Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
A Cross-Sectional Evaluation of Knowledge About Breast Cancer and Perceived Barriers to the Uptake of Mammogram Screening Among Northern Saudi Women: A Population-Based Study
Authors Alanazi MF, Thirunavukkarasu A, Alrowily M , Alaqel N, Alaqel A, Alruwaili M , Alazmi NNM, Alhassan O, Aljarallah MFM, Altaymani AM
Received 12 April 2023
Accepted for publication 22 June 2023
Published 10 July 2023 Volume 2023:15 Pages 451—460
DOI https://doi.org/10.2147/BCTT.S414635
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Muhannad Faleh Alanazi,1 Ashokkumar Thirunavukkarasu,2 Maily Alrowily,3 Nouf Alaqel,4 Abdulelah Alaqel,5 Mutlaq Alruwaili,5 Nouf Nashmi M Alazmi,5 Osamah Alhassan,5 Mona Fahad M Aljarallah,5 Afrah Mohaimeed Altaymani5
1Division of Radiology, Department of Internal Medicine, College of Medicine, Jouf University, Sakaka, Saudi Arabia; 2Department of Community and Family Medicine, College of Medicine, Jouf University, Sakaka, Saudi Arabia; 3Aljouf Health Cluster, Ministry of Health, Sakaka, Aljouf, Saudi Arabia; 4Department of Diagnostic Radiology, Prince Mutab Bin Abdulaziz Hospital, Sakaka, Aljouf, Saudi Arabia; 5College of Medicine, Jouf University, Sakaka, Aljouf, Saudi Arabia
Correspondence: Muhannad Faleh Alanazi, Division of Radiology, Department of Internal Medicine, College of Medicine, Jouf University, Sakaka, 72388, Saudi Arabia, Tel +966555 393 871, Email [email protected]
Background: Mammogram screening (MS) is the gold-standard method for early detection of breast cancer (BC), and its use has been proven to minimize BC-related deaths and reduce treatment costs. However, recent epidemiological surveys have reported that rates of mammogram uptake by the Saudi female population are low. Here, we assessed the knowledge of BC and perceived barriers to MS uptake among pre-eligible northern Saudi women.
Participants and Methods: We administered a standard and validated Arabic questionnaire to 400 women aged 40– 69 years. SPSS version 21.0 (IBM Corporation, Armonk, NY, USA) was used for data analysis. We applied logistic regression analysis to find the factors associated with participants’ knowledge of BC and MS. Spearman correlation test was applied to find the correlation between knowledge and barrier scores.
Results: The study participants reported that smoking habits (61.3%) and unhealthy food habits (57.8%) were the most common risk factors for BC. Of the studied participants, 56.3% had low or medium degrees of knowledge about BC risk factors and MS. The degree of knowledge was significantly associated with education level (adjusted odds ratio [aOR], 2.35; 95% confidence interval [CI]. = 1.61– 3.13; P = 0.008) and a family history of BC (aOR, 3.66; 95% CI, 1.94– 5.49; P < 0.001). Fear of a BC diagnosis (50.8%) and concerns regarding test procedures were the most common barriers to MS uptake. We also found a negative correlation between participants’ knowledge and perceived barriers to MS (rho = − 0.389, P < 0.001).
Conclusion: We recommend that concerned authorities offer women multiple health education sessions covering BC risk factors and the necessity for pre-eligible women to undergo MS spaced at regular intervals at different facilities. Furthermore, a multicentric mixed-methods survey is warranted to find the qualitative aspects of barriers to MS.
Keywords: breast cancer, screening, risk factors, mammogram, knowledge
Introduction
Breast cancer (BC) is the most frequently identified cancer among women globally, especially in developed countries, according to the World Health Organization.1–3 Similarly, in the Kingdom of Saudi Arabia (KSA), BC is now the most common cancer diagnosed in the female population due to changes in lifestyle and other factors, such as older age, a family history of BC, obesity, and low physical activity levels.4 Understanding risk factors associated with this disease and developing strategies to minimize them can help to reduce associated morbidity and mortality rates. In addition to targeting risk factors, making an early diagnosis is also vital for improving survival rates (to ≥90%) among this group, which may not be possible after a late diagnosis.5,6 The global initiative for BC, in addition to screening, advocates for good health by educating women and health care workers about the risk factors and the signs and symptoms of BC. Knowing this information is essential for early referral, screening, and the timely detection and management of BC.7
The American College of Radiology and several other organizations worldwide have suggested the use of mammograms for BC screening. Currently, mammography is the gold-standard method for early detection and screening of BC, and its use has been proven to minimize BC-related deaths and reduce treatment costs.8,9 In the KSA, mammogram screenings (MSs) are free for all KSA citizens. The Ministry of Health (MOH), KSA recommends MS for women ≥40 years without a family history of BC or beginning at 10 years younger than the age of BC onset in their family member for those women with a family history of BC. According to the MOH, KSA policy, all women aged 40–50 years must undergo MS every 2 years, while females those aged 51–69 years must undergo MS every 1–2 years.10 However, recent epidemiological surveys have reported that MS uptake by the female population is low. As with any other public health program, the involvement of all stakeholders, especially beneficiary women, is critical for successful implementation of an MS screening program. In 2020, Abdel-Salam et al revealed that the female Saudi population encounters several problems and barriers to MS uptake. They also reported several economic and personal barriers among Saudi women that hindered them from undergoing MS. Notably, their study concluded that this trend could be due to a number of factors, such as lack of information about mammograms, difficulty in obtaining leave from work, and long waiting times for medical appointments. Perceived fears related to radiation exposure, the discovery of BC, and errors in diagnosis and cancer treatment were also reported as barriers to MS uptake.11 Another study performed in the KSA also determined that, despite the availability of free MS sessions for eligible Saudi citizens, the rate of MS among beneficiaries is not optimal.12 Cultural norms about interactions with men apart from husbands and beliefs about modesty and privacy of the body have been identified as additional barriers limiting MS uptake by women at high risk for BC.13 A systematic review published by Wang et al based on global data concluded that, even though the level of awareness about the high mortality rates associated with BC is generally good, the degree of knowledge about BC risk factors and MS is very low. Furthermore, they reported that the understanding of BC risk factors among Asian and African women is much lower than that among women in Western cultures.14 A population study conducted in New Delhi, India, by Dey et al determined that only about 50% of surveyed women were aware of various aspects of BC. In their study, Dey et al linked women’s awareness to their education level and socioeconomic status. Also, they reported that alarmingly low levels (7%) of women had undergone a prior MS.
In Malaysia, Abdullah et al found that, despite high-risk factors among Malaysian women, only half of them had undergone MS. Older women and those recommended for MS by physicians had higher uptake of MS.15 An understanding of BC risk factors and the barriers to MS uptake is essential for developing targeted strategies to reduce morbidity and mortality rates among high-risk women in this region. By increasing awareness of the importance of mammograms and providing access to mammography equipment, Saudi women can have the best chance of BC detection in the earliest stages. Continuous evaluation of high-risk population knowledge and barriers to MS uptake is critical to help the MOH and other relevant authorities design appropriate BC education plans. However, we lack relevant data from the northern region of KSA. Given the importance of region-specific data, the current study aimed to assess BC and MS knowledge as well as perceived barriers to MS uptake by the Saudi female population in northern KSA. Furthermore, we aimed to identify the predictors for knowledge and correlation among the variables.
Materials and Methods
Study Design and Setting
This population-based cross-sectional study was conducted among a Saudi female population group aged 40–69 years from Aljouf Province between September 2022 and February 2023. This province is one of the 13 provinces of KSA and is situated in the northern part of the country. We included only Saudi women aged 40–69 years who could read and write in Arabic and who agreed to participate in the survey. We excluded expatriates and Saudi nationals from other provinces.
Sampling Description
The sample size was calculated using the Cochran’s sample-size estimation formula (n= z2 pq/e2).16 To calculate the minimum required sample size, the authors used the following criteria after reviewing the available literature: an expected frequency (p) of 50%, a confidence level of 95% (z = 1.96), and a margin of error (e) of 5%. Using the values and criteria listed above, we calculated a sample size of 384 and rounded it up to 400. We recruited eligible participants who visited public places like parks, shopping malls, and masjids using the convenience sampling method. In order to avoid enrolling participants from the same family who likely shared similar sociodemographic characteristics, we invited every 10th eligible participant for the present survey.
Ethical Consideration
We submitted the proposal for the present study and received approval from the regional ethics committee, Qurayyat Health Affairs, KSA MOH (reg. no. H-13-S-071). We followed the ethical principles of the Declaration of Helsinki. First, participants were given a brief orientation about the BC and its significance in the KSA, screening methods (mammography), and current survey purposes. Next, we obtained informed consent from the participants who were willing to participate in the survey. Since this was a questionnaire-based study, there was no risk to the participants. We ensured the privacy and confidentiality of all participants by using anonymous questionnaires.
Data-Collection Procedure
We used a structured and validated Arabic version data proforma adopted from a previous study. We obtained the required permission to use the questionnaire.11 The first section consisted of sociodemographic characteristics of the participants, such as age group, marital status, education level, employment status and monthly income, and family history of BC. The next section of the data-collection form included 14 items that asked about participants’ knowledge and awareness of BC risk factors and MS. The correct response to each item was marked “1”, while each wrong response was marked “0”. We calculated the total score by adding the scores of all 14 responses. The final section was composed of 19 questions that inquired about participants’ perceived barriers to MS uptake as implemented by the MOH. Each item asked about the specific barrier perceived by the participants. The overall MS barrier score was computed by assigning 2 points for agreement with each item, 0 points for non-agreement with each item, and 1 point for a neutral answer. Both knowledge and barriers scores were categorized into low (≤59% of the total score), medium (60–79% of the total score), and high (≥80% of the total score) groups. This categorization was completed according to Bloom’s cutoff values.17,18
Data Analysis
The present study used SPSS version 21 (IBM Corporation, Armonk, NY, USA) for coding, analyzing, and results output for the present study. We depicted the descriptive statistics as frequencies and percentages. The data were further tested for normality distribution with the Shapiro–Wilk test, and we observed that the data did not meet the normality assumption. Hence, we applied the Spearman correlation test to identify the correlation between BC knowledge and barrier scores. Furthermore, we combined the low and medium knowledge-degree categories into a single category and compared it with the high knowledge-degree category. We applied logistic regression analysis to find the factors associated with knowledge of BC risk factors and MS. We set P < 0.05, which was identified by two-tailed tests, as statistically significant.
Results
Of 400 participating women aged ≥40 years, the majority (58.3%) belonged to the age group of 40–49 years, were currently married (87.8%), had a monthly income of >7000 SAR (1 USD = 3.75 SAR) (40.7%), were living in urban areas (85.3%), and had at least a university-level education (66.5%). Regarding a family history of BC, 12.3% of participants reported that one of their family members had previously been diagnosed with BC (Table 1).
 |
Table 1 Participants’ Background Characteristics (n = 400) |
Regarding knowledge about BC risk factors and MS, the study participants reported that smoking habits (61.3%) and unhealthy dietary habits (57.8%) were the most common risk factors for BC, followed by a family history of BC (53.0%) and increased age (49.8%). Less than half (46.8%) of participants responded that MS is the ideal method for screening for early BC, and only 40% were aware of their eligibility to undergo MS as instituted by the KSA MOH (Table 2).
 |
Table 2 Participants’ Responses About Knowledge of BC and MS (n = 400) |
The barriers to MS uptake by study participants are depicted in Table 3. Fear of BC diagnosis (50.8%) and concerns regarding test procedures were the most common barriers to MS uptake, followed by lack of time, the embarrassment of undergoing a breast examination, and not receiving an adequate explanation of MS from health care workers.
 |
Table 3 Barriers to MS Uptake Women Aged ≥40 Years (n = 400) |
Of the studied participants, 56.3% had low knowledge about BC risk factors (Figure 1). Binomial logistic regression analysis revealed that the participant’s level of knowledge was significantly associated with their education level (adjusted odds ratio [aOR], 2.35; 95% confidence interval [CI], 1.61–3.13; P = 0.008), and a family history of BC (aOR, 3.66; 95% CI, 1.94–5.49; P < 0.001). The present study did not find any other predictors for a low level of knowledge about BC risk factors and MS (Table 4).
 |
Table 4 Binomial Logistic Regression Analysis to Find the Factors Associated with Knowledge of BC and MS Among the Participants (n = 400) |
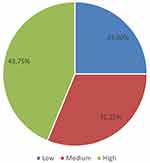 |
Figure 1 Degrees of knowledge about BC risk factors. |
We also found a negative correlation between participants’ knowledge and perceived barriers to MS (rho = −0.389, P < 0.001) (Table 5).
 |
Table 5 Correlation Between Knowledge and MS Barriers Scores |
Discussion
The results of this study indicate that a relatively small proportion of the study participants (12.3%) had a family member who was previously diagnosed with BC. This finding is consistent with prior research that reported varying rates of a family history of BC among women.19,20 It is important to note that a family history of BC is a significant risk factor for developing the disease.21,22 It remains important to encourage women with a family history of BC to undergo routine screening and surveillance despite the relatively low percentage of participants reporting a family history of BC. This may involve more frequent or earlier MS, genetic counseling, or other risk-reducing strategies. The high proportions of participants who were married, employed, and/or more highly educated may have implications for BC risk and awareness. Studies have shown that people with higher education levels are more aware of BC risk factors and screening methods.11,23 However, it is concerning to note that less than half of the respondents were aware and identified MS as the ideal method for screening for early BC, while only 40% were aware of their eligibility to undergo MS as instituted by the MOH, KSA. Our study findings are similar to those of a study by Abdel-Salam et al11 but conflict with those of previous studies reporting on women’s awareness and participation in MS in some of the European Union countries.14,24 Recent statistics on MS uptake among women in the European Union indicate that about two-thirds (66%) of women aged 50–59 years had been screened for BC using mammography. Of the countries surveyed, the highest level of MS uptake was observed in Sweden (95%), followed by in Finland (92%) and Denmark (82%). Interestingly, statistics from European Union countries in the Balkan region—namely, Bulgaria (36%) and Romania (9%)—showed that a lower proportion of women had undergone MS.24 Therefore, it is critical to explore further the reasons for the low levels of MS awareness and uptake in the Saudi Arabian context. Several cultural and contextual factors may influence women’s knowledge and attitudes toward BC and MS.25,26 Fear of BC diagnosis was the most common barrier, with 50.8% of participants citing this as a reason for not undergoing MS. This is followed by concerns regarding test procedures, not having enough time, embarrassment related to breast examination, and financial constraints. Therefore, It is crucial to address the anxiety associated with MS so that women feel comfortable undergoing screening.27,28 Similar to the present study results, D’almeida and Latha from India reported that about 57% of their study participants were frightened of the BC screening results.29 Concerns about the test procedures can also be a significant barrier to MS uptake among participants. It is important to provide clear and detailed information about the process and associated risks so that women feel informed and comfortable enough to undergo MS. Additionally, providing support and access to resources can help to address this barrier.30,31 A lack of time and financial constraints can also be significant barriers to MS uptake. It is vital to ensure that information on available programs and resources is readily available to eligible individuals. In addition, increasing the flexibility in scheduling can help to address the issue of a lack of time. Regarding a lack of time, Vahabi et al found that women who worked outside the home were less likely to participate in MS programs due to time constraints.32 Another study conducted in 2023 by Kaur et al stated that a lack of knowledge about MS and not understanding the importance of early diagnosis of BC were predictors for having barriers to MS.33
Other important barriers explored by the present study include a sense of embarrassment about the breast examination and an inadequate explanation of MS by health care workers. These findings are consistent with those of previous studies that identified fear and anxiety as significant barriers to MS uptake.34,35 A systematic review by Wardle et al found that women’s fear of BC and discomfort associated with the screening procedure were crucial factors in their decision not to participate in MS programs.32 In addition to radiation concerns and pain during the examination, the present study participants reported concerns about pain during the examination. Finally, the present study identified the fact that an inadequate explanation of MS by health care workers is also a barrier to MS uptake. Previous studies similarly found that women who did not receive clear and understandable information regarding the benefits and risks of MS were less likely to participate in screenings.36,37 Thus, health care providers should ensure patient comfort and provide them with accurate and precise information about the benefits and risks of MS as well as the process of the screening procedure itself.37 Multifaceted strategies, such as targeted education campaigns, better communication between health care providers and patients, and easier access to screenings, are needed to address these barriers identified in the present study.
Our study results indicated that more than half of the participants had limited knowledge about BC risk factors, which was significantly associated with their education level and a family history of BC. Nevertheless, the present study did not identify any factors associated with participants’ poor knowledge of BC risk factors and MS. According to previous studies, women, particularly those from low-income or less-educated backgrounds, are relatively unaware of BC risk factors and screening methods.26,38 Previous studies have reported that patients’ educational level and BC knowledge are related.11,26 The relative homogeneity of our study population may explain the lack of other identified predictors in our study. Future research could explore the role of other sociodemographic factors, such as income, employment status, and cultural beliefs, in shaping the knowledge and awareness of BC risk factors and screening methods. This study highlights the need to increase women’s awareness and education regarding BC risk factors and screening methods in KSA. A study in Pakistan by Saeed et al found that women with higher levels of education had significantly greater knowledge of BC risk factors than those with lower levels of education.26 Furthermore, Akhigbe et al found that women with higher education levels are more likely to better understand BC risk factors.39
This study found a negative correlation between participants’ knowledge of and perceived barriers to MS. Specifically, our findings indicated a statistically significant relationship between the two variables. Research suggests that people with greater knowledge about MS tend to perceive fewer barriers to undergoing screening; for example, Ayoub et al found a significant association between their study participants’ knowledge of BC and the breast self-examination screening method.40 This could be because their participants were more aware of the available screening methods and the potential benefits of managing their condition or because they better understood the condition, which can reduce fear or uncertainty about diagnosis and treatment.
The survey was carried out by the research team using a standard and validated tool with an adequate sample size. However, when reading the survey, some limitations should be kept in mind. First, the current survey, which assessed pre-eligible population knowledge and barriers, was limited to respondents from a single region. As a result, the findings may not be applicable to the entire KSA or other Middle Eastern countries. Second, we evaluated the factors associated with BC knowledge using a cross-sectional study design. As a result, we were unable to assess the temporal association. Finally, given the nature of our study, we cannot rule out recall, self-reported, and exaggerated response biases.
Conclusion
The present study determined that more than half of enrolled pre-eligible women had low or medium degrees of knowledge of BC risk factors and MS, which was significantly associated with their educational status and family history of BC. Fear of BC diagnosis and concerns regarding test procedures were the most common barriers to MS uptake. We also found a negative correlation between participants’ knowledge and perceived barriers to MS. This highlights the importance of providing access to appropriate educational resources to ensure that individuals are knowledgeable about the risks associated with BC and how to reduce them. Hence, health care professionals and educators should strive to provide appropriate educational materials and resources to individuals to ensure that everyone is aware of the potential risks associated with BC and how they can reduce them. Receiving reassurance and guidance from health care professionals may also be beneficial to reduce the perceived barriers to treatment further. We recommend that the concerned authorities organize multiple health education sessions at regular intervals at different facilities for women on BC risk factors and the necessity of MS uptake by pre-eligible women. Furthermore, a multicentric mixed-methods survey is warranted to find the qualitative aspects of the MS barriers.
Acknowledgments
We wish to thank all the participants for their willingness to participate in the survey. We extend our sincere thanks to the Ministry of Health, Jouf Health Affairs, Aljouf, for their kind cooperation.
Funding
This work was funded by the Deanship of Scientific Research at Jouf University under grant No (DSR2022-NF- 19).
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Breast cancer. World Health Organization; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Scope%20of%20the%20problem,the%20world’s%20most%20prevalent%20cancer.
2. Alkabban FM, Ferguson T. Breast cancer. In: StatPearls. StatPearls Publishing; 2022.
3. Yi M, Li T, Niu M, Luo S, Chu Q, Wu K. Epidemiological trends of women’s cancers from 1990 to 2019 at the global, regional, and national levels: a population-based study. Biomark Res. 2021;9(1):55. doi:10.1186/s40364-021-00310-y
4. Alqahtani WS, Almufareh NA, Domiaty DM, et al. Epidemiology of cancer in Saudi Arabia thru 2010–2019: a systematic review with constrained meta-analysis. AIMS Public Health. 2020;7(3):679–696. doi:10.3934/publichealth.2020053
5. Wang L. Early diagnosis of breast cancer. Sensors. 2017;17(7):25.
6. Milosevic M, Jankovic D, Milenkovic A, Stojanov D. Early diagnosis and detection of breast cancer. Technol Health Care. 2018;26(4):729–759. doi:10.3233/thc-181277
7. Anderson BO, Ilbawi AM, Fidarova E, et al. The Global Breast Cancer Initiative: a strategic collaboration to strengthen health care for non-communicable diseases. Lancet Oncol. 2021;22(5):578–581. doi:10.1016/S1470-2045(21)00071-1
8. Reeves RA, Kaufman T. Mammography. In: StatPearls. StatPearls Publishing; 2022.
9. Horsley RK, Kling JM, Vegunta S, Lorans R, Temkit H, Patel BK. Baseline mammography: what is it and why is it important? A cross-sectional survey of women undergoing screening mammography. J Am Coll Radiol. 2019;16(2):164–169. doi:10.1016/j.jacr.2018.07.002
10. Ministry of Health. Breast cancer early detection. Saudi Arabia: Ministry of Health; 2022. Available from: https://www.moh.gov.sa/en/Ministry/Projects/breast-cancer/Pages/default.aspx.
11. Abdel-Salam DM, Mohamed RA, Alyousef HY, et al. Perceived barriers and awareness of mammography screening among Saudi women attending primary health centers. Risk Manag Healthc Policy. 2020;13:2553–2561. doi:10.2147/rmhp.S277375
12. AlSaleh KA. Efficacy of breast cancer screening program in Kingdom of Saudi Arabia. Saudi Med J. 2022;43(4):428–430. doi:10.15537/smj.2022.43.4.20210823
13. Azaiza F, Cohen M. Health beliefs and rates of breast cancer screening among Arab women. J Womens Health. 2006;15(5):520–530. doi:10.1089/jwh.2006.15.520
14. Wang Y-J, Wang F, Yu L-X, et al. Worldwide review with meta-analysis of women’s awareness about breast cancer. Patient Educ Couns. 2022;105(7):1818–1827. doi:10.1016/j.pec.2021.12.012
15. Abdullah N, Baharudin N, Mohamad M, Mohamed-Yassin MS. Factors associated with screening mammogram uptake among women attending an urban university primary care clinic in Malaysia. Int J Environ Res Public Health. 2022;19(10):6103. doi:10.3390/ijerph19106103
16. Cochran WG. Sampling Techniques.
17. Khaled A, Siddiqua A, Makki S. The knowledge and attitude of the community from the Aseer Region, Saudi Arabia, Toward COVID-19 and their precautionary measures against the disease. Risk Manag Healthc Policy. 2020;13:1825–1834. doi:10.2147/rmhp.S271899
18. Thirunavukkarasu A, Al-Hazmi AH, Dar UF, et al. Knowledge, attitude and practice towards bio-medical waste management among healthcare workers: a northern Saudi study. PeerJ. 2022;10:e13773. doi:10.7717/peerj.13773
19. Chen WY, Colditz GA. Risk factors and hormone-receptor status: epidemiology, risk-prediction models and treatment implications for breast cancer. Nat Clin Pract Oncol. 2007;4(7):415–423. doi:10.1038/ncponc0851
20. Tavani A, Gallus S, La Vecchia C, et al. Risk factors for breast cancer in women under 40 years. Eur J Cancer. 1999;35(9):1361–1367. doi:10.1016/s0959-8049(99)00139-2
21. American Cancer Society. Breast cancer risk and prevention. American Cancer Society; 2023. Available from: https://www.cancer.org/cancer/breast-cancer/risk-and-prevention.html.
22. Alshahrani M, Alhammam SYM, Al Munyif HAS, et al. Knowledge, attitudes, and practices of breast cancer screening methods among female patients in primary healthcare centers in Najran, Saudi Arabia. J Cancer Educ. 2019;34(6):1167–1172. doi:10.1007/s13187-018-1423-8
23. Abdel-Aziz SB, Amin TT, Al-Gadeeb MB, et al. Perceived barriers to breast cancer screening among Saudi women at primary care setting. J Prev Med Hyg. 2018;59(1):E20–e29. doi:10.15167/2421-4248/jpmh2018.59.1.689
24. European Union. Mammogram screening statistics - 66% of women in the EU aged 50–69 got a mammogram. European Union; 2023. Available from: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20211025-1#:~:text=got%20a%20mammogram-,66%25%20of%20women%20in%20the%20EU%20aged%2050%2D69%20got,a%20mammogram%20%2D%20Products%20Eurostat%20News&text=In%202019%2C%20two%2Dthirds%20(,Interview%20Survey%20(EHIS)%20survey.
25. Alenezi AM, Thirunavukkarasu A, Wani FA, et al. Female healthcare workers’ knowledge, attitude towards breast cancer, and perceived barriers towards mammogram screening: a multicenter study in North Saudi Arabia. Curr Oncol. 2022;29(6):4300–4314. doi:10.3390/curroncol29060344
26. Saeed S, Asim M, Sohail MM. Fears and barriers: problems in breast cancer diagnosis and treatment in Pakistan. BMC Womens Health. 2021;21(1):151. doi:10.1186/s12905-021-01293-6
27. Claire ELJ, Jill M, Ruth HJ, et al. A systematic review of barriers to early presentation and diagnosis with breast cancer among black women. BMJ Open. 2014;4(2):e004076. doi:10.1136/bmjopen-2013-004076
28. Bourdeanu L, Alatrash M, Ketchedjian N, Pate B. Perceived fears, barriers, and benefits regarding breast cancer screening: a comparison of Lebanese and Lebanese-American women. JCO Glob Oncol. 2020;6:1200–1210. doi:10.1200/go.20.00019
29. D’Almeida D, Latha T. Barriers for early detection of breast cancer among South Indian Women. Indian J Community Med. 2021;46(4):706–709. doi:10.4103/ijcm.IJCM_751_20
30. Srinath A, van Merode F, Rao SV, Pavlova M. Barriers to cervical cancer and breast cancer screening uptake in low- and middle-income countries: a systematic review. Health Policy Plan. 2023;38(4):509–527. doi:10.1093/heapol/czac104
31. Castaldi M, Smiley A, Kechejian K, Butler J, Latifi R. Disparate access to breast cancer screening and treatment. BMC Womens Health. 2022;22(1):249. doi:10.1186/s12905-022-01793-z
32. Wardle J, Robb K, Vernon S, Waller J. Screening for prevention and early diagnosis of cancer. Am Psychol. 2015;70(2):119–133. doi:10.1037/a0037357
33. Kaur K, Jajoo R, Naman S, et al. Identifying barriers to early diagnosis of breast cancer and perception of women in Malwa region of Punjab, India. Global Health J. 2023;7(1):34–42. doi:10.1016/j.glohj.2023.02.006
34. Al-Azri M, Al-Rubaie K, Al-Ghafri S, Al-Hinai M, Murthi Panchatcharam S. Barriers and attitudes toward breast cancer screening among Omani women. Asian Pac J Cancer Prev. 2020;21(5):1339–1347. doi:10.31557/apjcp.2020.21.5.1339
35. Haghighi JD, Hormozi M, Sargolzaee N, Izadirad H, Hamdollahi F. Barriers to mammographic screening of breast cancer in women: a cross-sectional study in Southeastern Iran: barriers to mammography screening. Archiv Breast Cancer. 2022;174–178. doi:10.32768/abc.202292174-178
36. Amélie AE, Ruelle Y, Frèche B, et al. What do women and healthcare professionals expect of decision aids for breast cancer screening? A qualitative study in France. BMJ Open. 2022;12(3):e058879. doi:10.1136/bmjopen-2021-058879
37. Tsang E, Chan M, Chan L, Chan J, Lee S, Tsui M. Role of healthcare professionals in cancer screening. Hong Kong Med J Xianggang Yi Xue Za Zhi. 2020;26(6):546–548. doi:10.12809/hkmj209148
38. Al-Mousa DS, Alakhras M, Hossain SZ, et al. Knowledge, attitude and practice around breast cancer and mammography screening among Jordanian women. Breast Cancer. 2020;12:231–242. doi:10.2147/bctt.S275445
39. Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9(1):203. doi:10.1186/1471-2407-9-203
40. Ayoub NM, Al-Taani GM, Almomani BA, et al. Knowledge and practice of breast cancer screening methods among female community pharmacists in Jordan: a cross-sectional study. Int J Breast Cancer. 2021;2021:9292768. doi:10.1155/2021/9292768
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
