Back to Journals » Cancer Management and Research » Volume 12
With High-Risk Factors, Total Thyroidectomy is Preferred for Thyroid Cancer
Authors Han L, Li W, Li Y, Wen W, Yao Y, Wang Y
Received 11 February 2020
Accepted for publication 5 May 2020
Published 20 May 2020 Volume 2020:12 Pages 3713—3719
DOI https://doi.org/10.2147/CMAR.S249324
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Lin Han,1 Wenlei Li,2 Yingxue Li,1 Wenjuan Wen,1 Yumin Yao,2 Yongkun Wang2
1Department of Pathology, Liaocheng People’s Hospital, Affiliated to Shandong First Medical University, Liaocheng 252000, Shandong, People’s Republic of China; 2Department of Thyroid Surgery, Liaocheng People’s Hospital, Affiliated to Shandong First Medical University, Liaocheng 252000, Shandong, People’s Republic of China
Correspondence: Yongkun Wang
Department of Thyroid Surgery, Liaocheng People’s Hospital, Affiliated to Shandong First Medical University, Liaocheng 252000, Shandong, People’s Republic of China
Tel/ Fax +86-6358272235
Email [email protected]
Introduction: Based on thyroid cancer data from patients treated in Liaocheng People’s Hospital in 2017, with Chinese national and regional characteristics, in this study we addressed the controversy of which initial thyroid surgical mode, lobectomy or total thyroidectomy, is most effective.
Patients and Methods: Clinical and pathological data from 552 patients with thyroid cancer, who were initially diagnosed and treated surgically, were collected from the Department of Thyroid Surgery. Among them, 40 patients underwent endoscopic surgery, with resection including lobectomy + central lymph node dissection of the affected lobe, while 512 cases underwent total thyroidectomy + central lymph node dissection.
Results: The metastasis rate for all patients was 59.42%. Further, among patients with bilateral or multiple tumors or capsule invasion, the proportions who developed metastatic disease were 63.54% and 71.19% and 67.46%, respectively. Meanwhile, the incidence of contralateral accidental malignancy was 7.25% after postoperative paraffin pathology.
Discussion: Rates of neck lymph node metastasis are high, particularly among patients with risk factors for poor prognosis. It is recommended that, among patients with risk factors, initial treatment should comprise at least total thyroidectomy + central lymph node dissection in China, to avoid the risks associated with secondary surgery and effects on patient quality of life.
Keywords: thyroid cancer, metastasis, surgery, real world, initial treatment
Introduction
In the past 30 years, the incidence of thyroid cancer has been increasing annually worldwide, including China. Thyroid cancer has become the third most common malignancy in women in China, representing a heavy economic burden on both society and individuals.1
Effective and appropriate surgical treatment is the most important and effective clinical treatment for differentiated thyroid carcinoma. Differentiated thyroid carcinoma (DTC) accounts for 80–90% of thyroid cancer incidence. Cervical lymph node metastasis is one of the risk factors for DTC, and it is also the most common metastatic site. The initial surgical treatment of DTC is still controversial; total thyroidectomy or lobectomy is more preferred. There has been no large sample randomized controlled clinical trial to compare these two methods.2,3 It is obvious that when DTC is associated with multiple risk factors such as multiple, bilateral and capsule invasion, the lymph node metastasis rate does increase, and we believe this is also a high-risk factor for DTC.4–6
Chinese experts do not consider papillary thyroid microcarcinoma (PTMC; a lesion with a nodule diameter of ≤1 cm) a low-risk carcinoma, as any advanced thyroid cancer is a development from micro-cancer. Any cancer that initially occurs is not late-stage advanced papillary thyroid carcinoma (PTC).7,8 The incidence of lymph node metastasis in patients with central region PTC is 20–66%,9,10 which indicates that although PTC progresses slowly, its ability and tendency to metastasize to lymph nodes are obvious, and even for distant organs. It is unscientific to classify malignant tumors based on tumor size, as the invasiveness and distant metastatic ability of tumors are a consequence of the evolution of the tumor genome.11,12 We believe that some high-risk factors of tumor self-combination can also be used as one of the reference standards for its metastatic ability. These factors should arouse our attention in clinical work and treat them more actively.
We collected clinical and pathological data from 552 patients undergoing treatment at the Department of Thyroid Surgery, Liaocheng People’s Hospital, and analyzed their responses to current treatment approaches. We aimed to determine the most appropriate initial surgical intervention for patients in China with this condition.
Patients and Methods
Patient Selection
This study was a retrospective analysis of a total of 552 cases of PTC treated and undergoing surgery from January 1 to December 31, 2017 in the Department of Thyroid Surgery, Liaocheng People’s Hospital. All patients underwent fine-needle aspiration before surgery and had pathological diagnoses of papillary carcinoma or suspected papillary carcinoma.
Surgery
Surgical procedures were as follows: 40 cases underwent endoscopic surgery, with resection ranging from the lateral lobes of the affected side to central lymph node dissection of the affected side. The remaining 512 patients underwent total thyroidectomy and central lymph node dissection. For patients <18 years old, informed consent was obtained from both parents.
Ethical Approval
Surgical methods were based on the guidelines of Chinese Thyroid Cancer (CTA), following the experience of clinical professors. The study was conducted in accordance with the Declaration of Helsinki. The ethical approval number is 2016071.
Data Acquisition
Pathological data were obtained from the Department of Pathology, Liaocheng People’s Hospital, and were based on post-operative analysis of paraffin-embedded tumor samples. Information on all patients was systematically coded in a single computer file. Data from this system were exported for statistical analyses.
Results
All patients were treated directly after the discovery of the lesion, without any observation period. Cases included 105 males and 447 females, and were 13~72 years old, with 72 cases aged ≤35 years (Table 1). The pathological subtypes present among the 552 cases of PTC were classical (n = 537), follicular variant (n = 12), tall cell variant (n = 2), and solid variant (n = 1) (Figure 1).
 |
Table 1 The Age and Gender of Patients |
The mean incidence of metastasis was 59.42%, and the metastasis rate was positively correlated with tumor diameters ≤0.5 to >2 cm associated with rates from 44.68% to 77.53%, respectively (Table 2).
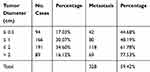 |
Table 2 Thyroid Cancer Diameter and Metastasis |
The proportion of PTMC (≤1 cm) was 47.10%, with a lymph node metastasis rate of 46.92% (Table 3).
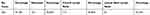 |
Table 3 The Proportion and Clinical Characteristics of Patients with Papillary Thyroid Microcarcinoma |
The proportion of bilateral cancer was 32.79%, with a metastasis rate of 63.54%, while the proportion of patients with multiple tumors was 21.38%, with a metastasis rate of 71.19%, in the same time, at the same time, the proportion of capsule invasion was 22.82%, with a metastasis rate of 67.46%. Where the contralateral lobe was negative before surgery, the incidence of contralateral malignancy diagnosed following surgery was 7.25% after postoperative pathology evaluation of paraffin-embedded samples (Table 4).
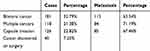 |
Table 4 High-Risk Factors Among Patients with Thyroid Cancer |
Among patients undergoing lobectomy and total thyroidectomy, the proportions with lymph node metastasis were 32.5% and 39.84% (Table 5).
 |
Table 5 Types of Surgery with Thyroid Cancer |
In addition, we enumerated the number of cases of surgery for thyroid cancer at our hospital from 2009 to 2018 and the results demonstrate that the number of cases generally rose annually by 4.72–18.16% (Figure 2).
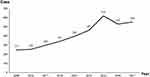 |
Figure 2 Numbers of cases of thyroid cancer treated at our hospital in the past 9 years. |
Discussion
According to the results of the SEER database of the National Cancer Center of the United States, the incidence of both PTC < 1.0 cm and thyroid cancers 1.0–4.0 cm increased from 1980 to 2010, especially among highly educated groups.13,14 At present, a lot of research has been conducted on risk factors related to thyroid cancer, and it has been found that autoimmune disorders, ionizing radiation, iodine intake, estrogen, environmental endocrine disruptors, negative psychosocial factors, and heredity, etc., which are closely related to thyroid cancer related.15–17
As available therapies for thyroid cancer are effective, there is no need for early diagnosis and surgical treatment, which is logically wrong, which violates the basic principles of early detection, early diagnosis and early treatment of malignant tumors. In addition, after the diagnosis of thyroid cancer, the patient waits for changes during follow-up before taking action. During this process, the psychological pressure of the patient is undoubtedly huge. Fear of cancer does not have “Chinese characteristics”. In 2014, the Memorial Sloan-Kettering Cancer Center in the United States launched a “wait-and-see” program for patients with thyroid cancer. Patients diagnosed with PTMC can choose not to be removed, but to have regular examinations. However, the vast majority of PTMC patients do not hesitate to choose surgical treatment. At the same time, some patients who choose to observe require surgery after a period of time. And doctors are worried about being sued for missing the best treatment time.18 Early treatment is not only effective, but it is also associated with reduced risk and fewer complications.19 In particular, the possibility of dedifferentiation increases with prolonged tumor-bearing time and patient age.20–22
According to our clinical and pathological data, as the diameter of the tumor mass increased from ≤0.5 to >2 cm, the proportion of lymph node metastasis rose from 44.68% to 77.53%, respectively. The proportion of micropapillary carcinoma ≤1 cm was 47.10%, with a corresponding lymph node metastasis rate of 46.92%, which is not consistent with the classification of microcarcinomas as low-risk tumors. Lymph node metastasis is also an indicator of malignancy. Over time, tumor size and the proportion and number of lymph node metastases will increase, leading to disease progression, increased difficulty and risk of surgery, and a gradual rise in the risk of recurrence and metastasis. When the mass was >2 cm, the proportion of patients with lymph node metastasis rose to 77.53%, indicating that PTC was progressing, including the level of malignancy and dedifferentiation, although there is no way to evaluate or predict such progression.
The proportions of bilateral and multiple cancers were 32.79% and 21.38%, respectively, with corresponding metastasis rates of 63.54% and 71.19%, at the same time, the proportion of capsule invasion was 22.82%, with a metastasis rate of 67.46%, consistent with literature reports.23 When associated with high-risk factors, such as bilateral and multiple lesions, the lymph node metastasis rate is significantly increased, suggesting that a more comprehensive preoperative clinical evaluation is required, to obtain more complete information on patient disease status, with the aim of optimizing the surgical approach.
The National Comprehensive Cancer Network (NCCN) guidelines recommend that patients with PTC aged <15 or >45 years should undergo total thyroidectomy. At the same time, the American Thyroid Association (ATA) guidelines recommend that all PTC patients with tumor diameters >1 cm undergo total thyroidectomy. The Chinese Thyroid Association (CTA) guidelines state that all patients with PTC should undergo central lymph node dissection, but there is no special requirement for age. Total thyroidectomy can have advantages for patients, including: 1) single treatment of multiple lesions, particularly bilateral cancer lesions; 2) facilitates postoperative monitoring of tumor recurrence and metastasis; 3) beneficial for postoperative I131 treatment; 4) reduces the recurrence rate of tumors and the probability of reoperation, which avoids increasing the incidence of serious complications due to reoperation; 5) accurate assessment of postoperative staging and risk stratification of patients; 6) prevention of recurrence of thyroid cancer from development into poorly differentiated thyroid cancer. For PTC with risk factors such as bilateral, multiple, and capsular invasion, no consensus has been reached on all current guidelines.
The incidence of contralateral malignancy discovered after the postoperative pathological examination of paraffin-embedded specimens was 7.25%, of which all such lesions were small (<0.1 cm). Preoperative color doppler ultrasound and CT examination were negative in this group of patients. Contralateral malignant lesions were detected after surgery in 40 patients, which suggests that our full clinical imaging assessment is still not ideal, and may miss malignant lesions. At present, due to the limitations of examination techniques, some preoperative examinations used in clinical practice cannot reveal suspected cancer lesions in the contralateral glandular lobe.23 But total thyroidectomy completely removes any such lesions and glands with potential lesions, thereby avoiding the risk of undetected cancer lesions, reducing the recurrence rate and improving patient prognosis.24,25 Thyroidectomy can lead to some inevitable complications, including the most common parathyroid injury (3–5%) and recurrent laryngeal nerve injury (1–5%). It is accepted that patients who undergo total or partial thyroidectomy must use thyroxine replacement, or even suppression, therapy for the rest of their lives.26,27 Endocrine suppression therapy is essential and has nothing to do with surgical methods. Hence, long-term endocrine suppression therapy was required for all patients with PTC, regardless of total thyroidectomy or lobectomy. Radioactive I131 therapy is also an important part of the comprehensive treatment of thyroid cancer.28,29 The method of treatment of thyroid cancer is a comprehensive treatment, which is influenced not only by surgeons but also by nuclear medicine, imaging, and other clinicians, and even by health insurance companies. Careful preoperative assessment and risk analysis of thyroid cancer will result in more accurate and more personalized treatment measures. We need to make a comprehensive judgment based on surgical principles, the willingness of the patient and medical resources available, together with the national considerations and regional factors in China, the degree of acceptance of the operation, and possible secondary surgery ultimately formulate a reasonable diagnosis and treatment plan.
Conclusion
The data from our department inform several important points. 1. The incidence of thyroid cancer cases in our hospital generally rose annually during 2009–2018 from a minimum of 247 to a maximum of 600 (increase rates from 4.72% to 18.16%). 2. PTC, even PTMC, has a high rate of local metastasis (59.42% and 46.92%, respectively) as, although it is an inert tumor after recovery, high invasiveness can occur on the evolution of the tumor genome, indicating that it cannot be considered to exhibit a low degree of malignancy. When tumor diameter was > 2 cm, the rate of cervical lymph node metastasis rose to 77.53%, suggesting that more aggressive and thorough treatment is required for patients with such tumors 3. When there were complications of high-risk factors, such as bilateral lesions, multiple lesions, and capsule invasion, tumors were highly aggressive, with metastasis rates of 63.54%, 71.19% and 67.46%, respectively, suggesting that priority should be given to total central thyroidectomy lymph node dissection. Postoperative complications and long-term follow-up data will be reported in the future.
Data Sharing Statement
We confirm that we will share the data underlying the findings reported in this manuscript and allow researchers to verify the results presented, replicate the analysis, and conduct secondary analyses.
Ethics Approval and Consent to Participate
All medical records are legal and reasonable. The study was approved and supervised by the ethics committee of Liaocheng People’s Hospital, affiliated to Shandong First Medical University.
Consent to Publish
All authors read and approved the final manuscript.
Acknowledgments
We thank Shandong First Medical University and Liaocheng People’s Hospital for supporting this study, and also the pathology and thyroid surgery staff for their support and assistance in conducting this study. We thank everyone involved in this study for their hard work.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries[J]. Lancet Glob Health. 2018;6(5):e555–e567. doi:10.1016/S2214-109X(18)30127-X
2. Bilimoria K, Bentrem DJ, Ko CY, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 2007;246(3):375–384. doi:10.1097/SLA.0b013e31814697d9
3. Ito Y, Miyauchi A, Oda H. Low-risk papillary microcarcinoma of the thyroid: a review of active surveillance trials. Eur J Surg Oncol. 2018;44(3):307–315. doi:10.1016/j.ejso.2017.03.004
4. Choi JB, Lee WK, Lee SG, et al. Long-term oncologic outcomes of papillary thyroid microcarcinoma according to the presence of clinically apparent lymph node metastasis: a large retrospective analysis of 5,348 patients. Cancer Manag Res. 2018;10:2883–2891. doi:10.2147/CMAR.S173853
5. Wu X, Li B, Zheng C, He X. Predicting factors of lateral neck lymph node metastases in patients with papillary thyroid microcarcinoma. Medicine. 2019;98(27):e16386. doi:10.1097/MD.0000000000016386
6. Pathak KA, Leslie WD, Klonisch TC, et al. The changing face of thyroid cancer in a population-based cohort. Cancer Med. 2013;2:537–544. doi:10.1002/cam4.103
7. Alwithenani R, DeBrabandere S, Rachinsky I, et al. Performance of the American Thyroid Association risk classification in a single center cohort of pediatric patients with differentiated thyroid cancer: A retrospective study. J Thyroid Res. 2019;2019:5390316. doi:10.1155/2019/5390316
8. Jingqiang Z, Jianyong L. Overtreatment and deficiency of micropapillary thyroid carcinoma. Chin J Practical Surg. 2016;36(5):520–523.
9. McDow AD, Pitt SC. Extent of surgery for low-risk differentiated thyroid cancer. Surg Clin North Am. 2019;99(4):599–610. doi:10.1016/j.suc.2019.04.003
10. Huang T. Standard diagnosis and treatment of micropapillary thyroid carcinoma: controversy, conclusion early. J Gen Clin Basis China. 2016;23(10):12.
11. Dettmer MS, Schmitt A, Komminoth P, et al. Poorly differentiated thyroid carcinoma: an underdiagnosed entity. Pathology. 2019. doi:10.1007/s00292-019-0600-9
12. Dong F, Zhang B, Shan G. Epidemic situation and influential factors of thyroid cancer in China. China Cancer J. 2016;26(1):47–52.
13. Li N, Du XL, Reitzel LR, et al. Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the surveillance, epidemiology, and end results registry, 1980–2008. Thyroid. 2013;23(1):103–110. doi:10.1089/thy.2012.0392
14. Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer epidemic-screening and overdiagnosis. N Engl J Med. 2014;371(19):1765–1767. doi:10.1056/NEJMp1409841
15. Pellegriti G, Frasca F, Regalbuto C, et al. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013;2013:965212. doi:10.1155/2013/965212
16. Choi WR, Roh JL, Gong G, et al. Multifocality of papillary thyroid carcinoma as a risk factor for disease recurrence. Oral Oncol. 2019;94:106–110. doi:10.1016/j.oraloncology.2019.05.023
17. Ruggiero R, Pirozzi R, Gualtieri G. Overview on surgical management of papillary thyroid microcarcinoma. G Chir. 2019;40(2):81–87.
18. Morris LG, Wong RJ, Tuttle RM. Ethical considerations when counseling patients with thyroid cancer about surgery vs observation. JAMA Otolaryngol Head Neck Surg. 2016;142(4):406–407. doi:10.1001/jamaoto.2016.0038
19. Yan L, Blanco J, Reddy V, et al. Clinicopathological features of papillary thyroid microcarcinoma with a diameter less than or equal to 5 mm. Am J Otolaryngol. 2019;40(4):560–563. doi:10.1016/j.amjoto.2019.05.003
20. Chen Y, Gao X, Cao M, et al. A case-control study of risk factors for thyroid cancer. Public Health China. 2014;30(7):955–957.
21. Zheng X, Peng C, Gao M, et al. Risk factors for cervical lymph node metastasis in papillary thyroid microcarcinoma: a study of 1,587 patients. Cancer Biol Med. 2019;16(1):121–130. doi:10.20892/j.issn.2095-3941.2018.0125
22. Hodax JK, Bowerman K, Quintos JB, et al. Benign thyroid nodules in pediatric patients: determining best practices for repeat ultrasound evaluations. J Pediatr Endocrinol Metab. 2019;32(8):895–901. doi:10.1515/jpem-2018-0476
23. Kaliszewski K, Diakowska D, Wojtczak B, et al. The occurrence of and predictive factors for multifocality and bilaterality in patients with papillary thyroid microcarcinoma. Medicine. 2019;98(19):e15609. doi:10.1097/MD.0000000000015609
24. Esnaola NF, Cantor SB, Sherman SI, et al. Optimal treatment strategy in patients with papillary thyroid cancer: a decision analysis. Surgery. 2001;130(6):921–930. doi:10.1067/msy.2001.118370
25. Gimm O, Brauckhoff M, Thanh PN, et al. An update on thyroid surgery. Eur J Nucl Med Imaging. 2002;29(suppl 2):447–452. doi:10.1007/s00259-002-0913-3
26. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1–133. doi:10.1089/thy.2015.0020
27. Polistena A, Sanguinetti A, Patrone R, et al. Unintentional recurrent laryngeal nerve injuries following thyroidectomy: Is it the surgeon who pays the bill? Int J Surg. 2017;41(Suppl 1):S55–S59. doi:10.1016/j.ijsu.2017.01.112
28. Yang T, Zheng SY, Jiao J, et al. Radioiodine remnant ablation in papillary thyroid microcarcinoma: a meta-analysis. Nucl Med Commun. 2019;40(7):711–719. doi:10.1097/MNM.0000000000001018
29. Conzo G, Polistena A, Calò PG, et al. Efficacy of combined treatment for anaplastic thyroid carcinoma: results of a multinstitutional retrospective analysis. Int J Surg. 2014;12(Suppl 1):S178–82. doi:10.1016/j.ijsu.2014.05.015
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

