Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Vitamin D and vitamin D receptor levels in children with attention-deficit/hyperactivity disorder
Authors Sahin N, Altun H, Kurutas EB , Balkan D
Received 27 November 2017
Accepted for publication 21 December 2017
Published 19 February 2018 Volume 2018:14 Pages 581—585
DOI https://doi.org/10.2147/NDT.S158228
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Nilfer Sahin,1 Hatice Altun,2 Ergül Belge Kurutas,3 Damla Balkan1
1Department of Child and Adolescent Psychiatry, Muğla Sıtkı Koçman University, Muğla, Turkey; 2Department of Child and Adolescent Psychiatry, Kahramanmaras Sutcu Imam University, Kahramanmaras, Turkey; 3Department of Biochemistry, Kahramanmaras Sutcu Imam University, Kahramanmaras, Turkey
Objective: In this study, we aimed to evaluate vitamin D and vitamin D receptor levels in children with attention-deficit/hyperactivity disorder (ADHD).
Patients and methods: In this cross-sectional study, a total of 80 children including 40 ADHD patients (aged 6–12 years; 28 males and 12 females) and 40 age-, sex-, and season of blood collection-matched controls (aged 6–12 years; 25 males and 15 females) were enrolled. Serum vitamin D and vitamin D receptor levels and calcium, phosphorus, and alkaline phosphatase were measured. The vitamin D receptor levels in the serum were measured using the quantitative sandwich enzyme immunoassay technique.
Results: Serum vitamin D and vitamin D receptor levels were found to be significantly lower in children with ADHD compared to healthy controls. No significant differences were found in serum calcium, phosphorus, and alkaline phosphatase levels. No significant differences were found among the ADHD subtypes in terms of serum vitamin D, vitamin D receptor, calcium, phosphorus and alkaline phosphatase levels.
Conclusion: This study suggests that children with ADHD have lower levels of vitamin D and vitamin D receptor. According to the authors’ knowledge, this is the first study to describe vitamin D receptor levels in ADHD.
Keywords: attention-deficit/hyperactivity disorder, vitamin D, vitamin D receptor
Introduction
Characterized by attention deficit and hyperactivity/impulsivity symptoms, attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder with childhood onset likely to persist into the adulthood. A comprehensive meta-analysis has estimated its prevalence to be 5.29%.1 It is almost three times more common in men than in women.2 Although it is a common disease, its etiology still remains largely unknown. Family, twin, adoption, and candidate gene studies have shown that genetic factors play a major role in the disease onset.3 In addition, various trace element deficiencies, vitamin deficiencies, polyunsaturated fatty acid deficiencies, and chemical exposures are blamed in its etiology.4 Furthermore, vitamin deficiencies are among the most discussed topics lately. In particular, vitamin D abnormalities are blamed in the etiology.5
Vitamin D is a fat-soluble vitamin which is involved in calcium (Ca) and phosphorus (P) homeostasis, with hormone-like functions. Blood, Ca, and P levels play an important role in regulating its synthesis. Being an intermediary metabolite and an endogenous vitamin precursor in the skin, cholecalciferol (inactive) can be synthesized from 7-dehydrocholesterol after ultraviolet irradiation, and inactive vitamin D is synthesized from animal-derived (cholecalciferol) and plant-derived (ergocalciferol) foods through diet, then activated in the body.6,7 1,25-Dihydroxycholecalciferol is its active form and plays a role in stimulating or suppressing >900 gene expressions, binding to steroid hormone receptor proteins in the nucleus (vitamin D receptor [VDR]).8
Vitamin D is also involved in bone production and cellular and neuromuscular functions. In addition, it has been shown that vitamin D is effective on the cardiovascular and immune systems.9
Recent studies have demonstrated that vitamin D stimulates cellular proliferation, differentiation, neurotransmission, and neuroplasticity in the central nervous system, and has neurotrophic and neuroprotective effects. The nerve growth factor is involved in the expression of neurotrophin-3, neurotrophin-4, and glial cell line-derived neurotrophic factor. However, its association with brain-derived neurotrophic factor expression still remains unclear. On the other hand, VDR has been found in the cerebellum, thalamus, hypothalamus, basal ganglia, hippocampus, olfactory system, temporal lobe, and orbital lobes of the central nervous system.10 Although the etiological role of vitamin D deficiency in psychiatric disease remains somewhat unclear, an association has been shown between many diseases and vitamin D deficiency, including depression, schizophrenia, autism spectrum disorder, and ADHD.11–14
Alterations in the cortico-striato-thalamic circuits and cerebellum through brain imaging studies to shed light on the etiology of ADHD and the presence of VDR in these regions have guided us through this study. Although previous studies have investigated the relationship between ADHD and vitamin D levels, in this study, we aimed to evaluate vitamin D and VDR levels in children with ADHD. To the best of our knowledge, this is the first study evaluating the relationship between VDR levels and ADHD in the literature.
Patients and methods
In this cross-sectional study, a total of 80 children including 40 ADHD patients (age: 6–12 years; 28 males and 12 females) and 40 age-, sex-, and season of blood collection-matched controls (age: 6–12 years; 25 males and 15 females) were enrolled. The diagnosis of ADHD was made based on clinical interview using the Diagnostic and Statistical Manual of Mental Disorders, Fifth edition.15 The Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version was conducted to support the diagnosis of ADHD and to rule out comorbid psychiatric disorders.16 It is a semi-structured interview, and the Turkish adaptation was conducted by Gökler et al.17 The ADHD group patients were not using any medication, when the blood samples were taken or in the preceding 6 weeks. Those with learning disabilities and autism spectrum disorders and genetic syndromes or any medical disorder, metabolic disorders, neurologic diseases, and those using vitamin and mineral supplementation within the past 6 months and/or drugs affecting vitamin D metabolism were excluded from the study. Children with no known neurodevelopmental/neurologic disorder, infection, and/or no history of vitamin and mineral supplements were selected as healthy controls. Medical disorders were excluded through screening the medical history, clinical examination findings by the pediatrician, and routine laboratory test results, including biochemical, hematologic, and thyroid function tests. The control group consisted of age-, sex-, and season of blood collection-matched participants. For both groups, those with an IQ of over 80 were included in the study.
The parents of the children were given the Conners’ Parent Rating Scale-Revised Long Form.18,19 The patient and control group teachers completed the Conners’ Teacher Rating Scale.20–22 For each patient, height and weight were recorded and the body mass index (BMI) values were calculated.
The study was approved by the local Ethics Committee of Sutcu Imam University, Faculty of Medicine, Kahramanmaras, Turkey and conducted in accordance with the principles of the Declaration of Helsinki. A written informed consent was obtained from each patient and parent.
Biochemical measurements
Venous blood samples were collected to measure serum vitamin D, VDR, Ca, potassium (P), and alkaline phosphatase (ALP) levels between 8:00 AM and 10:00 AM. The serum were collected and kept at −20°C until analysis. All patients were examined between March and September to eliminate vitamin D deficiency in the winter time. Vitamin D and VDR levels in the samples were analyzed using enzyme-linked immunoassay. In addition, Ca, P, and ALP were analyzed using the automated standard spectrophotometric laboratory method.
Statistical analysis
Statistical analysis was performed using the SPSS for Windows version 22.0 software package (IBM Corp., Armonk, NY, USA). Descriptive statistics were expressed in mean ± SD, and number (n) and frequency (%). The patient and control groups were compared using the chi-square test for categorical variables and independent sample t-test for the analysis of parametric numerical data. A p-value of <0.05 was considered statistically significant.
Results
Eighty individuals were included in the study. The mean age of the ADHD group (n=40) was 8.65±1.53 years, and 28 (70%) were males. The mean age of the control group (n=40) was 8.77±1.73 years, and 25 (62.5%) were males. Sociodemographic characteristics are shown in Table 1. No significant differences were found between the groups in terms of age, sex, weight, height, and BMI (p>0.05 for all). In addition, no significant differences in the birth seasons or seasons of blood collection were found.
  | Table 1 Sociodemographic characteristics of the study groups |
The mean serum vitamin D levels in the ADHD and control groups were 24.10±3.98 and 32.71±4.26 ng/mL, respectively, indicating statistical significance (p<0.001). The serum VDR levels were statistically significant and decreased in children with ADHD, compared to the healthy controls (1.69±0.22 vs 2.08±0.42 ng/mL, respectively, p<0.001; Table 2).
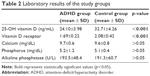  | Table 2 Laboratory results of the study groups |
In the ADHD and control groups, the mean Ca levels were 9.7±0.6 and 9.6±0.8 mg/dL, P levels were 5.2±1.2 and 5.1±0.4 mg/dL, and ALP levels were 193.5±48.4 and 191.3±60.7 U/L, respectively, indicating no statistically significant difference between the groups (p>0.05 for all; Table 2).
According to the ADHD subtype, the inattentive subtype (n=18, 45%) was the most prevalent type, followed by the combined subtypes (n=16, 40%) and the hyperactive/impulsive type (n=6, 15%). No significant differences were found among the ADHD subtypes in terms of serum vitamin D, VDR, Ca, P, and ALP levels (p>0.05 for all).
Discussion
In this study, we found that serum vitamin D and VDR levels in children with ADHD were lower than in healthy children. However, no significant differences were found between the ADHD and control groups in terms of serum Ca, P, and ALP levels.
In recent studies, vitamin D deficiency has been associated with anxiety disorders, mood disorders, and neurodevelopmental disorders.11,14,23 Vitamin D has been reported to have effects on brain development and function as a neuro-immunomodulator leading to behavioral and neuropsychiatric diseases.24,25 Certain components of the immune system, particularly the T cells, B cells, cytokines, and even regulatory T cells, affect congenital and adaptive immunity.26,27 Several studies have found an evidence to suggest that vitamin D supports normal brain growth, increases neuroprotection, and modulates matrix metalloproteinases and anti-inflammatory mechanisms, which are vital components for the brain.28,29 Animal studies have shown that developmental vitamin D deficiency resulted in brain abnormalities, enlarged lateral ventricles, weak tissue differentiation, and reduced expression of neurotrophic factors.28 In addition, clinical studies have shown that such brain changes in these animals manifested as abnormal behavioral changes and hyperlocomotion.30
Furthermore, vitamin D levels were previously investigated in ADHD case–control studies. In a study, Kamal et al31 compared vitamin D levels in 1,331 children with ADHD and 1,331 healthy children, and reported that vitamin D levels were significantly lower in the group with ADHD. However, consistent with our study findings, studies conducted by Sharif et al,14 Villagomez and Ramtekkar,32 Garipardic et al,33 and Goksugur et al34 found vitamin D levels to be lower in patients with ADHD than in healthy subjects. These findings suggest that vitamin D deficiency may have a role in the etiopathogenesis of ADHD. In addition, vitamin D deficiency is very common in children diagnosed with ADHD. In a study, Bener and Kamal35 found severe (<10 ng/mL) and moderate (10–20 ng/mL) levels of vitamin D deficiency in 64% of the patients diagnosed with ADHD.
Vitamin D affects brain development starting from the prenatal period. In their study, Mossin et al36 found a correlation between cord blood vitamin D levels under <25 or <30 nmol/L and ADHD, and suggested that prenatal vitamin D prophylaxis could be effective. Similarly, Daraki et al37 and Morales et al38 found a negative correlation between high vitamin D levels in the maternal circulation and symptoms resembling childhood ADHD. However, in their study using umbilical blood samples, Gustafsson et al39 found no significant correlation between vitamin D levels in the cord blood and ADHD findings. However, statistical drawbacks of the study and a small sample size were the main limitations of the study.
In this study, we attempted to shed light on the etiopathogenesis of ADHD, and consistent studies in the literature provide deeper insights on ADHD and guide us through novel treatment approaches. A double-blind, placebo-controlled study conducted by Mohammadpour et al40 compared methylphenidate + vitamin D supplementation with methylphenidate + placebo. Although the total ADHD symptom scores remained identical between the two groups, there was more control over the evening symptoms in the group treated with vitamin D.
Although the serum Ca and P levels are in normal ranges, it has been shown that mutations associated with VDR gene can inhibit vitamin D metabolism, thereby resulting in neurodevelopmental disorders.41 This study found no significant differences in serum Ca, P, and ALP levels in the group with ADHD and in the control group. Vitamin D exerts its effects by binding to VDR, which is found in various tissues, including the brain tissue and peripheral nerves.9 The VDR gene plays an important role in bone mineralization and vitamin D metabolism. Animal studies also demonstrated that VDRs were found in dopaminergic neurons.42 In this study, we found serum VDR levels to be lower in children with ADHD than in the controls. To the best of our knowledge, there is no study investigating serum VDR levels in ADHD. Based on our study results, we consider that low VDR levels can affect ADHD, irrespective of vitamin D levels. However, this is the first study evaluating serum VDR levels in patients with ADHD; therefore, further studies are needed to evaluate the correlation between VDR and ADHD.
Additionally, in this study, the lack of a significant difference between the two groups in terms of age, sex, weight, height, and BMI is useful to eliminate bias. Also, the fact that the blood samples were collected between March and September prevented low vitamin D bias associated with sun exposure during the winter season.
Limitations
Nonetheless, there are certain limitations to this study. Its cross-sectional design and small sample size are the main limitations. It is known that vitamin D can be obtained easily through synthesis by exposure to sunlight or through oral intake. An important limitation of this study is that it was not known how many hours the children in the study were exposed to sunlight. Individuals with ADHD are known to be often injured because of inattention and hyperactivity; as it was not known whether these children were restricted in outdoor physical activities to prevent injuries, this is also a limitation of the study. Lack of information about the oral diet habits, which is one of the factors that could affect vitamin D levels, was also evaluated as a limitation of the study.
Conclusion
In conclusion, our study suggests that low serum vitamin D and VDR can play an important role in the etiopathogenesis of ADHD. However, this is the first study identifying VDR levels in ADHD and evaluating the correlation between ADHD and VDR; therefore, further studies are needed to identify the exact mechanism of the contributions of these parameters on the etiology and treatment of ADHD. Furthermore, a more controlled study is needed to evaluate vitamin D intake in ADHD patients. Further studies are also needed to clarify the effects of vitamin D and VDR on clinical symptoms in patients with ADHD and optimal support strategies and its long-term effects on neurodevelopment in children.
Disclosure
The authors report no conflicts of interest in this work.
References
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalance of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948. | ||
Polanczyk G, Rohde LA. Epidemiyology of attention-deficit/hiperactivity disorder across the lifespan. Curr Opin Psychiatry. 2007;20(4):386–392. | ||
Sprich S, Biederman J, Crawford MH, Mundy E, Faraone SV. Adoptive and biological families of children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2000;39(11):1432–1437. | ||
Banerjee TD, Middleton F, Faraone SV. Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr. 2007;96(9):1269–1274. | ||
Bener A, Kamal M, Bener HZ, Bhugra D. Higher prevalence of iron deficiency as strong predictor of attention deficit hyperactivity disorder in children. Ann Med Health Sci Res. 2014;4 (Suppl 3):S291–S297. | ||
Brown AJ, Dusso A, Slatopolsky E. Vitamin D. Am J Physiol. 1999;277(2 Pt 2):F157–F175. | ||
Spiro A, Buttriss JL. Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39(4):322–350. | ||
Pike JW, Meyer MB, Martowicz ML, et al. Emerging regulatory paradigms for control of gene expression by 1,25-dihydroxyvitamin D3. J Steroid Biochem Mol Biol. 2010;121(1–2):130–135. | ||
Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G. Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev. 2016;96(1):365–408. | ||
Walbert T, Jirikowski GF, Prüfer K. Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in the limbic system of the rat. Horm Metab Res. 2001;33(9):525–531. | ||
Bener A, Khattab AO, Al-Dabbagh MM. Is high prevalence of Vitamin D deficiency evidence for autism disorder? In a highly endogamous population. J Pediatr Neurosci. 2014;9(3):227–233. | ||
Chiang M, Natarajan R, Fan X. Vitamin D in schizophrenia: a clinical review. Evid Based Ment Health. 2016;19(1):6–9. | ||
Józefowicz O, Rabe-Jabłonska J, Wozniacka A, Strzelecki D. Analysis of vitamin D status in major depression. J Psychiatr Pract. 2014;20(5):329–337. | ||
Sharif MR, Madani M, Tabatabaei F, Tabatabaee Z. The relationship between serum Vitamin D levels and attention deficit hyperactivity disorder. Iran J Child Neurol. 2015;9(4):48–53. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Ed. (DSM-5). USA: American Psychiatric Publishing; 2013. | ||
Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. | ||
Gökler B, Ünal F, Pehlivantürk B, Kültür EÇ, Akdemir D, Taner Y. Reliability and validity of schedule for affective disorders and schizophrenia for school age children-present and lifetime version-turkish version (K-SADS-PL-T). Turk J Child Adolesc Ment Health. 2004;11(3):109–116. | ||
Conners CK. Manual for the Conners’ Rating Scales-Revised. North Tonawanda, NY, USA: Multi-Health Systems; 1997. | ||
Kaner S, Büyüköztürk Ş, Işeri E, Ak A, Özaydin L. Validity and reliability study of the Conners’ Parent Rating Scale Revised Long Form. Antalya, XVI: National Child and Adolescent Psychiatry Meeting; 2006. | ||
Goyette CH, Conners CK, Ulrich RF. Normative data on revised Conners parent and teacher rating scales. J Abnorm Child Psychol. 1978;6(2):221–236. | ||
Dereboy Ç, Şenol S, Şener Ş, Dereboy F. Validity of the Turkish version short form Conners’ teacher and parent rating scales. Turk Psikiyatri Derg. 2007;18(1):48–58. | ||
Şener S, Dereboy C, Dereboy IF, Sertcan Y. Conners’ teacher rating scale Turkish version – I. Turk J Child Adolesc Ment Health. 1993;2(3):131–141. | ||
Chu F, Ohinmaa A, Klarenbach S, Wong ZW, Veugelers P. Serum 25-hydroxyvitamin D concentrations and indicators of mental health: an analysis of the Canadian Health Measures Survey. Nutrients. 2017;9(10):E1116. | ||
Fernandes de Abreu DA, Eyles D, Feron F. Vitamin D, a neuro-immunomodulator: implications for neurodegenerative and autoimmune diseases. Psychoneuroendocrinology. 2009;34 (Suppl 1):S265–S277. | ||
Eyles DW, Burne TH, McGrath JJ. Vitamin effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. 2013;34(1):47–64. | ||
Hewison M. Vitamin D and innate and adaptive immunity. Vitam Horm. 2011;86:23–62. | ||
Urry Z, Chambers ES, Xystrakis E, et al. The role of 1alpha,25-dihydroxyvitamin D3 and cytokines in the promotion of distinct Foxp3+ and IL-10+ CD4+ T cells. Eur J Immunol. 2012;42(10):2697–2708. | ||
Eyles DW, Feron F, Cui X, et al. Developmental vitamin D deficiency causes abnormal brain development. Psychoneuroendocrinology. 2009;34 (Suppl 1):S247–S257. | ||
Vinh Quoc Luong K, Thi Hoang Nguyen L. Vitamin D and Parkinson’s disease. J Neurosci Res. 2012;90(12):2227–2236. | ||
Groves NJ, Kesby JP, Eyles DW, McGrath JJ, Mackay-Sim A, Burne TH. Adult vitamin D deficiency leads to behavioural and brain neurochemical alterations in C57BL/6 J and BALB/c mice. Behav Brain Res. 2013;241:120–131. | ||
Kamal M, Bener A, Ehlayel MS. Is high prevalence of vitamin D deficiency a correlate for attention deficit hyperactivity disorder? Atten Defic Hyperact Disord. 2014;6(2):73–78. | ||
Villagomez A, Ramtekkar U. Iron, magnesium, vitamin D, and zinc deficiencies in children presenting with symptoms of attention-deficit/hyperactivity disorder. Children (Basel). 2014;1(3):261–279. | ||
Garipardic M, Doğan M, Bala KA, et al. Association of attention deficit hyperactivity disorder and autism spectrum disorders with mean platelet volume and vitamin D. Med Sci Monit. 2017;23:1378–1384. | ||
Goksugur SB, Tufan AE, Semiz M, et al. Vitamin D status in children with attention-deficit–hyperactivity disorder. Pediatr Int. 2014;56(4):515–519. | ||
Bener A, Kamal M. Predict attention deficit hyperactivity disorder? Evidence-based medicine. Glob J Health Sci. 2014;6(2):47–57. | ||
Mossin MH, Aaby JB, Dalgård C, Lykkedegn S, Christesen HT, Bilenberg N. Inverse associations between cord vitamin D and attention deficit hyperactivity disorder symptoms: A child cohort study. Aust N Z J Psychiatry. 2017;51(7):703–710. | ||
Daraki V, Roumeliotaki T, Koutra K, et al. High maternal vitamin D levels in early pregnancy may protect against behavioral difficulties at preschool age: the Rhea mother–child cohort. Eur Child Adolesc Psychiatry. Epub 2017 Jul 6. | ||
Morales E, Julvez J, Torrent M, et al. Vitamin D in pregnancy and attention deficit hyperactivity disorder-like symptoms in childhood. Epidemiology. 2015;26(4):458–465. | ||
Gustafsson P, Rylander L, Lindh CH, et al. Vitamin D status at birth and future risk of attention deficit/hyperactivity disorder (ADHD). PLoS One. 2015;10(10):e0140164. | ||
Mohammadpour N, Jazayeri S, Tehrani-Doost M, et al. Effect of vitamin D supplementation as adjunctive therapy to methylphenidate on ADHD symptoms: A randomized, double blind, placebo-controlled trial. Nutr Neurosci. 2016;7:1–8. | ||
Goltzman D, Hendy GN, White JH. Vitamin D and its receptor during late development. Biochim Biophys Acta. 2015;1849(2):171–180. | ||
Cui X, Pelekanos M, Liu PY, Burne TH, McGrath JJ, Eyles DW. The vitamin D receptor in dopamine neurons; its presence in human substantia nigra and its ontogenesis in rat midbrain. Neuroscience. 2013;236:77–87. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
