Back to Journals » Advances in Medical Education and Practice » Volume 13
Willingness to Select Initial Clinical Training Hospitals Among Medical Students at a Rural University in Japan: A Single-Center Cross-Sectional Study
Authors Yamashita S , Tago M , Tokushima M, Emura S, Yamashita SI
Received 16 May 2022
Accepted for publication 31 August 2022
Published 19 September 2022 Volume 2022:13 Pages 1081—1089
DOI https://doi.org/10.2147/AMEP.S374852
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Shun Yamashita,1 Masaki Tago,1 Midori Tokushima,2 Sei Emura,2 Shu-Ichi Yamashita1
1Department of General Medicine, Saga University Hospital, Saga, Japan; 2Saga Medical Career Support Center, Saga University Hospital, Saga, Japan
Correspondence: Shun Yamashita, Department of General Medicine, Saga University Hospital, 5-1-1 Nabeshima, Saga, 849-8501, Japan, Tel +81952343238, Fax +81952342029, Email [email protected]
Purpose: Many countries will be aged societies by 2060. As a super-aged society, Japan may offer a valuable reference point. The number of medical residents and doctors working at university hospitals in Japan has halved since 2004, resulting in serious shortages of doctors in rural areas. This study clarified factors influencing medical students to choose university hospitals as facilities for their initial training or to only choose community hospitals.
Methods: This single-center cross-sectional study was conducted in a typical rural city in Japan from February to March 2021. Data were collected using a questionnaire developed from a narrative review and discussion among four researchers. The participants were divided into those who chose university hospitals and those chose only community hospitals for logistic regression analysis.
Results: Of the 300 students who answered the questionnaire (46.4% response rate), 291 agreed to participate in the study. At the time, 93 students had not decided where to undertake initial training, and were excluded. Of the 198 analyzed students, 113 (57.1%) had chosen university hospitals. Significant factors affecting students’ choices were “good salary or fringe benefits” (odds ratio [OR] 2.6, 95% confidence interval [CI]: 1.3– 5.2) in the community hospital group, and “desire to have contact with doctors practicing in a medical setting before starting hospital training in the fifth and sixth grade” (OR 0.4, 95% CI: 0.2– 0.8) and “prefer Saga Prefecture for initial training” (OR 0.2, 95% CI: 0.1– 0.4) among the university hospital group.
Conclusion: University hospitals could offer a good salary or fringe benefits to secure residents. Other useful measures include preferential admission of students who pledge to work in the prefecture of their medical school after graduation and facilitating contact between motivated students and senior doctors before starting hospital training.
Keywords: medical student, initial clinical training, university hospital, community hospital, questionnaire, cross-sectional study
Introduction
Various countries, including developing countries, have rapidly aging populations and declining birth rates, meaning they will become aged societies by 2060.1 Among these countries, Japan is an unparalleled super-aged society.1 Through systems such as universal health insurance coverage, Japan has made efforts to address various problems caused by the aged population.2 These efforts could provide valuable reference information for other aging or aged countries. The shortage of medical doctors in rural areas is an important problem in aged societies, including Japan and many other countries. Therefore, this study aimed to investigate how to secure medical residents, especially in rural areas, in Japan with its large population of aged people. Our findings may have value for other countries wishing to address the shortage of medical doctors.
Before 2004, many medical students in Japan chose to enter a clinical department in their university following graduation and received their initial and subsequent clinical training at either the university hospital or other affiliated hospitals.3 To secure their staffing, most rural community hospitals in Japan successfully depended on temporary assignment of medical doctors, including residents from university hospitals. However, since the start of Postgraduate Medical Education (PGME) Program in 2004, medical residents are obliged to receive mandatory initial clinical training for 2 years after graduating from their university.4 The change in the system allowed medical students to apply to any hospitals in Japan that met criteria set by the Ministry of Health, Labour and Welfare (including university hospitals and community educational hospitals) for their initial clinical training. As a result, many medical students work as medical residents at community educational hospitals, which are mainly in urban areas.5 The ratio of graduates from rural universities who worked as residents at their own university hospitals decreased by half5–8 and the number of medical doctors who worked at the hospital affiliated to their university after their initial clinical training markedly decreased.6,8,9 Many rural community hospitals remain dependent on the assignment of medical doctors from university hospitals. The decrease in the number of medical doctors working at university hospitals impaired these hospitals’ ability to assign medical doctors, resulting in a serious shortage of them at community hospitals in rural areas. To overcome this situation, and maintain the rural community healthcare system, many universities in rural areas introduced regional quota programs giving priority of admission to students from the university’s “home” prefecture. Students had to pledge to work for a certain period in the prefecture of the medical school to which they applied after graduation, usually around 9 years.10 However, even the introduction of this promising system failed to rectify the uneven distribution of doctors between urban and rural areas.10,11 A new medical training system for doctors to be certified as specialists after completing their initial 2-year residency was introduced in 2018, and has reportedly worsened the situation.12 To maintain the system of community healthcare in rural areas in the future, and especially to secure enough medical doctors, it is essential to ensure that as many medical residents as possible are at university hospitals in rural areas.
Several cohort studies have examined the characteristics of hospitals that strongly attracted medical students. However, the results were not necessarily consistent.13,14 The marked differences between the roles of university hospitals in rural prefectures having only one university hospital and urban prefectures with several university hospitals could significantly influence the reasons for medical students to choose particular hospitals for their initial clinical training. The reasons why medical students select either a university hospital or a community educational hospital for their initial clinical training could therefore vary greatly from region to region.
This study involved a questionnaire survey that targeted all current medical students at Saga University, a typical rural university in Japan, and was designed to clarify factors influencing students’ decisions to include a university hospital as a facility for their initial clinical training, or to only choose community educational hospitals.
Materials and Methods
Study Design and Participants
This study was a subgroup analysis of data from a previous study about factors influencing whether medical students at a rural university in Japan chose the prefecture in which the university was located for their initial clinical training.15 Therefore, this study was a single-center cross-sectional study using a questionnaire method. The study population was all 647 medical students enrolled in the Saga University Medical School in February and March 2021. Those who did not respond to the questionnaire, did not agree to participate in the study, or had not decided where to do their initial clinical training were excluded from the analysis. The remaining students were divided into two groups: those who preferred including university hospitals as one of the facilities for their initial clinical training (UH group) and those who preferred only choosing community educational hospitals (CH group).
Setting
Saga Prefecture is a typical rural prefecture with a population of approximately 830,000, located in northwestern Kyushu (one of the main islands in southern Japan). Saga University, the study location, is the only national university with a medical school in Saga Prefecture. The prefecture only gained one medical doctor between 2016 and 2018, which was the second lowest of all the prefectures in Japan, following Okinawa Prefecture.16 The number of medical residents in Saga Prefecture in 2020 was 74.9% of the intake quota allocated by the Ministry of Health, Labour and Welfare, Japan, ranking Saga 31st among the 47 prefectures in Japan.17 The intake at Saga University Hospitals was only 53.8% of the quota, ranking 57th among 81 major university hospitals in Japan included in the recruiting system for medical residents, the “Matching System”.18
Data Sources
This study used a questionnaire method. The questionnaire was disseminated via email. An outline of this study was presented at the beginning of the questionnaire, and students were required to decide whether to participate in this study. Only those who agreed to participate could access the survey items. The items included in the questionnaire were determined following discussion of the results of a narrative literature review by four researchers: one medical student and three physicians engaged in teaching students at the medical school of Saga University. The questionnaire was created using Google Forms, and sent via email to all students enrolled in the medical school by the university’s Student Affairs Division in February 2021. The questionnaire was also sent via a social networking service (SNS) allocated to students in each grade and set up by the student union. Students subsequently received two remainders via the same SNS 2 and 3 weeks later. General survey items included: age; gender; students’ parents’ occupations; whether the students had relatives, acquaintances, or friends living in Saga Prefecture since before admission; whether they had a partner or spouse; whether they had been admitted on recommendation by their high school; whether they had been admitted through a regional quota program system; experience of repeating a school year; current university grade; home region; and future clinical department. Other questionnaire items included: preferred location for initial clinical training; preferred hospital type for initial clinical training; reasons for selecting hospitals for initial clinical training; satisfaction with university life; satisfaction with classroom lectures or practical training (for first to fourth grade students); satisfaction with hospital training (for fifth and sixth grade students); encounters with doctors during hospital training who they perceived as role models (for fifth and sixth grade students); and study morale. Definitions of these general survey items and questionnaire items are provided in Supplementary File 1 and Supplementary File 2, respectively.
Data Analysis
Continuous variables were expressed as median and interquartile range and compared using the Mann–Whitney U-test. Categorical variables were expressed as percentages and compared using the χ2 test. Missing data were excluded from the univariate and multivariate analyses. As a result of collinearity, candidate variables were selected that showed p < 0.1 with univariate analysis and a low correlation coefficient. When there was a Spearman’s r value > 0.7 or a Kendall coefficient r value > 0.7 between two items, one item was selected, and the other was removed. Logistic regression analysis was performed on the selected candidate variables to estimate the significant factors for the UH and CH groups and calculate their odds ratio. Statistical significance was set at p < 0.05. SPSS Statistics (version 25; IBM Corp., Armonk, NY, USA) was used for statistical analysis. The sample size for this study was calculated to be 70 (35 for each group) using a significance level of 95% and statistical power of 80%, which was based on a 2008 study reporting the satisfaction with their salary of medical residents in their second year of working at university hospitals or community educational hospitals.19
Sample Size
We calculated a required sample size of 50 participants for each group based on an alpha error of 0.05, beta error of 0.20, and an effect size of 0.24. These were estimated on the basis of the results of a previous study exploring the difference in medical residents’ satisfaction with their salaries at university and community hospitals.19
Results
Enrolment and Assignment of Research Subjects
From February to March 2021, 647 students (of whom 359 were men) were enrolled in the medical school and 300 responded to the questionnaire (46.4% response rate). Of these, 291 agreed to participate in the study. In total, 93 students had not decided on the location for their initial clinical training at the time of the study, leaving 198 responses for analysis. The UH group included 113 students (57.1%) and the CH group 85 students (42.9%) (Figure 1).
Reliability Analysis
The internal consistency of our questionnaire was assessed using Cronbach’s α coefficient, which showed an acceptable value of 0.617.
Univariate Analysis
The characteristics of the students are shown in Table 1. Six students did not respond to the question regarding their gender. The UH group had a higher percentage of students admitted through a regional quota program (34% vs 19%, p = 0.021) than the CH group. No significant differences were found between the two groups in age; gender; parents’ occupation; presence of relatives, acquaintances, or friends living in Saga Prefecture since before admission; presence of a partner or spouse; admission on recommendation by their high school; experience of repeating a school year; current grade; or home region.
 |
Table 1 Participant Characteristics |
The reasons for preferring particular places for initial clinical training and choice of future specialty are shown in Table 2. The CH group were more likely than the UH group to cite desire to work in an urban area (10% vs 20%, p = 0.040); good salary or fringe benefits (19% vs 40%, p = 0.001); extensive experience with common diseases (29% vs 49%, p = 0.004); and influence of senior students (7% vs 19%, p = 0.012). The UH group had a higher percentage of students who expressed (or thought) that Saga Prefecture was their first choice for initial clinical training (73% vs 21%, p < 0.001). No significant difference in future specialties was observed between the two groups.
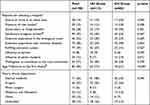 |
Table 2 Participants’ Reasons for Selecting Particular Hospitals for Initial Clinical Training, and Their Future Clinical Department |
The results on the students’ satisfaction with university life and their study morale are shown in Table 3. The CH group showed higher satisfaction with university life (8 vs 8, p = 0.029). No significant differences were found between the two groups in satisfaction with classroom lectures or practical training for first to fourth grade students, or satisfaction with hospital training for fifth and sixth grade students. There were also no significant differences between the two groups for the questionnaire items on study morale: desire to have contact with doctors practicing in a medical setting before starting hospital training in the fifth and sixth grade; desire to engage in medical research and write medical articles while a medical student; and desire to treat many patients during hospital training.
 |
Table 3 Student Satisfaction and Study Motivation |
Multivariate Analysis
The results of the multivariate logistic regression analysis are shown in Table 4. The only significant factor for the CH group was “good salary or fringe benefits” (odds ratio (OR) 2.6, 95% confidence interval [CI]: 1.3–5.2). The significant factors for the UH group were “desire to have contact with doctors practicing in a medical setting before starting hospital training in the fifth and sixth grade” (OR 0.4, 95% CI: 0.2–0.8) and “Saga Prefecture as the first choice for initial clinical training” (OR 0.2, 95% CI: 0.1–0.4).
 |
Table 4 Results of Multivariate Logistic Regression Analysis with a Backward Selection Method |
Discussion
Many countries could implement measures to address problems associated with the aging of society with reference to efforts that have been made in Japan, which is already the most super-aged and further aging society.1 Because the shortage of medical doctors in rural areas is an important problem for aged societies, our investigation of ways to secure the required number of medical residents, especially in rural areas in Japan, may be helpful for other aged countries. Since the start of the PGME Program for medical residents in Japan in 2004, the number of medical residents at university hospitals in the rural areas from which they were graduated halved.5–8 This led to a decrease in the number of medical doctors at rural university hospitals, which resulted in shortages at community educational and leading hospitals in rural areas. Therefore, it is essential to secure sufficient medical residents at university hospitals in rural areas. However, previous cohort studies that examined characteristics of hospitals that attracted medical students showed inconsistent results.13,14 Because studies on medical residents’ preferences for hospitals should be conducted on a regional basis, we conducted this study among medical students at Saga University in Saga Prefecture, which is a typical rural prefecture in Japan. We found that good salary or fringe benefits were significant for the CH group. However, those choosing university hospitals were influenced by wanting contact with doctors practicing in a medical setting before starting hospital training in the fifth and sixth grade and Saga Prefecture being their first choice for initial clinical training. Addressing these factors may be effective in Japan and in other aged countries, which also face problems such as shortages of medical doctors in their rural areas.
There have been two conflicting reports about the importance of salary and fringe benefits. One reported that financial incentives were a factor influencing medical students to select community educational hospitals for initial clinical training.13 The other found that financial incentives failed to attract medical students.14 Both results were obtained from nationwide surveys conducted by the Japan Residency Matching Program, when medical students in the sixth grade determined the hospitals for their initial clinical training. However, inconsistent survey periods or analytical methods might have caused these conflicting results.14 Regional characteristics such as whether the university is located in an urban or rural area, or whether the university hospital is the only one in the prefecture could also have affected the results. Our multivariate analysis showed that “good salary or fringe benefits” were significantly related to the selection of community educational hospitals for initial clinical training, but students’ choice of medical specialty was not. This could be because most medical students in Saga University were from rural areas. In Japan, the average income of people living in rural areas is less than that of those living in urban areas.20 For medical students in a typical rural area with lower income, good salary or fringe benefits might therefore be an attractive and significant factor in choosing the location of their initial clinical training.
We found that the desire to have contact with doctors practicing in a medical setting before starting hospital training in the fifth and sixth grade was a significant factor for the UH group. A previous study found that lower opportunities for contact with attending physicians could decrease the level of satisfaction of students, and that involvement of enthusiastic attending physicians or having many opportunities to practice physical examinations might increase student satisfaction.21 Providing medical residents or students with opportunities to participate in workshops on clinical training has also been found to increase their clinical capability and satisfaction, making hospitals preferable as an institution of initial clinical training.14,22 It is therefore clear that the quality of coaching from physicians is a significant factor in determining the satisfaction of medical residents or students. It is easy to imagine that medical students who want to have contact with physicians as early as possible, especially before starting hospital training in the fifth and sixth grade, might be more motivated about their initial clinical training. To encourage these students and maintain their high levels of morale, supervisory doctors need to find ways to contact medical students before they start their hospital training in the fifth and sixth grade.
It is commonly believed that university hospitals in Japan put a higher value on medical research. This is of course one of their primary missions, but this tendency could make it appear more difficult for them to provide medical students and residents with adequate quality and quantity of training in primary care and general healthcare.14 This belief might therefore lead to fewer medical residents at university hospitals. The ratio of medical residents working at hospitals affiliated to the university from which they graduated is significantly less than those at community educational hospitals.23 However, this study found that “Saga Prefecture as the first choice for initial clinical training” was significant for the UH group. This might suggest that medical students who want to work as residents in Saga Prefecture also want to do their initial clinical training at Saga University Hospital, the only university hospital in the prefecture. One of the major characteristics of Saga University Hospital is the established presence of the department of General Medicine, which could provide opportunities for training on basic clinical skills about primary care, even in an advanced care hospital. Our study did not include a question about the presence of a department of general medicine as one of the reasons of selecting a hospital for initial clinical training. However, this could have influenced the decisions of medical students who wanted to receive their initial clinical training in Saga Prefecture.
This study had some limitations. It was a cross-sectional study. It included medical students across all grades, but students may change their opinions during the course of their studies. It may therefore be helpful to repeat the survey among the same students as they progress. Additionally, 32.0% of respondents were excluded from the analysis because they had not decided on the location of their training. The results could therefore have changed depending on those students’ decisions. Finally, because we did not perform validation of this questionnaire by repetition of examination, the reproducibility of this questionnaire is yet to be determined.
Conclusion
It is important to offer a good salary or fringe benefits to medical residents. Other ways to secure enough medical residents at university hospitals may include adopting a preferential admission system for students who apply on the regional quota program pledging to work in the prefecture of their medical school following graduation, or encouraging motivated medical students to have contact with senior doctors before hospital training. The results of this study may be helpful for other aged countries that face shortages of medical doctors.
Abbreviations
OR, Odds ratio; PGME, Postgraduate medical education; SNS, Social networking service.
Data Sharing Statement
The datasets generated during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the ethics committee of the medical school of Saga University (Approval No. R2-37). The content of the study was disclosed on the website of the faculty. Informed consent was provided individually for each student at the beginning of the questionnaire; only students who agreed to participate this study were included in the analysis. This study conformed to the 1975 Declaration of Helsinki and the rule on Medical Ethics of the Faculty of Medicine.
Acknowledgments
This study was supported by Takaho Nakahashi, Fumi Sakai, Ayumi Nakagawa, Sumika Uno, Yoko Miyazaki, and Seira Nagashima, students of the Faculty of Medicine, Saga University. Megumi Hara, MD, PhD, from the department of Public Health at the medical school at Saga University, advised us about choosing suitable items for the questionnaire. We thank Melissa Leffler, MBA, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Masaki Tago is supported by grants from Japan Society for the Promotion of Science, JSPS KAKENHI Grant Number JP21H03166. Other authors declared no conflict of interest.
References
1. United Nations, Department of Economic and Social Affairs, Population Division 2019. World population prospects 2019: highlights. Available from: https://population.un.org/wpp/publications/files/wpp2019_highlights.pdf.
2. Ministry of Health, Labour and Welfare. Overview of medical service regime in Japan [Web site]. Available from: https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01_eng.pdf.
3. Koike S, Kodama T, Matsumoto S, Ide H, Yasunaga H, Imamura T. Residency hospital type and career paths in Japan: an analysis of physician registration cohorts. Med Teach. 2010;32(6):e239–47. doi:10.3109/01421591003695311
4. Matsumoto M, Kashima S, Owaki T, et al. Geographic distribution of regional quota program graduates of Japanese medical schools: a nationwide cohort study. Acad Med. 2019;94(8):1244–1252. doi:10.1097/ACM.0000000000002688
5. Sakai R, Tamura H, Goto R, et al. Evaluating the effect of Japan’s 2004 postgraduate training programme on the spatial distribution of physicians. Hum Resour Health. 2015;13(1):5. doi:10.1186/1478-4491-13-5
6. Fujimoto S. New early clinical resident training system and change of selection of future specialty: from the results of the analysis of a questionnaire for our students and graduates. J Nara Med Assoc. 2013;64:95–99.
7. Toyabe S. Trend in geographic distribution of physicians in Japan. Int J Equity Health. 2009;8(1):5. doi:10.1186/1475-9276-8-5
8. Tanihara S, Kobayashi Y, Une H, et al. Urbanization and physician maldistribution: a longitudinal study in Japan. BMC Health Serv Res. 2011;11(1):260. doi:10.1186/1472-6963-11-260
9. Sakai R, Wang W, Yamaguchi N, Tamura H, Goto R, Kawachi I. The impact of Japan’s 2004 postgraduate training program on intra-prefectural distribution of pediatricians in Japan. PLoS One. 2013;8(10):e77045. doi:10.1371/journal.pone.0077045
10. Matsumoto M, Inoue K, Takeuchi K. Quality of care in Japan: an additional strategy. Lancet. 2011;378(9807):e17. doi:10.1016/S0140-6736(11)61841-2
11. Yamamoto K, Ozaki A, Takita M, et al. Negative aspects of the regional quota system in Japan. JMA J. 2019;2(1):85–86.
12. Saito H, Tanimoto T, Kami M, et al. New physician specialty training system impact on distribution of trainees in Japan. Public Health. 2020;182:143–150. doi:10.1016/j.puhe.2020.02.008
13. Enari T, Hashimoto H. Does salary affect the choice of residency in non-university teaching hospitals? A panel analysis of Japan Residency Matching Programme data. Hum Resour Health. 2013;11(1):12. doi:10.1186/1478-4491-11-12
14. Nishizaki Y, Ueda R, Shinozaki T, Tokuda Y. Hospital characteristics preferred by medical students for their residency programs: a nationwide matching data analysis. J Gen Fam Med. 2020;21(6):242–247. doi:10.1002/jgf2.370
15. Miyazaki Y, Yamashita S, Tago M, Tokushima M, Emura S, Yamashita SI. Reasons for medical students selecting a rural prefecture in Japan for initial clinical training: a single-center-based cross-sectional study. J Rural Med. 2022;17(3):118–124. doi:10.2185/jrm.2021-043
16. Ministry of Health, Labour and Welfare. Overview of statistics of Japanese physicians, dentists and pharmacists in 2018. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/index.html. (In Japanese).
17. Ministry of Health, Labour and Welfare. The results of Japan residency matching in 2020. Available from: https://www.mhlw.go.jp/content/10803000/000685779.pdf. (In Japanese).
18. Japan Residency Matching Program. The results of Japan residency matching for each program in 2020. Available from: https://jrmp2.s3-ap-northeast-1.amazonaws.com/koho/2020/2020all-program-kekka.pdf.
19. Nomura K, Yano E, Mizushima S, et al. The shift of residents from university to non-university hospitals in Japan: a survey study. J Gen Intern Med. 2008;23(7):1105–1109. doi:10.1007/s11606-008-0644-7
20. Do SH. Japanese citizens move to rural areas seeking a slower life? Differences between rural and urban areas in subjective well-being. Bio-Based Appl Econ. 2018;7(1):1–17.
21. Okunomiya T, Morimoto T, Nakajima T, Ogura T, Hiraide A. Factors associated with satisfaction of medical students with clinical clerkships. Jpn Soc Med Educ. 2009;40(1):65–71.
22. Brown R, Doonan S, Shellenberger S. Using children as simulated patients in communication training for residents and medical students: a pilot program. Acad Med. 2005;80(12):1114–1120. doi:10.1097/00001888-200512000-00010
23. Kitada M, Chiba T, Ogawa O, Itoh T, Hiraide A. Changes in the career options of medical school graduates after enforcement of the new clinical training system. Jpn Soc Med Educ. 2012;43(2):123–126.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

