Back to Journals » Patient Preference and Adherence » Volume 17
Willingness to Undergo Gastroscopy for Early Gastric Cancer Screening and Its Associated Factors During the COVID-19 Pandemic – A Nationwide Cross-Sectional Study in China
Authors Ma K , Chen X, Xiang X, Mao X, Zhu N, Wang T, Ye S, Wang X, Deng M
Received 10 December 2022
Accepted for publication 18 February 2023
Published 1 March 2023 Volume 2023:17 Pages 505—516
DOI https://doi.org/10.2147/PPA.S400908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kejia Ma,1,2 Xuejie Chen,1,2 Xin Xiang,3 Xueyi Mao,3 Ningxin Zhu,1,2 Tianyu Wang,1,2 Shuyu Ye,1,2 Xiaoyan Wang,1,2,* Minzi Deng1,2,*
1Department of Gastroenterology, The Third Xiangya Hospital of Central South University, Changsha, Hunan, People’s Republic of China; 2Hunan Key Laboratory of Nonresolving Inflammation and Cancer, Changsha, Hunan, People’s Republic of China; 3Xiangya Medical College of Central South University, Changsha, Hunan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoyan Wang; Minzi Deng, Department of Gastroenterology, The Third Xiangya Hospital, Central South University, No. 138 Tongzipo Road, Changsha, Hunan, People’s Republic of China, Tel +86 139 7488 9301 ; +86 137 8615 2169, Email [email protected]; [email protected]
Purpose: This study aimed to investigate the willingness of Chinese adults aged 40 years and older to undergo gastroscopy for gastric cancer (GC) screening during the COVID-19 pandemic in 2020. The secondary purpose was to identify factors influencing willingness to undergo gastroscopy.
Methods: A cross-sectional questionnaire survey was conducted in selected cities and counties from nine provinces in China using a multi-stage sampling approach. A multivariate logistic regression model was used to determine the independent predictors of willingness to undergo gastroscopy.
Results: This study included 1900 participants, and 1462 (76.95%) responded that they would undergo gastroscopy for GC screening. Participants of younger age, from the eastern region, living in an urban area, with higher educational levels, with Helicobacter pylori (H. pylori) infection, or with precancerous stomach lesions, were more willing to undergo gastroscopy. The top four reasons to reject gastroscopy were fear of pain or discomfort, worry about a possible devastating test result, no symptoms in self-feeling, and concern about the high expense. Of all those who would reject gastroscopy for GC screening, 36.76% (161/438) would be willing to accept painless gastroscopy, while 24.89% (109/438) would be willing to undergo gastroscopy screening if higher medical reimbursement rates were available. Participants considered that gastroscopy was a relatively fearful and unknown procedure, accompanied by high risks and benefits compared to all other life events.
Conclusion: In general, 76.95% of participants over 40 years old were willing to undergo gastroscopy for GC screening in China during the COVID-19 pandemic. Participants’ willingness to undergo GC screening increased due to medical resource constraints and increased interest in their health. Individuals with H. pylori infection are more likely to undergo gastroscopy, whereas old age individuals, those with lower educational levels, and those living in rural areas are more likely to reject gastroscopy.
Keywords: gastrointestinal tumors, endoscopy, public health, early screening, questionnaire
Introduction
In March of 2020, the World Health Organization proclaimed a global pandemic of coronavirus disease 2019 (COVID-19) after the first case was reported in Wuhan, China, in 2019.1 The Chinese government has introduced relevant policies to limit crowd gathering and maintain social distancing to control the spread of COVID-19. It has also increased investment in medical resources for COVID-19 prevention, control, and treatment. Several studies have reported that cancer screening implementation and access declined during the COVID-19 pandemic.2,3 Early screening for gastric cancer (GC) has also been affected by COVID-19.4 GC is a common cause of cancer-related deaths worldwide, ranking fourth for mortality, and over one million new cases occurred in 2020.5 China has a high incidence of GC, contributing to 48.26% of the global incidence in 2019. While the mortality rate of GC in China decreased from 1999 to 2019, this decrease was still lower than the average percentage reduction worldwide.6 China has a higher mortality/incidence ratio than most developed countries.7 The rate of early GC diagnosis and treatment in China is less than 15%, which is far lower than that in other Asian countries with a high GC incidence, such as Korea and Japan.8
Due to the occult onset of GC, over 80% of patients are diagnosed in an advanced stage; therefore, there is an urgent need to increase the early screening rate.9 The fastest approach to reducing the GC incidence rate is to increase public awareness of endoscopic screening programs for high-risk groups and the necessity of screening. For example, Korean and Japanese screening programs and development of endoscopic treatment for early GC have led to substantial reductions in GC-associated mortality.10
Gastroscopy is the gold standard for GC diagnosis. The 2015 American Society for Gastrointestinal Endoscopy guidelines suggest that gastroscopy is effective for early GC identification in high-risk countries, and high-risk groups are recommended to undergo gastroscopy screening as soon as possible.11 Endoscopic resection and monitoring endoscopy are suggested in patients with confirmed gastrointestinal metaplasia with high dysplasia.11 GC screening is also recommended for individuals at average risk of GC who are over 40 years old. Therefore, most Asian countries have set the threshold age for screening to 40–45 years; in countries with a high incidence of GC, such as Japan and South Korea, the screening age is set at 40 years.12–14 Most case-control studies of imaging screening have shown a 40–60% reduction in GC mortality.15,16 However, due to the high cost, high human resource investment, and low acceptance among the population, there is currently no simple and effective diagnostic method for the general population. China has not implemented a large-scale population screening program for GC, other than several GC screening programs that have been restricted to selected areas.17 A survey conducted in Henan Province, China, among high-risk groups for upper gastrointestinal cancer showed that endoscopic screening compliance was low, at only 18.41%.18 The reason for the discrepancy between an individual’s high willingness to undergo gastroscopy for GC screening and their much lower compliance rate remains unclear. Therefore, an understanding of the reasons for individual willingness and rejection of gastroscopy for GC screening is relevant to future cancer screening promotion and clinical practice.
In this study, we investigated the cognition, willingness, and reasons for rejection of gastroscopy in populations over 40 years old during the COVID-19 pandemic, via cluster sampling in 36 communities in China. The findings are expected to provide reference data for decision-makers to identify ways to improve the GC screening rate. The overarching aim was to increase the rate of gastroscopy for GC screening among the public, thereby improving the early detection rate and reducing the GC mortality rate. By enhancing awareness of GC and various risk factors for precancerous lesions, the willingness to undergo gastroscopy may be improved to a certain extent.
Materials and Methods
Study Design and Population
We conducted a cross-sectional survey in nine provinces, representing all three regions of China: three each in the east (Hainan, Shandong, and Zhejiang), central region (Anhui, Shanxi, and Hunan), and west (Gansu, Guangxi, and Guizhou). The nine provinces are also representative of China’s socioeconomic status. Data collection was from March 25, 2020, to August 12, 2020. The inclusion criteria were 1) above 40 years old, 2) registration in a community administration, and 3) no history of cancer. The exclusion criteria were: 1) an incomplete questionnaire; 2) a completion time of less than 3 minutes, which indicated that the questionnaire responses were invalid; and 3) the patient refused the use of their questionnaire responses in this study.
Sample Size Calculation and Sampling Strategy
The sample size calculation formula (N = [με × π × (1-π)] / δ2) and related parameters are referred to in classic literature,19 with the prevalence rate (π) set as 30%. Based on the preliminary level of rejection for the study, the level of significance (α) was 0.05, and the allowable error (δ) was 0.25. Therefore, the required minimum sample size was 1291. Considering a non-response rate of 30%, a total sample size of 1845 was required. The sampling process of the population was multi-staged. The aim was to include at least 60 participants from each community, with a similar number of participants across gender, residence, and region. China’s mainland is classified into three geographic areas: eastern, central, and western (Figure 1). Of the 11 eastern region provinces, 8 central region provinces, and 12 western region provinces (autonomous regions, municipalities), we selected three provinces each: Shandong, Zhejiang, and Hainan; Shanxi, Anhui, and Hunan; and Gansu, Guizhou, and Guangxi, respectively. From the nine provinces selected, we chose four representative cities each. We sampled one community each, per city and county, to obtain at least 60 questionnaires from each community (Supplementary Figure 1). In the selection process, we ensured that the populations selected from the three regions were similar according to their economic, educational, and other background characteristics. Table 1 shows the study sampling results for each province. From the eastern/central/western regions, we received 620/658/622 questionnaires, respectively, and approximately 196–235 questionnaires for each province.
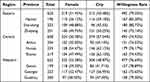 |
Table 1 Participants’ Willingness Rate Overall, and by Region, Province, Gender, and City |
 |
Figure 1 Cluster sampling of participants in the eastern/central/western region provinces of China. Blue circles highlight selected provinces from each region. Map source: NWCCW, NBS, UNICEF, Children in China: An Atlas of Social Indicators, 2018, available at: https://www.unicef.cn/en/chapter-1-population-demographics [accessed 13 December 2022]. |
Questionnaire Design
The questionnaire was designed to obtain information on individuals’ willingness to undergo gastroscopy for GC screening and determine the influencing factors (see Supplementary Material). Experts from the Xiangya College of Public Health and Department of Gastroenterology of the Third Xiangya Hospital jointly developed the questionnaire. The questionnaire had four main sections: 1) demographic characteristics, whether there were high-risk factors for GC, whether respondents agreed to the use of their questionnaire responses for this research; 2) willingness to undergo gastroscopy by the public, when informed of the need and necessity; 3) reasons for rejecting and willingness to undergo gastroscopy screening, after a change of mind; and 4) individuals’ awareness of risks, benefits, fears, and familiarity with gastroscopy and other life events.20,21 The high-risk groups included participants over 40 years old with any other high-risk factors, such as H. pylori infection, precancerous lesions, first-degree relatives with GC, high salt intake, pickled diet, smoking, and heavy drinking.22–24 The American Cancer Society and Chinese Anti-Cancer Association determined the risk factors included in our questionnaire.22
Before the participants completed the questionnaire, investigators explained what constituted the precancerous stomach lesions, such as chronic atrophic gastritis, gastric ulcer, gastric polyps, postoperative residual stomach, hypertrophic gastritis, and malignant anemia. A family history of GC was defined as having parents, children, or siblings with GC. Neither the participants nor public were involved in our research design, conduct, reporting, or dissemination plans.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki. The Ethics Committee of the Third Xiangya Hospital, Central South University, approved this study (the Institutional Review Board of the Third Xiangya Hospital, Central South University, approval no. I 21018). All study participants provided informed consent.
Data Collection
Due to the strict prevention and control of COVID-19, our research could not be conducted in-person; therefore, we decided to conduct it over the telephone. Trained investigators approached community residents by phone, and community administrators provided personal contact information. People who had difficulty understanding the questions completed the questionnaire with the help of their families. Investigators were trained to obtain accurate information. This study’s research committee managed all the questionnaires, while two data collectors entered the data in the database. To maximize the response rate, each participant received a telephone allowance worth ¥20 (approximately US $3).
Data Analysis
All data were analyzed using R software (version 4.0.2). Count data were described using numbers and percentages, and sample rates were compared using univariate analysis of variance. Variables with a P<0.20 in the univariate analysis were entered into the multivariate logistic regression analysis, which excluded the influence of other factors and explored the predictors. By using the P<0.20 standard, we also included region and precancerous stomach lesions as variables. P<0.05 was considered statistically significant.
Results
Sociodemographic Characteristics of the Participants
Among 2160 individuals who received the questionnaire, 1900 (87.96%) questionnaires were considered fully completed; this was more than the minimum sample size required. Among the 1900 participants, there were 51.2% (n=985) females and 48.2% (n=915) males. The average age was 50.5 years (standard deviation, 8.39). Of 1900 participants, 991 (52.2%) lived in urban areas, 312 (16.4%) had H. pylori infection, 239 (12.6%) had gastric precancerous lesions, 124 (6.5%) reported a family history of GC, and 273 (14.4%) had high-risk lifestyles for GC (Table 2).
 |
Table 2 Participants’ Sociodemographic Characteristics and Univariate Analysis Results According to Their Willingness or Unwillingness to Undergo Gastroscopy |
Willingness to Undergo Gastroscopy for GC Screening and Predictors
Among 1900 participants, 1462 (76.95%) were willing to undergo gastroscopy for GC screening. The univariate analysis indicated that five factors were significantly correlated with a higher likelihood of willingness to undergo gastroscopy: younger age, living in an urban area, higher education level, higher income, and H. pylori infection (Table 2). Multivariate logistic regression analysis results showed that six factors, including income, were significantly associated with willingness to undergo gastroscopy. Older individuals aged 50–59 years (odds ratio [OR] 0.77, 95% confidence interval [CI] 0.60–0.99, P=0.044) and >60 years (OR 0.56, 95% CI 0.40–0.78, P=0.001) compared to those aged 40–49 years, and individuals living in rural areas compared to urban areas (OR 0.79, 95% CI 0.63–0.99, P=0.043) were less willing to undergo gastroscopy. The higher the educational level of participants, the greater their willingness to undergo gastroscopy (OR 1.87, 95% CI 1.32–2.67, P<0.001). Individuals from the eastern region were more willing to undergo gastroscopy than those from the western region (OR 1.34, 95% CI 1.01–1.78, P=0.046). Individuals with H. pylori infection (OR 1.47, 95% CI 1.07–2.04, P=0.019) and precancerous lesions of the stomach (OR 1.48, 95% CI 1.04–2.15, P=0.032) were more willing to undergo gastroscopy (Figure 2).
Reasons for the Unwillingness to Undergo Gastroscopy Screening
In this study, 438 (23.1%) participants were unwilling to undergo gastroscopy. Individuals usually had seven reasons for rejecting gastroscopy. The top four reasons were fear of pain or discomfort (68.49%), worry about a possible devastating test result (39.73%), no symptoms in self-feeling (31.28%), and concern about the high expense (27.63%). The least frequent reason was a concern about privacy (Figure 3).
 |
Figure 3 Reasons for refusing gastroscopy for GC screening. Abbreviation: GC, gastric cancer. |
Reasons Why a Decision to Reject Gastroscopy Would Be Changed
For 300/438 (68.49%) individuals who rejected gastroscopy due to fear of pain or discomfort, 161 (64.9%) would accept painless gastroscopy. Among 121 (27.63%) participants who refused due to the high expense, 109 (90.8%) were willing to undergo gastroscopy if they had a higher medical reimbursement rate.
Individuals’ Level of Cognition of Gastroscopy
We measured the participants’ cognition of gastroscopy in relation to other everyday life events using a Likert scale. In terms of fear and familiarity, participants believed that they had a relative fear of gastroscopy as it was an unknown life event. Gastroscopy was also the most alarming event of all GC screening methods. Regarding benefits and risks, participants thought that the potential side effects of bleeding, nausea, and low insurance reimbursement were difficult to ignore. However, of all GC screening methods, gastroscopy was considered to have a relatively high risk and relatively low benefit (Figure 4).
 |
Figure 4 Plots showing individuals’ level of cognition of gastroscopy: (A) fear and familiarity; (B) benefits and risks. Blue circles highlight the location of “gastroscopy”. |
Discussion
The disease burden of GC in China is high. Since GC is frequently diagnosed at an advanced stage, its mortality rate is also high.6 Early screening and intervention are the most effective methods to reduce GC mortality. Gastroscopy is a recommended screening method for GC,25 but endoscopic screening compliance is only 18.41% in China. In this study, we carried out a cluster sampling questionnaire survey among individuals over 40 years old to evaluate the willingness and contributing factors for undergoing gastroscopy for GC screening in China in 2020.18 The willingness rate in our study was 76.95% (1462/1900), far higher than the screening rate.
Individuals of younger age, from the eastern region, living in urban areas, with higher education levels, with H. pylori infection, or who had precancerous stomach lesions, had a higher willingness rate to undergo gastroscopy for GC screening. A previous study showed that initial screening at ages 40 to 44 is associated with more health benefits, which may explain the greater willingness among younger individuals to undergo early GC screening.26 On the other hand, older people are more resistant to undergoing gastroscopy, as they are concerned with the possibility of a growing family burden if a significant disease is detected. The economic and education levels of individuals in the eastern region were higher than those of the central and western regions. Furthermore, the eastern region has a higher age-standardized mortality rate and mortality rate than the western and central regions, which may explain its higher willingness rate of gastroscopy.27 A cross-sectional study concluded that individuals with a higher educational level are significantly more likely to have a heightened awareness of colorectal cancer.28 In a meta-analysis, low socioeconomic status was a more significant risk factor than H. pylori for GC.29 Low income may lead to more worries about the high expense of endoscopy, which is the fourth most common reason for rejecting endoscopy in our study. Access to endoscopy might also be influenced by local healthcare systems and the personal cognition level,25 which may explain why people who lived in urban areas had a higher willingness rate of gastroscopy for GC screening. A survey of 3211 members of the public and 546 physicians revealed a lack of awareness and preventive measures for the hazards of H. pylori infection in China,30 which may be a reason why participants were unwilling to undergo gastroscopy for early cancer screening in our study. These results suggest the need for health education of specific groups about the significance of GC screening by healthcare providers.
Fear of pain or discomfort, worry about a possible devastating test result, no symptoms in self-feeling, and concern about high expense were the top reasons why participants rejected gastroscopy. Among 438 participants who refused gastroscopy, 161 would accept painless gastroscopy, and 109 would be willing if they had a higher medical reimbursement rate. A survey reported that 83.8% of people who visited medical centers thought that GC screening was helpful, but only 15.2% underwent the procedure, while 38.1% admitted fear of gastroscopy.21 These findings suggest that appropriate measures should be taken to improve the willingness rate of gastroscopy. For example, patient education may effectively minimize patients’ fear of gastroscopy.9 A cost-effectiveness study showed that the benefit of any screening strategy, including colonoscopy, outweighs the cost of no screening in southern China.31 Using incremental cost-effective ratio analysis, endoscopy was the most cost-effective screening method in high-risk populations, including Japan and Korea.32 Government or insurance companies should consider lowering the price of painless gastroscopy, which can effectively increase the detection rate of early cancer and reduce the burden on the state and society in the long run.33 In addition to painless gastroscopy, an oral contrast agent has been proposed to enhance transabdominal ultrasound.34 To reduce public fear of endoscopy, education of high-risk populations should be strengthened to emphasize the effectiveness of gastroscopic screening for early detection of GC, reduce the economic burden caused by early screening of GC, and minimize the discomfort associated with the examination. These experiences can reference other countries, especially those with a high incidence of GC.
Many studies showed declining screening rates for various cancers during the COVID-19 pandemic.2–4 COVID-19 might have impacted cancer patients because most healthcare facilities focused on treating COVID-19 patients or preventing the spread of COVID-19. This has resulted in a skewed healthcare resource, with cancer patients receiving less attention than before the pandemic. These circumstances may be associated with declines in cancer screening rates. Our study investigated people’s willingness to be screened early for GC during the COVID-19 pandemic; willingness rates were much higher than the actual screening rates reported in other studies, which reflects individuals’ level of anxiety about their health during this period. This was the first study to evaluate the willingness of individuals aged over 40 years in the general population of China to undergo gastroscopy for GC screening.
Nevertheless, this study has some limitations. First, a self-reported questionnaire survey can not exclude retrospective bias. However, our investigators were trained to obtain accurate information and offered an allowance to participants to enhance their motivation and engagement. Second, the sample size in our study was inadequate due to the COVID-19 epidemic and its prevention and control measures. Additional regions and larger sample sizes should be included in future studies. Third, sociocultural factors, such as traditions or beliefs, that possibly relate to screening decisions were not studied. A more comprehensive and structured survey should be conducted to evaluate the real-time improvement in people’s level of knowledge, willingness rate, and actual participation rate of gastroscopy for GC screening in the future.
Conclusion
Overall, 76.95% of people aged over 40 years were willing to undergo gastroscopy for GC screening in China during the COVID-19 pandemic in 2020. People who were infected with H. pylori were more willing to undergo gastroscopy for GC screening. Thus, physicians are reminded to suggest a H. pylori test for people aged over 40 years. Older individuals and those with lower educational levels and living in rural areas are more likely to reject gastroscopy; this indicates the need to improve GC screening for older individuals and those in rural areas. The government should consider providing a partial medical insurance reimbursement for painless gastroscopies in outpatient clinics for people over 40 years of age. Due to its unpredictable outcome, the Chinese tend to have a hesitant and fearful attitude. They also have a tendency towards fear because of the adverse effects of gastroscopy. Considering the above rejection reasons for gastroscopy and the significant implication for GC prognosis, decision makers should emphasize the importance of public education on the high necessity for gastroscopy and the safety of GC screening.
Data Sharing Statement
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The National Natural Science Foundation of China (81970494); Key Project of Research and Development Plan of Hunan Province (2019SK2041).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi:10.23750/abm.v91i1.9397
2. Feletto E, Grogan P, Nickson C, Smith M, Canfell K. How has COVID-19 impacted cancer screening? Adaptation of services and the future outlook in Australia. Public Health Res Pract. 2020;30(4):3042026. doi:10.17061/phrp3042026
3. Kuzuu K, Misawa N, Ashikari K, et al. Gastrointestinal cancer stage at diagnosis before and during the COVID-19 pandemic in Japan. JAMA Netw Open. 2021;4(9):e2126334. doi:10.1001/jamanetworkopen.2021.26334
4. Park H, Seo SH, Park JH, Yoo SH, Keam B, Shin A. The impact of COVID-19 on screening for colorectal, gastric, breast, and cervical cancer in Korea. Epidemiol Health. 2022;44:e2022053. doi:10.4178/epih.e2022053
5. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
6. He Y, Wang Y, Luan F, et al. Chinese and global burdens of gastric cancer from 1990 to 2019. Cancer Med. 2021;10(10):3461–3473. doi:10.1002/cam4.3892
7. Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J. 2021;134(7):783–791. doi:10.1097/CM9.0000000000001474
8. Pasechnikov V, Chukov S, Fedorov E, Kikuste I, Leja M. Gastric cancer: prevention, screening and early diagnosis. World J Gastroenterol. 2014;20(38):13842–13862. doi:10.3748/wjg.v20.i38.13842
9. Zong L, Abe M, Seto Y, Ji J. The challenge of screening for early gastric cancer in China. Lancet. 2016;388(10060):2606. doi:10.1016/S0140-6736(16)32226-7
10. Kim H, Hwang Y, Sung H, et al. Effectiveness of gastric cancer screening on gastric cancer incidence and mortality in a community-based prospective cohort. Cancer Res Treat. 2018;50(2):582–589. doi:10.4143/crt.2017.048
11. Evans JA, Chandrasekhara V, Chathadi KV, et al.; ASGE Standards of Practice Committee. The role of endoscopy in the management of premalignant and malignant conditions of the stomach. Gastrointest Endosc. 2015;82(1):1–8. doi:10.1016/j.gie.2015.03.1967
12. Endoscopy C, Endoscopy C. Chinese consensus on screening and endoscopic diagnosis and management of early gastric cancer (Changsha, April 2014). Chin J Gastroenterol. 2014;19:408–427. doi:10.3969/j.issn.1008-7125.2014.07.006
13. He J, Chen WQ, Li ZS, et al. 中国胃癌筛查与早诊早治指南(2022, 北京)[China guideline for the screening, early detection and early treatment of gastric cancer (2022, Beijing)]. Zhonghua Zhong Liu Za Zhi. 2022;44(7):634–666. Chinese. doi:10.3760/cma.j.cn112152-20220617-00430
14. Asaka M, Mabe K. Strategies for eliminating death from gastric cancer in Japan. Proc Jpn Acad Ser B Phys Biol Sci. 2014;90(7):251–258. doi:10.2183/pjab.90.251
15. Elmunzer BJ, Singal AG, Sussman JB, et al. Comparing the effectiveness of competing tests for reducing colorectal cancer mortality: a network meta-analysis. Gastrointest Endosc. 2015;81(3):700–709.e3. doi:10.1016/j.gie.2014.10.033
16. Fukao A, Tsubono Y, Tsuji I, HIsamichi S, Sugahara N, Takano A. The evaluation of screening for gastric cancer in Miyagi Prefecture, Japan: a population-based case-control study. Int J Cancer. 1995;60(1):45–48. doi:10.1002/ijc.2910600106
17. Chen Q, Yu L, Hao CQ, et al. Effectiveness of endoscopic gastric cancer screening in a rural area of Linzhou, China: results from a case-control study. Cancer Med. 2016;5(9):2615–2622. doi:10.1002/cam4.812
18. Guo L, Zhang S, Liu S, et al. Determinants of participation and detection rate of upper gastrointestinal cancer from population-based screening program in China. Cancer Med. 2019;8(16):7098–7107. doi:10.1002/cam4.2578
19. Hajian-Tilaki K. Sample size estimation in epidemiologic studies. Caspian J Intern Med. 2011;2(4):289–298.
20. Koliani-Pace JL, Haron AM, Zisman-Ilani Y, Thompson KD, Siegel CA. Patients’ perceive biologics to be riskier and more dreadful than other IBD medications. Inflamm Bowel Dis. 2020;26(1):141–146. doi:10.1093/ibd/izz121
21. Liu Q, Zeng X, Wang W, et al. Awareness of risk factors and warning symptoms and attitude towards gastric cancer screening among the general public in China: a cross-sectional study. BMJ Open. 2019;9(7):e029638. doi:10.1136/bmjopen-2019-029638
22. Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014;23(5):700–713. doi:10.1158/1055-9965.EPI-13-1057
23. Eslick GD, Lim LL, Byles JE, Xia HH, Talley NJ. Association of Helicobacter pylori infection with gastric carcinoma: a meta-analysis. Am J Gastroenterol. 1999;94(9):2373–2379. doi:10.1111/j.1572-0241.1999.01360.x
24. Poorolajal J, Moradi L, Mohammadi Y, Cheraghi Z, Gohari-Ensaf F. Risk factors for stomach cancer: a systematic review and meta-analysis. Epidemiol Health. 2020;42:e2020004. doi:10.4178/epih.e2020004
25. Veitch AM, Uedo N, Yao K, East JE. Optimizing early upper gastrointestinal cancer detection at endoscopy. Nat Rev Gastroenterol Hepatol. 2015;12(11):660–667. doi:10.1038/nrgastro.2015.128
26. Xia R, Zeng H, Liu W, et al. Estimated cost-effectiveness of endoscopic screening for upper gastrointestinal tract cancer in high-risk areas in China. JAMA Netw Open. 2021;4(8):e2121403. doi:10.1001/jamanetworkopen.2021.21403
27. Liu Y, Wang W, Liu J, et al. Cancer Mortality — china, 2018. CCDCW. 2020;2(5):63–68. doi:10.46234/ccdcw2020.019
28. Salimzadeh H, Bishehsari F, Delavari A, et al. Cancer risk awareness and screening uptake in individuals at higher risk for colon cancer: a cross-sectional study. BMJ Open. 2016;6(12):e013833. doi:10.1136/bmjopen-2016-013833
29. Yaghoobi M, McNabb-Baltar J, Bijarchi R, Hunt RH. What is the quantitative risk of gastric cancer in the first-degree relatives of patients? A meta-analysis. World J Gastroenterol. 2017;23(13):2435–2442. doi:10.3748/wjg.v23.i13.2435
30. Wu Y, Su T, Zhou X, Lu N, Li Z, Du Y. Awareness and attitudes regarding Helicobacter pylori infection in Chinese physicians and public population: a national cross-sectional survey. Helicobacter. 2020;25(4):e12705. doi:10.1111/hel.12705
31. Zhou Q, Li HL, Li Y, et al. Cost-effectiveness analysis of different screening strategies for colorectal cancer in Guangzhou, southern China: a Markov simulation analysis based on natural community screening results. BMJ Open. 2021;11(9):e049581. doi:10.1136/bmjopen-2021-049581
32. Choi KS, Suh M. Screening for gastric cancer: the usefulness of endoscopy. Clin Endosc. 2014;47(6):490–496. doi:10.5946/ce.2014.47.6.490
33. Suzuki H, Gotoda T, Sasako M, Saito D. Detection of early gastric cancer: misunderstanding the role of mass screening. Gastric Cancer. 2006;9(4):315–319. doi:10.1007/s10120-006-0399-y
34. Shen L, Zhang D, Huang Y, et al. Initial screening of gastric cancer using oral contrast-enhanced trans-abdominal ultrasonography in rural asymptomatic individuals. Cancer Epidemiol. 2022;80:102236. doi:10.1016/j.canep.2022.102236
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

