the SII for predicting MACEs in AMI patients was significantly greater than that of the NLR (P=0.01) or the PLR (P<0.001) (Table 2). These findings indicated that the SII had better predictive value for MACEs in AMI patients than did the NLR or PLR.
 |
Table 2 The Prediction Value of SII for MACEs |
Construction of a SII-Based Multivariable Model
The dataset was completely and randomly divided into a training set and a testing set. The results of the equilibrium test indicated that there was no significant difference between the data in the training set and the testing set (Supplementary Table 1). Predictors associated with MACEs were screened by bidirectional stepwise regression method, which revealed that age (OR=1.03, 95% CI: 1.01–1.05), Killip classification, BUN level (OR=1.13, 95% CI: 1.04–1.22), ECG-based diagnosis (OR=1.56, 95% CI: 1.00–2.45) and left ventricular ejection fraction (OR=0.96, 95% CI: 0.94–0.98) were associated with MACEs in AMI patients (Supplementary Table 2). The prediction model for MACES were constructed using logistic regression analysis, which based on SII (OR=4.35, 95% CI: 2.80–6.74) and other predictors, including age, Killip classification, BUN, ECG-based diagnosis and left ventricular ejection fraction. We have named the model as the “SII-based multivariable model”. The six abovementioned significant risk factors (SII, Killip classification, left ventricular ejection fraction, age, BUN, and ECG-based diagnosis) were further used to construct a nomogram (Figure 2). Each indicator corresponds to a score on the upper score line, and the total score is the sum of the scores of these six indicators. The total score is then projected onto the lowest scale, which indicates the probability of MACEs in Patients with AMI.
 |
Figure 2 The nomogram of SII-based multivariable model for MACEs. Abbreviation: SII, systemic immune inflammation index. |
Validation of the SII-based multivariable model
The AUC of SII-based multivariable model was 0.862 (95% CI=0.833–0.891) in the training cohort, 0.905 (95% CI=0.870–0.940) in the testing cohort, and 0.875 (95% CI=0.852–0.897) in all patients. The NPV was 0.849 (95% CI: 0.815–0.882) in the training cohort and 0.851 (95% CI: 0.793–0.898) in the testing cohort, and the accuracy was 0.807 (95% CI: 0.777–0.837) in the training cohort and 0.826 (95% CI: 0.777–0.868) in the testing cohort. Sensitivity analysis revealed that the AUC was 0.868 (95% CI=0.840–0.897) in the training cohort, 0.903 (95% CI=0.867–0.938) in the testing cohort and 0.879 (95% CI=0.856–0.901) in all patients after excluding patients who abandoned treatment at discharge because they had terminal conditions (Table 3).
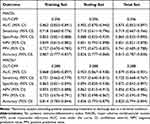 |
Table 3 The Predictive Values of SII-Based Multivariable Model for MACEs |
The calibration curves in the training set, the testing set and the total set showed that the SII-based multivariable model was well calibrated (Supplementary Figure 2). The decision curve analysis (DCA) plot for the nomogram model is shown in Figure 3. When the predicted risk of MACEs was 0.03–0.94 in the training cohort, 0.02–0.92 in the testing cohort, and 0.04–0.91 in the total cohort, treating patients with MACEs identified using the SII-based multivariable model had a more significant net benefit than treating patients treated with MACEs when no treatment was applied.
Comparison of Prediction Models
The AUC of the SII-based multivariable model was greater than that of the prediction model without the SII and the prediction model based on GRACE data (P<0.001). Sensitivity analysis also indicated that, compared with those of the prediction model without the SII and the prediction model based on GRACE data, the AUCs of SII-based multivariable model were greater (P<0.001) (Table 4). In addition, DCA showed that SII-based multivariable model had a wider clinical prediction range and greater net clinical benefit (Figure 3), suggesting that SII-based multivariable model in our study might have better predictive ability for MACEs in AMI patients and wider clinical application value.
 |
Table 4 Comparison of Prediction Models for MACEs |
Discussion
This is the first study to incorporate inflammatory markers into a nomogram to predict the in-hospital risks of MACEs in AMI patients. We performed a retrospective study involving 954 consecutive patients with AMI at Xiangdong Hospital of Hunan Normal University. First, we compared the in-hospital risk of MACEs according to the NLR, PLR, and SII and found that the SII had the greatest predictive value. We subsequently selected predictors for predicting the in-hospital risk for AMI patients, and SII-based multivariable model was established. Finally, we compared the nomogram with the traditional GRACE scoring system and demonstrated that our nomogram had better predictive value.
AMI is a severe coronary heart disease, and its essence is due to coronary atherosclerosis and thrombosis. The immune-inflammatory system plays a key role in all stages of vessel wall damage, lipid deposition, fibrous cap formation, atherosclerotic plaque rupture, and thrombosis in atherosclerotic cardiovascular disease.36–39 A substantial body of research has already demonstrated the relationship between inflammation and coronary heart disease,40,41 and inflammatory markers such as C-reactive protein (CRP) and the CRP to albumin ratio (CAR) can predict adverse outcomes in coronary heart disease.42,43
The white blood cells constituting the immune system, including lymphocytes, neutrophils, monocytes, and macrophages, play distinct roles in atherosclerosis. Platelets not only serve as primary participants in the initiation of atherosclerosis but also promote the formation of atherosclerosis and thrombosis through interactions with neutrophils, monocytes, and other white blood cells.44,45 These indicators can be obtained rapidly, efficiently, and at low cost through routine blood tests, the most commonly performed test in clinical practice. Studies have shown that indicators such as NLR, PLR and a recently introduced index, namely, the systemic immune inflammation index (SII), calculated as (neutrophil × platelet)/lymphocyte count, can effectively predict the prognosis of coronary heart disease through the combination of the abovementioned cell types.46,47 SII provides a relatively comprehensive reflection of the balance between host inflammation and immune status.48 Research indicates that the SII levels on admission can predict contrast-induced nephropathy(CIN) development after PCI in patients with CIN development after carotid artery angiography (CAAG) in patients with carotid artery stenosis (CAS), the development of atrial fibrillation following coronary artery bypass grafting, the severity of CAS in patients undergoing CAAG, NSTEMI.49–52 Patients with AMI often require urgent intervention, and rapid and efficient predictive index SII hold greater clinical significance.
In the present study, for the first time, we compared the in-hospital risk of MACEs according to the NLR, PLR, and SII and demonstrated that an SII≥970 was significantly associated with an increased risk of MACEs in patients with AMI (OR=4.87, 95% CI=2.80–6.74), The AUC of the SII for predicting MACEs was 0.684 (95% CI=0.654–0.714) and had better predictive value for MACEs than did the NLR (AUC=0.654, (95% CI=0.623–0.685)) and PLR (AUC=0.597, (95% CI=0.564–0.629)). Several existing studies on the predictive value of the SII for MACEs are mainly limited mainly to patients receiving PCI treatment,53,54 and the universality of the prognostic value of the SII for all AMI patients has not been confirmed. The population we studied included all patients with AMI, and thus the resulting model has wide application value.
No prior studies have developed a predictive model or risk scoring system to assess the impact of incorporating inflammatory markers on identifying in-hospital risk for MACEs in AMI patients. Our research addresses this gap by introducing a predictive model that integrates the SII with other predictors, including age, Killip classification, BUN level, ECG-based diagnosis, and left ventricular ejection fraction. This model demonstrated strong predictive performance for in-hospital MACEs in AMI patients. Importantly, we highlighted the significant contribution of the SII to the nomogram. The AUC of the nomogram, considering the SII and other predictors, was 0.862 (95% CI= 0.833–0.891). In contrast, excluding the SII resulted in a decreased AUC of 0.833 (95% CI=0.0.800–0.866), demonstrated the impact of the SII on enhancing the predictive value of the model.
Based on the rapidly acquired data of patients with STEMI, Yehong Liu et al constructed a nomogram risk prediction model for no-reflow after PCI that included Killip grade ≥2, D-dimer and fibrinogen levels, and SII/100 and further demonstrated that it could predict the in-hospital risk of MACEs well.55 Our study included a wider range of data available within 24 hours, including not only data from our hospital but also data from hospital transfers. This makes our study more akin to real-world research. Our research focused on the prediction of hospital risk and thus can help physicians make the right clinical decisions in terms of treatment strategy and hospital resource allocation.
To further demonstrate the value of the model we developed, we compared it with the GRACE score. The GRACE score was developed based on clinical, ECG, and biochemical data to improve prognostication and promote consistency in the investigation of patients with acute coronary syndrome (ACS).56 The European Society of Cardiology guidelines for the management of NSTEMI state that the GRACE score should be considered a tool for estimating the prognosis of these patients.57 Studies have shown that the GRACE score can accurately predict in-hospital and long-term mortality in ACS patients, even in the era of hs-cTnT.58 In the present study, the predictive value for MACEs in AMI patients of the model constructed based on the SII combined with other predictors for MACEs in AMI patients was better than that of the GRACE score. These results suggested that the SII-based multivariable model might be useful for identifying AMI patients who are at high risk of MACEs and offering timely treatments to prevent their occurrence.
Limitations
The present study was a single-center, retrospective study with a small sample size, which inevitably imparted a certain degree of selection bias. Although our nomogram model demonstrated good stability and clinical net benefit after internal bootstrap validation, external validation with a large sample size from multiple centers should be conducted to help promote its broad application. This study mainly evaluated the occurrence of in-hospital MACEs, and the predictive value of the SII for the long-term prognosis of AMI still needs to be verified by further multicenter studies. This study compared the predictive value of the SII for MACEs with that of the NLR and PLR. However, several traditional markers of inflammation, such as C-reactive protein, were not routinely tested and could not be compared. Additionally, the other important data such as syntax score were not analyzed, and these might be included in future studies to verify the findings of our study.
Conclusions
This study evaluated the prognostic value of the SII for the risk of in-hospital MACEs in AMI patients and further established a SII-based multivariable model combining the SII with other clinical indicators. Our study demonstrated that a high SII was associated with an increased risk of MACEs in AMI patients, and the SII-based multivariable model has good predictive value for MACEs in AMI patients. These findings might lead to the use of a quick and easy tool for identifying AMI patients at high risk of developing MACEs and offer timely interventions to those patients to improve their outcomes.
Funding
This work was supported by the Education Department of Hunan Province(20C1145), Health Commission of Hunan Province (D202303018299), and Guangzhou Key Research and Development Program (202206080014).
Disclosure
The authors have no conflicts of interest to disclose for this work.
References
1. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. New Engl J Med. 2010;362(23):2155–2165. doi:10.1056/NEJMoa0908610
2. Wu X, Reboll MR, Korf-Klingebiel M, Wollert KC. Angiogenesis after acute myocardial infarction. Cardiovascul Res. 2021;117(5):1257–1273. doi:10.1093/cvr/cvaa287
3. Zellweger MJ, Kaiser C, Jeger R, et al. Coronary artery disease progression late after successful stent implantation. J Am College Cardiol. 2012;59:793–799. doi:10.1016/j.jacc.2011.11.024
4. Jernberg T, Hasvold P, Henriksson M, Hjelm H, Thuresson M, Janzon M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015;36:1163–1170. doi:10.1093/eurheartj/ehu505
5. Li J, Li X, Wang Q, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2015;385:441–451. doi:10.1016/s0140-6736(14)60921-1
6. Murugiah K, Wang Y, Nuti SV, et al. Are non-ST-segment elevation myocardial infarctions missing in China? Eur Heart J Qual Care Clin Outcomes. 2017;3:319–327. doi:10.1093/ehjqcco/qcx025
7. Holmstrom L, Chugh SS. How to minimize in-hospital mortality from acute myocardial infarction: focus on primary prevention of ventricular fibrillation. Eur Heart J. 2022;43:4897–4898. doi:10.1093/eurheartj/ehac578
8. Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Int Med. 2003;163:2345–2353. doi:10.1001/archinte.163.19.2345
9. Castro-Dominguez Y, Dharmarajan K, McNamara RL. Predicting death after acute myocardial infarction. Trend Cardiovasc Med. 2018;28:102–109. doi:10.1016/j.tcm.2017.07.011
10. Sincer I, Mansiroglu AK, Aktas G, Gunes Y, Kocak MZ. Association between hemogram parameters and coronary collateral development in subjects with non-ST-elevation myocardial infarction. Rev Assoc Med Bras. 2020;66(2):160–165. doi:10.1590/1806-9282.66.2.160
11. Sincer I, Gunes Y, Mansiroglu AK, Cosgun M, Aktas G. Association of mean platelet volume and red blood cell distribution width with coronary collateral development in stable coronary artery disease. Adv Int Cardiol. 2018;14(3):263–269. doi:10.5114/aic.2018.78329
12. Sincer I, Gunes Y, Mansiroglu AK, Aktas G. Differential value of eosinophil count in acute coronary syndrome among elderly patients. Aging Male. 2020;23(5):958–961. doi:10.1080/13685538.2019.1643310
13. Aktas G. Association between the Prognostic Nutritional Index and Chronic Microvascular Complications in Patients with Type 2 Diabetes Mellitus. J Clin Med. 2023;12. doi: 10.3390/jcm12185952
14. Kocak MZ, Aktas G, Erkus E, Sincer I, Atak B, Duman T. Serum uric acid to HDL-cholesterol ratio is a strong predictor of metabolic syndrome in type 2 diabetes mellitus. Rev Assoc Med Bras. 2019;65(1):9–15. doi:10.1590/1806-9282.65.1.9
15. Kosekli MA, Kurtkulagii O, Kahveci G, et al. The association between serum uric acid to high density lipoprotein-cholesterol ratio and non-alcoholic fatty liver disease: the abund study. Rev Assoc Med Bras. 2021;67(4):549–554. doi:10.1590/1806-9282.20201005
16. Ong SB, Hernández-Reséndiz S, Crespo-Avilan GE, et al. Inflammation following acute myocardial infarction: multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol Ther. 2018;186:73–87. doi:10.1016/j.pharmthera.2018.01.001
17. Westman PC, Lipinski MJ, Luger D, et al. Inflammation as a driver of adverse left ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol. 2016;67(17):2050–2060. doi:10.1016/j.jacc.2016.01.073
18. Song L, Zhao X, Chen R, et al. Association of PCSK9 with inflammation and platelet activation markers and recurrent cardiovascular risks in STEMI patients undergoing primary PCI with or without diabetes. Cardiovasc Diabetol. 2022;21(1):80. doi:10.1186/s12933-022-01519-3
19. Burger PM, Dorresteijn JAN, Fiolet ATL, et al. Individual lifetime benefit from low-dose colchicine in patients with chronic coronary artery disease. Eur J Prev Cardiol. 2023;30(18):1950–1962. doi:10.1093/eurjpc/zwad221
20. Chen Y, Chen S, Han Y, Xu Q, Zhao X. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio are important indicators for predicting in-hospital death in elderly AMI patients. J Inflamm Res. 2023;16:2051–2061. doi:10.2147/jir.S411086
21. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. doi:10.1093/eurheartj/ehx393
22. Machado GP, Araujo GN, Carpes CK, et al. Comparison of neutrophil-to-lymphocyte ratio and mean platelet volume in the prediction of adverse events after primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. Atherosclerosis. 2018;274:212–217. doi:10.1016/j.atherosclerosis.2018.05.022
23. Zhang S, Diao J, Qi C, et al. Predictive value of neutrophil to lymphocyte ratio in patients with acute ST segment elevation myocardial infarction after percutaneous coronary intervention: a meta-analysis. BMC Cardiovasc Disord. 2018;18:75. doi:10.1186/s12872-018-0812-6
24. Dentali F, Nigro O, Squizzato A, et al. Impact of neutrophils to lymphocytes ratio on major clinical outcomes in patients with acute coronary syndromes: a systematic review and meta-analysis of the literature. Int J Cardiol. 2018;266:31–37. doi:10.1016/j.ijcard.2018.02.116
25. Li XT, Fang H, Li D, et al. Association of platelet to lymphocyte ratio with in-hospital major adverse cardiovascular events and the severity of coronary artery disease assessed by the Gensini score in patients with acute myocardial infarction. Chin Med J. 2020;133:415–423. doi:10.1097/cm9.0000000000000650
26. Fang L, Moore XL, Dart AM, Wang LM. Systemic inflammatory response following acute myocardial infarction. J Geriatr Cardiol. 2015;12:305–312. doi:10.11909/j.issn.1671-5411.2015.03.020
27. Dziedzic EA, Gąsior JS, Tuzimek A, et al. Investigation of the associations of novel inflammatory biomarkers-Systemic Inflammatory Index (SII) and Systemic Inflammatory Response Index (SIRI)-with the severity of coronary artery disease and acute coronary syndrome occurrence. Int J Mol Sci. 2022;23. doi:10.3390/ijms23179553
28. Taslamacioglu Duman T, Ozkul FN, Balci B. Could systemic inflammatory index predict diabetic kidney injury in type 2 diabetes mellitus? Diagnostics. 2023;13. doi:10.3390/diagnostics13122063
29. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138:e618–e651. doi:10.1161/cir.0000000000000617
30. Oki T, Ishii S, Takigami Y, et al. Re-worsening left ventricular ejection fraction after response to cardiac resynchronization therapy. J Cardiol. 2022;79:358–364. doi:10.1016/j.jjcc.2021.10.010
31. Armillotta M, Amicone S, Bergamaschi L, et al. Predictive value of Killip classification in MINOCA patients. Eur J Intern Med. 2023;117:57–65. doi:10.1016/j.ejim.2023.08.011
32. Luo E, Wang D, Yan G, et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention. Cardiovascul Diabetol. 2019;18:150. doi:10.1186/s12933-019-0957-3
33. Hicks KA, Tcheng JE, Bozkurt B, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). Circulation. 2015;132:302–361. doi:10.1161/cir.0000000000000156
34. Dharmarajan K, Li J, Li X, Lin Z, Krumholz HM, Jiang L. The China Patient-Centered Evaluative Assessment of Cardiac Events (China PEACE) retrospective study of acute myocardial infarction: study design. Circ Cardiovasc Qual Outcomes. 2013;6:732–740. doi:10.1161/circoutcomes.113.000441
35. Wu C, Huo X, Liu J, et al. Development and validation of a risk prediction model for in-hospital major cardiovascular events in patients hospitalised for acute myocardial infarction. BMJ open. 2021;11:e042506. doi:10.1136/bmjopen-2020-042506
36. Björkegren JLM, Lusis AJ. Atherosclerosis: recent developments. Cell. 2022;185:1630–1645. doi:10.1016/j.cell.2022.04.004
37. Libby P, Buring JE, Badimon L, et al. Atherosclerosis. Nat Rev Dis Primers. 2019;5:56. doi:10.1038/s41572-019-0106-z
38. Wolf D, Ley K. Immunity and inflammation in atherosclerosis. Circ Res. 2019;124:315–327. doi:10.1161/circresaha.118.313591
39. Chen Y, Li X, Lin X, et al. Complement C5a induces the generation of neutrophil extracellular traps by inhibiting mitochondrial STAT3 to promote the development of arterial thrombosis. Thromb J. 2022;20:24. doi:10.1186/s12959-022-00384-0
40. Harrington RA. Targeting inflammation in coronary artery disease. N Engl J Med. 2017;377:1197–1198. doi:10.1056/NEJMe1709904
41. Wirtz PH, von Känel R. Psychological stress, inflammation, and coronary heart disease. Curr Cardiol Rep. 2017;19:111. doi:10.1007/s11886-017-0919-x
42. Kelesoglu S, Yilmaz Y, Elcık D. Relationship between C-reactive protein to albumin ratio and coronary collateral circulation in patients with stable coronary artery disease. Angiology. 2021;72:829–835. doi:10.1177/00033197211004392
43. Aday AW, Bagheri M, Vaitinadin NS, Mosley JD, Wang TJ. Polygenic risk score in comparison with C-reactive protein for predicting incident coronary heart disease. Atherosclerosis. 2023;379:117194. doi:10.1016/j.atherosclerosis.2023.117194
44. Massberg S, Brand K, Grüner S, et al. A critical role of platelet adhesion in the initiation of atherosclerotic lesion formation. J Exp Med. 2002;196:887–896. doi:10.1084/jem.20012044
45. Pfeiler S, Stark K, Massberg S, Engelmann B. Propagation of thrombosis by neutrophils and extracellular nucleosome networks. Haematologica. 2017;102:206–213. doi:10.3324/haematol.2016.142471
46. Trakarnwijitr I, Li B, Adams H, Layland J, Garlick J, Wilson A. Age modulates the relationship between platelet-to-lymphocyte ratio and coronary artery disease. Int J Cardiol. 2017;248:349–354. doi:10.1016/j.ijcard.2017.06.127
47. Agarwal R, Aurora RG, Siswanto BB, Muliawan HS. The prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease. Coron Artery Dis. 2022;33:137–143. doi:10.1097/mca.0000000000001040
48. Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20:6212–6222. doi:10.1158/1078-0432.Ccr-14-0442
49. Yilmaz Y, Kelesoglu S, Kalay N. A novel predictor of contrast-induced nephropathy in patients with carotid artery disease; the systemic immune inflammation index. Angiology. 2022;73:781–787. doi:10.1177/00033197211061919
50. Kelesoglu S, Yilmaz Y, Elcik D, et al. Increased serum systemic immune-inflammation index is independently associated with severity of carotid artery stenosis. Angiology. 2023;74:790–797. doi:10.1177/00033197221144934
51. Kelesoglu S, Yilmaz Y, Elcık D, et al. Systemic immune inflammation index: a novel predictor of contrast-induced nephropathy in patients with Non-ST segment elevation myocardial infarction. Angiology. 2021;72:889–895. doi:10.1177/00033197211007738
52. Yilmaz Y, Kelesoglu S, Elcik D, Ozmen R, Kalay N. Predictive values of systemic immune-inflammation index in new-onset atrial fibrillation following coronary artery bypass grafting. Braz J Cardiovasc Surg. 2023;38:96–103. doi:10.21470/1678-9741-2021-0278
53. Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50:e13230. doi:10.1111/eci.13230
54. Huang J, Zhang Q, Wang R, et al. Systemic immune-inflammatory index predicts clinical outcomes for elderly patients with acute myocardial infarction receiving percutaneous coronary intervention. Med Sci Monit. 2019;25:9690–9701. doi:10.12659/msm.919802
55. Liu Y, Ye T, Chen K, et al. A nomogram risk prediction model for no-reflow after primary percutaneous coronary intervention based on rapidly accessible patient data among patients with ST-segment elevation myocardial infarction and its relationship with prognosis. Front Cardiovasc Med. 2022;9:966299. doi:10.3389/fcvm.2022.966299
56. Moledina SM, Kontopantelis E, Wijeysundera HC, et al. Ethnicity-dependent performance of the Global Registry of Acute Coronary Events risk score for prediction of non-ST-segment elevation myocardial infarction in-hospital mortality: nationwide cohort study. Eur Heart J. 2022;43:2289–2299. doi:10.1093/eurheartj/ehac052
57. Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–1367. doi:10.1093/eurheartj/ehaa575
58. Meune C, Drexler B, Haaf P, et al. The GRACE score’s performance in predicting in-hospital and 1-year outcome in the era of high-sensitivity cardiac troponin assays and B-type natriuretic peptide. Heart. 2011;97:1479–1483. doi:10.1136/hrt.2010.220988
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


