Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
Willingness to Pay and Time Trade-off in Thai Patients with Port-Wine Stains
Authors Jantarakolica T, Wanitphakdeedecha R , Yan C , Yogya Y, Sirisuthivoranunt S , Wongdama S, Phumariyapong P , Sudhipongpracha T
Received 27 July 2022
Accepted for publication 8 September 2022
Published 22 September 2022 Volume 2022:14 Pages 635—642
DOI https://doi.org/10.2147/CEOR.S382735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Tatre Jantarakolica,1 Rungsima Wanitphakdeedecha,2 Chadakan Yan,2 Yuri Yogya,2 Surachet Sirisuthivoranunt,2 Supisara Wongdama,2 Phumithep Phumariyapong,2 Tatchalerm Sudhipongpracha3
1Faculty of Economics, Thammasat University, Bangkok, Thailand; 2Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand; 3College of Interdisciplinary Studies, Thammasat University, Bangkok, Thailand
Correspondence: Rungsima Wanitphakdeedecha, Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Pran-nok Road, Bangkok, 10700, Thailand, Tel +66-2419-4333, Fax +66-2411-9922, Email [email protected]
Background: Port-wine stains are congenital vascular abnormalities that impact children’s and parents’ quality of life (QoL). There are currently no established criteria for assessing the quality of life in PWS patients. Utility measures such as willingness-to-pay (WTP) and time trade-off (TTO) can be used to quantify disease burden, impact on QoL, and assess the cost-effectiveness of interventions.
Methods: This was a cross-sectional questionnaire-based survey study in Thailand from July 2021 to April 2022. The questionnaire included sociodemographic data and preference-based measurement, WTP and TTO. The primary outcome was a WTP and TTO for PWS laser treatment. The subsample analysis for the primary outcome was based on gender (male and female) and age (< 5 years and ≥ 5 years). The household income was measured for time trade-off outcome.
Results: Out of 46 respondents, WTP for the base case at 40% improvement cost 6109.01 baht per visit. Patients were willing to spend their time 9.95 hours per visit for a clinical improvement of 40%. Female was willing to pay and spend more time than male, while those aged≥ 5 years were willing to pay and spend more time than those aged < 5 years. High household income > 100k per month willing to spend less time than lower income groups.
Conclusion: There were obvious correlations between WTP and TTO with clinical outcomes. Utility indicators such as WTP and TTO can be used to measure disease burden, impact on QoL, and assess the cost-effectiveness of interventions. WTP and TTO could provide a more personalized approach to improving QoL, considering each patient’s unique treatment plan and priority. This could help with patient uncertainty and long-term planning strategies to increase the QoL cost-effectively.
Keywords: port-wine stain, time trade-off, willingness to pay
Introduction
Port-wine stain (PWS) or port-wine birthmark is a congenital capillary malformation commonly found in the head and neck. It affects males and females equally, with an incidence of 0.3–0.9% in newborns.1,2 At first, the lesions present as pink or red macules, which do not spontaneously involute and may eventually develop to reddish-purple and become more difficult to treat.3 Patients primarily suffer from aesthetic problems when the lesions are located in the facial area.4 The stigma associated with having a disfiguring facial birthmark can lead to significant negative psychosocial impacts,5,6 disturbing the development of interpersonal and personality relationships.5 Physical appearance is usually considered higher than a person’s character.6 Apart from cosmetic disfigurement, PWS hypertrophy may also impair hearing, sight, nasal breathing, and speech.7
Lasers have been used to treat PWS for over 30 years.8 As demonstrated by its clinical efficacy, the pulsed dye laser (PDL) is the treatment of choice for PWS.9 Shakespeare et al10 evaluated the influence of laser treatment on quality of life (QoL) and found a significant improvement in mental health after treatment. Currently, there is no accepted standard for assessing the QoL in patients with PWS. The evaluation of the QoL is specially indicated for health economic analyzes that are based on three elements: (i) the influence on the quality of, (ii) life the assessment of clinical efficacy, and (iii) short-term and long-term therapy costs.11 QoL Questionnaires and utility indicators such as willingness-to-pay (WTP) and time trade-off (TTO) have been used successfully in patients with chronic skin diseases, such as atopic eczema or psoriasis vulgaris.12
Utility indicators such as WTP and TTO can be used to quantify disease burden and impact on quality of life and analyze the cost-effectiveness of the intervention.13 The utility is the desirability people associate with a particular outcome when faced with uncertainty. The values for specific health state descriptions may come from society or patients.14 WTP is a parameter for the evaluation of the QoL assessed by asking the patients how much money they would be willing to pay for therapy that would be able to relieve their disease. In theory, the greater the patient’s willingness to pay, the greater the disease’s impact on their QoL, and vice versa. The principle of TTO assesses how much a patient is willing to offer from their remaining life expectancy for therapy that would release them from their disease for the rest of their life. The more the patient is willing to give, the greater the disease’s burden and the poorer the patient’s present QoL.4
To the best of our knowledge, this is the first study that assessed the correlation between WTP and TTO for PWS. Using utility measures might help analyze the quality of life-based on the valuations of time and economic status in patients with PWS. This study aims to assess the willingness to pay and time trade-off in patients with port-wine stains to perform laser treatment.
Materials and Methods
In this cross-sectional study, we gathered the information using a questionnaire of PWS patients at a University Hospital in Bangkok, Thailand, from July 2021 to April 2022. The questionnaire had 2 components: sociodemographic data and preference-based measurement; WTP and TTO. The inclusion criteria were all age patients with a clinical diagnosis of facial PWS. The exclusion criteria were patients or parents who were not willing or unable to answer the questionnaire.
The primary outcome of this study was a WTP and TTO for PWS laser treatment. The socio-demographic data, including gender, age, and household income, were analyzed descriptively. The subsample analysis was categorized by age and gender. In addition, the difference in household income was used as a subgroup for the measurement of TTO.
Multivariate analysis using the random effects logit model for the respondents’ decision on discrete choice experiment questions based on different scenarios was employed.
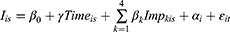
Index function of random effects logistic model can be stated as:
where:  = Decision to treat the patient of respondent i under scenario s, equals to 1 for yes, and 0 otherwise.
= Decision to treat the patient of respondent i under scenario s, equals to 1 for yes, and 0 otherwise.
 = Price for port-wine stain laser treatment for respondent i under scenario s.
= Price for port-wine stain laser treatment for respondent i under scenario s.
 = Number of additional visits to reach k% improvement from the based case of 40% improvement that respondent i faced under scenario s, where k =1 for 60% (=5 visits), 2 for 70% (=5 visits), 3 for 80% (=9 visits), and 4 for 100% (=24 visits).
= Number of additional visits to reach k% improvement from the based case of 40% improvement that respondent i faced under scenario s, where k =1 for 60% (=5 visits), 2 for 70% (=5 visits), 3 for 80% (=9 visits), and 4 for 100% (=24 visits).
 = Cross-sectional random effects of respondent i.
= Cross-sectional random effects of respondent i.
 = Stochastic random error of respondent i under scenario s.
= Stochastic random error of respondent i under scenario s.
The formula can be estimated using the Maximum Likelihood Estimation (MLE) method using Gauss-Hermite Quadrature Algorithm.
the time-trade-off for port-wine stain treatment, multivariate analysis using the random effects logit model for the respondents’ decision on discrete choice experiment questions based on different scenarios was employed.
Index function of random effects logistic model can be stated as:
where:  = Decision to treat the patient of respondent i under scenario s, equals to 1 for yes, and 0 otherwise.
= Decision to treat the patient of respondent i under scenario s, equals to 1 for yes, and 0 otherwise.
 = Time spending for port-wine stain laser treatment (hours per visit) for respondent i under scenario s.
= Time spending for port-wine stain laser treatment (hours per visit) for respondent i under scenario s.
 = Number of additional visits to reach k% improvement from the based case of 40% improvement that respondent i faced under scenario s, where k =1 for 60% (=5 visits), 2 for 70% (=5 visits), 3 for 80% (=9 visits), and 4 for 100% (=24 visits).
= Number of additional visits to reach k% improvement from the based case of 40% improvement that respondent i faced under scenario s, where k =1 for 60% (=5 visits), 2 for 70% (=5 visits), 3 for 80% (=9 visits), and 4 for 100% (=24 visits).
 = Cross-sectional random effects of respondent i.
= Cross-sectional random effects of respondent i.
 = Stochastic random error of respondent i under scenario s.
= Stochastic random error of respondent i under scenario s.
The formula can be approximated using the Gauss-Hermite Quadrature Algorithm and the Maximum Likelihood Estimation (MLE) approach.
The statistical analysis was conducted using Stata (Stata-Corp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). The p-value less than 0.05 was considered statistically significant.
The ethical committee of the Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University, approved this study (certificate of approval no. si 1059/2020). The study adhered to the guidelines of the Declaration of Helsinki of 1964 and its later amendments. Additionally, this research was registered with the Thai Clinical Trials Registry (identification number TCTR20201110003). Written informed consent was obtained from all participants over the age of 20. Parental informed consent was also obtained from the parents/legal guardians of study participants under the age of 20 prior to study commencement.
Results
Forty-six respondents was included in the final analysis. The demographic data were categorized by gender and age of the respondents enrolled and are presented in Table 1. The majority of the gender was female, with 68.4% in age <5 and 63.0% in age≥ 5.
 |
Table 1 Respondents Categorized by Gender and Age |
To estimate WTP based on gender and age, WTP for the base case at 40% improvement costs 6109.01 baht per visit in Table 2. The result showed decreasing trend of cost that parents willing to pay from base case at 40% improvement of 3.71% (5882.32 baht), 6.41% (5717.29 baht), 9.61% (5521.77 baht) and 10.83% (5453.45 baht) for the improvement of 60–70–80% and 100%, respectively. When comparing based on gender and age groups, the female was willing to pay 6341.28 baht per visit while the male was willing to pay 5429.19 per visit at a 40% improvement. Patients under 5 were willing to pay only 2822.44 baht, while the older age group paid 6751.75 baht (Table 2, Table S1).
 |
Table 2 Estimated Results of Willingness to Pay and Subsample Analysis Based on Gender and Age (Unit: Baht per Visit) |
For the total willingness to pay in the sub-sample based on gender and age, the total WTP at 40% improvement at 5 visits of laser treatment was 30,545 baht. The estimated total WTP were 59,957-baht, 88,543-baht, 138,239-baht and 269,122-baht for 60–70–80%-100% improvement. When expected 100% improvement, patients aged more than 5 years were willing to pay the highest amount of 300,804 baht for treatment of PWS. Moreover, females were more willing to pay than males at any improvement level. The parents of the patient more than 5 years were also willing to pay more than younger ages, as shown in Table 3.
 |
Table 3 Estimated Results of Total Willingness to Pay and Subsample Analysis Based on Gender and Age (Unit: Baht) |
Regarding TTO, patients are willing to spend 9.95 hours per visit for the based case clinical improvement of 40% (Table 4). The result showed that Female was willing to spend time 10.36 hour per visit while males were willing to spend 7.32 hour per visit for a 40% improvement. The pattern of decrease in time spent was similar to the willingness to pay of the patients in total, gender, and age groups. Youngers aged less than 5 years were willing to spend less time compared to patients with age more than 5 years, which were 6.10 hours per visit and 10.65 hours per visit, respectively (Table 4, Table S2).
 |
Table 4 Estimated Results of Time Trade off and Subsample Analysis Based on Gender and Age (Unit: Hours per Visit) |
Estimated Results of TTO based on household income, which categorized the income group into <20k, 20k-40k, 40k–100k, and >100k baht per month in Table 5. In based case (40% improvement), Families with 40k–100k income were willing to spend the longest time compared to another group, while families with >100k income per month were willing to spend 7.04 hours per visit. The trend of time spent decreased when the improvement of the lesion increased (Table 5, Table S3).
 |
Table 5 Estimated Results of Time Trade off and Subsample Analysis Based on Income (Unit: Hours per Visit) |
Discussion
Port-wine stains are congenital conditions that impair individuals’ appearance and are associated with a social stigma.15 The facial PWS would significantly affect QoL, and the effect would be similar to other obvious skin conditions such as vitiligo and alopecia.16 Patients with PWS generally suffer from significant psychological impairments. These conditions do not improve with advancing age and may cause further adaptation issues to their social environment.6 Clinicians caring for patients with PWS should consider QoL when discussing long-term strategies and the optimal number of treatments to be cost-effective.
In clinical decision-making, patients are often involved in eliciting values for health conditions that possibly concern outcomes related to their disease and the optimal number of treatments.17 At the individual level, we must establish what people wish or desire regarding health outcomes and what trade-offs they are willing to make to achieve desirable results.13 Our concern in this study is how to integrate welfare economics and decision sciences to make cost-effective treatment until the patients achieve desirable outcomes. In our previous study, we calculated the prediction of the clinical improvement from the laser treatment sessions based on the estimated fixed-effects model. The first five treatments are expected to provide a 40% improvement, while the following five treatments (treatments 6–10) will lead to an additional gain of 20%. Due to the rapid decline in its clinical efficacy, the third five treatments (visits 11–15) will only provide an additional 10% improvement, while the fourth five treatments (treatments 16–20) will provide less than 5% improvement.18 Utility metrics such as WTP can be used to quantify disease burden and influence on QoL and assess an intervention’s cost-effectiveness. WTP is a method in its intrinsic favoring of the treatment and disease.19 The estimation of WTP based on gender and age, the WTP for the base case at 40% improvement costs 6109.01 baht per visit. The result showed decreasing trend of cost that parents WTP from base case at 40% improvement of 3.71% (5882.32 baht), 6.41% (5717.29 baht), 9.61% (5521.77 baht) and 10.83% (5453.45 baht) for the improvement of 60–70–80% and 100%, respectively. Interestingly, there were apparent significant correlations between WTP with clinical improvement. The result showed a decreasing trend in the cost parents were willing to pay after a 40% improvement. These findings were consistent with Schiffner et al,12 who suggested a positive correlation between patients’ satisfaction and clinical outcome. Patients with a greater level of satisfaction would pay less for therapy than those with a lower level of satisfaction. This suggests that the more impairment in QoL, the more the patients are willing to pay for the treatment.
Time trade-off is usually used to measure a chronic health state where participants remain in the impaired health state for many years.17 In terms of TTO, patients are willing to spend their time 9.95 hours per visit for the based case clinical improvement of 40%. On average, patients with PWS were willing to give up 1.2 h per day for therapy that completely cured the disease.12 Our result showed the patients would offer around 41% for the rest of the day. TTO was more significant in our study, suggesting the patient might benefit most from the intervention. In comparison with other dermatological conditions, the TTO per day for a hypothetical cure in mild hyperpigmentation was 1.4 hours;20 melasma (1.9 hours); and psoriasis (2.8 hours).12,21 The decrease in time spent is similar to the WTP for the patients in total, gender, and age groups. Younger ages less than five years are willing to spend less time compared to patients older than five years, which are 6.10 hours per visit and 10.65 hours per visit, respectively.
Children with PWS are usually discriminated against by their peers.22 A study was conducted on children with visible facial conditions, such as PWS, burn scar, infantile hemangioma, and congenital melanocytic nevus. They tend to have impaired QoL and psychological well-being compared to the norm, but these findings were not seen in preschool children.23 Our study found a similar pattern in those patients under five who were willing to pay only 2822.44 baht while older people were willing to pay 6751.75 baht. Our study showed patients aged more than five were willing to pay and spend more time compared to patients aged less than five children. When the patient is young and socially isolated, this asymptomatic condition does not cause harm. However, as the patient ages and matures, the unique appearance of the lesion impacts the child’s self-esteem, emotional, and psychological development, which in turn affects daily life.16 This condition could be defined as a future stigma. Our previous study revealed young children had no or less concern about PWS than adolescents and young adults.5 Adolescents with PWS frequently experience rejection, exclusion, and devaluation in their daily life.24 Jiang et al15 reported that children’s QoL was more affected as they got older or the color of the lesions darkened. Initiating laser treatment earlier during infancy or early childhood could be an excellent strategy to improve the physiological and QoL to prevent future stigma. Hagen et al16 also found that improved QoL in PWS patients who received laser treatment is improved, especially if initiated during infancy or early childhood.
Sex is a key factor affecting QoL in patients with skin disorders that affect appearance.25 In particular, females with PWS reported significantly have higher median stress levels than male patients.2 Our study showed female patients are more willing to pay than males, and patients with ages more than five years are willing to spend time per visit more than males. The result showed that females were willing to spend 10.36 hours per visit while males were willing to spend 7.32 hours and paid 6341.28 baht per visit, while males were willing to pay 5429.19 per visit at a 40% improvement. Van Raath et al2 found that female PWS patients were more open to experimental and intravenous therapy than their male counterparts. According to Jiang et al,15 parents place a higher value on the looks and well-being of their daughters than they do on their sons, a finding that reflects long-standing gender disparities in parenting. When developing education and treatment programs for patients and their families, physicians should be aware that the sex of the child might predict the impact on parents’ quality of life.
Estimated Results of TTO based on household income, which categorized the income group into <20k, 20k-40k, 40k-100k, and >100k baht per month. Based on the case (40% improvement), families with 40k-100k income were willing to spend the longest time compared to other groups, while families with >100k income per month were willing to spend 7.04 hours per visit. Schiffner et al12 demonstrated that patients were willing to offer 0.3–4.5 hours per day for an imaginary therapy to get a complete cure. The TTO in our study had a significant correlation with household income. Trade-off means converting one alternative to receive another. In this study, the participants are asked to trade off the duration of time against their health status. For example, Schiffner et al12 revealed that patients with facial PWS would give about 20% (a mean value of 1.2 hours per day for therapy) of the rest of their day and are willing to pay 11.8% of their monthly income, with a daily schedule of about eight hours sleep and ten hours of employment. Several variables may affect the TTO based on household income, we believe the variations in spending time between groups in our study are due to distorting factors. The distorting elements could be divided into internal, such as time preference, and external, such as cognitive understanding.17 We are aware that specific populations might have different valuations of time. Kawakami et al26 reported there might be a connection between time preference and individual values. According to several studies, priority values are related to various health outcomes and psychological well-being,27–29 as well as other important determinants, such as personal identity, profession, attitudes, and behavior toward people.30
Limitations
The limitation of this study is a single-center study, which restricts the generalizability of our results. These results may not be generalizable to other countries with different socioeconomic status. A verification of the presented results on a larger study population and multicenter still seems necessary.
Conclusion
According to our knowledge, this is the first study to examine the relationship between WTP and TTO among PWS. There were obvious correlations between WTP and TTO with clinical outcomes. Utility indicators such as WTP and TTO can be used to measure disease burden and impact on QoL and assess the cost-effectiveness of interventions. WTP and TTO could provide a more personalized approach to improving QoL, which considers each patient’s unique treatment plan and priority. This could help with patient uncertainty and long-term planning strategies on how the patient will increases the QoL cost-effectively.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the ethics committee of the Siriraj Institutional Review Board (SIRB protocol no. 941/2563/COA no. si 1059/2020). Written informed consent was obtained for the publication and use of all patients’ data prior to their enrollment in the study. This study was performed in accordance with the Helsinki Declaration of 1964 and its subsequent amendments.
Acknowledgments
The authors wish to thank Ms. Phonsuk Yamlexnoi, Ms. Chutikan Kiatphansodsai, Ms. Apichaya Jutaphonrakul, and Dr. Thanyaporn Leesanguankul for their assistance in recruiting subjects and managing the database.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research project is supported by the Faculty of Medicine Siriraj Hospital, Mahidol University.
Disclosure
All authors declare that they have no conflicts of interest in relation to this work.
References
1. de Arruda JAA, Andrade ES, Andrade RA, Pereira JRD, Callou G. Vascular malformation of the face: a rare case with follow-up of 18 years. Acta Stomatol Croat. 2017;51(4):332. doi:10.15644/asc51/4/8
2. van Raath MI, Bambach CA, Dijksman LM, Wolkerstorfer A, Heger M. Prospective analysis of the port-wine stain patient population in the Netherlands in light of novel treatment modalities. J Cosmet Laser Ther. 2018;20(2):77–84. doi:10.1080/14764172.2017.1368669
3. Ho WS, Chan HH, Ying SY, Chan PC. Laser treatment of congenital facial port‐wine stains: long‐term efficacy and complication in Chinese patients. Lasers Surg Med. 2002;30(1):44–47. doi:10.1002/lsm.10003
4. Schiffner R, Landthaler M, Stolz W. Willingness-to-pay and time-trade-off: useful utilities in patients with psoriasis vulgaris? Dermatol Psychosom. 2000;1(3):100–103. doi:10.1159/000017516
5. Wanitphakdeedecha R, Sudhipongpracha T, Ng JNC, Yan C, Jantarakolica T. Self‐stigma and psychosocial burden of patients with port‐wine stain: a systematic review and meta‐analysis. J Cosmet Dermatol. 2021;20(7):2203–2210. doi:10.1111/jocd.14199
6. Lanigan S, Cotterill J. Psychological disabilities amongst patients with port wine stains. Br J Dermatol. 1989;121(2):209–215. doi:10.1111/j.1365-2133.1989.tb01800.x
7. Heiser A, Jowett N, Occhiogrosso J, Tessler O, Tan OT. Societal-perceived health utility of hypertrophic facial port-wine stain and laser treatment. Facial Plast Surg Aesthet Med. 2020;22(5):327–335. doi:10.1089/fpsam.2020.0059
8. De Borgie C, Bossuyt P, van der Horst C, van Gemert M. Introduction of the flash‐lamp pulsed‐dye laser treatment of facial port‐wine stains in childhood: a case of health care technology assessment. Lasers Surg Med. 2001;28(2):182–189. doi:10.1002/lsm.1037
9. Faurschou A, Olesen AB, Leonardi‐Bee J, Haedersdal M. Lasers or light sources for treating port‐wine stains. Cochrane Database Syst Rev. 2011;11. doi:10.1002/14651858.CD007152.pub2
10. Shakespeare V, Shakespeare P, Cole R. Measuring patient satisfaction with pulsed dye laser treatment of vascular lesions. Lasers Med Sci. 1998;13(4):253–259. doi:10.1007/s101030050004
11. Kaplan RM, Bush JW. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1(1):61. doi:10.1037/0278-6133.1.1.61
12. Schiffner R, Brunnberg S, Hohenleutner U, Stolz W, Landthaler M. Willingness to pay and time trade‐off: useful utility indicators for the assessment of quality of life and patient satisfaction in patients with port wine stains. Br J Dermatol. 2002;146(3):440–447. doi:10.1046/j.1365-2133.2002.04613.x
13. Torrance GW. Utility measurement in healthcare. Pharmacoeconomics. 2006;24(11):1069–1078. doi:10.2165/00019053-200624110-00004
14. Stefanidou M, Evangelou G, Kontodimopoulos N, et al. Willingness to pay and quality of life in patients with pruritic skin disorders. Arch Dermatol Res. 2019;311(3):221–230. doi:10.1007/s00403-019-01900-5
15. Jiang F, Shao J, Chen L, Yang N, Liu J, Li Z. Influence of port-wine stains on quality of life of children and their parents. Acta Derm Venereol. 2021;101(8):adv00516–adv00516. doi:10.2340/00015555-3883
16. Hagen SL, Grey KR, Korta DZ, Kelly KM. Quality of life in adults with facial port-wine stains. J Am Acad Dermatol. 2017;76(4):695–702. doi:10.1016/j.jaad.2016.10.039
17. Lugnér AK, Krabbe PF. An overview of the time trade-off method: concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert Rev Pharmacoecon Outcomes Res. 2020;20(4):331–342. doi:10.1080/14737167.2020.1779062
18. Wanitphakdeedecha R, Jantarakolica T, Ng JNC, et al. The cost-effectiveness of pulsed-dye laser therapy among Thai patients with facial port-wine stain: a retrospective study and economic evaluation. Dermatol Ther. 2021;11(2):465–473. doi:10.1007/s13555-021-00484-1
19. Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996;276(14):1172–1177. doi:10.1001/jama.1996.03540140060028
20. Maymone MB, Rajanala S, Widjajahakim R, Secemsky E, Saade D, Vashi NA. Willingness-to-pay and time trade-off: the burden of disease in patients with benign hyperpigmentation. J Clin Aesthet Dermatol. 2019;12(5):46.
21. Leeyaphan C, Wanitphakdeedecha R, Manuskiatti W, Kulthanan K. Measuring melasma patients’ quality of life using willingness to pay and time trade-off methods in Thai population. BMC Dermatol. 2011;11(1):1–8. doi:10.1186/1471-5945-11-16
22. Demellweek C, Humphris GM, Hare M, Brown J. Children’s perception of, and atitude towards, unfamiliar peers with facial port-wine stains. J Pediatr Psychol. 1997;22(4):471–485. doi:10.1093/jpepsy/22.4.471
23. Masnari O, Schiestl C, Rössler J, et al. Stigmatization predicts psychological adjustment and quality of life in children and adolescents with a facial difference. J Pediatr Psychol. 2013;38(2):162–172. doi:10.1093/jpepsy/jss106
24. van der Horst CM, De Borgie CA, Knopper JL, Bossuyt PM. Psychosocial adjustment of children and adults with port wine stains. Br J Plast Surg. 1997;50(6):463–467. doi:10.1016/S0007-1226(97)90335-0
25. Maul JT, Navarini A, Sommer R, et al. Gender and age significantly determine patient needs and treatment goals in psoriasis–a lesson for practice. J Eur Acad Dermatol Venereol. 2019;33(4):700–708. doi:10.1111/jdv.15324
26. Kawakami N, Watanabe K, Nishi D, Takagi D, Hashimoto H, Tanaka SC. Time preference and personal value: a population-based cross-sectional study in Japan. BMC Psychol. 2020;8(1):1–11. doi:10.1186/s40359-020-00458-6
27. Sagiv L, Schwartz SH. Value priorities and subjective well‐being: direct relations and congruity effects. Eur J Soc Psychol. 2000;30(2):177–198. doi:10.1002/(SICI)1099-0992(200003/04)30:2<177::AID-EJSP982>3.0.CO;2-Z
28. Bobowik M, Basabe N, Páez D, Jiménez A, Bilbao M. Personal values and well-being among Europeans, Spanish natives and immigrants to Spain: does the culture matter? J Happiness Stud. 2011;12(3):401–419. doi:10.1007/s10902-010-9202-1
29. Yasuma N, Watanabe K, Iida M, Nishi D, Kawakami N. Personal values in adolescence and psychological distress in adults: a cross-sectional study based on a retrospective recall. PLoS One. 2019;14(11):e0225454. doi:10.1371/journal.pone.0225454
30. Schwartz SH. Universals in the content and structure of values: theoretical advances and empirical tests in 20 countries. In: Advances in Experimental Social Psychology. Vol. 25. Elsevier; 1992:1–65.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.