Back to Journals » Journal of Inflammation Research » Volume 16
A Nomogram Model for Post-Intubation Hypotension in Patients with Severe Pneumonia in the Emergency Department
Authors Pan P, Cheng T, Han T, Cao Y
Received 8 August 2023
Accepted for publication 17 October 2023
Published 13 November 2023 Volume 2023:16 Pages 5221—5233
DOI https://doi.org/10.2147/JIR.S430488
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Pan Pan, Tao Cheng, Tianyong Han, Yu Cao
Department of Emergency Medicine, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
Correspondence: Yu Cao, Email [email protected]
Background: Post-intubation hypotension (PIH) frequently occurs in the management of critically ill patients and is associated with prognosis. The study aimed to construct a prediction model for PIH events by analyzing risk factors in patients with severe pneumonia in the emergency department.
Methods: We retrospectively enrolled 572 patients with severe pneumonia diagnosed in the emergency department of West China Hospital of Sichuan University. Five hundred patients with severe pneumonia who underwent endotracheal intubation were included in the study. All patients were randomized according to 7:3 and divided into a training cohort (n=351) and a validation cohort (n=149). Risk factors for PIH were analyzed using Least Absolute Shrinkage and Selection Operator (LASSO) and multivariable logistic regression. Calibration curves, receiver operating characteristic (ROC) curve, and decision curve analysis were applied to assess the predictive model’s fitness, discrimination, and clinical utility.
Results: A total of 500 patients with severe pneumonia who underwent endotracheal intubation were enrolled in this study, and PIH occurred in 234 (46.8%) of these patients. Age, heart rate, systolic blood pressure, chronic obstructive pulmonary disease, acute physiology and chronic health evaluation II score, and induction agent use were identified as significant risk factors for the occurrence of PIH. Additionally, the body mass index was the opposite of the above. The area under the ROC curve (AUC) for the model was 0.856 (95% CI, 0.818– 0.894) in the training cohort and 0.849 (95% CI, 0.788– 0.910) in the validation cohort. The nomogram model was validated and demonstrated good calibration and high net clinical benefit. Finally, to facilitate application by clinicians, an online server has been set up which can be accessed free of charge via the website https://chinahospitals.shinyapps.io/DynNomapp/.
Conclusion: The nomogram is used for individualized prediction of patients with severe pneumonia prior to intubation and is simple to perform with high clinical value.
Keywords: post-intubation hypotension, severe pneumonia, prognosis, induction agent, nomogram
Introduction
Pneumonia continues to be the leading cause of hospitalization and death worldwide. In 2015, pneumonia was the eighth leading cause of death in the United States, the fourth leading cause of death worldwide, and the leading cause of death in low-income countries.1,2 Fever, cough, and increased sputum production are common symptoms of pneumonia.3 However, when it develops into severe pneumonia, it is often accompanied by hemodynamic instability and the need for mechanical ventilation, leading to increased mortality and intra- and extra-pulmonary complications.4 Endotracheal intubation is widely used in clinical practice as one of the effective means of improving ventilation and oxygen saturation. However, endotracheal intubation in emergency patients is often associated with a high rate of adverse events, including hypotension, cardiac arrest, and an increased risk of death.5,6
Hypotension, one of the most common complications after endotracheal intubation, occurs by mechanisms including blunting of catecholamines due to sedation inducers, decreased preload due to positive pressure ventilation, vasospasm, and myocardial depression.7–9 Post-intubation hypotension (PIH) is often associated with an adverse prognosis,10–12 with death occurring in one-third of cases.10 In a cohort study of 479 critically ill patients, PIH was observed in 46% of patients and was correlated with a significant increase in overall mortality, ICU length of stay, and duration of mechanical ventilation.11 In a systematic evaluation of emergency departments and ICUs, the incidence of PIH ranged from 0.5% to 44%, dramatically higher than elective intubation.13 In an attempt to investigate risk factors for PIH, it has been suggested that advanced age, chronic obstructive pulmonary disease (COPD), hemodynamic instability prior to tracheal intubation, acute respiratory failure, use of induction agents, and disease severity are all associated with the occurrence of PIH.8,9,14,15 However, no validated predictive model for PIH can be used to assess patients with severe pneumonia in the emergency department prior to endotracheal intubation. Early intervention in patients at high risk may reduce the incidence of PIH.
This study aimed to develop and validate a predictive model for PIH in patients with severe pneumonia in the emergency department. Firstly, clinical data were analyzed for risk factors for PIH in patients with severe pneumonia in the emergency department. Secondly, an effective and convenient predictive model for PIH in clinical practice was constructed. Finally, the predictive model for PIH was internally validated to assess its predictive effectiveness and clinical application.
Materials and Methods
Study Design and Setting
This project retrospectively enrolled 572 patients diagnosed with severe pneumonia in the emergency department of West China Hospital, Sichuan University, between January 2011 and December 2021, all of whom underwent emergency endotracheal intubation during treatment. Based on inclusion and exclusion criteria, 500 patients with severe pneumonia were eventually enrolled in this study. According to a 7:3 randomization, all patients were divided into a training cohort (n=351) and a validation cohort (n=149). The flow chart for developing and validating the prediction model is shown in Figure 1. The project followed the principles of the Declaration of Helsinki. The work was approved by the Ethics Committee of the West China Hospital of Sichuan University, which waived written informed consent (No. 2022–0493).
 |
Figure 1 The flow diagram of developing and validating the prediction model. |
Participants and Data Collection
In this study, all patients were enrolled from the case system of West China Hospital of Sichuan University. The patient’s primary diagnosis at the emergency department was severe pneumonia; all had emergency endotracheal intubation during their treatments in the hospital. Patients with the following conditions were excluded: age <18 years, systolic blood pressure <90 mmHg or mean arterial pressure <60 mmHg before endotracheal intubation, vasopressors or intravenous fluids (≥500mL) administered 30 minutes prior to intubation, hemodynamic instability or ongoing cardiopulmonary resuscitation, death within 24 h of admission.
The following clinical data were collected within 24 hours of patient admission: gender, age, body mass index (BMI), physiological data on admission (heart rates, respiratory rate, blood pressure, oxygen saturation), pre-admission comorbidities, acute physiology and chronic health evaluation (APACHE) II score, Glasgow coma scale (GCS), use of induction agent, laboratory tests (white blood cell count, neutrophils, albumin, serum creatinine, lactate), and incidence of PIH, etc. If a variable reported more than one value in the first 24 hours, the worst was selected for analysis.
Measurement and Definition
The diagnostic criteria for severe pneumonia follow the 2007 Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) consensus guidelines on managing community-acquired pneumonia in adults.16 Diagnostic criteria for PIH:10,11,14 any of the following occurring within 15 minutes of endotracheal intubation: (a) systolic blood pressure (SBP) <90 mmHg; (b) 20% reduction in SBP from baseline levels; (c) mean arterial pressure (MAP) <60 mmHg; (d) need for an increased infusion dose of vasopressors (push or infusion); (e) requires an infusion volume of ≥ 30 mL/kg. Baseline SBP was defined as the average of all SBP values recorded 30 minutes prior to endotracheal intubation. Pre-tracheal hypotension was defined as any SBP <90 mmHg or diastolic blood pressure (DBP) <60 mmHg in the 30 minutes prior to endotracheal intubation.
Model Development and Validation
Predictive models were developed by analyzing risk factors for PIH through a training cohort. The effectiveness and application value of the predictive model was assessed by a validation cohort (retrospective data).
Clinical Outcomes
The primary outcome was the incidence of PIH in patients with severe pneumonia. Secondary outcomes were the length of hospital stay, ICU stay, in-hospital mortality, and 28-day mortality in patients.
Statistical Analysis
In this study, the primary characteristics of all study populations were analyzed by descriptive statistics. We used the Kolmogorov–Smirnov method to test for the normality of continuous variables. Means and standard deviations were used to describe normally distributed continuous variables, while non-normally distributed continuous variables were expressed as median and interquartile range. For categorical variables, frequencies and percentages are the best way to represent them. The least absolute shrinkage and selection operator (LASSO) was first introduced by Robert Tibshirani in 1996.17 LAASO not only fits generalized linear models but is also capable of variable selection and regularization. In our study, risk factors were selected by the LASSO binary logistic regression model, and risk factors were selected when their coefficients were non-zero. Multivariable logistic regression was performed to analyze risk factors for PIH and variables with significant correlations were selected to develop a nomogram.
The accuracy of the nomogram model was assessed by validation. The area under the ROC curve (AUC) was employed to assess the model’s discriminatory power, comparing the AUC in the training and validation cohorts. Assessment of model fitness was accomplished using calibration plots, which analyzed how close the actual results of each nomogram model were to the predicted results.18 Decision curve analysis (DCA) showed the standardized net benefit of the prediction model at different risk thresholds and was used to assess the clinical utility of the model.19 The clinical impact curves revealed the number of high-risk individuals and true-positive patients at different thresholds. Additionally, Kaplan-Meier curves were used in the survival analysis to analyze the prognosis of patients with severe pneumonia.
Statistical analysis was conducted with SPSS (IBM SPSS Statistics 22.0, SPSS Inc., Chicago, IL) and R language (version 4.1.3, www.R-project.org/). The R packages used in our study were displayed in Supplementary Table 1. All statistical tests were two-sided, and statistical significance was set at 0.05.
Results
Demographic and Baseline Characteristics
In this study, we enrolled 572 emergency patients with severe pneumonia. Based on inclusion and exclusion criteria, 500 patients with severe pneumonia ultimately participated in the construction of the PIH model [319 (63.8%) males; mean (SD) age, 64.73 (17.32) years]. A total of 234 (46.8%) patients in the study experienced post-intubation hypotensive events, 162 (46.2%) in the training cohort and 72 (48.3%) in the validation cohort. There were no significant differences between the training and validation cohorts for any variables (Supplementary Table 2). Moreover, we compared risk factors for PIH in the training cohort. Age, BMI, heart rate, respiratory rate, oxygen saturation, blood pressure, history of COPD, APACHE II score, GCS, use of induction agents, hemoglobin, and albumin were associated with PIH in patients with severe pneumonia. However, gender did not show significant differences (Table 1). In addition, patients in the PIH group had significantly higher rates of propofol [147 (62.8) vs 126 (47.4), p=0.001] and remifentanil [32 (13.7) vs 19 (7.1), p=0.016] than those in the non-PIH group (Supplementary Table 3).
 |
Table 1 Comparison of Clinical Characteristics of Patients with PIH and Non-PIH in the Training Cohort |
The Construction of Nomogram Model Based on Risk Factors
We analyzed risk variables in the training cohort of 351 patients with severe pneumonia (162 with PIH) by the LASSO binary logistic regression model. Combining clinical experience and LASSO regression results, we screened for seven predictors with non-zero coefficients (Figure 2A and B, Supplementary Table 4). After multivariable logistic regression analysis, age (OR: 1.022, 1.004–1.040), BMI (OR: 0.680, 0.585–0.790), APACHE II score (OR: 1.118, 1.056–1.185), heart rate (OR: 1.014, 1.004–1.024), systolic blood pressure (OR: 1.029, 1.018–1.041), induction agent use (OR: 3.579, 2.216–4.937), and history of COPD (OR: 2.341, 1.257–4.361) were the primary risk factors for PIH (Figure 3). We weighted the regression coefficients of the risk factors incorporated in the regression model and constructed a risk score formula to predict PIH. Risk score = −2.004 + 0.021 (age) - 0.386 (BMI) + 0.112 (APACHE II score) + 0.014 (heart rate) + 1.275 (if induction agent is used) + 0.029 (systolic blood pressure) + 0.851 (if COPD is positive). Predicted risk =1/(1 + e−risk score) (Supplementary Table 5). We developed a nomogram model for predicting PIH based on the above risk factors and regression coefficients. A real case is shown in Figure 4.
 |
Figure 3 Multivariable logistic regression demonstrating the association of variables with PIH. |
Validation and Evaluation of the Nomogram
In order to assess the fit of the prediction model in the study, we performed an internal validation of the nomogram model. We used calibration curves to assess the agreement between the predicted and observed results in the validation process. The nomogram model’s predictions and observations fit well in the training cohort (Hosmer-Lemeshow χ2 = 5.335, p = 0.721) (Figure 5A). Furthermore, we also assessed the fit between predicted and observed outcomes in the validation cohort, and the study also showed a good fit (Hosmer-Lemeshow χ2 = 8.706, p = 0.368) (Figure 5B). To assess the predictive performance of the nomogram model, we analyzed the results using the area under the ROC curve. We found no significant difference in AUC for the training cohort [AUC:0.856, 95% CI (0.818–0.894)] compared to the validation cohort [AUC:0.849, 95% CI (0.788–0.910)] (p = 0.841) (Figure 5C and Supplementary Table 6).
Clinical Usefulness
Decision curve analysis (DCA) is significantly superior for assessing the value of predictive models for clinical application and can quantify the net clinical benefit at different thresholds. In this study, we found that both the training and validation cohorts demonstrated higher net clinical benefit in the nomogram model compared to the thresholds of “no intervention” and “all intervention” (Figure 6A). Additionally, the clinical impact curves showed that patients at risk of PIH converged with those who experienced a PIH event within this risk threshold (Figure 6B and C). These results suggest that the PIH prediction model has good clinical application.
Outcomes
Among the 500 patients with severe pneumonia, the mean number of days in the hospital was 8.00 (3.00–19.00), the in-hospital mortality rate was 51.8%, and the 28-day mortality rate was 48.6%. PIH events occurred in 234 (46.8%) of all patients. The length of hospital stay, length of ICU stay, 28-day mortality, and in-hospital mortality were all significantly higher in patients with PIH than in those with non-PIH (Table 2). In addition, we performed a survival analysis of 28-day mortality in patients with severe pneumonia. The results showed that the early period (within one week) in which a PIH event occurred did not significantly impact patient prognosis. When the PIH event occurred one week later, mortality in patients with PIH increased progressively with time (Figures 7 and 8).
 |
Table 2 Outcomes in Patients with or Without Post-Intubation Hypotension |
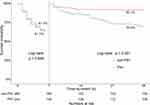 |
Figure 8 Comparison of 7-day and 28-day mortality in tracheally intubated patients. |
Discussion
In this study, we analyzed clinical data from 500 patients with severe pneumonia to develop and validate a nomogram model of PIH. Our results, analyzed by LASSO and multivariable logistic regression, showed that age, BMI, APACHE II score, heart rate, systolic blood pressure, induction agent use, and history of COPD were the main predictors of PIH. We developed a nomogram prediction model based on these predictors. After evaluating the model’s fit, clinical utility, and predictive performance, the nomogram showed good calibration, discrimination, and clinical utility.
In the emergency department, endotracheal intubation is one of the most effective ways to improve ventilation, increase oxygen saturation and save the lives of critically ill patients.20 However, PIH is one of the most common complications that affect emergency physicians’ management of critically ill patients.6,12,21–23 More scholars have tried to explore the risk factors for PIH events and to develop early predictive models for them. In a retrospective study that included 147 critically ill patients, pre-intubation blood pressure, use of induction agents and intubation complications were the main risk factors for PIH.14 In critically ill patients with COVID-19, an albumin level <2.92 g/dL was strongly associated with the occurrence of PIH.24 In an observational study that included 4866 trauma patients, age, heart rate, and SBP were the main variables in a PIH scoring system. The scoring system had an AUC of 0.820 and good predictive performance, but it failed to visualize the system and was not convenient for clinicians to apply.25 In addition, Zhou et al26 developed a prediction model for PIH using machine learning methods and showed good predictive performance with an AUC of 0.865 in the training cohort. However, the prediction model by Zhou et al lacked analysis of inducer use,23,27 which may have biased the prediction results. In this study, we combined clinical practice and multivariable logistic regression results to develop a PIH prediction model for patients with severe pneumonia. Risk variables such as pre-intubation vital signs, disease severity, and pre-intubation medication were incorporated into the model. The nomogram model had an AUC of 0.856, suggesting good predictive performance. Furthermore, we visualized the model, which has good application in clinical practice.
COPD is a common respiratory disease that plays an important role in developing PIH.28 When patients with severe pneumonia are being treated, respiratory distress, reduced oxygen saturation, anxiety, agitation or other causes can lead to functional disturbances in the body. For example, increased sympathetic tone, adrenaline secretion, and preload and afterload pressures on the heart,29 lead to normal or elevated blood pressure in patients. In addition, the presence of COPD may further exacerbate the symptoms of hypoxia and hypercapnia in the organism.30 When patients’ respiratory distress and hypoxia are improved by endotracheal intubation, the patient’s sympathetic tone will be significantly reduced, the preload and afterload of the heart will change, and those patients with normal SBP prior to intubation may experience PIH events.14,25,31 Therefore, a normal SBP before intubation may be an artifact and needs to be carefully screened by clinicians. In this study, COPD was the main risk factor for PIH. COPD increased the risk of PIH events by 2.341 times relative to patients without COPD. Moreover, SBP serves as an important indicator of vital signs. The finding in this study that pre-intubation SBP was higher in the group of patients who developed hypotension is inconsistent with the findings of Heffner et al.8 We believe that the inclusion of different study populations will influence the final results. In the Heffner AC study, all emergency department patients were included. In contrast, only patients with severe pneumonia in the emergency department were analyzed in this study, and most patients with severe pneumonia could significantly improve ventilation and oxygen saturation with endotracheal intubation. Thus, this may be one of the reasons for the high pre-intubation SBP in this study. In clinical practice, we should pay more attention to patients who are preintubation agitated and have COPD.
Besides a history of COPD and SBP, the patient’s age, BMI and APACHE II score should also be assessed before endotracheal intubation. Several studies have demonstrated that age as a main risk factor for PIH. In this study, the mean age of the patients in the PIH group was 68 years, which is consistent with the age of the patients who experienced hypotensive events in the Smischney NJ team’s study.14 Patients of advanced age are more likely to have a PIH event related to reduced physiological reserve or co-morbidities.25 Regarding BMI, it has been suggested that patients with a low BMI tend to have poor nutritional status and are more likely to develop PIH.32 In this study, patients with PIH had a lower BMI than the non-PIH group. Thus, the incidence of PIH is significantly higher in older and lower weight patients and should be of greater concern to clinicians. Additionally, the APACHE II score, an important variable in assessing the severity of a patient’s condition,33 was also strongly associated with PIH events. In this study, APACHE II score was dramatically higher in the PIH group than in the non-PIH group [15.00 (12.00–18.00) vs 12.00 (9.00–17.00), p<0.001]. The results indicated that critically ill patients often have multiple organ dysfunction and were weaker than the normal population in regulating all body functions.
Inducers, as one of the drugs often used prior to intubation, are chosen with great care in terms of type. The use of induction agents during endotracheal intubation is often associated with the incidence of PIH.27,34 Inducers can contribute to the development of PIH by inhibiting the action of catecholamines in the body35 and suppressing adrenocortical function.36,37 In a retrospective study that included 469 critically ill patients in the emergency department, induction agents increased the incidence of PIH events.27 The association of induction agents with PIH was also confirmed in the study by April et al.38 In this study, we found that the use of induction agents prior to intubation increased the risk of hypotensive events by 3.579-fold, consistent with the findings of the investigators mentioned above. In addition, patients in the PIH group had significantly higher rates of propofol [147 (62.8) vs 126 (47.4), p=0.001] and remifentanil [32 (13.7) vs 19 (7.1), p=0.016] than those in the non-PIH group. These results suggested that propofol and remifentanil may have contributed to PIH events. However, some investigators have found that ketamine, a safer induction agent with sympathomimetic properties that indirectly releases catecholamines39 and reduces the risk of hypotension, may be used in patients who are hemodynamically unstable in the emergency department.40 Other studies have shown that etomidate does not inhibit sympathetic tone or myocardial function and produces minimal hemodynamic changes during endotracheal intubation.41,42 Therefore, the choice of induction agent still needs further confirmation in prospective clinical studies with large samples.
Although a predictive model for PIH in patients with severe pneumonia was developed in this study, there are still some limitations. Firstly, this research is a non-randomized retrospective clinical study, and there may have been selection bias in the inclusion of patients. Secondly, induction agents are the main risk factors for PIH, and different induction agents may produce different hemodynamic effects. Therefore, the characteristics of different inducers need to be considered when applying predictive models. In addition, different inducers may be applied in different regions or hospitals. Only three inducers were applied in this study, resulting in the possibility that accurate prediction results may not be obtained when applying other inducers and cannot be generalized to a larger population. Finally, this study was internally validated using only retrospective data and lacked results validated in prospective trials. Our team will conduct a multicenter prospective validation in a subsequent study to further assess the validity and clinical application value of the prediction model.
Conclusion
In this study, we developed and validated a predictive model for the occurrence of PIH in patients with severe pneumonia. Although this nomogram model allows individualized prediction of post-intubation hypotensive events, more prospective trials are needed for validation.
Data Sharing Statement
The datasets for this manuscript will be made available upon request, further inquiries can be directed to the corresponding author Yu Cao, [email protected].
Ethics Approval and Informed Consent
All procedures performed in studies involving human participants were performed in accordance with the Declaration of Helsinki and approved by the ethics committee of the West China Hospital of Sichuan University (No.2022-0493). The ethics committee of the West China Hospital of Sichuan University waived the need for written informed consent provided by participants due to the retrospective nature of the study. All patient data were analyzed anonymously, and no additional informed consent was required.
Acknowledgments
We sincerely thank the Information Management Department of West China Hospital of Sichuan University for their support in the data extraction process.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by a grant from the Peking Union Medical Foundation - Rui E (Rui Yi) Special Fund for Emergency Medicine Research (No. 22222012003).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Torres A, Cilloniz C, Niederman MS, et al. Pneumonia. Nat Rev Dis Primers. 2021;7(1):25. doi:10.1038/s41572-021-00259-0
2. Nair GB, Niederman MS. Updates on community acquired pneumonia management in the ICU. Pharmacol Ther. 2021;217:107663. doi:10.1016/j.pharmthera.2020.107663
3. Lanks CW, Musani AI, Hsia DW. Community-acquired pneumonia and hospital-acquired pneumonia. Med Clin North Am. 2019;103(3):487–501. doi:10.1016/j.mcna.2018.12.008
4. Cilloniz C, Torres A, Niederman MS. Management of pneumonia in critically ill patients. BMJ. 2021;375:e065871. doi:10.1136/bmj-2021-065871
5. Mort TC, Waberski BH, Clive J. Extending the preoxygenation period from 4 to 8 mins in critically ill patients undergoing emergency intubation. Crit Care Med. 2009;37(1):68–71. doi:10.1097/CCM.0b013e318192845e
6. Nolan JP, Kelly FE. Airway challenges in critical care. Anaesthesia. 2011;66(Suppl 2):81–92. doi:10.1111/j.1365-2044.2011.06937.x
7. Heffner AC, Swords DS, Neale MN, Jones AE. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation. 2013;84(11):1500–1504. doi:10.1016/j.resuscitation.2013.07.022
8. Heffner AC, Swords DS, Nussbaum ML, Kline JA, Jones AE. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care. 2012;27(6):587–593. doi:10.1016/j.jcrc.2012.04.022
9. Green RS, Edwards J, Sabri E, Fergusson D. Evaluation of the incidence, risk factors, and impact on patient outcomes of postintubation hemodynamic instability. CJEM. 2012;14(2):74–82. doi:10.2310/8000.2012.110548
10. Green RS, Butler MB, Erdogan M. Increased mortality in trauma patients who develop postintubation hypotension. J Trauma Acute Care Surg. 2017;83(4):569–574. doi:10.1097/TA.0000000000001561
11. Green RS, Turgeon AF, Mcintyre LA, et al. Postintubation hypotension in intensive care unit patients: a multicenter cohort study. J Crit Care. 2015;30(5):1055–1060. doi:10.1016/j.jcrc.2015.06.007
12. Perbet S, De Jong A, Delmas J, et al. Incidence of and risk factors for severe cardiovascular collapse after endotracheal intubation in the ICU: a multicenter observational study. Critical Care. 2015;19(1):257. doi:10.1186/s13054-015-0975-9
13. Green R, Hutton B, Lorette J, Bleskie D, Mclntyre L, Fergusson D. Incidence of postintubation hemodynamic instability associated with emergent intubations performed outside the operating room: a systematic review. CJEM. 2014;16(1):69–79. doi:10.2310/8000.2013.131004
14. Smischney NJ, Demirci O, Diedrich DA, et al. Incidence of and risk factors for post-intubation hypotension in the critically Ill. Med Sci Monit. 2016;22:346–355. doi:10.12659/msm.895919
15. Green RS, Butler MB. Postintubation hypotension in general anesthesia: a retrospective analysis. J Intensive Care Med. 2016;31(10):667–675. doi:10.1177/0885066615597198
16. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious diseases society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–72. doi:10.1086/511159
17. Tibshirani R. The lasso method for variable selection in the Cox model. Stat Med. 1997;16:385–395. doi:10.1002/(sici)1097-0258(19970228)16:
18. Coutant C, Olivier C, Lambaudie E, et al. Comparison of models to predict nonsentinel lymph node status in breast cancer patients with metastatic sentinel lymph nodes: a prospective multicenter study. J Clin Oncol. 2009;27(17):2800–2808. doi:10.1200/JCO.2008.19.7418
19. Fitzgerald M, Saville BR, Lewis RJ. Decision curve analysis. JAMA. 2015;313:409–410. doi:10.1001/jama.2015.37
20. Mort TC. Complications of emergency tracheal intubation: immediate airway-related consequences: part II. J Intensive Care Med. 2007;22(4):208–215. doi:10.1177/0885066607301359
21. Smischney NJ, Seisa MO, Heise KJ, et al. Practice of intubation of the critically ill at mayo clinic. J Intensive Care Med. 2019;34(3):204–211. doi:10.1177/0885066617691495
22. Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34(9):2355–2361. doi:10.1097/01.Ccm.0000233879.58720.87
23. Jaber S, Jung B, Corne P, et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive Care Med. 2010;36(2):248–255. doi:10.1007/s00134-009-1717-8
24. Ergun B, Ergan B, Yakar MN, et al. Incidence of and risk factors for postintubation hypotension in critically ill patients with COVID-19. Rev Bras Ter Intensiva. 2022;34(1):131–140. doi:10.5935/0103-507X.20220007-pt
25. Elmer J, Brown F, Martin-Gill C, Guyette FX. Prevalence and predictors of post-intubation hypotension in prehospital trauma care. Prehosp Emerg Care. 2020;24(4):461–469. doi:10.1080/10903127.2019.1670300
26. Zhou CM, Xue Q, Liu P, et al. Construction of a predictive model of post-intubation hypotension in critically ill patients using multiple machine learning classifiers. J Clin Anesth. 2021;72:110279. doi:10.1016/j.jclinane.2021.110279
27. Foster M, Self M, Gelber A, et al. Ketamine is not associated with more post-intubation hypotension than etomidate in patients undergoing endotracheal intubation. Am J Emerg Med. 2022;61:131–136. doi:10.1016/j.ajem.2022.08.054
28. Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399(10342):2227–2242. doi:10.1016/S0140-6736(22
29. Ziegler MG, Milic M. Sympathetic nerves and hypertension in stress, sleep apnea, and caregiving. Curr Opin Nephrol Hypertens. 2017;26(1):26–30. doi:10.1097/MNH.0000000000000288
30. Abdo WF, Heunks LM. Oxygen-induced hypercapnia in COPD: myths and facts. Critical Care. 2012;16:323. doi:10.1186/cc11475
31. Smischney NJ, Kashyap R, Khanna AK, et al. Risk factors for and prediction of post-intubation hypotension in critically ill adults: a multicenter prospective cohort study. PLoS One. 2020;15(8):e0233852. doi:10.1371/journal.pone.0233852
32. Lin CC, Chen KF, Shih CP, Seak CJ, Hsu KH. The prognostic factors of hypotension after rapid sequence intubation. Am J Emerg Med. 2008;26(8):845–851. doi:10.1016/j.ajem.2007.11.027
33. Mirsaeidi M, Peyrani P, Ramirez JA. Predicting mortality in patients with ventilator-associated pneumonia: the APACHE II score versus the new IBMP-10 score. Clin Infect Dis. 2009;49(1):72–77. doi:10.1086/599349
34. Freeman J, Alkhouri H, Knipp R, Fogg T, Gillett M. Mapping haemodynamic changes with rapid sequence induction agents in the emergency department. Emerg Med Austral. 2022;34(2):237–243. doi:10.1111/1742-6723.13867
35. Zed PJ, Abu-Laban RB, Harrison DW. Intubating conditions and hemodynamic effects of etomidate for rapid sequence intubation in the emergency department: an observational cohort study. Acad Emerg Med. 2006;13(4):378–383. doi:10.1197/j.aem.2005.11.076
36. Gu WJ, Wang F, Tang L, Liu JC. Single-dose etomidate does not increase mortality in patients with sepsis: a systematic review and meta-analysis of randomized controlled trials and observational studies. Chest. 2015;147(2):335–346. doi:10.1378/chest.14-1012
37. Cuthbertson BH, Sprung CL, Annane D, et al. The effects of etomidate on adrenal responsiveness and mortality in patients with septic shock. Intensive Care Med. 2009;35(11):1868–1876. doi:10.1007/s00134-009-1603-4
38. April MD, Arana A, Schauer SG, et al. Ketamine versus etomidate and peri-intubation hypotension: a national emergency airway registry study. Acad Emerg Med. 2020;27(11):1106–1115. doi:10.1111/acem.14063
39. Panzer O, Moitra V, Sladen RN. Pharmacology of sedative-analgesic agents: dexmedetomidine, remifentanil, ketamine, volatile anesthetics, and the role of peripheral mu antagonists. Crit Care Clin. 2009;25(3):451–469. doi:10.1016/j.ccc.2009.04.004
40. Ishimaru T, Goto T, Takahashi J, et al. Association of ketamine use with lower risks of post-intubation hypotension in hemodynamically-unstable patients in the emergency department. Sci Rep. 2019;9(1):17230. doi:10.1038/s41598-019-53360-6
41. Bruder EA, Ball IM, Ridi S, Pickett W, Hohl C. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Cochrane Database Syst Rev. 2015;1(1):CD010225. doi:10.1002/14651858.CD010225.pub2
42. Forman SA, Warner DS. Clinical and molecular pharmacology of etomidate. Anesthesiology. 2011;114(3):695–707. doi:10.1097/ALN.0b013e3181ff72b5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





